Abstract
Background:
Providing the right care for each individual patient is a key element of quality palliative care. Complexity is a relatively new concept, defined as the nature of patients’ situations and the extent of resulting needs. Classifying patients according to the complexity of their care needs can guide integration of services, anticipatory discussions, health service planning, resource management and determination of needs for specialist or general palliative care. However, there is no consistent approach to interpreting and classifying complexity of patient needs.
Aim:
The aim of this article is to identify and describe classification systems for complexity of patient care needs in palliative care.
Design:
Narrative systematic review (PROSPERO registration number CRD42020182102).
Data sources:
MEDLINE, Embase, CINAHL and PsychINFO databases were searched without time limitations. Articles were included that described classification systems for complexity of care requirements in populations with palliative care needs.
Results:
In total, 4301 records were screened, with nine articles identified reporting the use of patient classification systems in populations with palliative care needs. These articles included the use of six classification systems: HexCom, Perroca Scale, AN-SNAP, Hui Major Criteria, IDC-Pal and PALCOM. These systems were heterogenous in the manner they determined complexity of care needs. The HexCom and IDC-Pal systems contained items that covered all domains of complexity as described by Hodiamont; personal, social support, health care team and environment.
Conclusion:
Although six classification systems have been developed, they access differing aspects of care needs and their application has been limited. The HexCOM and IDC-Pal systems offer the broadest determinations of complexity from an individual perspective. Further research is needed to apply these systems to populations external to those in which they were developed, and to appreciate how they may integrate with, and impact, clinical care.
Keywords: Palliative care, complexity, classification, casemix classification, patient needs, systematic review
What is known about this topic?
Complexity is defined as the nature of patients’ situations and the extent of resulting needs and care demands
An understanding of individual patient complexity can assist in facilitating discussions relating to future care, guiding integration of services, health service planning, resource management and determination of needs for specialist or general palliative care.
Classification systems can provide a systematic approach to determining patient complexity
What this paper adds?
This paper identifies six classification systems that have been applied to populations with palliative care needs.
These systems are heterogeneous, accessing differing aspects of care needs. The HexCOM and IDC-Pal systems offer the broadest determinations of complexity from an individual perspective.
Implications for practice, theory or policy
Complexity is an emerging concept, and there is a need for standardisation as to how it is defined, measured and applied to clinical care.
Classification systems may enable a systematic approach to determining care based on patient’s needs.
Further research is required to apply these classification systems to other populations and settings, in particular developing countries where issues of access and resource limitations may take precedence.
Background
Patients who receive palliative care are heterogeneous; with vastly different underlying personal needs, medical histories, symptom concerns and family and caregiver support.1 Equally, their situations are influenced by external factors, such as living environment, health system resources, formal and informal services and access to care. Their resultant needs and preferences for care, and those of their families and carers, are diverse. There has been an increasing focus in palliative care to appreciate the extent of these care needs, to proactively engage appropriate services and care at the right time for each individual. Current evidence suggests that access to specialist palliative care services poorly correlates with care requirements, which are more often determined by diagnosis, age, location and socio-economic factors.2 This is of increasing relevance as we are faced with older, multimorbid populations; the requirements for multi-disciplinary care to facilitate their multiple care needs; and the systemic effects of health systems balancing limited resources and specialist services.2 For many patients, palliative care may be optimally provided through existing general and primary health services that is appropriate to their and their family’s needs, wishes and set within their own sociocultural setting.3 A systematic approach to classifying patient care needs is critical to proactively addressing the care requirements of the individual; to engage appropriate resources and manage health service planning, to ensure consistent and high quality palliative care.4,5
The concept of complexity has recently emerged in palliative care to characterise patient situations and the resultant care needs.2,6 Complexity is broadly defined as the nature of patients’ situations and the extent of resulting needs and care demands.6 It is widely understood that palliative care provision is challenging and subject to many influences; involving patients and their families, many care providers, systems, relationships and patients with multiple and evolving care needs.1 Complexity provides a framework to appreciate the many influencing factors impacting the provision of care. It may assist in providing an appreciation of patient situation and care needs; guiding integration of palliative care and other services, and encourage conversations with patients as to how these might be addressed.2,7 Understanding complexity of care needs may distinguish between those patients with requirements for specialist palliative care input, from those who can be managed by general or primary palliative care.6 From a health service perspective, it may enable an appreciation of the casemix of particular services, guiding resource allocation, costs, service and staff planning.8 The process of assessing patient complexity can facilitate discussions regarding the patient and families care needs and preferences; contributing to shared decision making.
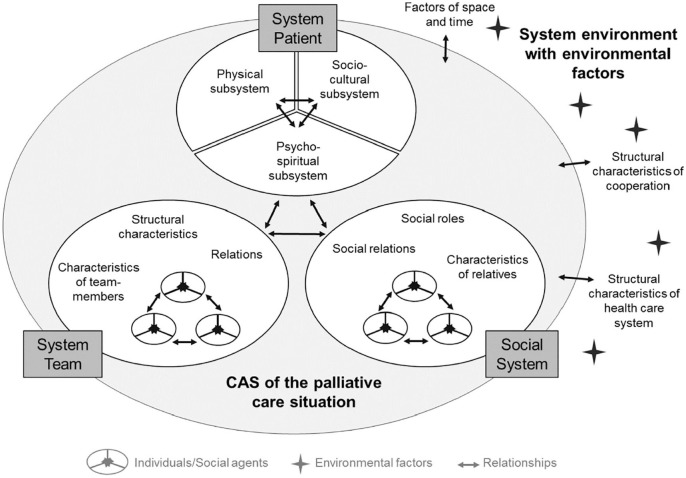
Palliative care patients are often considered to have complex care needs, yet a standardised manner to determine complexity is lacking.2 Recent articles by Pask et al.,2 and Hodiamont et al.6 have focused on the conceptual basis of complexity to consider which patients are viewed as complex, and how what factors determine this. Complexity of care needs is resultant from many aspects of the patient’s situation: their symptoms, functional ability, care environment, social support, access to services and the capacity for their formal and informal care providers to engage in care.6 Additionally, family and carers are impacted by the patient’s condition; being both providers and recipients of care.2 Importantly, complexity is not static, evolving over time in response to the perturbations of illness, environment and the supportive networks in which the patient is embedded.1,2 Put simply, the patient does not exist in isolation, and the many broad factors that impact care must be taken into account when considering level of care needs. Hodiamont et al.6 proposed a model for complexity in palliative care that will be applied to this study to appreciate these determinants as fitting within a number of domains: the patient system, social system, care team system and the environment (see Figure 1). Whilst there is no standard approach to complexity, for the purpose of this article we will operationalise this as being the quantity and extent of care needs for an individual patient, incorporating all those factors that may influence care provision across the care domains described by Hodiamont.2,6 Care needs being the ability to benefit from health care.9
Figure 1.
