Abstract
We report that a case of adult testicular granulosa cell tumor in a 40-year-old man who presented with a palpable testicular mass. The sectioned surface of the testis revealed a well-circumscribed, yellowish tan, solid mass with hemorrhagic foci. Histologically, the tumor was arranged in solid nests, trabeculae, gyriform, pseudopapillae and macro-and microfollicles in a fibrocollagenous stroma. The tumor cells were ovoid or carrot-shaped with scant cytoplasm and nuclear grooves. Immunohistochemically, the tumor cells were diffusely strongly positive for estrogen receptor, progesterone receptor, androgen receptor, CD10, CD56, calretinin and vimentin, and multifocally positive for inhibin, synaptophysin and cytokeratin.
Keywords: Adult granulosa cell tumor, Testis, Immunohistochemistry
Highlights
-
•
Testicular adult- type granulosa cell tumor (GCT) is extremely rare.
-
•
The immunohistochemistry for vimentin, inhibin and calretinin is consistently positive in testicular adult GCT.
-
•
The immunopositivity for estrogen receptor, progesterone receptor, androgen receptor, CD10 and CD56 is a characteristic of testicular adult GCT.
Introduction
Testicular granulosa cell tumor (GCT) is a rare neoplasm composed of sex cord cells resembling granulosa cells of the ovary.1 Similar to more common their ovarian counterpart, testicular GCTs are divided into juvenile and adult types based on clinical and histological characteristics.2 Almost all juvenile type GCT of the testis occurs in infancy and is exclusively benign, whereas adult type GCT of the testis occurs over a wide age range with a mean age of 40 years and can show metastatic disease.2 Herein, we report a case of adult-type GCT of the testis.
Case report
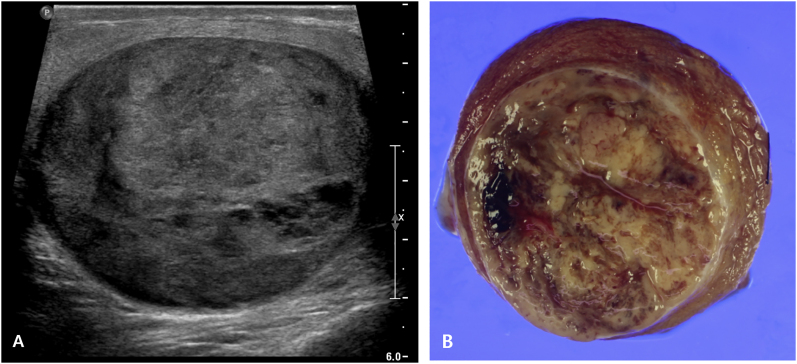
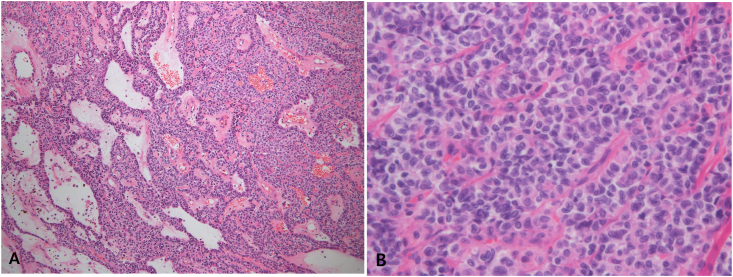
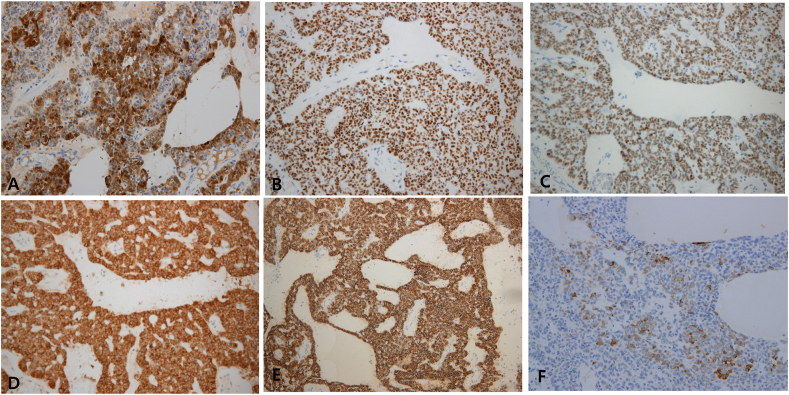
A 40-year-old man presented with a palpable testicular mass without scrotal pain. The mass was incidentally detected at the time of having vasectomy 5 years ago and has been enlarged slowly. The patient had no specific past medical history. He has had no estrogenic manifestation such as gynecomastia. Laboratory workup revealed no abnormal results. Especially, the germ cell tumor markers including alpha fetoprotein, human chorionic gonadotropin and lactate dehydrogenase were within normal limit. Ultrasonography of scrotum showed a 6.0-cm well-circumscribed heterogeneously hypoechoic mass with bulging contour and small cystic changes in right testis and no abnormal findings in left testis (Fig. 1A). Color-Doppler ultrasound showed increased vascularity in the mass. Computed tomography of scrotum showed a 6.0-cm circumscribed