Abstract
The COVID-19 pandemic has hit the electroconvulsive therapy (ECT) services hard worldwide as it is considered an elective procedure and hence has been given less importance. Other reasons include the risk of transmission of infections, lack of resources, and the scarcity of anesthesiologists due to their diversion to intensive care units to manage COVID-19 patients. However, ECT is an urgent and life-saving measure for patients diagnosed with depression and other severe mental illnesses who have suicidality, catatonia, or require a rapid therapeutic response. COVID-19 pandemic is a significant source of stress for individuals due to its impact on health, employment, and social support resulting in new-onset psychiatric illnesses and the worsening of a pre-existing disorder. Hence, a continuation of the ECT services during the COVID-19 pandemic is of paramount importance. In this narrative review, the authors from India have compiled the literature on the ECT practice during the COVID-19 pandemic related to the screening and testing protocol, necessity of personal protective equipment, modification in ECT Suite, electrical stmulus settings, and anesthesia technique modification. The authors have also shared their experiences with the ECT services provided at their institute during this pandemic. This description will help other institutes to manage the ECT services uninterruptedly and make ECT a safe procedure during the current pandemic.
Keywords: COVID-19, ECT practice, Anesthesia, Personal protective equipment
1. Importance of continuing ECT during COVID-19 pandemic
Electroconvulsive therapy (ECT) remains an urgent and life-saving measure for specific indications like depression and other severe mental illnesses with significant suicidality, catatonia, or requiring rapid therapeutic response (Kellner et al., 2020; Mankad et al., 2010). Besides, ECT forms an essential management strategy in treatment-resistant mood and psychotic disorders when conventional pharmacological approaches have failed (Baghai and Möller, 2008; Kellner et al., 2020). Many such patients are continued on maintenance ECT to prevent relapse or recurrence of their psychiatric illnesses (Petrides et al., 2011). Hence, ECT qualifies as an essential service, the availability of which is paramount during the ongoing SARS-CoV-2 (commonly referred to as COVID19) pandemic (Espinoza et al., 2020).
The Covid-19 pandemic is in itself a significant source of stress for individuals due to its impact on health, employment, social support, and for some, even necessities like food and shelter (Das, 2020). New-onset psychiatric illnesses and the worsening of pre-existing disorders have emerged in this background (Andrade, 2020; Rajkumar, 2020). Unfortunately, the ensuing lockdown during the COVID19 outbreak led to restrictions in people's movement and difficulty accessing ECT services in India (Grover et al., 2020) and across the globe (Amad et al., 2020; Sienaert et al., 2020; Tor et al., 2020a, b). Many centers worldwide also stopped ECT services with the pandemic's onset due to fear of causing the spread of COVID-19. Another major obstacle in providing ECT services was the shortage of anesthesiologists secondary to their deputation to intensive care units to treat sick patients who have tested positive for COVID (Espinoza et al., 2020; Gil-Badenes et al., 2020). Due to the limited availability of ECT services, worsening of pre-existing psychiatric illnesses, including suicides, was recorded (Vindegaard and Benros, 2020; Tor et al., 2020a, b).
2. Concerns in providing ECT during COVID-19 pandemic
The SARS-CoV-2 virus causes COVID-19 infection. The virus spreads from an infected person to others who are in close contact through aerosols and respiratory droplets generated during coughing, sneezing, and talking and through fomites. The transmission occurs when people do not maintain social distancing, do not wear masks, and do not regularly clean their hands. Patients with psychiatric illnesses may not adhere to the guidelines to prevent disease spread because of their mental status.
Based on an initial negative clinical screen, the administration of ECT does not rule out the risk of transmission from asymptomatic patients (Tong et al., 2020). Patients with initial negative reverse transcriptase-polymerase chain reaction (RT-PCR) test can still spread the infection as the test's sensitivity is only around 60–70 % (Tahamtan and Ardebili, 2020). Also, patients with initial negative RT-PCR might still get infected during the ECT course and hospital stay (Boland and Dratcu, 2020). The risk further increases with an increasing number of patients requiring ECT each day, multiple ECT sessions for a given patient, and both inpatient-based and outpatient-based ECTs occurring in the same ECT area on the same day, when outpatients carry a higher risk of exposure from the community.
The ECT requires sizeable hospital resources in-terms of COVID-19 tests and consumables like personal protective equipment (PPE), airway devices, and human resources.
During ECT, psychiatrists and anesthesiologists are in close proximity with the patients, and their relatives during the pre-procedure assessment, physical examination, anesthesia administration, and post-procedure care. The ECT under anesthesia is an aerosol-generating procedure with the associated risk of infection transmission to the health care workers (HCWs), supporting staff, and fellow patients (Tran et al., 2012; Anelli et al., 2020; Purushothaman et al., 2020). The time points with high vulnerability are listed below -
-
1)
Pre-anesthetic consultation (PAC): Doctors come close to the patients for clinical examination (physical distancing is difficult)
-
2)
Administration of anesthesia: During bag and mask ventilation (BMV) and airway instrumentations (Guedal airway, laryngeal mask airway, endotracheal intubation), there is a high risk of aerosol generation
-
3)
Recovery from anesthesia: Suctioning of oral secretions, airway handling (ex: jaw thrust), and instrumentation in case of airway obstruction and coughing during recovery from anesthesia generate aerosols and contaminate the ECT suite.
-
4)
Prolonged airway care: In situations like arterial desaturation, prolonged apnea, and bronchospasm, airway interventions are required, and the anesthesiologist needs to spend more time with the patients nearby. Such scenarios are more common in obese and elderly patients with associated comorbidities.
-
5)
In a rare situation, if a patient sustains cardiac arrest requiring cardiopulmonary resuscitation (CPR).
-
6)
Handling of equipment like breathing circuits, face mask, anesthesia machine, and vital sign monitors between cases can contaminate these equipment. These can act as fomites and transmit infection among HCWs while checking the equipment and during cleaning.