The palliative care situation as a complex adaptive system.6
Classification systems, or casemix classifications are designed to systematically determine the level of patient care needs; thus, classifying patients according to their complexity. Such systems have been employed in acute medicine to determine patient’s resource usage and care needs, based primarily based upon diagnoses, but have been shown to not reflect care requirements in palliative care services.2,8 It is unclear what classification systems have been developed or applied to populations with palliative care needs, which aspects of complexity they address, and their effect on clinical care. Given that complexity is a relatively new concept in palliative care, it is possible that there are classification systems may pre-date the use of this terminology. The systematic classification of patients according to the complexity of their care needs may provide important insights into the situational needs of patients; to determine care pathways, identify those who may benefit from additional care input, to assist health services in resource management, and to proactively engage with patients about their future care needs. Appreciating how complexity is understood and operationalised in different settings (i.e. home, hospice) may enable palliative care services to consider schemas relevant to their specific needs and populations.
The aim of this study is to identify and describe classification systems for complexity of patient care needs in palliative care.
Review questions
What classification systems have been used and studies to characterise complexity of patient care needs in populations with palliative care needs?
What are the main characteristics and domains of care examined through these classification systems? This includes the methodological characteristics (system of classification, validation, populations to which they have been applied) of these systems and how they represent the different domains of complexity: the patient system, the social system, the care team system and the environment.6
Methods
A narrative systemic review was conducted with literature search strategy following the PALETTE method and narrative synthesis informed by Popay’s concept mapping.10,11 This manuscript conforms to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines (PRISMA).12 The protocol was prospectively registered with Prospero (CRD42020182102).
Data sources and searches
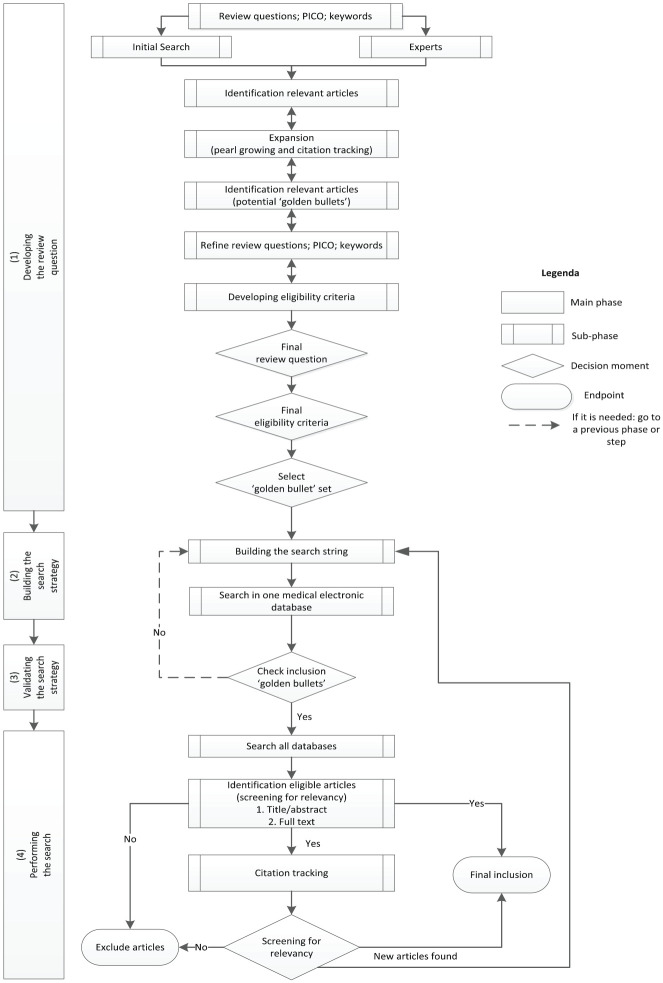
An initial scoping of the literature revealed that articles addressing aspects of this concept were not consistent in the use of terminology, especially in older articles. As such, the initial phase of this systematic review was exploratory, to understand the terminology utilised in the literature referring to classification of patient care needs, in order to allow optimal article identification. We decided to apply an iterative four-step PALETTE method described by Zwakman et al.10 (see Figure 2) to direct our search strategy.
Figure 2.
A diagrammatic representation of the PALETTE method.10
Following the PALETTE methods, the initial step involved scoping of articles through PubMed search and contact with senior researchers who had previously conducted work on complexity in palliative care.10 As a result, six key articles related to the aim of the study were identified. Backward and forward citation tracking of the six key articles yielded a total of nine highly relevant articles, referred to as ‘golden bullets’.10 ‘Golden bullets’ were articles that met at least two of the three inclusion criteria for the review. These articles were all specific to the concept of complexity in palliative care, but not solely focused on classification systems. The second step focused on building the search strategy, using the terminology, keywords and MESH headings within the ‘golden bullet’ articles. The third step involved validation of the search strategy, with numerous strategies trialled until all golden bullets were included in the search results.10 It was purposefully decided to employ a broad search strategy given the diverse range of terms used to describe the concept of complexity of patient care needs. This review used the population, interest, context (PIC) structure: palliative care, complexity and classification. This approach was broadened, through focusing the search on population (palliative care) and interest (complexity).13 This broader approach enabled capturing of all ‘golden bullets’. In the fourth step, the search strategy was finalised, included in Appendix 1. Studies were identified through searches on 17 April 2020 in computerised databases Medline (Ovid), PsycINFO, CINAHL and Embase. Searches were limited to English language and no limits applied to year of publication.
