Abstract
Background: The global impact of COVID-19 pandemic continues to affect the lives of billions of people with recurrent waves. Healthcare systems are struggling to manage pre-existing patient care and recurring covid-19 demands. As a result, we evaluated the mental health impact using systematic review and meta-analysis.
Methods: A comprehensive search was undertaken from April 2020 to 22nd January 2021 using multiple electronic databases. A systematic review protocol was developed and published on PROSPERO registration; CRD42020181481. A random-effects model was used to compute pooled estimates of anxiety, depression, PTSD, insomnia and suicidal thoughts.
Findings: Our search yielded 11,295 studies and of those 287 met the inclusion criteria. The meta-analysis of 206 studies revealed minimal differences in prevalence of anxiety, depression, and PTSD among HCPs compared with the public during the pandemic but higher prevalence of suicidal thoughts/ideation or self-harm (11% vs 5.8%) and lower prevalence of wellbeing (28.2% vs 52.6%) among the public compared to HCPs.
Interpretation: The pandemic has led to a high mental health burden especially amongst HCPs and higher suicidal ideation and lower wellbeing in general public which warrants further investigation and management globally. These findings highlight an emerging critical public health issue that requires urgent solutions.
Keywords: Sars-CoV-2, COVID-19, Healthcare professionals, Health, Mental health and physical wellbeing
Research in context.
Evidence before this study
Mental health impact associated studies exploring the impact of SARS-CoV-2 have been lacking. The likelihood of these studies increasing in the near future is limited, partly due to limited funding availability for mental health associated research in comparison to other clinical areas, as well as the recurring outbreaks which demonstrates that the pandemic is still here and therefore, the mental health impact is equally recurring. Previous systematic reviews have reported primarily on mental health symptoms using different methodologies that demonstrated limited evidence based robustness that could provide better insight to clinicians, clinical researchers and policy makers.
Added value of this study
The added value of this study is based on the evidence based methodology used in the context of a systematic review to evaluate clinical outcomes in mental health. To our knowledge, previous systematic reviews and meta-analysis published do not focus on the impact and array of mental health outcomes using multiple cohorts. Whilst we obtained similar prevalence of anxiety, depression, PTSD, and insomnia among healthcare professionals and the general public, a new development in this study is that there appears to be higher prevalence of suicidal thoughts/ideation or self-harm (11% vs 5.8%) and lower prevalence of wellbeing (28.2% vs 52.6%) among the public compared to healthcare professionals which had previously not been reported. As a result, the clinical significance associated with anxiety, depression and PTSD provide invaluable information to health care services in particular to Mental Health care providers to plan clinical management strategies short, medium and long-term.
Implications of all the available evidence
The prevalence varies between healthcare professionals, patients and the public. However, a common theme that would support global and national healthcare systems would be the development of a mental healthcare strategy for pandemic-related interventions/ treatments and service provision both short, medium and long-term use.
Additionally, self-reporting and subsequent self-assessment using digital interventions could provide support to both patients and organizations to prepare for future pandemics, given the most commonly reported symptomatologies appear to be anxiety and depression. This has both research and clinical implications for current and future patients, clinicians as well as researchers.
Alt-text: Unlabelled box
1. Introduction
The coronavirus disease 2019 (COVID-19) could be considered as the most complex pandemic during the 4th industrial revolution. The pandemic and lockdown has caused an unprecedented sense of fear and anxiety across the globe. This catastrophic phenomenon has resulted in both short- and long-term mental health (MH) and psychosocial implications. A recent review reported adverse psychological effects, which included post-traumatic stress (PTSD) symptoms, confusion and anger to be some of the concerns associated with the current pandemic [1]. An abundance of cross-sectional surveys have demonstrated a high prevalence of depression and anxiety. For example, Rathod and colleagues [2] reported from a three-week analysis of their global survey, healthcare professionals recorded a high proportion of mild depression and anxiety.
Prior to the COVID-19 pandemic, a staff survey conducted in the UK's National Health Service (NHS) in 2019 found 40.3% of healthcare professionals (HCP) reported work-related stress in the previous 12 months that led to issues around wellbeing [3]. This proportion has steadily been increasing, with the latest survey from 2020 stating 33% of frontline doctors and over a quarter of GPs are suffering from anxiety, depression, stress, emotional distress, occupational burnout and/or other mental health conditions [4]. Therefore, it could be hypothesized based on the current research data and clinician reported outcomes, available, these conditions may have been heightened during the pandemic.
The current psychological impact of frontline staff appears to be similar to those recorded during the SARS outbreak in 2003 [5]. Wu and colleagues [5] reported that 549 frontline HCPs of the SARS pandemic reported consistent PTSD symptomatologies over the course of their 3-year study. Further literature has highlighted the COVID-19 pandemic is an event that is unmanageable and unfamiliar, increasing the likelihood of individuals developing PTSD due to the trauma experienced during this ongoing pandemic [[6], [7], [8]]. Exposure to traumatic disasters is not limited to pandemics, it also includes alternative large scale disasters like the 9/11 attacks. An extensive body of literature concluded that since the 9/11 attacks in the past 10 years reported that the prevalence of PTSD among individuals who experienced a high level of exposure to 9/11 was significant [9]. This research coincides with the hypothesis that the greater “dose” of trauma healthcare professionals face during the COVID-19 pandemic leads to a greater adverse effect psychologically.
As per the current reports, COVID-19 first emerged in December 2019, when a cluster of patients with pneumonia of unknown cause in Wuhan were recognized. Furthermore, it has been continuously observed that a significant proportion of patients recovering from severe COVID-19 disease may develop long term and persistent psychological symptoms, either as direct result of the virus or as a result of their experiences of the illness including trauma, treatment and long-term health implications [10]. Some may also present with varying degrees of communication and cognitive impairment [11]. It is now widely recognized that respiratory symptoms of COVID-19 are extremely heterogeneous, ranging from minimal symptoms to significant hypoxia with acute respiratory distress syndrome (ARDS) [12] whilst the pathophysiology remains relatively unknown. The definition of asymptomatic, mild, moderate, severe and critical is summarized in Table 1.
Table 1.
Classification of COVID-19 symptomology.
| Asymptomatic | COVID nucleic acid test positive. Without any clinical symptoms and signs and the chest imaging is normal |
| Mild | Symptoms of acute upper respiratory tract infection (fever, fatigue, myalgia, cough, sort throat, runny nose, sneezing) or digestive (nausea, vomiting, abdominal pain, diarrhea) |
| Moderate | Pneumonia (frequent fever, cough) with no obvious hypoxemia, chest CT with lesions |
| Severe | Pneumonia with hypoxemia (SpO2 <92%) |
| Critical | Acute respiratory distress syndrome (ARDS), may have shock, encephalopathy, myocardial injury, heart failure, coagulation dysfunction and acute kidney injury |
A report from Wuhan mentioned that the time between the onset of symptoms and the development of ARDS was as short as nine days, suggesting that the respiratory symptoms could progress rapidly [13]. Although, further research would need to be conducted to evaluate these findings comprehensively, as there could be a MH impact due ARDS as well. Current medical management is largely supportive with no targeted therapy available as with any virus, which remains dormant until the assimilation with the host. Several drugs including lopinavir-ritonavir, remdesivir, hydroxychloroquine, and azithromycin have been tested in clinical trials [14–15] although, currently there is no evidence to suggest a definitive treatment strategy. However, early interim analysis from these trials show initial aptitude for immune-suppression [16]. To date several vaccines have been approved globally for emergency treatment of the virus including Oxford-AstraZeneca, Pfizer- Biontech, Moderna, etc. However, the MH implications associated with the population pre and post vaccination for example remains unclear.
As of 22nd February 2021, SARS-CoV-2 has affected more than 219 countries resulting in 110,974,862 confirmed cases and 2460,792 deaths and 225,839 new cases [17]. A summary of prevalence and mortality rates by country can be found in Table 2. However, caution must be taken when interpreting this data as there are multi-factorial deficits to the current published datasets with regards to incidence and mortality reporting. These may not include primary, secondary and tertiary care healthcare settings, as well as those that were unreported due to mild symptomatology.
Table 2.