Considering the risk of transmission of infection during ECT in the COVID-19 pandemic, an appropriate modification to the ECT techniques, particularly in anesthesia technique, is needed to minimize the aerosolization and transmission risks among the ECT team members and to other patients. It is essential to make ECT a safe procedure without interrupting the services to the non-COVID-19 and COVID-19 affected psychiatric patients.
3. Review of recommendations/suggestions for ECT across the world during COVID-19 pandemic
Keeping in mind the importance of providing uninterrupted ECT services to the needy people, clinical experts and professional bodies introduced operating protocols to administer ECT, ensuring the safety of both the patients and the HCWs. Though, these protocols across different countries appeared similar, differences did exist. The contributing factors for these differences include the pandemic stage, the phase of lockdown, the state/ national healthcare policy for COVID-19, and the availability of resources (testing and protective equipment). In this narrative review, information on ECT practice experience from centers across the world was collated from the published literature and from the guidelines prescribed by professional societies. A search was made on the online platform (Google Scholar, Pubmed, Ebsco) using the keyword combinations, ‘Electroconvulsive therapy’, ‘Covid pandemic’, ‘airway management’, ‘protective equipments’, and 'ventilation’. The published literature was mainly in the form of clinical experts opinion, society recommendations based on pathophysiology and good clinical practices, case reports and case series.
3.1. Baseline screening and testing protocols
Screening includes a recent history of travel, exposure to suspected or diagnosed cases, and the presence of Covid-19 symptoms requiring Covid-19 RT-PCR testing from nasopharyngeal swab (Burhan et al., 2020; Gil-Badenes et al., 2020; Lapid et al., 2020; Schumann et al., 2020). A few recommend baseline RT-PCR testing for all patients 1–2 days before the first ECT (Bryson and Aloysi, 2020; Flexman et al., 2020; Sienaert et al., 2020). Most groups advised avoiding ECT in Covid-19 positive cases for the first two weeks unless it is urgent and life-saving due to the risk of infection spread (Flexman et al., 2020; Gil-Badenes et al., 2020; Lapid et al., 2020; Ramakrishnan et al., 2020). Conversely, COVID-19 positive patients have received ECT successfully in tertiary care hospitals without the above restrictions (Sienaert et al., 2020), even during the symptomatic phase of COVID-19 infection (Braithwaite et al., 2020). Furthermore, many added information regarding the possible risks of contracting COVID-19 disease to the informed consent (Burhan et al., 2020; Lapid et al., 2020). During ECT, it is recommended to monitor the patients daily for fever and respiratory symptoms. Repeated swab testing is not advised routinely unless the patient develops symptoms. However, some have recommended weekly RT-PCR testing for all patients irrespective of the symptoms (Gil-Badenes et al., 2020; Sienaert et al., 2020).
3.2. Use of personal protective equipment (PPE)
All ECT centers worldwide have adopted the policy of universal safety precautions for administration of ECT during COVID-19 due to possible false-negative test results and asymptomatic carriers. Recommendations for full PPE include N95/ FFP2 (or higher) masks, face-shields, eye goggles, fluid-resistant long-sleeved gowns, and double gloves for all members who are actively involved in ECT administration (Bellini et al., 2020; Bryson and Aloysi, 2020; Burhan et al., 2020; Chevance et al., 2020; Colbert et al., 2020; Flexman et al., 2020; Gil-Badenes et al., 2020; Lapid et al., 2020; Schumann et al., 2020; Sienaert et al., 2020; Tor et al., 2020a, b; Purushothaman et al., 2020). The housekeeping staff involved in disinfection of the ECT room should wear at least N95/ FFP2 (or higher) face masks and gloves and limit their exposure to the bare minimum (Lapid et al., 2020). Most experts advise that the team's active members can use the same PPE (excluding outer gloves) for the entire day's sessions.
3.3. Modification in ECT administration area and Recovery area
Most publications advise updating the ECT administration area to an airborne infection isolation room (AIIR) to retain the infective droplets (Bryson and Aloysi, 2020; Burhan et al., 2020; Flexman et al., 2020; Schumann et al., 2020). Other alternatives include shutting doors and windows during ECT and opening them for 15 min once the patient has been shifted to the recovery room (Gil-Badenes et al., 2020) or using two rooms alternately (Lapid et al., 2020).
For recovery rooms, recommendations include having a limited number of beds with adequate distancing (up to 6 feet) and using physical barriers such as curtains between beds (Gil-Badenes et al., 2020; Lapid et al., 2020). The ECT room, along with the equipment, should be disinfected by the team members after every case (Burhan et al., 2020; Chevance et al., 2020; Sienaert et al., 2020). In case the patients are called batch-wise, the room can be decontaminated between separate batches (Tor et al., 2020a, b). At the end of each day's sessions, terminal disinfection is advised (Lapid et al., 2020).
3.4. Modification in the ECT requirement criteria and the electric current settings
During the ongoing Covid-19 pandemic, ECT should be restricted to urgent and life-saving cases (Burhan et al., 2020; Lapid et al., 2020; Tor et al., 2020a, b). Similarly, the decision to maintain/ space/stop ECT is to be taken after accounting for the potential risks and benefits in the current pandemic situation (Bryson and Aloysi, 2020; Sienaert et al., 2020). Tor et al., have recommended a model of ethical triaging of patients for ECT based on the principles of beneficence, non-maleficence, autonomy, and justice. Many centers limited the number of patients per day to three to six (Bryson and Aloysi, 2020; Gil-Badenes et al., 2020). The frequency of sessions for an individual patient is also kept at two per week (Bellini et al., 2020; Gil-Badenes et al., 2020; Tor et al., 2020a, b). Age-based determination of seizure threshold is suggested to reduce the number of ECT sessions (Lapid et al., 2020).