The search results were imported into reference management software (Endnote X9) and duplicates removed manually. All articles were screened independently according to eligibility criteria first on title and abstract by MG and EG, using the screening program Rayyan.14 Articles were then selected for inclusion based on full article review, assessed independently by two authors (MG and EG) for eligibility. If there was uncertainty as to whether articles fit within the inclusion criteria, they were discussed between the two authors to reach consensus, and a third author was consulted if consensus not reached.
Inclusion criteria
Publications were included in this review if the following inclusion criteria were met: (1) applicable to populations with palliative care needs; (2) complexity of care needs/casemix classification were detailed; and (3) described systems characterising patients according to level of complexity. Publications were excluded if the system was focused on paediatric palliative care or did not provide a classification of patient needs.
Articles that were published in peer-reviewed journals were included. Articles in which the full article was not written in English, conference abstracts, posters and unpublished studies were excluded.
Data extraction
A data extraction form was designed by the authors to describe the indicators of complexity and their empirical basis. It consisted of a general description, definition of complexity used by the study, results of the study, validation, development processes and domains of complexity the classification system assessed.6 Where there was a lack of information, previous articles or authors were consulted to seek further information.
Two researchers (MG and EG) conducted the data extraction. Any uncertainty was resolved between the reviewers by consensus.
Data synthesis
A narrative approach to data synthesis was adopted. The development and application of the classification tools were critically examined, and content and assessment criteria compared. The approach to data synthesis was informed by the work of Popay et al. on developing descriptive syntheses, specifically concept mapping.11
The measures used by the classification systems were mapped in accordance with domains of complexity as described by Hodiamont et al.6 (Figure 1).
Patient system
Social system
Care and team
Environment
Quality assessment
Two authors (MG and EG) completed quality assessment of each article. The articles included in this review comprised of a heterogeneous range of methods, requiring multiple assessment tools. The Joanna Briggs method-specific quality assessment tools were employed for cohort, cross-sectional studies and systematic reviews.15 For the Delphi study, in lieu of a published quality assessment tool, the EQUATOR reporting guidelines were applied to assist in assessing study quality.16 No studies were excluded based on quality assessment.
Results
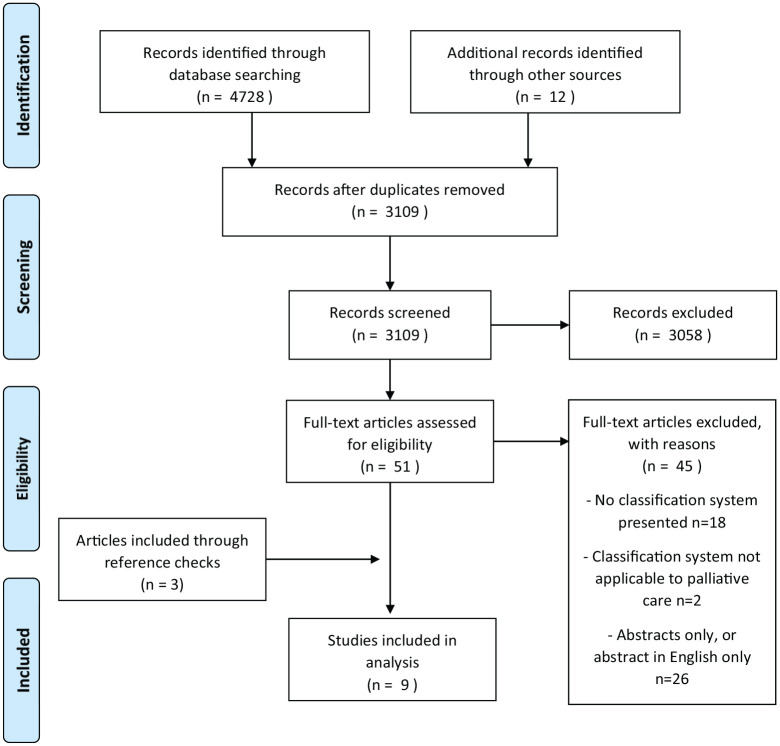
In total, 4740 records were identified through data search and other sources. Once duplicates were removed, 3109 articles were screened on title and abstract. Fifty-one articles were assessed on full-text review, with forty-five of these excluded. Six articles remained, and reference checking identified three additional articles. In total nine article were included that described classification systems in populations with palliative care needs. Figure 3 details the study selection process.
Figure 3.
PRISMA diagram.
Characteristics of included studies
The nine included studies were conducted in Australia (four), Spain (three), Brazil (one) and USA (one). Four of the studies used mixed methods, two were cohort studies, one cross-sectional, one Delphi study and one review article which subsequently presented the classification system. Details of the nine included articles are included in Table 1. In these nine articles, six different classification systems were described. They included studies published between 1997 and 2020.
Table 1.
Summary of the included articles.
