Abstract
Although antihypertensive medications are effective, inexpensive, and recommended by clinical practice guidelines, a large percentage of older adults with hypertension have uncontrolled blood pressure (BP). Improving BP control in this population may require a better understanding of the specific challenges to BP control at older age. In this narrative review, we propose a framework for considering how key steps in BP management occur in the context of aging characterized by heterogeneity in function, multiple co-occurring health conditions, and complex personal and environmental factors. We review existing literature related to 4 necessary steps in hypertension control. These steps include the BP measure which can be affected by the technique, device, and setting in which BP is measured. Ensuring proper technique can be challenging in routine care. The plan includes setting BP treatment goals. Lower BP goals may be appropriate for many older adults. However, plans must take into account the generalizability of existing evidence, as well as patient and family’s health goals. Treatment includes the management strategy, the expected benefits, and potential risks of treatment. Treatment intensification is commonly needed and can contribute to polypharmacy in older adults. Lastly, monitor refers to the need for ongoing follow-up to support a patient’s ability to sustain BP control over time. Sustained BP control has been shown to be associated with a lower rate of cardiovascular disease and multimorbidity progression. Implementation of current guidelines in populations of older adults may be improved when specific challenges to BP measurement, planning, treating, and monitoring are addressed.
Keywords: blood pressure, blood pressure control, hypertension, older adults
The prevalence of hypertension and the incidence of hypertension-related cardiovascular disease (CVD) increase with older age, making blood pressure (BP) control among older adults an important population health goal.1,2 Although antihypertensive medications are effective, inexpensive, and recommended by clinical practice guidelines, a large percentage of older adults with hypertension have uncontrolled BP.3,4 This may be due in part to several factors. For older adults, BP management occurs in the context of aging characterized by heterogeneity in function, multiple co-occurring health conditions, as well as an often complex set of personal and environmental factors.5–7 In addition to issues related to aging, there are also specific considerations for measuring and treating hypertension in older age.8
In this article, we first review hypertension prevalence, treatment, and control in older adults highlighting current clinical practice guideline definitions and their implications for identifying hypertension in older adults. Next we describe the unique considerations for controlling hypertension at older ages and propose a framework for BP management in this population. This framework considers the aging context as well as the specific steps in hypertension management. Based on this framework, we then review the existing literature as it relates to 4 necessary steps in hypertension control: (i) measuring BP, (ii) planning and goal setting, (iii) treating hypertension, and (iv) monitoring BP over time. Lastly, we use this framework to guide a discussion on implementation challenges and opportunities for improving care for older adults with hypertension.
EPIDEMIOLOGY
Guideline definitions and treatment goals
The 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults classifies BP into 1 of 4 categories: Normal, Elevated, Stage 1, and Stage 2.4 The guideline defines normal BP as systolic BP (SBP) <120 mm Hg and diastolic BP (DBP) <80 mm Hg. Elevated BP is defined as SBP 120–129 mm Hg and DBP <80 mm Hg. Stage 1 hypertension is defined as SBP 130–139 mm Hg or DBP 80–89 mm Hg and Stage 2 hypertension is defined as SBP ≥140 mm Hg or DBP ≥90 mm Hg. These categories replace the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) classification, adding the new category Elevated BP, eliminating the prehypertension category, and lowering the BP levels for defining Stage 1 hypertension.4,9 Furthermore, these BP categories are the same for all adults, including the oldest-old.
New to these guidelines are also recommendations for thresholds to initiate BP-lowering medications and BP goals based on CVD risk. Among patients with clinical CVD, guidelines recommend treatment for secondary prevention of CVD events with a BP goal <130 mm Hg/<80 mm Hg. For primary prevention among those without known CVD, guidelines recommend first estimating the 10-year atherosclerotic cardiovascular disease risk. BP-lowering medications are recommended for goal BP levels of <130 mm Hg/<80 mm Hg for patients with an atherosclerotic cardiovascular disease risk of >10%. As 88% of adults over 65 years and 100% of those over 75 years old have an atherosclerotic cardiovascular disease risk of ≥10%, the recommended BP goal for the vast majority of older adults is <130 mm Hg/<80 mm Hg.4 In addition to antihypertensive medication to achieve these goals, the 2017 ACC/AHA guidelines also recommend nonpharmacological interventions including weight loss among those overweight or obese, a heart-healthy diet, sodium restriction, increased physical activity, and reduction in alcohol consumption. These treatment recommendations are the same for adults of all ages.