Prevalence and mortality rate of COVID-19 by country.
| Country | Mortality Rate | Prevalence Rate | Total COVID-19 Tests | Definition of Mortality |
|---|---|---|---|---|
| China | 4641 | 84,780 | Unavailable | Not Provided |
| India | 16,893 | 566,840 | 8.61 million | Cases with confirmed positive test for COVID-19 only. Not counting suspected cases |
| Italy | 34,744 | 240,436 | 5.39 million | Any death of patient with COVID-19 that has a death caused by COVID-19 |
| Singapore | 26 | 43,661 | 414,396 | WHO guidelines followed |
| South Korea | 282 | 12,800 | 1.25 million |
|
| Spain | 28,355 | 249,271 | 3.64 million | Cases with confirmed positive test for COVID-19 only |
| United Kingdom | 43,730 | 311, 965 | 7.33 million | WHO Guidelines followed although Dept of Health specified definition used; fatality where COVID-19 mentioned on death certificate. |
| England | 39,187 | 160,587 | 2.29 million | Deaths included if the deceased had a positive test for COVID-19, however long after the test they died. |
| Scotland | 2482 | 18,251 | 272,561 | Deaths that have been registered with a confirmed lab diagnosis of COVID-19 in the 28 days prior to death |
| Wales | 1510 | 15,743 | 182,303 | Deaths of hospital or care home residents where COVID-19 has been confirmed with a lab diagnosis or the clinician suspects this was the causative factor in the death |
| Northern Ireland | 551 | 160,587 | 101,506 | Deaths where the deceased had a positive test for COVID-19 and died within 28 days, whether or not COVID-19 was the causative factor |
| United States | 126,140 | 2.59 million | 32.31 million | Fatality where COVID-19 mentioned on death certificate |
| Japan | 972 | 18,593 | 461,446 | |
| New Zealand | 22 | 1178 | 402,000 |
|
| Canada | 8566 | 103,907 | 2.68 million | Numbers are collated from different provinces which all have own methodologies. |
| France | 29,813 | 164,260 | Unavailable |
*Data up to 30th June 2020.
Whilst the current pandemic is the fifth documented within the last few centuries, there have been many others prior to the most recent outbreaks. But there has been a lag in both scientific theory and evidence-based discussions around pandemics. Therefore, it is critical to now try and understand the cognitive and psychological impact of the virus, as well as the ‘real-world’ psychological impact of the pandemic on healthcare professionals, patients and the general public. This is especially so given the rapid spread of the pandemic, pathogenicity, with antiviral treatments and vaccine development rightly being the primary focus.
2. Methods
An evidence synthesis methodology was developed with a systematic protocol that was peer reviewed and registered with PROSPERO database (CRD42020181481) [67]. The reporting of the systematic review and meta-analysis was conducted as per PRISMA guidelines.
2.1. Search strategy and selection criteria
A comprehensive, systematic search was conducted for published articles using multiple databases of PubMed, Proquest, EBSCOhost and ScienceDirect from April 2020 to 22nd January 2021. Suitable articles were selected in two stages using the PICO (Population/Participants, Intervention(s), Comparison, Outcome) strategy. We included studies comprising empirical, qualitative or quantitative evidence on COVID-19 and mental health in the patients, general public and healthcare professional population. We excluded editorials, commentary, letters to the editor, simple reviews and studies that did not have the outcomes measures specified in the protocol.
2.2. Study selection and data extraction
First, the title and abstract of each article were screened independently by investigators (KE, TT, SA-Y). If there was a consensus that an article was not suitable for inclusion the article was excluded. Next, the full text articles were screened independently by two investigators and included if all authors agreed. The following information was extracted from all included studies, citation details, methods used to establish processes and corresponding characteristics, key findings, limitations and conclusions reported. Any differences of opinion or quires were reviewed and resolved by (PP &GD). The authors were not blinded with respect to the article's authors or the journal in which it was published. The investigators organized the articles into three categories, namely: healthcare professionals, patients and general public. Two investigators extracted predefined clinical variables (summarized in supplementary Table 1). Each variable was then inspected to understand if it was a pre-existing condition, direct result of COVID, if treatment was received and the symptomology. Investigators (GD& PP) independently cross-checked data retrieved from each article as per our refinement protocol (supplementary Fig. 1).
2.3. Risk of bias (quality) assessment
Majority of the studies included were cross-sectional. All literature retrieved were critically appraised on an individual basis using common variables. Independent reviewers appraised methodological quality and risk of bias according to the Newcastle-Ottawa Scale (NOS) that has validity for use in cohort studies Wells et al. [18] and the adapted version by Modesti et al. [19] was used for cross-sectional studies in meta-analyses. An eight item scale with three quality parameters (i) selection, (ii) comparability and (iii) outcome. We rated the quality of the studies (good, fair and poor) by allocating each domain with stars in this manner:
-
•
A Good quality score was awarded 3 or 4 stars in selection, 1 or 2 in comparability, and 2 or 3 stars in outcomes
-
•
A Fair quality score was awarded 2 stars in selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes.
-
•
A Poor quality score was allocated 0 or 1 star(s) in selection, 0 stars in comparability, and 0 or 1 star(s) in outcomes domain [18].
Following the application of the refinement protocol, 287 studies were evaluated, and their full text was reviewed to confirm the inclusion/exclusion criteria were met. The extraction of data had a specific focus on highlighting variables reported within the studies and any symptomologies reported within the three population groups, namely: patients, HCPs and the general public, in addition to providing an overall scientific justification for the inclusion of each study.
2.4. Outcomes
The following outcomes were included in the meta-analysis based on the availability of statistics reported by each study:
-
•
Prevalence of anxiety, depression, PTSD, insomnia, suicidal thoughts/ideation, or self-harm and wellbeing among HCP and the public
-
•
Prevalence of poor sleep quality and alcohol use among the public
-
•
Clinical significance of the prevalence data identified
-
•
Critical interpretive synthesis of common MH reported outcomes amongst HCPs and the general public
The outcomes for patients could not be synthesized for the meta-analysis; therefore, these are presented as narrative review only.
2.5. Statistical analysis
Estimates for studies that reported median and interquartile range were converted to mean and standard deviation before meta-analyses [20]. For studies that reported only mean (SD) or median (IQR) and no prevalence we employed Monte Carlo simulations to estimate the prevalence based on appropriate cut-off points for the tool used to measure the outcome. For this we assumed normality of the distribution. For each outcome, if a study reported estimates for multiple groups of healthcare professionals or the public, we combined these estimates into one estimate for that study. A random-effect model was used to estimate pooled estimate of prevalence. We used the I2 statistic to assess heterogeneity between the studies; values of 25%, 50%, and 75% were used to categorize the degree of heterogeneity into low, moderate, and high, respectively [21]. We investigated sources of heterogeneity by conducting stratified analyses by mean/median age (≤30 years vs >30 years), country, outcome measurement tool, and study quality. We also conducted sensitivity analyses by estimating the pooled prevalence after removal of studies for which the prevalence was calculated from simulations. Publication bias was assessed using visualization of funnel plots and Egger's test for estimates with a sample size ≥10. We constructed funnel plots by study quality to examine if it contributed to publication bias. Meta-analyses were conducted using STATA version 14.0 (StataCorp, College Station, TX, USA). Statistical testing was conducted at a two-tailed alpha level of 0.05.
2.6. Role of funding
KE, GD, and PP are supported by National Institute for Health Research (NIHR) Research Capability Funding (RCF) and by Southern Health NHS Foundation Trust and Oxford Brain Health Clinical Trials Unit. All of the study sponsors had no further role in the study design, data collection, analysis and interpretation of data; in the writing of the report and in the decision to submit the paper for publication.