3.5. Modifications in the anesthesia techniques for ECT
Society for Neurosciences in Anaesthesiology and Critical Care (SNACC), in its guidelines on anesthesia practice for ECT during COVID-19 pandemic, as well as a few other experts have advised to pre-medicate patients with anticholinergics (intravenous glycopyrrolate or atropine) to reduce salivation, and to minimize the risk of aerosol generation (Flexman et al., 2020; Gil-Badenes et al., 2020; Lapid et al., 2020; Schumann et al., 2020; Sienaert et al., 2020).
Due to aerosol risks, instead of hyperventilating patients with BMV to provoke seizures, induction agents like ketamine, etomidate, or methohexitone have been recommended by the SNACC society, as these medications reduce the seizure threshold. (Flexman et al., 2020).
There is a controversy regarding the dose of muscle relaxant. A lesser quantity reduces the apneic time and subsequent BMV, while a more liberal dose ensures complete muscle relaxation (Bellini et al., 2020; Thiruvenkatarajan et al., 2020a, b).
A variety of suggestions/recommendations have been published on oxygen administration techniques during induction and the apneic period. To reduce aerosolization during oxygen administration, face masks/nasal cannula is to be placed beneath the surgical mask (Flexman et al., 2020; Schumann et al., Gil-Badenes et al., 2020; Thiruvenkatarajan et al., 2020a, b). Apneic ventilation with BMV is a source of aerosolization (Tran et al., 2012). To avoid BMV, some centers adopt a more extended period of preoxygenation and/or self-hyperventilation, or use head straps for holding the mask and avoiding BMV completely (Bellini et al., 2020; Flexman et al., 2020; Lapid et al., 2020; Sienaert et al., 2020; Gil-Badenes et al., 2020)) and restrict BMV to cases with desaturation (Luccarelli et al., 2020). Others recommend to continue using low tidal volume BMV along with preoxygenation, provided a high-quality mask seal is achieved (Bryson and Aloysi, 2020; Schumann et al., 2020; Tor et al., 2020a, b; Gil-Badenes et al., 2020.). Alternatively, apneic oxygenation using nasal prongs or laryngeal mask airway has also been suggested (Flexman et al., 2020; Thiruvenkatarajan et al., 2020a, b). High flow oxygen therapy using a nasal cannula is considered as an alternative to standard oxygen therapy. The risk of aerosolization remains similar in both techniques, and it may avoid the need for invasive airway management/ BMV (Thiruvenkatarajan et al., 2020a, b, Li et al., 2020). Few centers prefer placing an endotracheal tube (ETT) for airway management (Braithwaite et al., 2020). Though ETT and LMA can provide better oropharyngeal/airway seal, maintain closed-loop ventilation, prevent the need of BMV and allow the anesthesiologist to maintain a safe distance from the patient, higher incidence of cough during recovery and subsequent aerosolisation negates the benefits. There is also a concern about increased anesthesia time. For these reasons, routine use of ETT and LMA has been advised against by few experts (Limoncelli et al., 2020). However, if an airway needs to be secured, LMA is preferred over an ETT as it is less invasive.
Concerning the breathing circuit, a closed circuit is ideal for preventing environmental contamination, though the use of Mapleson-C and Jackson-Rees circuits have also been suggested (Intensive care medicine and Anaesthesia societies UK, 2020; Limoncelli et al., 2020).
A high-efficiency particulate air (HEPA) filter between the reservoir bag - anesthesia circuit and between mask – anesthesia circuit is advised to prevent contamination of the breathing circuit (Schumann et al., 2020; Luccarelli et al., 2020; Limoncelli et al., 2020; Gil-Badenes et al., 2020) and the surrounding. Filters may be disposed of after each session (Bryson and Aloysi, 2020; Tor et al., 2020a, b) or maybe stored and reused for the same patient, based on the affordability and availability (Lapid et al., 2020).
Physical barrier enclosures such as disposable plastic covers over the patient or specially designed aerosol boxes (Ramakrishnan et al., 2020; Schumann et al., 2020; Gil-Badenes et al., 2020; Brown et al., 2020) placed over the patient's head to limit aerosol spread during manual ventilation are used in some centers across the world.
If airway suction is unavoidable, then a closed suction system instead of an open system should be preferred (Flexman et al., 2020), or suctioning can be considered before the muscle relaxant effect weans off (Schumann et al., 2020). Some centers prefer antitussive agents like remifentanil and lidocaine to reduce coughing at emergence. (Flexman et al., 2020; Lapid et al., 2020; Schumann et al., 2020).
In a rare cardiac arrest situation in a COVID-19 suspect or confirmed case requiring CPR, it is recommended to initiate chest compression-only CPR (Resuscitation council UK, 2020). Early airway protection, preferably using LMA, should be considered before commencing chest-compression (Resuscitation council UK, 2020; Ott et al., 2020). Chest compression should be stopped while securing the airway, and external compression devices should be preferred for chest compression if available (Tang and Chan, 2020).
In conducting an ECT session during the Covid pandemic, clinicians must take into consideration the country’s infection rate, stage of the pandemic, available resources including manpower, local hospital infection control policy statements and state/country health care policy and guidelines to practice ECT in a safe environment.
4. ECT practice at National Institute of Mental Health and Neuro Sciences (NIMHNAS), Bengaluru, India before and during COVID-19 pandemic
4.1. ECT practice before COVID-19 pandemic
Our institute caters to the psychiatry patients from all over India. On an average, around 25–30 patients receive ECT each day under anesthesia. The ECT is provided at a dedicated location, which has a patient receiving area, holding area, ECT room, and recovery room/ post-anesthesia care unit (PACU) from where patients go back to the respective wards or get discharged if ECT is given on outpatient basis. The various aspects of the ECT administration practiced prior to the COVID-19 pandemic are listed in Table 1 and are compared with the changes adopted during the pandemic in the same table.