Prevalence, treatment, and control
The prevalence of hypertension increases with age. Most epidemiologic studies have used BP ≥140/90 mm Hg to define hypertension. For example, according to an analysis of data from the National Health and Nutrition Examination Survey (NHANES) conducted between 2011 and 2014, the prevalence of hypertension was 10.5%, 29.5%, 52.4%, 63.6%, and 75.1%, among US adults 20–44, 45–54, 55–64, 65–74, and ≥75 years old, respectively.1 Applying the 2017 ACC/AHA guideline definition of hypertension as BP ≥130/80 mm Hg classified a higher percentage of US adults as having hypertension (45.6% and 31.9% for 2017 ACC/AHA and JNC7, respectively). However, among those 75 years old and older, the difference in those meeting the definition of hypertension (82.3% vs. 75.1%) or who would receive recommendations for antihypertensive medications (82.3% vs. 78.5%) were small. In the general US population, gender differences in the prevalence of hypertension have also been reported with a higher percentage of men compared with women meeting the definition for hypertension. However, after age 65 years the prevalence of hypertension is higher among women than men.2
The percentage of older adults with awareness of hypertension and receiving treatment are generally high. Awareness of hypertension, defined as BP ≥140/90 mm Hg has been shown to be 67.3%, 79.3%, 85.4%, and 82.1% among US adults 18–44, 45–64, 65–74, and ≥75 years old, respectively.3 Hypertension awareness has been shown to be more common among those with a usual health care provider, which may explain in part the higher prevalence of awareness at older ages as older adults often require more frequent interactions with the healthcare system. Among those aware they had hypertension, antihypertensive medication use has also been shown to be high among older adults. Among those who reported awareness, the percentage taking antihypertensive medication were 75.8%, 87.7%, 94.1%, and 96.0% at 18–44, 45–64, 65–74, and ≥75 years old.3
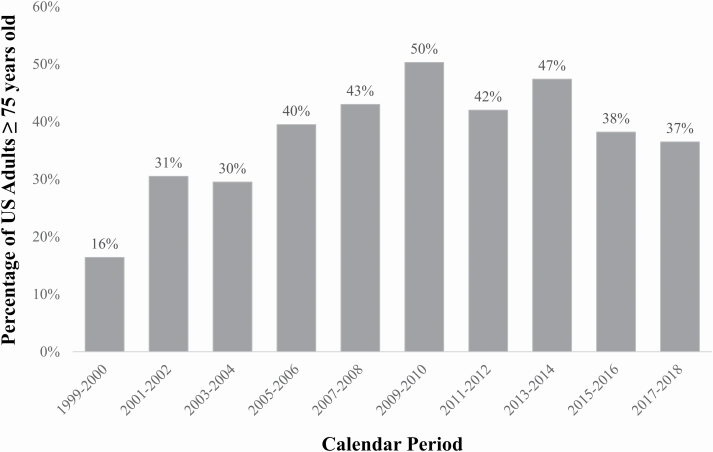
Among older adults with hypertension, the percentage with controlled BP has generally been reported to be less than 50%. A recent analysis reported trends in BP control using NHANES calendar periods across nearly 2 decades.3 Serial cross-sectional surveys took place over 2-year intervals from 1999–2000 through 2017–2018. Overall, an increasing percentage of adults with controlled BP was seen through 2013–2014, followed by a decrease in calendar periods 2015–2016 and 2017–2018. This trend was also seen among those ≥75 years old (Figure 1). In a pooled analysis from 2015 to 2018, the prevalence ratio for controlled BP among those taking antihypertensive medication was 0.96, 0.84, and 0.63 at ages 45–64, 65–74, and ≥75 years old, compared with 18–44 years old, respectively.3
Figure 1.