oval heterogeneously enhancing solid mass in right scrotum. There was no evidence of distant metastasis or significantly enlarged lymph node in the abdomen and pelvic cavity. Radiological impression was malignant germ cell tumor. The patient underwent radical orchiectomy. The sectioned surface of the testis revealed a well-circumscribed, lobulated, heterogeneous, yellowish tan, solid mass with focal hemorrhage (Fig. 1B). Histopathologically, the tumor was arranged in solid nests, trabeculae, gyriform, pseudopapillae, and macro-and microfollicles in a fibrocollagenous and edematous stroma (Fig. 2A). Multifocal hemorrhagic foci with abundant hemosiderin-laden macrophages were observed within the tumor. The tumor was composed of relatively uniform ovoid or carrot-shaped cells with scant cytoplasm and angular nuclei with grooves (Fig. 2B). Mitotic figures were numbered up to 3/10 high power fields and no abnormal mitoses were seen. Neither significant nuclear atypia nor lymphovascular invasion was detected. Leydig cell component was not found within the tumor. The non-neoplastic testicular tissue showed normal spermatogenesis. Immunohistochemically, tumor cells were diffusely strongly positive for calretinin(Fig. 3A), estrogen receptor (ER) (Fig. 3B), progesterone receptor (PR), androgen receptor (AR) (Fig. 3C), CD10 (Fig. 3D), CD56 (Fig. 3E) and vimentin; multifocally positive for inhibin (Fig. 3F), synaptophysin, cytokeratin, c-kit and cyclin D1; very focally positive for WT1 protein; negative for epithelial membrane antigen (EMA), S100 protein, chromogranin, placental alkaline phosphatase (PLAP), smooth muscle actin, glypican 3, alpha fetoprotein, CD99, GATA3, PAX8, SALL4 and MART-1. Nuclear beta-catenin expression was absent. Ki67- labelling index was about 2%. Thus, the tumor was diagnosed as adult GCT. His postoperative course was uneventful. The patient is doing well 18 months after surgery.
Fig. 1.
A. Gray-scale ultrasonography shows a well-defined oval hypoechoic solid mass with small cystic changes in the testis. B. The sectioned surface of the testis reveals a well-circumscribed, lobulated, heterogeneous, yellowish tan, solid mass with focal hemorrhage.
Fig. 2.
A. Microscopically, the tumor is arranged in solid nests, trabeculae, gyriform, pseudopapillary, and macro-and microfollicles in a fibrocollagenous and edematous stroma. B. Higher magnification of tumor cells shows uniform round or carrot-shaped cells with angular nuclei and nuclear grooves.
Fig. 3.
Immunohistochemical staining reveals diffuse strong positivity for calretinin (A), estrogen receptor (B), androgen receptor (C), CD10 (D) and CD56 (E). Inhibin shows patchy positivity (F).