Table 1.
Comparison of ECT practices at our institute before and during COVID-19 pandemic.
| ECT practice | Before COVID-19 pandemic | During COVID-19 pandemic |
|---|---|---|
| ECT Facility | Dedicated facility with patient holding area, ECT room, recovery room | ECT facility reorganised into orange/red zones with COVID-19 positive cases treated in red zones and all other patients treated as suspects and treated in orange zone |
| ECT consent form | Consent form for ECT included risk of the procedure and anesthesia | Additional consent added explaining the risk of contracting COVID-19 infection during the therapy and the expected measures to be taken by the patient and family |
| ECT team | 7 HCWs: | 4 HCWs: |
| * Psychiatrists - 2 | * Psychiatrists-1 | |
| * Anesthesiologist - 1 | * Anesthesiologist-1 | |
| * Anesthesia technician - 1 | * Anesthesia technician - 0 | |
| * Nursing officers - 3 | * Nursing officers- 2 | |
|
|
|
| * Housekeeping staffs - 2 | * Housekeeping staffs - 2 | |
| Number of ECT /day | 27−30 | 7−8 |
| Anesthetic technique | ||
| a. Preoxygenation | Using Bain’s circuit with O2 flows at 6−8 L/min | Initial months-preoxygenation with Bain’s circuit with O2 at <6 L/min and since october preoxygenation with closed loop circuit with O2 <5 L/min for 3−5 min |
| b. Induction | Induction agents -thiopentone, Propofol, ketamine and suxamethonium chloride or atracurium. Anti-sialogogue's use restricted to patients manifesting profuse oral secretions during their first ECT session | No change |
| c. Ventilation | BMV post induction of anesthesia, during apnoea peroad till recovery of spontaneous breathing | BMV avoided or restriced to minimum with low tidal volume ventilation |
| d. Post-current administration | Once the patient recovers from anesthesia, the patient is placed in the recovery position for observation, and oral cavity suctioned if required | Oral cavity suctioning is done only if necessary |
| Current stimulus |
|
|
| Patient recovery |
|
|
| Patient movement workflow | Pre-ECT waiting room-ECT room-Recovery room-ward | Screening area - ECT room -directly shifted back to ward or discharged |
| Turn around time | 10min | 30min |
| Cleaning of the ECT room | At the end of the day | In-between the cases and terminal cleaning at the end of the day |
| Additional changes | – |
|
4.2. ECT practice during COVID-19 pandemic
4.2.1. Organization and training of the ECT team
Following the hospital infection control committee's advice, the hospital is divided into three working zones to reduce cross-infection among patients and HCWs and to ensure judicious use of limited resources. The level of barrier precautions varied based on the working zones. The three working zones include - (i) Green (clean) zone: Admitted patients are RT-PCR negative, and infection was ruled out clinically and on high-resolution CT-Thorax (if needed), (ii) Orange zone (suspect) zone: Admitted patients have symptoms, signs suggestive of COVID-19 and awaiting for RT-PCR results, and (iii) Red (confirmed) zone: Admitted patients are RT-PCR/Antigen positive for COVID-19.
Our current ECT receiving area comes under the orange zone where all the treated patients are considered suspects even if they were negative on initial RT-PCR. This is due to the inability to perform RT-PCR tests before every ECT session. There are chances that these patients might acquire the infection from other patients/relatives during their hospital stay. In order to minimize exposure, the ECT team members were reduced to 4 (Table 1). All staff members screen themselves daily and are advised to isolate themselves in case of unprotected exposure to high-risk contacts or development of symptoms and follow the institutional protocol for case management. In such situations, pre-defined substitutes trained in the ECT took over the service.
The confirmed COVID-19 cases requiring ECT receive it in the red zone, a building dedicated to COVID-19 positive cases of the entire hospital, including psychiatric patients requiring ECT. The ECT was administered in the operation theatre (OT), adjacent to the ICU. A separate team managed ECT in the red zone.
4.2.2. Baseline screening and testing protocols
Screening is conducted for both inpatient and outpatient before each ECT session, along with recording the body temperature. Patients who screened positive or are deemed high-risk secondary to the contact with a COVID-19 positive person are isolated and undergo COVID-19 RT-PCR testing from a nasopharyngeal swab. Further ECT treatment was deferred till a negative swab report came. This protocol was continued till June 2020.
With the increase in the number of suspected cases, ECT is not withheld for them. Such patients started receiving ECT treatment at the end of the day in the orange zone to avoid infection spread to other patients. From the 1st week of September 2020, we refined the screening protocol, and COVID-19 RT-PCR testing has been mandatory for all the patients before starting the ECT course. Subsequently, for all outpatients, the COVID-19 rapid antigen test is repeated after 14 days. As inpatients have restricted outdoor activities, the COVID-19 test is not repeated during the ECT course unless they develop COVID-19 related symptoms.
New patients are assessed, and informed consent is taken. Additional consent is sought, explaining the possible risk to the patient of contracting COVID-19 infection, despite taking all the standard precautions during ECT-therapy. Consent form also enumerated the precautionary steps to be followed by the patient and the family in between the ECT sessions.
4.2.3. Use of personal protective equipment (PPE)
All HCWs of the ECT team working in the orange and red zones wear full PPE (Coveralls, shoe covers, N95-99 masks/respirators, surgical cap, triple gloves, goggles, visor). Supporting staff involved in the sanitization wear N95 mask with double gloves and disposable gowns in the orange zone and full PPE In the red zone (World Health Organization (WHO, 2020; MOHFW, India, 2020). It has also been ensured that both patients and their caregivers wear face masks at the ECT suite. These strategies have prevented ECT staff from contracting an infection during the ECT of asymptomatic patients and those whose COVID-19 positivity was known later.