| Reference | Tool | Country | Study design | Objectives | Aim of the classification system | Comparator/proxy measure of complexity | Population and size | Percentage of patients identified according to complexity rating |
|---|---|---|---|---|---|---|---|---|
| Busquet-Duran et al.17 | HexCom | Spain | Cross sectional | To describe differences in complexity across disease groups in specific home care for advanced disease and/or at the end-of-life patients, both in general and as relates to each domain and subdomain. | The instrument defines situations that are refractory to treatment options as ‘high complexity’, and situations that are difficult to resolve as ‘moderate complexity’. In this sense, classifying patients according to the level of complexity they present helps distinguish between those who need specialised palliative care and those who do not. | – | Community patients with advanced disease or at the end of life (N = 832) | High complexity 42.4%. Medium complexity 47%. Low complexity 10.2% |
| Dos Santos et al.18 | Perroca scale | Brazil | Retrospective cohort | To evaluate the complexity of care, using the Perroca scale, as well as discharges and deaths that occurred in the period. | Is a system for evaluating complexity of care, and a management tool for planning nursing care | – | Inpatient palliative care unit (N = 1568) | Four levels of complexity. – Minimal complexity 22% – Intermediate care 38% – Semi-intensive care 36% – Intensive care 4% |
| Eagar et al.20 | AN-SNAP | Australia | Cross sectional analysis | To assess the ability of commonly used patient measures to predict the resource consumption of sub-acute and non-acute patients | To classify patient casemix according to predictors of use of resources. | Health service usage – staff time, recourse consumption, services. | Palliative care N = 3104 episodes. | – |
| Eagar et al.8 | AN-SNAP | Australia, New Zealand | Cross sectional analysis | To provide a nontechnical discussion of the development of a palliative care casemix classification and some policy implications of its implementation. | To classify patient casemix according to resource usage. | Health service usage – staff time, recourse consumption, services. | Inpatient and community palliative care in Australia and New Zealand. 3866 patients, 4596 episodes of care | – |
| Eagar et al.21 | AN-SNAP | Australia, New Zealand | Cross sectional analysis | To develop a palliative care casemix classification for use in all settings including hospital, hospice and home-based care. | To classify patient casemix according to resource usage. | Health service usage – staff time, recourse consumption, services. | Inpatient and community palliative care in Australia and New Zealand. 3866 patients, 4596 episodes of care | – |
| Green and Gordon22 | AN-SNAP | Australia, New Zealand | Cross sectional analysis | To describe the first review of the AN-SNAP casemix classification. | To classify patient casemix for sub- and non-acute care that reflected costs and resource usage. | Classification system, health resource usage | 2 cohorts of inpatient and community palliative care N = 1868 episodes and N = 10,505 episodes | – |
| Hui et al.23 | USA | Delphi | To develop consensus on a list of criteria for referral of patients with advanced cancer at secondary or tertiary care hospitals to outpatient palliative care. | To optimise the use of scarce palliative-care resources, patients need to be referred at the right time for the right reasons. Therefore, consensus on simple, robust, and valid referral criteria is urgently needed. | – | – | – | |
| Martin-Rosello et al.19 | IDC-Pal | Spain | Review article | To presents the state of art of the role of complexity in specialist palliative care provision. | To diagnose and stratify complexity. It was designed to maximise consensus among professionals of the different level of care provision, facilitate effective communication between resources, and enhance a shared care model for palliative care. | – | – | – |
| Tuca et al.7 | PALCOM | Spain | Prospective cohort | To identify the factors influencing level determination of complexity, propose predictive models, and build a complexity scale of PC. | To create a predictive model of PC complexity aimed at differentiating patients with low palliative complexity, in whom basic PC would be indicated, from patients with medium-high complexity who would require shared care with specialised PC teams. | Clinician grading of complexity | Advanced cancer patients (N = 324) | High complexity 41% Medium complexity 42.9% Low complexity 16.1% |
The terminology used to describe patient care needs were not consistent throughout the articles. The term ‘complexity’ was used in four of the articles to broadly describe patient’s care and situational needs.7,17–19 The other articles described classification of patients based on care needs and resource usage. Four of these articles are all related to the one classification system in Australia (AN-SNAP); which predate the other articles, being published between 1997 and 2007.8,20–22 Hui et al.23’s article does not use the term complexity, but describes the need to identify patients with ‘complex supportive care needs who would benefit from specialist palliative care’ (p. 552).
Quality of studies
The included studies were all assessed on their quality. Of the cross-sectional studies three were of good quality, three reasonable quality and the Delphi study was of good quality. The cohort study and review were low quality.18,19 It was decided to include these studies as they describe classification systems whose development and application had been described in non-English articles. We believed it important to include these classification systems as representative of wider research, not only through the articles in which they were published in English.
Description of classification systems
Six classifications systems were described in the nine articles included in this systematic review, which are summarised in Table 2. These systems classified patients with palliative care needs according to their care needs. Three of these systems were developed in Spain (HexCom, Pal-IDC and PALCOM), and one each in Australia (AN-SNAP), Brazil (Perroca Scale) and USA (Hui Major Criteria). These systems have been used and translated to a number of languages: English, Spanish, German and Portuguese. The objective of four of the classification systems was to distinguish between those patients with general and specialist palliative care needs (HexCom, Pal-IDC, Hui, PALCOM). The Hui Major Criteria and PALCOM have been developed for, and contain items that are specific for advanced cancer populations.
Table 2.
Summary of the classification systems.