Trends in blood pressure (BP) control among US adults ≥75 years old from the National Health and Nutrition Examination Survey (NHANES).3
Most studies of hypertension have focused on community-dwelling older adults. Therefore, data on the prevalence, treatment, and control of hypertension among special populations of older adults such as the oldest-old or those residing in nursing homes are limited. One analysis of NHANES reported the prevalence among US adults ≥80 years old to be 76.5%, with similar percentage of those with control among those on hypertension medications to those ≥75 years old during the same time period.10 Importantly, a large increase in antihypertensive polypharmacy, defined as 3 or more classes of BP-lowering medications, was found over time. The percentage of US adults ≥80 years old with antihypertensive polypharmacy was 7.0%, 19.2%, and 30.9% during calendar NHANES assessments occurring in 1988–1994, 1999–2004, and 2005–2010, respectively.10 Data on the prevalence of hypertension among older nursing home residents are limited. Because of the high prevalence of multimorbidity in the nursing home population, the prevalence of hypertension in combination with other chronic conditions has been described. For example, 1 report showed that 27% of nursing home patients had co-occurring hypertension and dementia.11 A separate analysis of over 250,000 US nursing home residents with hypertension on antihypertensive medications found that 40% were receiving 2 or more classes of medication.12 The intensity of treatment did not differ for those with and without moderate–severe cognitive impairment, raising questions about whether hypertension is overtreated among some nursing home residents who have limited life expectancy.
BP control and disabling conditions
As many older adults prioritize remaining independent in late life, it is important to recognize the association between BP control and conditions that reduce cognitive and physical function. Uncontrolled BP is a known risk factor for disabling conditions including stroke, heart failure, and coronary heart disease.2 Studies have also shown direct associations of hypertension with cognitive and physical function.13 For example, BP ≥120/80 mm Hg during midlife was found to be associated with a greater risk of developing dementia in later life.14 Therefore, a life-course perspective is helpful for understanding the detrimental effects of uncontrolled BP that may accumulate over many years leading to disability.15
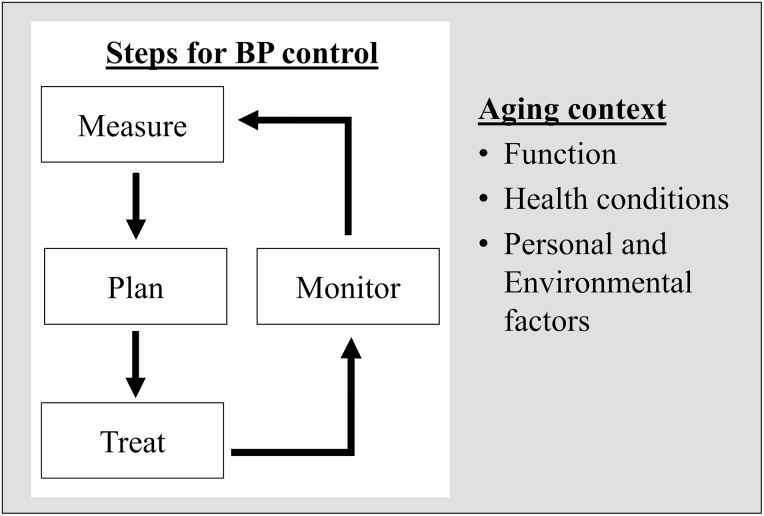
FRAMEWORK
The combination of an aging US population, a decreasing percentage with controlled hypertension, and recommendations for lower BP goals will likely result in an expanding population of older adults with uncontrolled BP who are at risk for CVD events. Population health efforts to improve BP control often focus on increasing awareness and treatment. However, awareness and treatment have remained high among older adults. An alternative approach may be to recognize specific challenges to BP control among older adults. We proposed a framework for considering how key steps in BP management occur in the context of common issues with aging (Figure 2).
Figure 2.
A framework to improve blood pressure (BP) control that considers how key steps in BP management occur in the context of common aging issues.