4.2.4. Modification in ECT administration and recovery areas
To prevent cross-infection among the patients, on a given day, first inpatients receive ECT followed by outpatients with negative RT-PCR, and lastly, outpatients without RT-PCR report and who are negative on the clinical screen receive ECT. Seating arrangements at the ECT waiting room are made, ensuring appropriate physical distancing, and the patients are called from one ward at a time in a batch of 2−4. A dedicated battery-driven transport vehicle was arranged to facilitate the patient's quick commute from the wards to the ECT building and the patient was accompanied by only one attendee (Fig. 1 ). Specific areas were identified within the ECT suite for donning and doffing pictorial instructions as per the institute guidelines. All the rooms have adequate ventilation with multiple windows. A single patient is called in at a time for the ECT. On the completion of his / her session, the next patient is called in. One nursing officer helps in the ECT administration, including anesthesia. The other screens the patients at the entry for temperature and room air oxygen saturation and directly take them to the ECT room. After completing the ECT, the same nursing officer escorts the patient out and receives the next patient. The second nursing officer also serves as a standby to assist in the ECT if extra help is required.
Fig. 1.
Patient commuted from ward to ECT facility in a battery-operated vehicle to facilitate a quick commute.
4.2.5. Modifications in deciding the need for ECT and the electric current settings
For outpatient-based ECT, the risk-benefit analysis is done for each session. For maintenance ECTs, the interval between sessions was increased to the extent possible. ECT is stopped altogether in some cases, with a plan to start rescue ECTs if illness relapses. In general, brief-pulse ECT with bilateral (bifrontal or bitemporal) ECTs are preferred to right unilateral ECT to avoid an ineffective session of determining seizure threshold. The titration-based method is only used to determine the seizure threshold, but erring on the higher electrical stimulus. In cases with available details of the past history of ECT, we administer a suprathreshold electrical stimulus from the first session based on the seizure threshold of the previous ECT course. Seizure duration is monitored through a motor component to reduce ECT administration time.
4.2.6. Modification in anesthesia administration for ECT
Changes observed from the usual anesthesia practice are as follows–
-
-
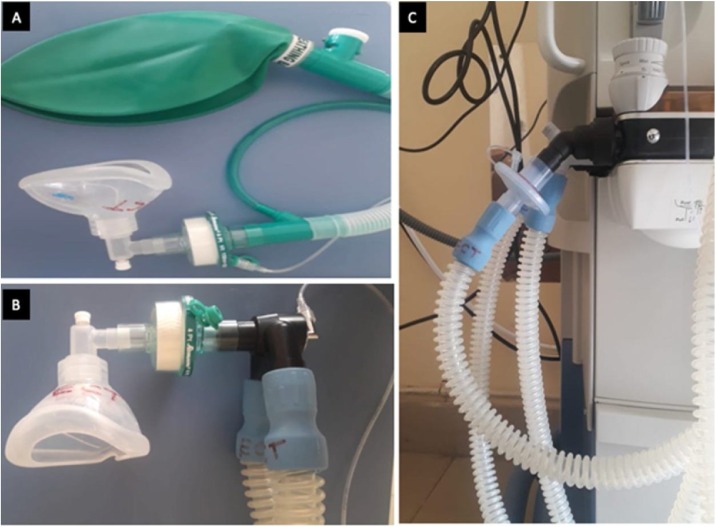
Use of filters between the patient end of the Bain's/closed circuit and the anatomical reusable face mask and between the expiratory limb and anesthesia workstation (Fig. 2 ).
-
-
Restriction of oxygen flows < 6 L/min
-
-
Preoxygenation of all the patients for 3−5 min with 100 % oxygen.
-
-
Apnea ventilation with BMV kept to a minimum, and if required, low tidal volume ventilation is given when peripheral oxygen saturation falls below 92 %.
-
-
Airway manipulations are avoided, and suctioning of the airway at the time of recovery is done when the patient is still under the effect of anesthesia.
-
-
Close distance with the patient is kept to the minimum.
-
-
Patients are allowed to recover completely in the ECT area, followed by a direct shift from the ECT room (without shifting the patient to the recovery room).
-
-
As the ECT room is not a "negative pressure room," all the windows are kept open for ventilation.
-
-
Anesthesia workstation is installed in the orange zone in October 2020 to facilitate low-flow anesthesia, and better maintain a close loop.
Fig. 2.
Heat moisture exchange (HME) filter between the patient end of the Bain's/closed circuit and the anatomical reusable face mask (2A), patient end of the closed circuit and the mask (2B) and between the expiratory limb of the closed circuit and anesthesia workstation (2C).
Modifications practiced at the discretion of the attending anesthesiologists include the following-
-
-
Use of barrier airway techniques like an acrylic box (20 sessions) or transparent plastic sheet (45 sessions) primarily during the initial period of the pandemic (Fig. 3 A, B).
-
-
High flow oxygen therapy (11 sessions) (Fig. 3C, D).
-
-
Administration of anticholinergic as premedication (ex: glycopyrrolate in around 25 sessions).
Fig. 3.
Barrier methods for ECT administration using Acrylic box (3A), & plastic sheet (3B). Oxygen administration using highflow oxygen therapy with nasal cannula underneath the surgical mask (3C,D).
4.2.7. Measures taken to make ECT economical
-
-
One Bain's circuit (till September) and one closed-loop circuit (since October) is used for all the patients for a given day though the HME filter is changed for every patient.
-
-
After each patient, all team members change their outer gloves. Visors are cleaned with alcohol wipes if soiled by patients' secretions.
-
-
Different anesthesia masks (reusable) are used for each patient and reused after appropriate gas sterilisation.
-
-
For non-affording patients, the HME filter is packed, labeled, and reused a maximum of five times for the same patient.
-
-
PPE is not changed between patients.