3. Results
3.1. General characteristics
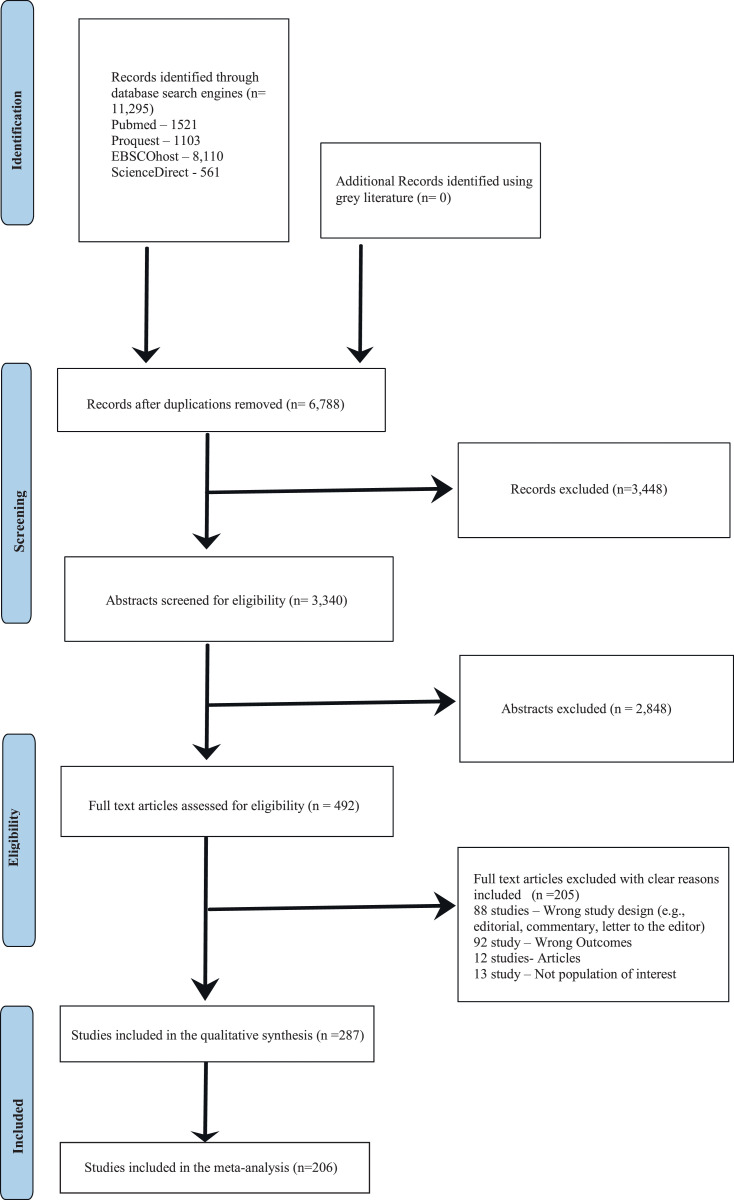
Our comprehensive literature search undertaken on April 2020 (up to 22nd January 2021) identified 11,295 articles of these (n = 287) met the inclusion criteria as shown in Fig. 1. Detailed descriptions of the studies included in this review are displayed in STable 1. This also includes provides NOS quality assessment scores of included studies.
Fig. 1.
PRISMA Chart.
3.2. Meta-analysis
For the meta-analysis we included 206 studies (83 in healthcare professionals, 134 among the public, and 11 studies in both these populations) with a sample size of 721,244 and mean/median age ranging from 15.3 to 71 years. About a third of the studies was conducted in China (n = 62) followed by U.S.A. (n = 18), the U.K. (n = 16), and Italy (n = 15) and nine were multinational.
There were 69, 66, 19, 17, four, and three studies included in the meta-analysis with prevalence data of anxiety, depression, PTSD, insomnia, suicidal thoughts/ideation or self-harm, and wellbeing among healthcare professionals, respectively. There were 102 studies included for anxiety, 105 for depression, 19 for PTSD, 14 for insomnia, six for poor sleep quality, ten for suicidal thoughts/ideation or self-harm, nine for wellbeing, and 11 for alcohol use among the public. There were 13 studies that reported mental health outcomes in patients; however, none of these could be harmonized or the number of studies for an outcome was too small for a meta-analysis.
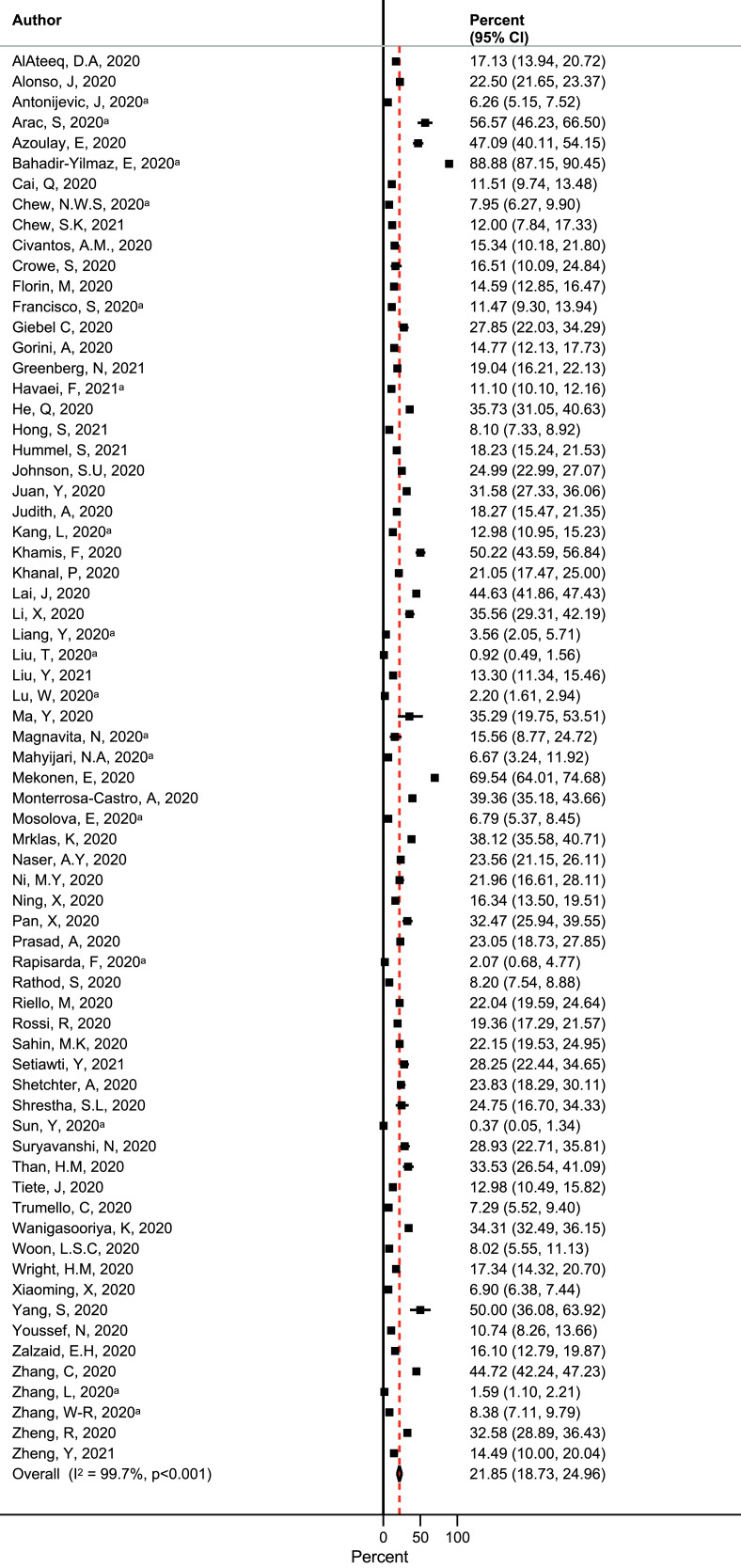
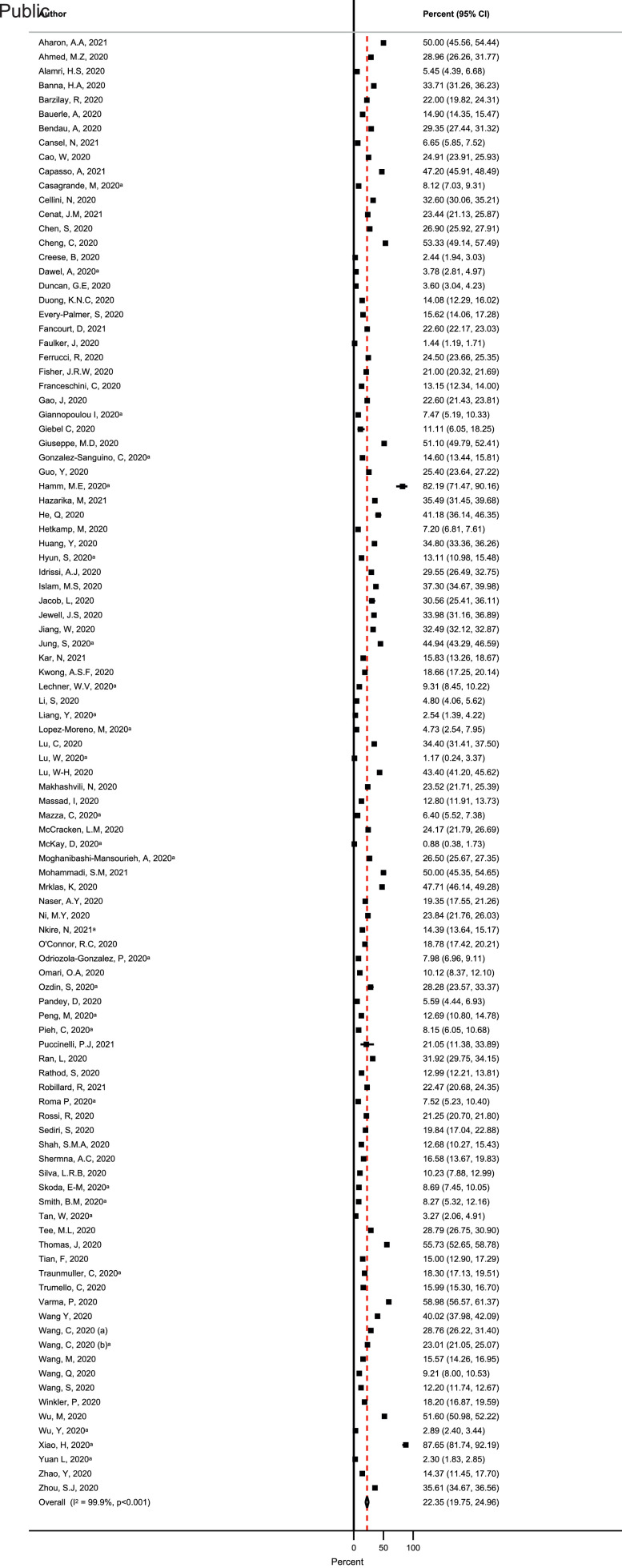
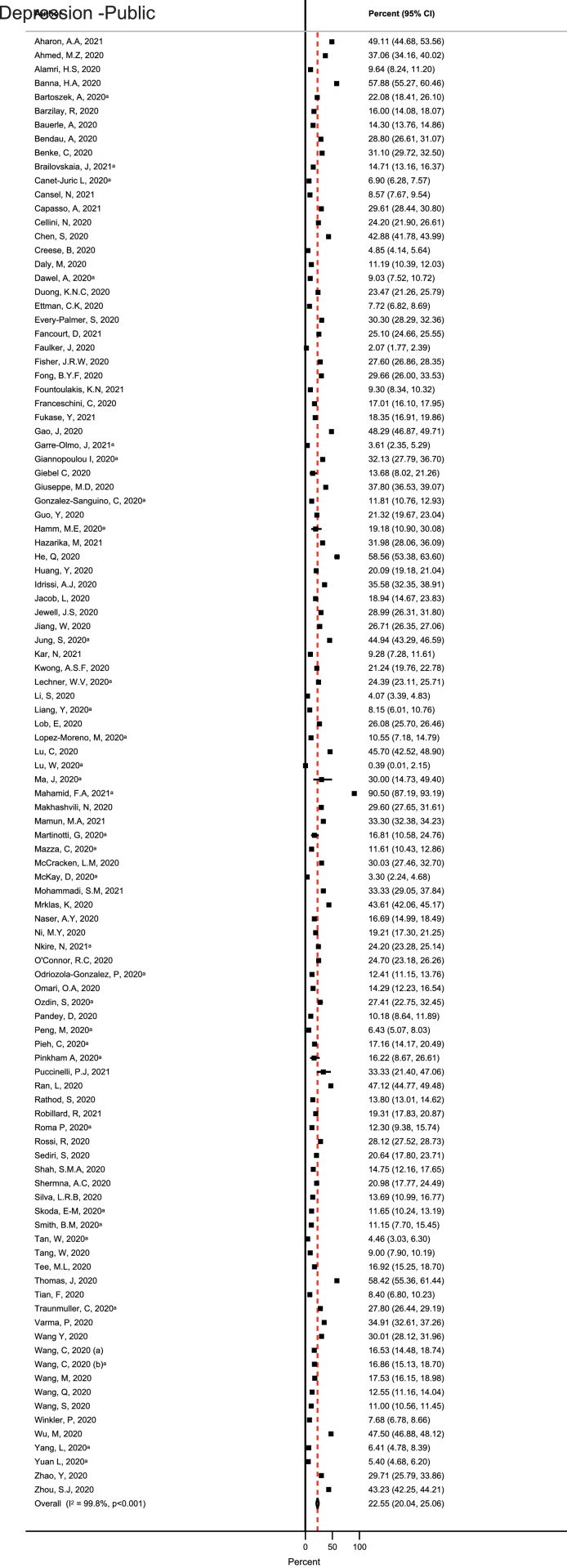
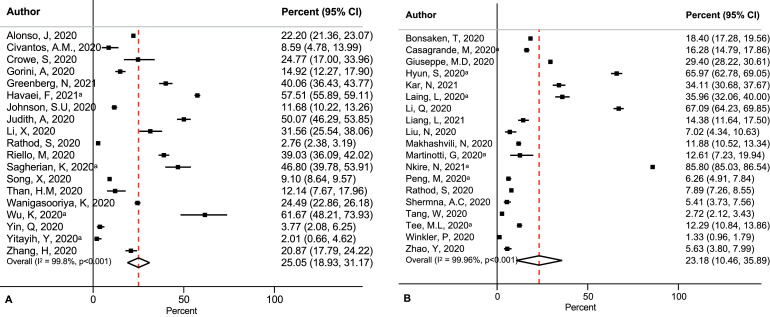
Among healthcare professionals, the pooled prevalence of anxiety was 21.9% (95% CI: 18.7−25%) (Fig. 2) whereas this estimate was 22.4% (95% CI: 19.8 – 25%) among the public (Fig. 3). The estimates for depression were 23.4% (95% CI: 20.6−26.3%) (Fig. 4) and 22.6% (95% CI: 20.0−25.1%) (Fig. 5) among healthcare professionals and the public, respectively.
Fig. 2.
Forest plot of prevalence of anxiety among healthcare professionals. Note: aPrevalence calculated from mean and standard deviation using Monte Carlo simulation.
Fig. 3.
Forest plot of prevalence of anxiety among the public. Note: aPrevalence calculated from mean and standard deviation using Monte Carlo simulation.
Fig. 4.
Forest plot of prevalence of depression among healthcare professionals. Note: aPrevalence calculated from mean and standard deviation using Monte Carlo simulation.
Fig. 5.