| Classification system | Classification objectives | Number of items | Patient domain items |
Care team domain items | Social domain items | Environmental domain items | Assessment tools used (individual items are described under their specific domain) | Grading | |
|---|---|---|---|---|---|---|---|---|---|
| History and function | Symptoms | ||||||||
| HexCom | To distinguish between those with specialist PC needs | 18 Items | Severity physical symptoms Emotional state Risk factors of psychological vulnerability Feeling loved Confident facing unknown Coherency of being |
Desire for hastened death Resource limitations Managing basic care needs Communication |
Family support External support networks Risk for bereavement Emotional state of family |
Access to care Financial resources planning for death Ability to manage death in care environment |
Three levels – High/Medium/Low complexity. High or medium complexity require community team intervention |
||
| Perocca scale | To evaluate the complexity of care provision | 13 Items | Mobility Limb movement Feeding Self-care Elimination |
Wound or skin issues Altered conscious state |
Frequency of observations Education needs Intravenous therapy Communication difficulties Behavioural issues Requiring oxygen |
Four levels of complexity – minimal, intermediate, semi-intensive, intensive | |||
| AN-SNAP palliative care | To classify casemix in accordance with health resource use | 9 Items total | Phase of illness Mobility Toileting Eating Transfers |
Pain Other Sx Psychospiritual Sx |
Family or carer distress | RUG-ADL PC Problem severity score (PCPSS) |
11 Classification for inpatient, 22 for community | ||
| Hui major criteria | To determine need for specialist versus general palliative care | 11 Items | Poor prognosis Progressive disease despite chemotherapy Brain metastases or leptomeningeal disease Spinal cord compression or cauda equina |
Delirium Spiritual or emotional crisis Severe physical Sx Severe emotional Sx |
Request for specialist PC Request for hastened death Assistance with decision-making and planning |
Two levels – complex (requiring specialist PC) or non-complex (general PC) | |||
| IDC-Pal | To diagnose and stratify complexity, and recommends need for specialist PC | 36 Items (35 patient items and one item to add up total score) | Paediatric patient Addiction issues Previous disability Mental illness Patient is a health professional Significant social role Abrupt change in functional autonomy |
Difficult Sx Refractory Sx, Urgent terminal Sx Difficult to control terminal Sx Progressive clinical situation Decompensated organ failure Severe cognitive Sx Severe constitutional Sx Difficult to Mx comorbidity Suicide risk Inadequate emotional coping Spiritual suffering |
Communication conflicts with health care team Request for hastened death Limitations in professional competence Difficulty in coordination of services Non-compliance issues Difficult palliative sedation Difficult medication Mx Difficult interventions |
Family communication conflict Family or carer burden Complex bereavement Inadequate family support Lack of carer competence Dysfunctional family |
Environmental limitations Difficulty accessing material or techniques |
Three levels – Non-complex – no need for specialist PC. – Complex – potential role for spec PC – High complex – spec PC recommended |
|
| PALCOM 1 | To assess complexity in palliative care, to manage referral to specialised PC services | 24 Items | Karnofsky performance status | Mechanism of pain Pain characteristics Previous narcotic use Cognitive function Psychological distress Presence of pain Asthenia Anorexia Nausea & Vomiting Constipation Dyspnoea Somnolence Insomnia Anxiety Depression |
Conflict of information Discrepancies regarding proportionality of treatment Loss of desire to remain alive or hasten death Wish for euthanasia |
Absence of carer Carer limitations due to physical health Carer limitations due to work obligations Another person in family requiring care Carer overload Conflict within family |
Karnofsky Performance scale Edmonton Classification System for Cancer Pain (ECS-CP) |
Three levels – Low Complexity, for general PC – Medium Complexity, for specialised PC – High complexity. for specialised PC |
|
PC: Tool – palliative care; Sx: Symptoms; Mx: Management.
The Hexagon Model of Complexity (HexCom)
HexCom is a Spanish model that aims to define situations according to differing levels of patient complexity. It proposed a three-tiered classification to distinguish between patients with specialist (moderate or high complexity) or general PC needs (low complexity). It consists of 18 items, each item graded as high, moderate, or low complexity, or not assessed. Complexity level is determined on the highest level of complexity on any of the items. These items address all four domains of complexity. It is a paper-based instrument to be used by clinical staff, and also incorporate a section to identify the strengths and resources of the patient. This system has been applied in community populations.
Patient Classification System (Perroca Scale)
The Perroca Scale was developed in Brazil and has been widely used in various hospital settings. It aims to classify patients according to complexity, in order to optimise resources and anticipate care needs. There have been a number of iterations of the Perroca scale, employing between ten to thirteen items. Each item is graded from 1 to 5, which are added together to form a final score corresponding to the care needs of the patient: minimal, intermediate, semi-intensive and intensive care. Dos Santos et al utilised the thirteen-item scale in an inpatient palliative care unit, the clinical staff filling out the scale electronically on admission. The items focus on the personal and health care domains of complexity. This classification system had not been developed specifically for palliative care populations and has not been validated in these cohorts.
The Australian National Subacute and non-acute patient classification (AN-SNAP)
AN-SNAP is an Australian casemix classification, that aims reflect health service use and costs for subacute and non-acute patients. It has a specific classification system for palliative care; both inpatient and community. The initial items and classification were developed by the clinicians and researchers, and detailed clinical and service utilisation, to stratify casemix according to resource use. There have been four iterations of the AN-SNAP, with the included studies describing version 1 and 2, including 8462 episodes of patient care from Australia and New Zealand. The system classifies patients according to 11 scales for inpatient and 22 for community patients. The classification consists of nine items including the phase of illness and the use of assessment tools: the RUG-ADL and the Palliative Care Problem Severity Score (PCPSS) (REFS). These items are focused on the personal domain, with one item of the PCPSS assessing the social domain.
Hui Major Criteria
The Hui Major Criteria was created to establish classification for patients with complex care needs, who would benefit from specialist palliative care referral. It was developed in the USA through Delphi method, incorporating the input of 60 international experts in PC and oncology to establish consensus criteria. It is developed specifically for oncology patients. The major criteria consist of 11 items, the presence of any of these items suggesting the need for specialist palliative care. These items covered only the personal and health care domains. In addition, this process also developed 36 minor criteria for specialist palliative care referral, yet these items were not clear in how they could be applied to patient classification.
IDC-Pal
The IDC-Pal was designed in Spain in order to diagnose and stratify patient complexity, thus recommending need for specialist PC. It was developed through literature review identifying clinical situations that were perceived as complex and graded according to degree of complexity by an expert group. The system has been validated for content, reliability and feasibility and translated to English and German. The system classifies patient complexity according to three levels: non-complex, for general PC; complex, with a potential role for specialist PC; and, high complexity, for whom specialist PC is recommended. It consists of 36 items, addressing each of the four domains. Each item is graded as high, complex or non-complex, with overall patient complexity determined on the highest score on any one item.
PALCOM
The PALCOM was developed in Spain with the objective of assessing complexity in PC, in identify those with increased needs for whom referral to specialised PC services is indicated. It was developed through a prospective observation cohort study of 324 advanced cancer patients, collecting data demographic, clinical, symptom, functional, social and health care team data. Logistic regression was used to identify variable influencing determination of level of PC complexity based on clinician assessment. It is comprised of 24 items, including the Karnofsky functional scale and the Edmonton Classification System for Cancer Pain (ECS-CP); covering personal, social and health team domains. The article proposes two models – PALCOM 1 and 2 – both with high predictive value, though the second model requires further calculations, making it more challenging to apply clinically. A final complexity score derived from a cumulative score from the 24 items classifies the patient situation to be high, medium or low complexity. The article concluded those patients classified as medium complexity should be referred to specialist PC, and high complexity patients needing intensive specialised PC.