4.2.8. Disinfection and cleaning
-
-
Surface disinfection of the high exposure surfaces like trolley, anesthesia machine, and monitor, Bain's circuit, ECT machine and electrodes, side railings of the cot, and suction tubing is done by wiping it with 2 % glutaraldehyde solution followed by spraying the surfaces with 70 % alcohol spray.
-
-
Used anesthesia mask after each case and Bain's circuit at the end of all the cases are put in 1 % hypochlorite solution for at least 20−30 min. Later, they are cleaned with soap water, dried and packed in the zip-lock plastics, and sent for gas sterilisation.
-
-
Floor is cleaned with 1 % hypochlorite solution between patients' ECT sessions, and terminal cleaning is done at the end of the day.
5. Impact of COVID-19 pandemic on ECT practice - Institute experience
We observed a reduction in the number of patients receiving ECT as ECT services in the early period of the pandemic was restricted to emergent or urgent indications (such as catatonia, significant risk of harm to self or others in various psychiatric illnesses), the effect of the nationwide lockdown during the initial months (March to May 2020). ECT service was restricted to three days per week (April to August 2020). Since September 2020, we resumed our ECT services to six days a week as more patients started visiting the hospital with ease of transportation. From April till November 2020, we have administered 1083 sessions with an average of 7 sessions per day as against 1927 sessions during the period January to March 2020 with an average of 27 sessions per day (Table 2 ). The turnover time between the patients increased from 10 min to 30 min. We have not observed any significant change in the complication rate (5/1083 vs. 12/1927). All patients who sustained post-ECT desaturation had a higher BMI and got settled by oxygen supplementation through a Hudson mask. They were then isolated and tested for COVID-19, but none of them turned out to be positive. As of November 2020, we have administered ECT to 5 COVID-19 positive patients with a total of 11 sessions without any complications in the red zone OT complex. The COVID-19 positive cases did not have any respiratory signs and symptoms. Glycopyrrolate was administered for two patients in-view of excess oral secretions. BMV and airway suctioning were avoided in all the patients. ECT was uneventful in all these patients. Till now, none of our ECT team members has developed any symptoms suggestive of COVID-19, nor antibody tested positive.
Table 2.
Details of ECT service during the COVID-19 pandemic.
| Month in 2020 | No. of Days of ECT services | No. of Patients | No. of Sessions | Complications (number of patients) | Remarks |
|---|---|---|---|---|---|
| January | 26 | 93 | 663 | 5 | Oxygen desaturation settled by oxygen supplementation |
| February | 24 | 88 | 618 | 3 | Desaturations settled by oxygen supplementation |
| March | 21 | 93 | 646 | 4 | Desaturations settled by oxygen supplementation |
| April | 9 | 25 | 56 | 0 | |
| May | 17 | 33 | 141 | 0 | |
| June | 18 | 33 | 146 | 1 | prolong desaturation during recovery |
| -post-procedure X-ray, CT chest were clear. | |||||
| Pt kept in observation till evening. | |||||
| At discharge, saturation 98 % on room air | |||||
| July | 17 | 24 | 77 | 0 | |
| August | 19 | 32 | 114 | 4 | 2- prolong desaturation at recovery, requiring oxygen support and observation for 3 h |
| 1- upper airway obstruction leading to insertion of nasal airway, | |||||
| 1- obese patient had desaturation during ECT, managed with bag-mask ventilation | |||||
| September | 27 | 38 | 169 | 0 | |
| October | 26 | 45 | 193 | 0 | |
| November | 24 | 47 | 187 | 0 |
6. Minimum Standards for conducting ECT-therapy based on our experiences
-
1
ECT therapy can be given to the patients deemed necessary.
-
2
Educate the patient and their family members about the hand hygiene, social distancing and mask etiquettes with repeated reinforcement.
-
3
Screening of all the patients for temperature and SpO2, coming for ECT.
-
4
Identify the ECT team members, keep them to minimum and conduct regular training program.
-
5
Segregation of the patients posted for the ECT, based on their COVID-19 positivity or clinical suspicion and if feasible to have dedicated facility for COVID-19 positive patients for judicious use of available resources.
-
6
Testing policies for the ECT patients as per the infection rate and institution policies.
-
7
Irrespective of the test results, minimum standards of barrier precautions (surgical cap, goggles / visor, N95 or higher mask, surgical dress, double gloves and shoe covers) to be maintained throughout the ECT therapy.
-
8
Change of outer gloves between the cases and cleaning of visors if soiled with secretions.
-
9
Prolonged preoxygenation (3−5 min) with low-oxygen flows <6 L/min.
-
10
Use HME filters between the anatomical face mask and anesthesia circuit (to be changed for every case) and between expiratory port of the breathing circuit and anesthesia machine (can be changed at the end of the day).
-
11
Use separate anatomical face mask for each patient for a given day.
-
12
Avoid BMV (or keep it to minimal) and avoid airway handling.
-
13
Appropriate handling, disposal and cleaning of the used anatomical mask, circuits, anesthesia and ECT machine at the end of the day.
-
14
In-between patients, appropriate cleaning and disinfection of the cots, ECT and anesthesia machines followed by terminal cleaning at the end of the day.
7. Conclusion
ECT is a vital treatment modality for psychiatry patients providing immediate symptom relief. The COVID-19 pandemic has taught us multiple lessons in reorganizing the patient flow, safe practice, preventing cross-contamination, and ensuring patient safety even in trying times.
Disclosure statement
The authors report no financial disclosure.
Declaration of Competing Interest
The authors report no conflict of interest.
Acknowledgement
None.