Forest plot of prevalence of depression among the public. Note: aPrevalence calculated from mean and standard deviation using Monte Carlo simulation.
The prevalence for PTSD was 25.0% (95% CI: 18.9−31.2%) (Fig. 6A) for healthcare professionals whereas among the public this estimate was marginally lower at 23.2% (95% CI: 10.5−35.9%) (Fig. 6B). There was minimal difference in the prevalence of insomnia among healthcare professionals and the public (24% vs 23%) (SFig. 1A and B). In addition to this, about 39% of the public reported poor quality of sleep that was mostly measured using the Pittsburgh Sleep Quality Index (PSQI) questionnaire (SFig. 2). The prevalence of suicidal thoughts/ideation or self-harm was 11% (95% CI: 6.4−15.7%) among the public (SFig.3B) whereas among healthcare professionals the estimate was 5.8% (95% CI: 4.7– 7.0%) (SFig. 3A). The prevalence of higher wellbeing was higher among healthcare professionals (52.6%, 95% CI: 43.8– 61.4%) (SFig. 4A) whereas among the public the prevalence was 28.2% (16– 40.4%) (SFig. 4B). There was minimal difference in the prevalence of alcohol use among the public for increased (22.9%) and decreased (21.7%) alcohol use but the prevalence for no change in alcohol use was high at 52% (SFig.5).
Fig. 6.
Forest plot of prevalence of post-traumatic disorder among (A) healthcare professionals and (B) the public. Note: aPrevalence calculated from mean and standard deviation using Monte Carlo simulation.
The heterogeneity was high for all outcomes included in the meta-analysis.
3.3. Sensitivity and subgroup analysis
We were able to conduct sub-group analysis by mean/median age (≤30 years vs >30 years) for prevalence estimates of anxiety, depression, PTSD, and insomnia among healthcare professionals and the public. These analyses found insufficient evidence for heterogeneity by mean/median age for prevalence estimates of anxiety, depression, PTSD, and insomnia among healthcare professionals (SFigs. 6, 8, 10, and 12). Among the public there was insufficient evidence to explain heterogeneity by mean/median age groups for anxiety and insomnia (SFigs. 7 and 13). However, there was evidence for heterogeneity by mean/median age (≤30 years vs >30 years) for depression (P value heterogeneity: 0.003) and PTSD (P value heterogeneity: 0.04) estimates (SFigs. 9 and 11). The prevalence of depression among the public was greater for ≤30 years age group compared to >30 years age group (31% vs 18.4%) (SFig.9). Similarly, the prevalence of PTSD was higher among ≤30 years compared to >30 years (49% vs 12.8%) (SFig. 11).