Domains covered by classification systems
The classification systems described were heterogeneous in their approach to covering the different domains of complexity, described in Table 2. The focus of the majority of classification systems was on the personal domain. The HexCom and the Pal-IDC contained items that covered all four domains of complexity. Of these, the HexCom contained 18 items, with at least four items in each domain, however, did not include any functional assessments in the personal domain. Pal-IDC contained 36 items, with at least two items in each domain, and was focused on personal history and symptom issues. The determination of overall complexity was dependant on each system, with some systems using cumulative scores and others based upon the highest level of complexity on a single item. Thus, it is not possible to contrast the weighting of these domains in determining overall level of patient care needs.
Discussion
Main findings
This review identified six classification systems to determine complexity of patient care needs in palliative care populations. These systems determined these classifications through assessing many elements of care: symptom burden, illness history, functional ability, social and carer supports, resources, relationships, communication and the care environment. The HexCom and Pal-IDC systems assess complexity across the personal, social, health care and environment domains; thus, may be well-suited to determining complexity on an individual level. The AN-SNAP system has been applied to differing populations over an extended period and may be appropriate for population level classification.
The clinical application of these classification systems remains limited. The exception is the AN-SNAP system has been used extensively in clinical practice for the past two decades. It has been applied to multiple cohorts of patients in New Zealand and Australia, and the classification structure has been revaluated throughout this period four times.8,20–22 The included articles reference the first two version of AN-SNAP in which the palliative care classification structure is unchanged. The HexCom and IDC-Pal systems have also been applied in other populations, although the articles describing this were published in languages other than English, thus not included.24–27 The application of the Hui major criteria in clinical populations has not been reported in the literature. The Perocca scale has been widely applied in hospital settings, and the included study is the only described use in palliative care.18 There are a number of items in this system that may be of differing relevance in palliative populations, such as frequency of observations, use of intravenous therapies and oxygenation.
Validation of these classification systems varies. The AN-SNAP system has been externally validated in multiple populations. The HexCOM, IDC-Pal, and PALCOM models are all reported to have undergone content and construct validation, though these are mostly reported in articles in languages other than English.24,26,28–30 External validation of these systems has not been reported in English. The Perroca system has been validated in acute hospital settings, but not in palliative care populations.31
There is no standard manner to determine complexity, which is reflected in these articles. Complexity of care needs is primarily a phenomenon defined through clinical reasoning. The majority of systems, other than AN-SNAP and Perroca, described using clinician reasoning as the basis for determining patient complexity to which their system is compared. The basis for determining level of patient care needs in AN-SNAP was measured through health care and practitioner resource usage.20,21 None of the systems describe incorporating patient or consumer perspectives of complexity into this determination. This may be an explanation for these systems being largely focused on the patient domain of complexity, reflecting biomedical frameworks for interpreting complexity as a medical issue, rather that influenced by a broader array of factors. Incorporating patient and carer perceptions of complexity may provide a more complete understanding of care needs and requirements, particularly those in the social and environmental domains.
This review identified a number of systems that were relevant to complexity in palliative care but did not fit the inclusion criteria. Specifically, these included INTERMED, a measure of biopsychosocial case complexity in stable cohorts of patients with multiple sclerosis.32 Hong et al.33’s work developing a prediction model of complexity was developed for general practice populations, and has not been applied to populations with known palliative care needs. There were other tools that were developed to identify patient care needs, but did not classify case complexity: including, the three-levels-of-need questionnaire, the holistic common assessment, the Omaha system and the healthcare task difficulty assessment.34–37 Additionally, it should be noted that there are complexity classification systems in development, identified through two protocols.38,39
These classification systems represent a small number of developed countries. The lack of articles from developing settings is particularly relevant given the applicability of complexity classifications in optimising resource utilisation. The classification systems identified in this article of likely to be of differing relevance in developing countries. Determinations of complexity and influences on care needs may differ between care systems. For this reason, it is of utmost importance that complexity classifications address the broad influences that contribute to each individual’s care needs; as issues of access to health provision, medications, financial support and health professional training are likely to be of increasing importance in developing settings.
Strengths and limitations
This review presents the first systematic description of complexity classification systems in palliative care. A broad and iterative search strategy was applied to identify potential studies, incorporating classification systems that predate the recent emergence of the concept of complexity in palliative care research.
There are a number of limitations to this study. Firstly, complexity is a concept that is not well-defined in the scientific literature, and articles representing this concept do not fit within particular MeSH headings. This was identified in the initial exploratory phase of the review, with concepts and keywords referred to those initial articles being quite disparate. As a result, we employed the PALETTE method as a robust literature search method to iteratively construct the search strategy, to enable identification of the majority of articles related to this concept. We also referenced searched all included articles and abstracts. The relatively small number of classification systems identified in our literature review is in line with our initial expectations.
The theoretical approach of this paper was developed upon a complex adaptive systems framework, as it enables palliative care provision to be appreciated as part of a complex system, and each system is different dependant on the many patient, health practitioner, systemic, care network and environmental factors. The strength of this approach was an analysis that highlighted these broad influences on patient care and measures that may address these impacts. However, this limited the study to a descriptive rather than comparative approach, as these classification systems have differing aims and were developed in response to their own local factors.
The inclusion criteria limited articles to those in English and that were peer-reviewed full articles. There were a number of identified articles in languages other than English (Spanish, Portuguese and German) and conference abstracts that described complexity classification systems.24–27,40 All the systems referenced in these articles and abstracts were the subject of other articles in English that were included in the nine articles included in the analysis. We believe this inclusion criteria were justified; as these excluded studies did not present new systems; included numerous other languages; and for the conference abstracts, would not be possible to properly perform quality assessment.
What this study adds
This review describes six differing classification systems for complexity, which use different frameworks for interpreting patient complexity and have varying outcomes for use of that classification. Many factors influence the nature of patients’ situations and the extent of care needs, and it is important a broad range of these factors are taken into account when classifying patient complexity. Incorporating patient and carer perspectives of determining factors of complexity may enrich these classification systems, and highlight important contrasts to the manner in which health practitioner determine complexity. The application of complexity classifications remains limited, and it is not known how such classifications impacts of patient care and health service utilisation. Apart from the AN-SNAP, these systems have not been applied to other settings, and further research would ideally address their broader utility, particularly in resource limited environments.