Discussion
Adult testicular GCT is an extremely rare and has been reported in single case reports or a few small case series.2, 3, 4 This tumor is characterized by typical morphologies of tumor cells showing granulosa cell differentiation.1,2 Tumor cells have their coffee-bean like, angulated and grooved nuclei and are arranged in diffuse, insular, spindled, microfollicular (Call-Exner bodies), trabecular, corded, watered-silk, palisading, and pseudopapillary growth patterns.1,2 Histologically adult testicular GCT can be distinguished from other types of testicular sex cord-stromal tumor. Leydig cell tumor shows a diffuse pattern of tumor cells with abundant eosinophilic cytoplasm, round nuclei and prominent nucleoli.1 Sertoli cell tumor shows prominent tubular differentiation and polygonal tumor cells with abundant pale cytoplasm.1
A recently published systematic review article2 describes 239 patients with testicular GCT. According to this review, the majority of the cases have juvenile testicular GCT (166/239, 69%), while 73/239 (31%) patients have adult testicular GCT. Juvenile testicular GCTs represent a benign entity whereas adult testicular GCTs have metastatic potential.2,4 Due to the few cases reported, the risk factors and treatment outcomes of adult testicular GCTs are poorly understood.2 According to the systematic review,2 tumor size, presence of angiolymphatic invasion or gynecomastia represent risk factors for metastatic disease. In the metastatic setting, aggressive surgical and systemic treatment might cure patients.2
Immunohistochemistry is helpful to lead a more accurate diagnosis of adult testicular GCT.2, 3, 4 Negative stainings for germ cell tumor markers such as PLAP, AFP, glypican-3 and SALL4 are useful to rule out more common germ cell tumors.1 The most frequently reported immunohistochemistry includes vimentin, inhibin and calretinin which are consistently positive for adult testicular GCT.2, 3, 4 The immunohistochemical studies with other antibodies are not frequent in adult testicular GCT and their results are variable. Tanner et al.3 demonstrated c-kit-positivity and our case showed patchy weak positivity for c-kit partially supporting the previous report. CD99-positivity has been reported4 but our case failed to demonstrated CD99-positivity. In our case diffuse and strong positivity for ER, PR, AR, CD10 and CD56 was truly remarkable and supports that these immunohistochemical markers may be also very useful to the diagnosis of adult testicular GCT. CD56 is a sensitive and diagnostically useful immunohistochemical marker of ovarian sex cord-stromal tumors5 but immunoreactivity for CD56 in the adult testicular GCT has not been reported so far. To the best of our knowledge, this case is the first to demonstrate the immunoreactivity for CD10 and CD56 in the adult testicular GCT.
Conclusion
Adult testicular GCT is extremely rare. This report adds to the clinicopathologic data regarding this tumor and suggests that the immunopositivity for ER, PR, AR, CD10 and CD56 may be helpful in distinguishing this tumor from other testicular tumors.
Declaration of competing interest
The authors declare that they have no conflicts of interest.
References
- 1.Young R.H. Sex cord-stromal tumors of the ovary and testis: their similarities and differences with consideration of selected problems. Mod Pathol. 2005 Feb;18(Suppl 2):S81–S98. doi: 10.1038/modpathol.3800311. PMID: 15502809. [DOI] [PubMed] [Google Scholar]
- 2.Grogg J.B., Schneider K., Bode P.K. Risk factors and treatment outcomes of 239 patients with testicular granulosa cell tumors: a systematic review of published case series data. J Canc Res Clin Oncol. 2020 Nov;146(11):2829–2841. doi: 10.1007/s00432-020-03326-3. Epub 2020 Jul 27. PMID: 32719989; PMCID: PMC7519920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanner S.B., Morilla D.B., Schaber J.D. A case of adult granulosa cell tumor of the testis. Am J Case Rep. 2014 Oct 30;15:471–475. doi: 10.12659/AJCR.891389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schubert T.E., Stoehr R., Hartmann A., Schöne S., Löbelenz M., Mikuz G. Adult type granulosa cell tumor of the testis with a heterologous sarcomatous component: case report and review of the literature. Diagn Pathol. 2014 Jun 3;9:107. doi: 10.1186/1746-1596-9-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCluggage W.G., McKenna M., McBride H.A. CD56 is a sensitive and diagnostically useful immunohistochemical marker of ovarian sex cord-stromal tumors. Int J Gynecol Pathol. 2007 Jul;26(3):322–327. doi: 10.1097/01.pgp.0000236947.59463.87. PMID: 17581419. [DOI] [PubMed] [Google Scholar]