The analyses by country found insufficient evidence to explain the high heterogeneity found in the meta-analysis for anxiety and depression among healthcare professionals (SFigs. 14 and 16) and anxiety among the public (SFig.15). However, it revealed significant heterogeneity by country of study (P value heterogeneity: <0.0001) (SFig. 17). For prevalence estimates of PTSD and insomnia there were insufficient number of studies to conduct stratified analyses, but inclusion of studies conducted only in China found little difference in the prevalence of PTSD and insomnia among healthcare professionals in China (SFigs.18 and 20) the estimates from the main meta-analysis. However, among the public studies conducted solely in China has a lower prevalence of PTSD and insomnia compared the estimates from the main meta-analysis (19.8% vs 23.2% for PTSD and 18.7% vs 23% for insomnia) (SFigs.19 and 21).
The analyses stratified by measurement tool for anxiety, depression, and PTSD among healthcare professionals and the public did not find sufficient evidence for heterogeneity (SFigs. 22, 23, 24, 25, 26, and 27).
The high heterogeneity persisted in the sensitivity analyses that were conducted after removal of studies in which prevalence was computed using simulations of reported mean/median and SD/IQR (SFigs. 28, 29, 30, 31, 32, 33, 34, 35). There was not much difference in the prevalence of anxiety, depression, PTSD, and insomnia among healthcare professionals and anxiety and depression among the public for meta-analyses that included original prevalence estimates and meta-analyses that included both the original and simulated estimates. However, the prevalence was lower in the analysis that included only original prevalence estimates for PTSD (17.1% vs 23.2% for both original and simulated estimates) (SFig. 33) and higher for prevalence of insomnia (28.2% vs 23% for both original and simulated estimates) among the public (SFig. 35).
Stratified analyses by study quality revealed that lower prevalence of anxiety among healthcare professionals for good quality studies (15.6%) (SFig. 36) and significant heterogeneity between good and fair quality studies (Pheterogeneity =0.01). Among the public, there was minimal difference in the prevalence of anxiety (fair quality: 23.8% vs good quality: 20.2%); however, study quality could not explain the heterogeneity between the studies (Pheterogeneity =0.18) (SFig. 37). For depression, there was not much difference in the prevalence by study quality among healthcare professionals (SFig. 38) and the public (SFig. 39) with no evidence for heterogeneity by study quality.
3.4. Publication bias
We were able to assess publication bias for prevalence of anxiety, depression, PTSD, and insomnia among both healthcare professionals and the public and alcohol use among the public. Visual inspection of funnel plots indicated publication bias for all these analyses (SFigs. 40, 41, 42, 43, 44, 45, 46, 47, and 48). Egger's test found evidence for publication bias for prevalence estimates of anxiety (bias (SE): 12.8 (2.6), p <0.0001), depression anxiety (bias (SE): 11.6 (2.1), p <0.0001), PTSD anxiety (bias (SE): 14.4 (5.4), p = 0.02), and insomnia anxiety (bias (SE): 21.3 (6.7), p <0.01) estimates among healthcare professionals. Among the public, Egger's test suggested publication bias for anxiety (bias (SE): 12.6 (4.1), p <0.0001) and insomnia (bias (SE): 13.8 (5.4), p = 0.03) estimates but not for depression (bias (SE): 7.2 (3.7), p = 0.053) and PTSD (bias (SE): 17.9 (18.9), p = 0.36) estimates.
When we examined publication bias by study quality, we found publication bias for studies that were deemed fair and included in the prevalence estimate of both anxiety and depression among the public but not for good quality studies (SFigs. 50, 52). Among healthcare professionals, the publication bias persisted for both good and fair quality studies (SFigs. 49, 51).
3.5. Studies among patients
There were three studies that reported anxiety among COVID-19 patients [[22], [23], [24]]. Hao et al. reported mean (SD) DASS-21 of 6.6 (9) among psychiatric patients and 1.5 (2.7) among healthy controls. Hamm, [24] reported mean PROMIS-anxiety of 57.5 (8) among older adults with MDD. Zhang et al. reported mean GAD-7 score of 10.8 (1.2) among patients of mean age of 42.5 years [22].Three studies reported mean depression scores – Hao et al. reported mean DASS-21 of 8.3 (10.3) among psychiatric patients and 2.2 (3.5) among healthy controls. Hamm et al. reported mean depression score of 8.7 (5) using PHQ-9 among older adults with MDD. Zhang et al. reported mean PHQ-9 score of 11.7 (1.4). Two studies [22–23] reported insomnia among COVID-19 patients using ISI. Hao et al. found a mean score of 10.1 (7.2) among psychiatric patients and 4.6 (4.0) among healthy controls whereas Zhang et al. found a mean ISI score of 8.7 (1.9) among 30 COVID-19 patients. Other outcomes that were reported among patients were sleep quality, suicidal behavior, COVID-induced psychosis, and death by suicide. Muruganadam [25], reported disturbed but manageable sleep among 26.5% patients and disturbed but unmanageable sleep among 11.4% patients. Xiao [26], reported mean PSQI score of 8.5 (4.5) among 170 patients. Mamun [27], Griffiths [28], reported suicidal behavior among 12 and six patients, respectively, whereas Bhuiyan [29], reported eight deaths by suicide among COVID-19 patients. Three patients who presented to the emergency medical services with new-onset psychotic symptoms reported COVID-induced psychosis [30].
Synthesizing qualitative studies is growing momentum [31]. Given our large number of cross-sectional studies we used thematic synthesis to identify key themes from included studies. Table 3 provides a list of key emergent themes and in which groups they were prevalent.
Table 3.
Themes.
| Themes | Population Groups | ||
|---|---|---|---|
| General Public (n = 60%) | Healthcare Professionals (n = 35%) | Mental Health Patients (n = 5%) | |
| Anxiety | ++++++++++++++++++++++++++++++++++++++++++++++++ ++++++++++++++++++++++++++++++++++++++++++++ ++++++++++++++++ |
+++++++++++++++++++++++++++++++++++ +++++++++++++++++++++++++++++++++++++ |
++++++ |
| Depression | +++++++++++++++++++++++++++++++++++++++++++++++++ +++++++++++++++++++++++++++++++++++++++++++++++++++ |
+++++++++++++++++++++++++++++++++++ ++++++++++++++++++++++++++ |
+++++++ |
| Sleep disruption/quality | +++++++++++++++++++++++++ | ++++++++++++ | +++ |
| PTSD | +++++++++++++++++++++++ | +++++++++++++++++++++++ | + |
| Insomnia | ++++++++++++ | ++++++++++++++ | |
| Well-being | ++++++++++++++ | +++++ | |
| Suicide/Suicidal behavior | +++++++++++++++ | ++++ | ++ |
| Stress | ++++++++++ | +++++++ | |
| Alcohol consumption | ++++++++++ | + | + |
| Physical Activity | +++++++ | + | |
| Substance Abuse | ++++ | + | ++ |
| Fear | ++++ | + | + |
| OCD | ++++ | ++ | |
| Gender Differences | ++++ | ||
| Loss of work | +++ | ||
| Psychotic Symptoms | + | + | + |
| Isolation | ++ | + | |
| Psychosis | + | + | |
| Persecution | + | ||
| Risk Perception | + | ||
| Headache | + | ||
| Overwhelming Workload | + | ||
| Quality of Life | + | ||
| Life Stressors | + | ||
| Disgust | + | ||
| Knowledge surrounding COVID-19 | + | ||
| Murder-suicide | + | ||
| Starvation | + | ||
| Psychosis post COVID infection | + | ||
| Economic Status | + | ||
| Social Support | + | ||
| Infodemia | + | ||
| Rumination | + | ||
| Diet | + | ||
| Trauma | + | ||
| Religion | + | ||
| Workplace violence | + | ||
4. Discussion
In this systematic review and meta-analysis, we found similar prevalence of anxiety, depression, PTSD, and insomnia among healthcare professionals and the general public, but higher prevalence of suicidal thoughts/ideation or self-harm (11% vs 5.8%) and lower prevalence of wellbeing (28.2% vs 52.6%) among the public compared to healthcare professionals indicative of impact of the pandemic on both physical and mental health of these cohorts. However, in most studies, different rating scales were used to confirm symptoms thereby preventing MH outcomes to be unilaterally confirmed due to the subjectivity the reporting may include. Furthermore, it was generally unclear if any clinical diagnoses were made which could have unreported clinical implications that is difficult to predict. In relation to HCPs, it remains unclear if these were both frontline and non-frontline staff. Similarly, a breakdown of the staffing categories were not reported, this would be vital for both clinical and service delivery decision making associated with occupational burnout, resources and meeting capacity to demand would be based on some of these factors.