Assessing and classifying the complexity of patient needs can improve care in multiple ways. The process of assessing complexity is intrinsically valuable, promoting an understanding of the many factors that influence the patient’s situation and care needs. This may engage discussion with patient and family regarding current challenges, preferences and future care needs; stimulating shared decision making and focusing consultation on the patient’s needs and wishes. From a public health perspective that classification of complexity enables systematic care planning: to provide the right care and systems of care for each individual patient.2,6 Health systems operate with finite resources, and thus identifying patients with complex needs allows these resources to be allocated where they will be of most clinical benefit. Primary and general health services are well placed to provide high quality palliative care, and through a systematic approach to identifying the individual’s specific care needs can these services be optimally and appropriately engaged.3 Patient complexity has potential to detail health service casemix on a population level; to better manage staff caseloads, assess likely resources implications, classify patient cohort according to care needs, and assist with coordination with other services.
A key challenge for any classification system is the clinical applicability; their ease of use, integration and impact on clinical practice. The classification systems ranged from 9 to 36 items; including items that are routinely collected in clinical practice and those that require specific questioning. The AN-SNAP classification is unique in this manner, that routine collection of these items has become integrated into inpatient and community care. The remaining systems require specific questioning on items, however, cover meaningful domains of care needs. None of the classification systems appeared to be overly burdensome on clinical staff, with the majority of items likely to be addressed through the routine clinical consultation. The impact of these classification systems on clinical care is not addressed by these articles. Further research is required to identify these outcomes; as to whether classification of patient complexity enables greater consistency in anticipatory care planning, resource allocation, appropriate service provision, and its impacts on quality of care in clinical practice.
Conclusions
Complexity remains as emerging concept, and future research is needed to properly operationalise how it is applied to clinical care. There is no standardised definition to complexity, nor international guidance as to how it might be assessed. This review provides a systematic description of these classification systems, and the domains and aspects of care they assess, which vary quite considerably. It is unknown how these systems might be applied in foreign settings, where the circumstances of patients and care provision may be subject to many differing influences. Finally, clinical application of complexity classification is limited, with research needed to assess outcomes of classifying patients according to levels of complexity, in particular its effects on service provision and resource usage.
The identification and classification of patients with complex needs has the potential to facilitate patient-centred discussions, improve multidimensional clinical care and health service planning. This systematic review describes six systems that classify patients in accordance with their care needs. Applying these systems, or the aspects of care they identify, to clinical care, may assist in anticipatory planning for health care professionals. In particular, as specialist palliative care services such as high care hospices are faced with resource challenges, it may identify those patients for whom general palliative services are appropriate.
Appendix 1
Search strategy for Pubmed (Ovid)
(exp Terminal Care/ OR bereave$.af. OR hospice$.mp. OR advanced cancer.tw. OR end of life.af. OR terminally ill.mp. OR palliative$.tw. OR Palliative Care/ OR exp palliative therapy/) AND (complexity/ OR casemix/ OR complex needs/ OR classification.ti)
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was funded through ZonMW project number: 844001406.
ORCID iD: Matthew Grant  https://orcid.org/0000-0002-6878-9197
https://orcid.org/0000-0002-6878-9197
References
- 1. Pype P, Mertens F, Helewaut F, et al. Healthcare teams as complex adaptive systems: understanding team behaviour through team members’ perception of interpersonal interaction. BMC Health Serv Res 2018; 18(1): 570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pask S, Pinto C, Bristowe K, et al. A framework for complexity in palliative care: a qualitative study with patients, family carers and professionals. Palliat Med. 2018; 32(6): 1078–1090. [DOI] [PubMed] [Google Scholar]
- 3. Mitchell GK, Senior HE, Johnson CE, et al. Systematic review of general practice end-of-life symptom control. BMJ Support Palliat Care 2018; 8(4): 411–420. [DOI] [PubMed] [Google Scholar]
- 4. Dixon J, King D, Matosevic T, et al. Equity in the provision of palliative care in the UK: review of evidence. 2015. [Google Scholar]
- 5. Mitchell H, Noble S, Finlay I, et al. Defining the palliative care patient: its challenges and implications for service delivery. BMJ Support Palliat Care 2013; 3(1): 46–52. [DOI] [PubMed] [Google Scholar]
- 6. Hodiamont F, Junger S, Leidl R, et al. Understanding complexity – the palliative care situation as a complex adaptive system. BMC Health Serv Res 2019; 19(1): 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tuca A, Gómez-Martínez M, Prat A. Predictive model of complexity in early palliative care: a cohort of advanced cancer patients (PALCOM study). Support Care Cancer 2018; 26(1): 241–249. [DOI] [PubMed] [Google Scholar]
- 8. Eagar K, Gordon R, Green J, et al. An Australian casemix classification for palliative care: lessons and policy implications of a national study. Palliat Med 2004; 18(3): 227–233. [DOI] [PubMed] [Google Scholar]
- 9. Higginson IJ, Hart S, Koffman J, et al. Needs assessments in palliative care: an appraisal of definitions and approaches used. J Pain Symptom Manage 2007; 33(5): 500–505. [DOI] [PubMed] [Google Scholar]
- 10. Zwakman M, Verberne LM, Kars MC, et al. Introducing PALETTE: an iterative method for conducting a literature search for a review in palliative care. BMC Palliat Care 2018; 17(1): 82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews, https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf (2006).