References
- Amad A., Magnat M., Quilès C., Yrondi A., Sauvaget A., Bulteau S., Plaze M., Rotharmel M., Polosan M., Lévy-Chavagnat D., Jaafari N., Vaiva G., Thomas P. Évolution of electro-convulsive therapy activity in France since the beginning of the COVID-19 pandemic. L’encephale. 2020;46:S40–S42. doi: 10.1016/j.encep.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade C. COVID-19 and lockdown: delayed effects on health. Indian J. Psychiatry. 2020;62:247–249. doi: 10.4103/psychiatry.IndianJPsychiatry_379_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anelli F., Leoni G., Monaco R., Nume C., Rossi R.C., Marinoni G., Spata G., De Giorgi D., Peccarisi L., Miani A., Burgio E., Gentile I., Colao A., Triassi M., Piscitelli P. Italian doctors call for protecting healthcare workers and boosting community surveillance during a covid-19 outbreak. BMJ. 2020;368:m1254. doi: 10.1136/bmj.m1254. [DOI] [PubMed] [Google Scholar]
- Baghai T.C., Möller H.J. Electroconvulsive therapy and its different indications. Dialogues Clin. Neurosci. 2008;10:105–117. doi: 10.31887/DCNS.2008.10.1/tcbaghai. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellini H., Cretaz E., Rigonatti L.F., Conto C.D.R.D., Melzer-Ribeiro D.L., Busatto-Filho G., Brunoni A.R., Gallucci-Neto J. Electroconvulsive therapy practice during the COVID-19 pandemic. Clinics. 2020;75:e2056. doi: 10.6061/clinics/2020/e2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boland X., Dratcu L. Electroconvulsive therapy and COVID-19 in acute inpatient psychiatry: more than clinical issues alone. J. ECT. 2020;36:223–224. doi: 10.1097/YCT.0000000000000708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite R., McKeown H.L., Lawrence V.J., Cramer O. Successful electroconvulsive therapy in a patient with confirmed, symptomatic COVID-19. J. ECT. 2020;36:222–223. doi: 10.1097/YCT.0000000000000706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown H., Preston D., Bhoja R. Thinking outside the box: a low-cost and pragmatic alternative to aerosol boxes for endotracheal intubation of COVID-19 patients. Anesthesiology. 2020;133:683–684. doi: 10.1097/ALN.0000000000003422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryson E.O., Aloysi A.S. A strategy for management of electroconvulsive therapy patients during the COVID-19 pandemic. J. ECT. 2020;36:149–151. doi: 10.1097/YCT.0000000000000702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burhan A.M., Safi A., Blair M., O’Reilly R. Electroconvulsive therapy for geriatric depression in the COVID-19 era: reflection on the ethics. Am. J. Geriatr. Psychiatry. 2020;28:900–902. doi: 10.1016/j.jagp.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevance A., Gourion D., Hoertel N., Llorca P.M., Thomas P., Bocher R., Moro M.R., Laprévote V., Benyamina A., Fossati P., Masson M., Leaune E., Leboyer M., Gaillard R. Assurer les soins aux patients souffrant de troubles psychiques en France pendant l’épidémie à SARS-CoV-2 [Ensuring mental health care during the SARS-CoV-2 epidemic in France: A narrative review] L’Encephale. 2020;46:S3–S13. doi: 10.1016/j.encep.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colbert S.A., McCarron S., Ryan G., McLoughlin D.M. Immediate impact of coronavirus disease 2019 on electroconvulsive therapy practice. J. ECT. 2020;36:86–87. doi: 10.1097/YCT.0000000000000688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das S. Mental health and psychosocial aspects of COVID-19 in India: the challenges and responses. J. Health Manag. 2020;22:197–205. doi: 10.1177/0972063420935544. [DOI] [Google Scholar]
- Espinoza R.T., Kellner C.H., McCall W.V. Electroconvulsive therapy during COVID-19: an essential medical procedure-maintaining service viability and accessibility. J. ECT. 2020;36:78–79. doi: 10.1097/YCT.0000000000000689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flexman A.M., Abcejo A.S., Avitsian R., De Sloovere V., Highton D., Juul N., Li S., Meng L., Paisansathan C., Rath G.P., Rozet I. Neuroanesthesia practice during the COVID-19 pandemic: recommendations from society for neuroscience in anesthesiology and critical care (SNACC) J. Neurosurg. Anesthesiol. 2020;32(3):202–209. doi: 10.1097/ANA.0000000000000691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil-Badenes J., Valero R., Valentí M., Macau E., Bertran M.J., Claver G., Bioque M., Baeza I., Bastidas Salvadó A., Lombraña Mencia M., Pacchiarotti I., Bernardo M., Vieta E. Electroconvulsive therapy protocol adaptation during the COVID-19 pandemic. J. Affect. Disord. 2020;276:241–248. doi: 10.1016/j.jad.2020.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover S., Mehra A., Sahoo S., Avasthi A., Tripathi A., D’Souza A., Saha G., Jagadhisha A., Gowda M., Vaishnav M., Singh O., Dalal P., Kumar P. State of mental health services in various training centers in India during the lockdown and COVID-19 pandemic. Indian J. Psychiatry. 2020;62:363. doi: 10.4103/psychiatry.IndianJPsychiatry_567_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intensive Care Medicine and Anaesthesia societies COVID-19 web site, London, UK . 2020. COVID-19 Airway Management Principles.https://icmanaesthesiacovid-19.org/covid-19-airway-management-principles March 19. [Google Scholar]
- Kellner C.H., Obbels J., Sienaert P. When to consider electroconvulsive therapy (ECT) Acta Psychiatr. Scand. 2020;141:304–315. doi: 10.1111/acps.13134. [DOI] [PubMed] [Google Scholar]