Based on the findings, it appears, the general public may have had challenges with their mental health. However, it remains to be seen those who contracted COVID-19 versus those who didn't and the mental health implications across these 2 groups. Similarly, it remains unclear, of the general public that took part in these studies, those who were tested for covid-19 with a negative result versus the opposite as this would further alter the clinical significance and implications surrounding the mental healthcare needs. Since most cross-sectional studies included in this study do not appear to have longitudinal data, this further purports the need for comprehensive longitudinal research to be conducted to evaluate the long-term MH impact of COVID-19 on patients, HCPs and the general public as well as the healthcare systems. Equally, it would be important to understand any potential comorbidities associated with the HCPs, patients and the general public, as these underlying conditions could further exacerbate the MH impact determined. As a result, it could be said, a bi-directional relationship could exist between the reported as well as perceived MH impact and the psychosocial dynamics that could influence even cultural paradigms that are deterrents of social constructs.
These findings show some consistency with several other systematic reviews and editorials published. Three systematic reviews published reports on the prevalence of anxiety and depression within the general public [[32], [33], [34]] which are the two most common indicators of psychological impact reported in our systematic review. The prevalence rate of anxiety and depression symptoms was 33% and 28%, respectively, in Luo et al. [32] and 31.9% and 33.7% in Salari et al. [33], with these findings being consistent with the current systematic review that indicated a pooled prevalence of 22.4% for anxiety and 22.6% for depression in the general public. Furthermore, all quantitative studies included in Luo et al. review were cross-sectional surveys or cohort studies, which is consistent with the type of publications included within the current systematic review. However, the review [34] showed noticeable variation in the prevalence of anxiety ranging from 6.33 to 50.9% and depression ranging from 14.6% to 48.3%. The variation in prevalence rates from across the 19 studies included could have been due to the various measurement scales used, plus also potential cultural differences towards mental health and reporting patterns. An additional review by Sheraton et al. [35] reported higher incidence of insomnia within healthcare professionals during COVID-19 which is similar to the reports of insomnia in the healthcare professionals included in this current review. However, this review consisted of only 14 publications and was not specific to mental healthcare professionals.
Our review found consistently higher levels of distress in healthcare workers and echoes studies such as Rathod et al. [2] where data gathered over a 3 week period demonstrated a comparison of HCPs and non-HCPs self-reporting higher proportion of mild depression and anxiety. A snapshot to the current psychological state of HCPs of similar increases in the prevalence rate of depression, anxiety and sleep disturbances has been provided by Ho et al. [36] and Ali et al. [37].
It is evident, the imperative role of the global healthcare systems are playing in trying to maintain high quality care levels to patients and the general public. As a consequence of this, HCP's own MH and wellbeing has been impacted negatively. To resolve this, several hospitals for example in China that were greatly impacted by COVID-19 implemented a three-staged method to care for the psychological wellbeing of staff. The approach involved development of online courses, a hotline team that provided supervision and guidance to callers with psychological problems, and interventions that aim to alleviate stress [38]. Similar approaches could be used by other healthcare systems. Acceleration of digital platforms and tele-psychiatry due to the pandemic provide opportunities to adapt more pandemic preparedness interventions and services including popular health apps to combat the combat the surge in mental health problems. Two apps support by UKRI through the Industrial Strategy Challenge Fund, Sleepio and Daylight apps are specific for NHS workers designed to maintain sleep efficiency, reduce anxiety symptoms and to address mental health issues by providing healthcare workers evidence-based techniques [39–40].
It is equally important to use a ‘lessons learnt’ approach, for example with previous studies outbreaks such as the severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) that showed adverse psychological impacts on HCPs. Their MH outcomes were high levels of anxiety, depression, and stress that resulted in many HCPs having post-traumatic stress disorder [41–42]. These findings have a direct correlation with another recent study exploring the impact of COVID-19 that highlighted a considerable proportion of HCPs in China experiencing a high level of anxiety and depression, insomnia and psychological distress [43]. The meta-analysis of this study further affirms these findings. HCPs in locations affected by pandemics are prone to symptoms of anxiety and depression long term [44]. It is unclear whether these findings are generalizable to the UK for example, but it is worth considering conducting research to implement any preventative strategies for future populations.
Based on our thematic and narrative synthesis, patients admitted to critical care for example, with ARDS experienced higher levels of anxiety (40%), depression (30%) and PTSD (20%) symptomatologies [45]. This is asserted by Bauerle and colleagues [46] study that demonstrated similar findings along with psychological stress within the general population. Another recent survey of patients which compared those with a previous history of a mood disorder with those with no previous or current mental disorders found that psychological distress was elevated, with the highest level of depression and stress in those with bipolar disorder [47]. On the other hand, psychosis and recurrence of more longstanding MH problems are rarer based on current data. Sleep disturbance is common in critically ill patients up to 12 months after hospital discharge, with prevalence ranging between 10 and 60% at six months [48] although this association in the current pandemic can only be hypothesized given the lack of data available. Both subjective and objective studies, however, suggest that sleep disturbance improves over time. Although, this cross-sectional work will require further elaboration in longitudinal studies to confirm the generalizability of these findings.
Additionally, social media in general has inevitably created fear and stress around being infected by COVID-19. Whilst, this could impact those with existing MH disorders significantly, obsessive compulsive disorder (OCD) patients in particular, have had an increase in the symptomatologies since the start of lockdown. In particular, those who displayed contamination symptomatologies prior to the start of the pandemic experienced a worsening during lockdown [49]. It is further reported, people living with schizophrenia could be at increased risk due to a potential lack of insight and poorer decision-making abilities, which could result in difficulties adopting necessary protective measures [50]. This could attribute to an increase in covid-19 incidence and/or transmission rates. Therefore, considerations should be made to preventing relapse or worsening of symptomatologies in those with MH disorders if lockdown and/or self-isolation measures are introduced in the future. Strategies such as remote monitoring of symptomatologies using tele-psychiatry method for example could be useful. Additionally, the use of online psychological intervention tools may be of benefit to those with acute mental wellbeing issues although, where possible, clinicians could provide recommendations for those with an existing clinical diagnoses as well [51]. Undoubtedly, some patients may prefer face to face appointments to remote consultations, whilst others may find the reduced wait and travelling time to be advantageous [52]. Between consultations, text messaging has been found to be an effective way of improving engagement with clinical services [53] and may be useful for HCPs in particular to consider in the current climate.
Another facet to consider are patients recovering from COVID may have ongoing difficulties with any of their daily activities, including personal care, domestic tasks, leisure activities and instrumental activities of daily living [54] which could impact their MH. Based on the evidence of this study, there appears to be a lack of data associated with this aspect and is a knowledge gap that should be addressed by way of conducting research that could include these participants as well.
The evidence indicates that there are a number of unilateral mental health issues to consider and therefore, healthcare systems would need to manage their capacity to demand with caution. MH provision remains a challenge for example in the UK, where the NHS has had various challenges to cater to growing demand. Whilst improvement in MH services are a priority as reported in the NHS long-term plan in the UK, the inadvertent impact of the pandemic would only foster a sense of urgency to address the service issues [55]. Depression and anxiety affect 15–20% of the adult population at any one time and has huge personal and economic burden [56] and a major contributor to suicide [57]. It is evident that the pandemic has exacerbated the presentation of these issues. Although the current pandemic represents a national and global challenge, it also presents opportunities for how the NHS and other healthcare systems initiate better ways to deliver critical care and interventions remotely where possible, and bringing forth a new era in healthcare access. Use of tele-psychiatry and its effectiveness [58] in the UK in particular, warrants further investigation [59] to curb future pandemics. When considering the psychological impact on HCPs and frontline staff, it is crucial for novel psychological interventions to become more adaptable for use in digital platforms such as virtual and augmented reality (VR/AR) [[60], [61], [62], [63]] for ease of access by a busy clinical workforce. With serious workforce shortages currently in global MH services in particular, further resource losses should be prevented. Therefore, the findings from this review should inform policy, training and service development and implementation to move towards a more integrated care model.
To our knowledge, this is the first systematic review and meta-analysis to examine the psychosocial and MH impact taking into consideration, physical symptomatologies as well across 3 cohorts. The number of studies that met the eligibility criteria for inclusion into the meta-analysis was relatively low, although a total of 103,097 subjects were involved in the current review. This does provide a much higher N and demonstrates a statistical significance prompting a call for further longitudinal research to be conducted. We conducted a thorough literature search in several databases, and the results of the current systematic review reinforce the high relevance and importance of considering MH outcomes across various cohorts when developing clinical and public health measures. The extraction of information from each study adhered to the refinement protocol, with this current review being the only study thus far during the pandemic to utilize such a method.