- 12. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;151(4): 264–269. [DOI] [PubMed] [Google Scholar]
- 13. Rietjens JA, Bramer WM, Geijteman EC, et al. Development and validation of search filters to find articles on palliative care in bibliographic databases. Palliat Med 2019; 33(4): 470–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile app for systematic reviews. Systemat Rev 2016; 5(1): 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. In: Joanna Briggs Institute reviewer’s manual. 2017:2019-05. [Google Scholar]
- 16. Banno M, Tsujimoto Y, Kataoka YJBo. Reporting quality of the Delphi technique in reporting guidelines: a protocol for a systematic analysis of the EQUATOR Network Library. BMJ Open 2019; 9(4): e024942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Busquet-Duran X, Jiménez-Zafra EM, Manresa-Domínguez JM, et al. Describing complexity in palliative home care through HexCom: a cross-sectional, multicenter study. J Multidiscip Healthc 2020; 13: 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. dos Santos CE, Klug D, Campos L, et al. Analysis of the Perroca scale in palliative care unit. Rev Esc Enferm USP 2018; 52: e03305. [DOI] [PubMed] [Google Scholar]
- 19. Martin-Rosello ML, Sanz-Amores MR, Salvador-Comino MR. Instruments to evaluate complexity in end-of-life care. Curr Opin Support Palliat Care 2018; 12(4): 480–488. [DOI] [PubMed] [Google Scholar]
- 20. Eagar K, Cromwell D, Kennedy C, et al. Classifying sub-acute and non-acute patients: results of the New South Wales Casemix Area Network study. Aust Health Rev 1997; 20(2): 26–42. [DOI] [PubMed] [Google Scholar]
- 21. Eagar K, Green J, Gordon R. An Australian casemix classification for palliative care: technical development and results. Palliat Med 2004; 18(3): 217–226. [DOI] [PubMed] [Google Scholar]
- 22. Green J, Gordon R. The development of Version 2 of the AN-SNAP casemix classification system. Aust Health Rev 2007; 31(Suppl 1): S68–S78. [DOI] [PubMed] [Google Scholar]
- 23. Hui D, Mori M, Watanabe SM, et al. Referral criteria for outpatient specialty palliative cancer care: an international consensus. Lancet Oncol 2016; 17(12): e552–e559. [DOI] [PubMed] [Google Scholar]
- 24. Comino MRS, Garcia V, Lopez M, et al. Assessment of IDC-pal as a diagnostic tool for family physicians to identify patients with complex palliative care needs in Germany: a pilot study. Gesundheitswesen 2018; 80(10): 871–877. [DOI] [PubMed] [Google Scholar]
- 25. de Miguel C, Ruiz S, de la Uz A, et al. Are the patients attended by home care support teams complex? Medicina Paliativa 2018; 25(1): 7–16. [Google Scholar]
- 26. Esteban-Perez M, Fernandez-Ballart J, Boira Senli RM, et al. Agreement between the complexities observed from different levels of care in complex chronic patients, with advanced disease or at the end of life through a model of complexity approach. Medicina Paliativa 2018; 25(4): 236–244. [Google Scholar]
- 27. Esteban-Pérez M, Grau IC, Trilla GC, et al. Complejidad asistencial en la atención al final de la vida: criterios y nivelesde intervención en atención comunitaria de salud. Medicina Paliativa 2015; 22(2): 69–80. [Google Scholar]
- 28. Comino MRS, Beck T, Amzat R, et al. Validation of the diagnostic tool for complexity in palliative care—pilot study (S727). J Pain Symptom Manage 2018; 55(2): 670–671. [Google Scholar]
- 29. Martin-Rosello ML, Fernandez-Lopez MA, Vidal-Espana F, et al. Development of a method of diagnosing complexity in palliative care. (in Spanish: IDC-Pal: instrumento diagnostico de la complejidad en cuidados paliativos). Palliat Med 2014; 28(6): 761–762. [Google Scholar]
- 30. Esteban-Pérez M, Fernández-Ballart J, Senlí RMB, et al. Concordancia entre la complejidad observada desde diferentes niveles asistenciales en pacientes crónicos complejos, con enfermedad avanzada o al final de la vida mediante un modelo de abordaje de la complejidad. Medicina Paliativa 2018; 25(4): 236–244. [Google Scholar]
- 31. Cucolo DF, Perroca MGJRl-ade. Assessment of the nursing care product (APROCENF): a reliability and construct validity study. Rev Latino Am Enfermagem 2017; 25: e2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. de Jonge P, Hoogervorst EL, Huyse FJ, et al. INTERMED: a measure of biopsychosocial case complexity: one year stability in multiple sclerosis patients. Gen Hosp Psychiatry 2004; 26(2): 147–152. [DOI] [PubMed] [Google Scholar]
- 33. Hong CS, Atlas SJ, Ashburner JM, et al. Evaluating a model to predict primary care physician-defined complexity in a large academic primary care practice-based research network. J Gen Int Med 2015; 30(12): 1741–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. NHS National End of Life Care Programme. Holistic common assessment of supportive and palliative care needs for adults requiring end of life care. NHS National End of Life Care Programme, 2010. [Google Scholar]
- 35. Boyd CM, Wolff JL, Giovannetti E, et al. Healthcare task difficulty among older adults with multimorbidity. Med Care 2014; 52(3, Suppl 2): S118–S125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lazerowich V. Development of a patient classification system for a home-based hospice program. J Commun Health Nurs 1995; 12(2): 121–126. [DOI] [PubMed] [Google Scholar]
- 37. Johnsen AT, Petersen MA, Pedersen L, et al. Development and initial validation of the three-levels-of-needs questionnaire for self-assessment of palliative needs in patients with cancer. J Pain Symptom Manage 2011; 41(6): 1025–1039. [DOI] [PubMed] [Google Scholar]
- 38. Guo P, Dzingina M, Firth AM, et al. Development and validation of a casemix classification to predict costs of specialist palliative care provision across inpatient hospice, hospital and community settings in the UK: A study protocol. BMJ Open 2018; 8(3):e020071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Iglesias FH, Celada CA, Navarro CB, et al. Complex care needs in multiple chronic conditions: population prevalence and characterization in primary care. a study protocol. Int J Intergr Care 2018; 18(2): 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Santos CEd, Klug D, Campos L, et al. Análise da Escala de Perroca em unidade de cuidados paliativos. Rev Esc Enferm 2018; 52: e03305. [DOI] [PubMed] [Google Scholar]