- Lapid M.I., Seiner S., Heintz H., Hermida A.P., Nykamp L., Sanghani S.N., Mueller M., Petrides G., Forester B.P. Electroconvulsive therapy practice changes in older individuals due to COVID-19: expert consensus statement. Am. J. Geriatr. Psychiatry. 2020;28:1133–1145. doi: 10.1016/j.jagp.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Fink J.B., Ehrmann S. High-flow nasal cannula for COVID-19 patients: low risk of bio-aerosol dispersion. Eur. Respir. J. 2020;55 doi: 10.1183/13993003.00892-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limoncelli J., Marino T., Smetana R., Sanchez-Barranco P., Brous M., Cantwell K., Russ M.J., Fogarty Mack P. General anesthesia recommendations for electroconvulsive therapy during the coronavirus disease 2019 pandemic. J. ECT. 2020;36:152–155. doi: 10.1097/YCT.0000000000000705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luccarelli J., Fernandez-Robles C., Fernandez-Robles C., Horvath R.J., Berg S., McCoy T.H., Seiner S.J., Henry M.E. Modified anesthesia protocol for electroconvulsive therapy permits reduction in aerosol-generating bag-mask ventilation during the COVID-19 pandemic. Psychother. Psychosom. 2020;89:314–319. doi: 10.1159/000509113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mankad M.V., Beyer J.L., Weiner R.D., Krystal A.D. American Psychiatric Publishing, Inc.; Arlington, VA, US: 2010. Clinical Manual of Electroconvulsive Therapy, Clinical Manual of Electroconvulsive Therapy. [Google Scholar]
- Ministry of Health and Family Welfare Directorate General of Health Services, Government of India . 2020. Novel Coronavirus Disease 2019 (COVID-19): Additional Guidelines on Rational Use of Personal Protective Equipment (setting Approach for Health Functionaries Working in non-COVID Areas)https://www.mohfw.gov.in/pdf/AdditionalguidelinesonrationaluseofPersonalProtectiveEquipmentsettingapproachforHealthfunctionariesworkinginnonCOVIDareas.pdf [Google Scholar]
- Ott M., Milazzo A., Liebau S., Jaki C., Schilling T., Krohn A., Heymer J. Exploration of strategies to reduce aerosol-spread during chest compressions: a simulation and cadaver model. Resuscitation. 2020;152:192–198. doi: 10.1016/j.resuscitation.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrides G., Tobias K.G., Kellner C.H., Rudorfer M.V. Continuation and maintenance electroconvulsive therapy for mood disorders: review of the literature. Neuropsychobiology. 2011;64:129–140. doi: 10.1159/000328943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purushothaman S., Fung D., Reinders J., Garrett-Walcott S., Buda M., Moudgil V., Emmerson B. Electroconvulsive therapy, personal protective equipment and aerosol generating procedures: a review to guide practice during Coronavirus Disease 2019 (COVID-19) pandemic. Australas. Psychiatry. 2020;28:632–635. doi: 10.1177/1039856220953699. [DOI] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramakrishnan V.S., Kim Y.K., Yung W., Mayur P. ECT in the time of the COVID-19 pandemic. Australas. Psychiatry. 2020;28:527–529. doi: 10.1177/1039856220953705. [DOI] [PubMed] [Google Scholar]
- Resuscitation Council UK . 2020. Statement on COVID-19 in Relation to CPR and Resuscitation in Healthcare Settings.https://www.resus.org.uk/media/statements/resuscitation-council-uk-statements-on-covid19-coronavirus-cpr-and-resuscitation/covid-healthcare/ May 13. [Google Scholar]
- Schumann R., Silberman E.K., Hotin H.M., Quraishi S.A. Electroconvulsive therapy during a highly contagious respiratory pandemic-A framework during COVID-19. Saudi J. Anaesth. 2020;14:378–382. doi: 10.4103/sja.SJA_455_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sienaert P., Lambrichts S., Popleu L., Van Gerven E., Buggenhout S., Bouckaert F. Electroconvulsive therapy during COVID-19-Times: our patients cannot wait. Am. J. Geriatr. Psychiatry. 2020;28:772–775. doi: 10.1016/j.jagp.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahamtan A., Ardebili A. Real-time RT-PCR in COVID-19 detection: issues affecting the results. Expert Rev. Mol. Diagn. 2020;20(5):453–454. doi: 10.1080/14737159.2020.1757437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang G., Chan A.K.M. Anaesthesia Tutorial of the Week, Tutorial 421. 2020. Perioperative management of suspected/confirmed cases of COVID-19.https://www.wfsahq.org/components/com_virtual_library/media/1c4ec5c64b9aaacf7c47f76a61fb6edc-atow-422-01.pdf [Google Scholar] [Google Scholar]
- Thiruvenkatarajan V., Dharmalingam A., Armstrong-Brown A., Weiss A., Waite S., Van Wijk R. Uninterrupted anesthesia support and technique adaptations for patients presenting for electroconvulsive therapy during the COVID-19 era. J. ECT. 2020;36:156–157. doi: 10.1097/YCT.0000000000000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiruvenkatarajan V., Wong D.T., Kothandan H., Sekhar V., Adhikary S.D., Currie J., Van Wijk R.M. Airway management in the operating room and interventional suites in known or suspected COVID-19 adult patients: a practical review. Anesth. Analg. 2020;131:677–689. doi: 10.1213/ANE.0000000000005043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong Z.D., Tang A., Li K.F., Li P., Wang H.L., Yi J.P., Zhang Y.L., Yan J.B. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerging Infect. Dis. 2020;26:1052–1054. doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tor P.C., Phu A., Koh D., Mok Y.M. Electroconvulsive therapy in a time of coronavirus disease. J. ECT. 2020;36(2):80–85. doi: 10.1097/YCT.0000000000000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tor P.C., Tan J., Loo C. Model for ethical triaging of electroconvulsive therapy patients during the COVID-19 pandemic. BJPsych Bull. 2020:1–4. doi: 10.1192/bjb.2020.99. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) 2020. Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations During Severe Shortages: Interim Guidance.https://apps.who.int/iris/handle/10665/331695 April 6. [Google Scholar]