This review does not come without certain limitations. Firstly, all the quantitative studies included were cross-sectional with very limited follow-up, if any. Due to the cross-sectional nature of the included studies, there would only be a limited comparison of results. In addition, the studies included within the current review use a variety of instruments to measure the psychological impact of COVID-19 on specified variables (e.g. depression and anxiety, among others). None of the studies conducted in-person surveys and standardized clinical interviews to diagnose participants; therefore, there remains a question whether subjects had sub-threshold symptomatologies and/or clinically diagnosed disorders. A variety of instruments were used to measure anxiety and depression among the public, whereas among HCPs, anxiety was mainly measured using GAD-7 and PHQ-9 was used for depression. This could be a factor in the differences seen in the prevalence estimates between these populations. We were also limited by the number of studies that could be included in the subgroup analysis. Moreover, the variation in countries where the studies were conducted was limited. Due to the outbreak of COVID-19 being observed first in China, 48% of the studies include originated from there. Also, with the inclusion of studies solely written in the English language, this may have introduced further publication bias. Another limitation is that due to the inability to synthesize evidence from studies that reported mental health outcomes among COVID-19 patients, comparisons were not possible between the outcomes among patients and healthcare professionals and the public. Finally, even though we conducted sensitivity analyses to examine sources of heterogeneity by age, country, outcome measurement tool, study quality, and after removal of studies in which prevalence was computed using simulations of reported mean/median and SD/IQR we found insufficient evidence to explain this high heterogeneity. The only exceptions being age as a significant predictor of heterogeneity for depression among the public and study quality for anxiety among healthcare professionals. A possible reason for the high heterogeneity is that these estimates are for healthcare professionals as a whole and the general public in total. However, healthcare professionals consist of a group of individuals from different professions and occupations. Similarly, members from the public are comprised of individuals from different backgrounds, living and working in different environments, and having a wide range of physical, mental, and emotional health. Additionally, there may be methodological differences between the studies that we were unable to investigate. Though we used random effects models to pool the estimates of prevalence the presence of such high heterogeneity indicates that the results from the meta-analysis should be interpreted with caution.
The direct and indirect psychosocial impact of the Covid-19 pandemic is evident and could have long-term effects, more so in light of long COVID [64]. Whilst the prevalence of the MH symptomatologies and their exacerbation enforces a MH impact, these could be different in various sub-groups and there could be underlying mechanistic triggered responses as a result of exposure to the direct and indirect effects of COVID-19 may including adverse effects on brain function as suggested by Holmes and colleagues [65]. The requirement for distinguishing the difference between symptomatologies and diagnosed conditions should be considered as a priority for future research conducted to determine the MH impact due to COVID-19. The requirement for distinguishing the difference between symptomatologies and diagnosed conditions should be considered at the time of designing the study and reporting the results as well as the publication stage by all parties involved. Given the significant impact of COVID on Black, Asian Minority Ethnic (BAME) groups [66], studies exploring role of ethnicity are warranted. Additionally, core outcome-based reporting methods should be considered by researchers as this would aid in interpreting the data in a unified manner in the future. Furthermore, researchers, funders and policy makers should deploy studies to evaluate the psychosocial and neuroscientific effects of the pandemic using longitudinal studies to mobilize better infrastructure to manage infection and lockdown for healthcare professionals, patients and the general public. Whilst it is important to propose frameworks and policies for prioritization of developing this research further, it is vital to have multidisciplinary approaches to effectively address the ongoing and future mental healthcare needs of the global population.
Declaration of Competing Interest
PP has received research grant from Novo Nordisk, and other, educational from Queen Mary University of London, other from John Wiley & Sons, other from Otsuka, outside the submitted work. SR reports other from Janssen, Lundbeck and Otsuka outside the submitted work. All other authors report no conflict of interest.
The views expressed are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or the Academic institutions.
Acknowledgments
Data sharing statement
The authors declare that the data collected was gathered from publicly available studies and is available upon reasonable request. Request should be made to the corresponding author
Funding
KE, GD, and PP are supported by National Institute for Health Research (NIHR) Research Capability Funding (RCF) and by Southern Health NHS Foundation Trust and Oxford Brain Health Clinical Trials Unit. All of the study sponsors had no further role in the study design, data collection, analysis and interpretation of data; in the writing of the report and in the decision to submit the paper for publication
Contribution of each author
PP and GD developed study design and wrote the first draft of the manuscript. KE, TT, GD and SA-Y conducted database searches and study selection and data extraction. RR performed statistical analyses and contributed to the results’ section. GD, RR, KE, VR, TT, SR, DK, SWC, OWW, EKW, SSC, NS, NH, SA-Y and PP critically reviewed and revised the manuscript. All authors approved the final version of the manuscript.
Acknowledgements
The authors acknowledge support from Southern Health NHS Foundation Trust and Oxford Brain Health Clinical Trials Unit.
This paper is part of the multifaceted EPIC project that is sponsored by Southern Health NHS Foundation Trust and in collaboration with the University of Oxford's Oxford Brain Health Clinical Trials Unit and The Chinese University of Hong Kong.
We would like to acknowledge Dr Mustafa Soomro for his contribution and valuable comments to the SR protocol.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.100806.
Appendix. Supplementary materials
References
- 1.Cenat J.M., Blais-Rochette C., Kokou-Kpolou K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Dalexis R.D., Goulet M.A., Labell P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;295(113599) doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rathod S., Pallikadavath S., Young A.H., Graves L., Rahman M.M., Brooks A., Soomro M., Rathod P., Phiri P. Psychological impact of COVID-19 pandemic: protocol and results of first three weeks from an international cross-section survey – focus on health professionals. J Affect Disord Rep. 2020 doi: 10.1016/j.jadr.2020.100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Health Service . NHS Survey Coordination Centre; Oxford: 2019. NHS staff survey results. [Google Scholar]
- 4.British Medical Association. (2020) COVID-19: analyzing the impact of coronavirus on doctors. https://www.bma.org.uk/advice-and-support/covid-19/what-the-bma-is-doing/covid-19-analysing-the-impact-of-coronavirus-on-doctors
- 5.Wu P., Fang Y., Guan Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2013;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phiri P., Rathod S., Elliot K., Delanerolle G. The Impact of COVID-19 on the mental wellbeing of healthcare staff. EJPMR. 2020;7(8):66–71. [Google Scholar]
- 7.Marshall R.D., Galea S., Kilpatrick D. Psychaitric consequences of September 11. JAMA. 2002;288(21):2683–2684. doi: 10.1001/jama.288.21.2683-jlt1204-1-3. [DOI] [PubMed] [Google Scholar]
- 8.Marshall R.D., Bryant R.A., Amsel L., Suh E.J., Cook J.M., Neria Y. The psychology of ongoing threat: relative risk appraisal, the September 11 attacks, and terrorism-related fears. Am Psychol. 2007;62(4):304–316. doi: 10.1037/0003-066X.62.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neira Y., DiGrande L., Adams B.G. Posttraumatic stress disorder following the September 11, 2001, terrorist attacks. Am Psychol. 2011;66(6):429–446. doi: 10.1037/a0024791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang H.J., Nan J., Lv Z.Y., Yang J. Psychological impacts of the COVID-19 epidemic on Chinese people: exposure, post-traumatic stress symptoms, and emotion regulation. Asian Pac J Trop Med. 2020;13(6):252–259. [Google Scholar]
- 11.Steardo L., Steardo L., Zorec R., Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol. 2020;229(3):e13473. doi: 10.1111/apha.13473. (Oxf) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin Immunol. 2020;215 doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G., Wang C. A trial of lopinavir-ritonavir in adults hospitalized with severe COVID-19. N Engl J Med. 2020;382(19):1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gautret P., Lagier J.C., Parola P., Hoang V.T., Meddeb L., Mailhe M., Raoult D. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Horby P.W., Landray M.J. Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomized, controlled, open-label, platform trial. Lancet. 2020;396:1345–1352. doi: 10.1016/S0140-6736(20)32013-4. October 5, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO Coronavirus Disease (COVID-19) Dashboard. Retrieved from https://covid19.who.int/ 2020
- 18.Wells G., Shea B., O'Connel D., Peterson J., Welch V., Loso M., Tugwell P. Ottawa Hospital Research Institute; Ottawa, ON, Canada: 2000. The newcastle-ottawa scale (Nos) for assessing the quality of nonrandomised studies in meta-analyses. [Google Scholar]
- 19.Modesti P.A., Reboldi G., Cappuccio F.P., Agyemang C., Remuzzi G., Rapi S., Perruolo E., Parati G., ESH Working Group on CV Risk in Low Resource Settings Panethnic differences in bloody pressure in Europe: a systematic review and meta-analysis. PLoS ONE. 2016;11(1) doi: 10.1371/journal.pone.0147601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(13) doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins J.P.T., Thompson S.G., Deeks J.J. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang H., Qin S., Zhang L., Feng Z., Fan C. A psychological investigation of coronavirus disease 2019 (COVID-19) patients in mobile cabin hospitals in Wuhan. Ann Transl Med. 2020;8(15):941. doi: 10.21037/atm-20-4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamm M.E., Brown P.J., Karp J.F., Lenard E., Cameron F., Dawdani A., Lavretsky H., Miller J.P., Mulsant B.H., Pham V.Y.T., Reynolds C.F., Roose S.P., Lenze E.J. Experiences of American older adults with pre-existing depression during the beginnings of the COVID-19 pandemic: a multicity, mixed-methods study. Am J Geriatr Psychiatry. 2020;28(9):924–932. doi: 10.1016/j.jagp.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muruganandam P., Neelamegam S., Menon V., Alexander J., Chaturvedi S.K. COVID-19 and severe mental illness: impact on patients and its relation with their awareness about COVID-19. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med Sci Monit Int Med J Exp Clin Res. 2020;26 doi: 10.12659/MSM.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mamun M.A., Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? – the forthcoming economic challenges for a developing country. Brain Behav Immun. 2020;87:163–166. doi: 10.1016/j.bbi.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Griffiths M.D., Mamun M.A. COVID-19 suicidal behaviour among couples and suicide pacts: case study evidence from press reports. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhuiyan A., Sakib N., Pakpour A.H., Griffiths M.D., Mamun M.A. COVID-19-related suicides in Bangladesh due to lockdown and economic factors: case study evidence from media reports. Int J Ment Health Addict. 2020:1–6. doi: 10.1007/s11469-020-00307-y. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferrando S.J., Klepacz L., Lunch S., Tavakkoli M., Dornbush R., Baharani R., Smolin Y., Bartell A. COVID-19 Psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? Psychosomatics. 2020;61(5):551–555. doi: 10.1016/j.psym.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8(45) doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatric Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Rasoulpoor S., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xiong J., Lipsitz O., Nasri F., Lui L., Gill H., Pphan L., Chen-Li D., lacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheraton M., Deo N., Dutt T., Surani S., Hall-Flavin D., Kashyap R. Psychological effects of the COVID-19 pandemic on healthcare workers globally: a systematic review. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singap. 2020;49:155–160. http://www.ncbi.nlm.nih.gov/pubmed/32200399 pmid. [PubMed] [Google Scholar]
- 37.Ali S., Maguire S., Marks E., Doyle M., Sheehy C. Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the South-East of Ireland: an observational cohort multicenter study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J., Zhang Z. Mental health care for medical staff in China During the COVID-19 outbreak. Lancet. 2020;7(4) doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.UKRI. (2020). Apps to help distancing and NHS staff. Available: https://www.ukri.org/our-work/tackling-the-impact-of-covid-19/addressing-technological-challenges/apps-to-help-distancing-and-nhs-staff/. Last accessed 23rd Feb 2021
- 40.Rodriguez, A. (2020). Sleepio might be just what the professor ordered. Available: https://medicalxpress.com/news/2020-10-sleepio-professor.html. Last accessed 23rd Feb 2021
- 41.Lee S.M., Kang W.S., Cho A.-.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tam C.W.C., Pang E.P.F., Lam L.C.W., Chiu H.F.K. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34:1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- 43.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chong M.Y., Wang W.C., Hsieh W.C. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- 45.Bienvenu O.J., Colantuoni E., Mendez-Tellez P.A., Shanholtz C., Dennison-Himmelfarb C.R., Pronovost P.J., Needham D.M. Co-occurrence of and remission from general anxiety, depression, and posttraumatic stress disorder symptoms after acute lung injury: a 2-year longitudinal study. Crit Care Med. 2015;43(3):642–653. doi: 10.1097/CCM.0000000000000752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bäuerle A., Teufel M., Musche V., Weismüller B., Kohler H., Hetkamp M., Dörrie N., Schweda A., Skoda E.M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health. 2020:fdaa106. doi: 10.1093/pubmed/fdaa106. (Bangkok) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Rheenen T.E., Meyer D., Neill E. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: initial results from the COLLATE project [published online ahead of print. J Affect Disord. 2020;2020(275):69–77. doi: 10.1016/j.jad.2020.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Altman M.T., Knauert M.P., Pisani M.A. Sleep disturbance after hospitalization and critical illness: a systematic review. Ann Am Thorac Soc. 2017;14(9):1457–1468. doi: 10.1513/AnnalsATS.201702-148SR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Davide P., Andrea P., Martina O., Andrea E., Davide D., Mario A. The impact of the COVID-19 pandemic on patients with OCD: effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113213. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kozloff N., Mulsant B.H., Stergiopoulos V., Voineskos A.N. The COVID-19 global pandemic: implications for people with schizophrenia and related disorders. Schizophr Bull. 2020;46(4):752–757. doi: 10.1093/schbul/sbaa051. VolumeIssuePages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hulsbosch A.M., Nugter M.A., Tamis P., Kroon H. Videoconferencing in a mental health service in the Netherlands: a randomized controlled trial on patient satisfaction and clinical outcomes for outpatients with severe mental illness. J Telemed Telecare. 2017;23(5):513–520. doi: 10.1177/1357633X16650096. [DOI] [PubMed] [Google Scholar]
- 52.Thiyagarajan A., Grant C., Griffiths F., Atherton H. Exploring patients' and clinicians' experiences of video consultations in primary care: a systematic scoping review. BJGP Open. 2020;4(1) doi: 10.3399/bjgpopen20×101020. bjgpopen20×101020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.D'Arcey J., Collaton J., Kozloff N., Voineskos A.N., Kidd S.A., Foussias G. The use of text messaging to improve clinical engagement for individuals with psychosis: systematic review. JMIR Ment Health. 2020;7(4):e16993. doi: 10.2196/16993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.England.nhs.uk. (2020). Aftercare needs of inpatients recovering from COVID-19. Retrieved from https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/06/C0705-aftercare-needs-of-inpatients-recovering-from-covid-19-aug-2020.pdf
- 55.NHS. (2019). The NHS long term plan. Available:https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf. [Last accessed: 25th Feb 2021]
- 56.Greenberg P.E., Fournier A.A., Sisitsky T., Pike C.T., Kessler R.C. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) J Clin Psychiatry. 2015;76(2):155–162. doi: 10.4088/JCP.14m09298. [DOI] [PubMed] [Google Scholar]
- 57.Chesney E., Goodwin G.M., Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13(2):153–160. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Palylyk-Colwell E., Argaez C. CADTH; (CADTH Rapid Response Report: Summary with Critical Appraisal); Ottawa: 2018. Telehealth for the assessment and treatment of depression, post-traumatic stress disorder, and anxiety: clinical evidence. [PubMed] [Google Scholar]
- 59.Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlof E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn Behav Ther. 2018;47(1):1–18. doi: 10.1080/16506073.2017.1401115. [DOI] [PubMed] [Google Scholar]
- 60.Judd T., Aquilina A.L., Hunter I. Virtual reality medical training: a non-inferiority randomized controlled trial of VR vs face-to-face training. J Med Educ Train. 2020;4:044. [Google Scholar]
- 61.Shiban Y., Schelhorn I., Pauli P., Muhlberger A. Effect of combined multiple contexts and multiple stimuli exposure in spider phobia: a randomized clinical trial in virtual reality. Behav Res Ther. 2015;71:45–53. doi: 10.1016/j.brat.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 62.Didehbani N., Allen T., Kandalaft M., Krawczyk D., Chapman S. Virtual reality social cognition training for children with high functioning autism. Comput Hum Behav. 2016;62:703–711. doi: 10.1007/s10803-012-1544-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saposnik G., Redelmeier D., Ruff C.C., Tobler P.N. Cogntive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak. 2016;16(138) doi: 10.1186/s12911-016-0377-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Iqbal S.Z., Li B., Onigu-Otito E., Naqvi M.F., Shah A.A. The long-term mental health effects of COVID-19. Psychiatr Ann. 2020;50(12):522–525. doi: 10.3928/00485713-20201103-01. [DOI] [Google Scholar]
- 65.Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przbylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Phiri P., Delanerolle G., Al-Sudani A., Rathod S. COVID-19 and black, Asian, and minority ethnic communities: a complex relationship without just cause. JMIR. 2020;7(2) doi: 10.2196/22581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Delanerolle G., Phiri P., Soomro M., Raymont V., Elliot K., Rathod S. A systematic review of evaluating the psychosocial impact of the COVID-19 pandemic on patients, general public and mental healthcare professionals. PROSPERO. 2020:1–7. CRD42020181481 Available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020181481. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.