Aging context
A sizable proportion of older adults, including many who are frail, will benefit from intensive BP control, defined as a SBP <120 mm Hg. However, other older adults are unlikely to benefit. The World Health Organization (WHO) has developed a model that is useful for helping to identify those who may be less likely to derive benefit from intense efforts to control BP. The WHO International Classification of Functioning (ICF) model describes 4 aging domains: (i) function, (ii) health conditions (i.e., multimorbidity), (iii) personal factors, and (iv) environmental factors.5,16 This model considers the impact of functional limitations on daily activities such as chronic disease self-management tasks. The health conditions domain acknowledges that older adults often experience multiple chronic conditions.17,18 Examples of personal factors include individual health goals, personal financial resources, and availability of family caregivers. Examples of environmental factors include living situations such as independent living vs. nursing home residence, and geographic issues such as neighborhood-level poverty. While these considerations may be important regardless of age, the prevalence of functional limitations and complexity of health conditions are known to increase at older age.19 Consequently, some older adults rely on personal and environmental factors to maintain independence and manage their health conditions.20
The interaction of function, co-occurring health conditions, and personal and environmental factors are relevant to BP control. This is illustrated by considering the multiple self-management tasks necessary for BP control. Limitations with physical and cognitive function may reduce one’s capacity to follow physical activity recommendations, adhere to medication scheduling, and refill medications on-time.21 While some conditions have overlapping treatment goals with hypertension, reinforcing the need for treatment (e.g., angiotensin-converting enzyme inhibitor among those with hypertension, chronic kidney disease, and diabetes), the presence of multimorbidity often makes self-management more complex.22,23 Older adults may not receive guidance on how to reconcile opposing treatment recommendations.24 This may be especially true when older adults face choices about treating conditions that are symptomatic vs. those that are asymptomatic such as hypertension.25 The presence or absence of a family caregiver or resources to pay caregivers, can influence one’s ability to overcome functional and cognitive limitations.
In addition to impacts on ability to self-manage BP, functional limitations and multimorbidity may provide important prognostic information.26 For example, many older adults with poor function and advanced illness are at end-of-life. Those with a life expectancy of less than 2 years are unlikely to live long enough to experience the benefits of intensive BP treatment.27,28 Because of the wide range of functional abilities, health conditions, and personal and environmental resources in older age, a one-size-fits-all approach is unlikely to be effective for setting BP goals or controlling BP.
Steps in BP management
In addition to issues related to older age influencing BP control, there are specific components involved in achieving and sustaining BP control (Table 1). This framework acknowledges that the BP measure can be affected by the technique, device, and setting in which BP is measured. The plan refers to setting a goal BP in the context of the patient and family’s overall health goals. Treatment refers to the management strategy including the use of BP-lowering medications, the expected benefits of treatment, and risk for adverse events. Lastly, monitor refers to need for ongoing follow-up to support a patient’s ability to sustain BP control over time. Below we highlight some of the relevant literature for each of these 4 steps.
Table 1.
Description of steps in hypertension control and relevant considerations for older adults
| Description | Relevance to older adults | |
|---|---|---|
| Measure | Technique, device, setting | • Proper technique limited by physical and cognitive impairment or geriatric conditions • Competing demands for clinical assessments among older adults with multimorbidity (i.e., proper technique a low priority) • Higher prevalence of treated white coat hypertension at older age |
| Plan | Setting goals | • Concerns about generalizability of clinical trial evidence for some older adults • Wide range in health goals and willingness to accept tradeoffs between benefits and harms at older age |
| Treat | Management strategy, benefits vs. harms | • Treatment intensification likely to result in polypharmacy • Physical and cognitive impairment may limit self-management • Dependence on caregivers for self-management support • Falls are a common cause and death and disability in older adults. Fear of precipitating a fall may affect treatment decisions |
| Monitor | Follow-up over time | • Heterogeneity in life expectancy and time for which BP monitoring may be necessary • Intervening health events and declining function occur at older age and may affect BP control or treatment goals |
Abbreviation: BP, blood pressure.
Measure
Differences in BP measurement based on the technique and setting are common at all ages, but especially true in this population. The AHA Scientific Statement on Measurement of BP in Humans describes 6 overall steps and 20 specific instructions for the proper technique to obtain seated BP in the office.29 Large-scale studies have demonstrated that implementing the proper technique is feasible, however approaches used in clinical trials have not been widely adopted in practice. Clinic-level challenges include ensuring a 3- to 5-minute relaxation period, not talking to the patient during the measurement, as well as determining the proper cuff size. At the patient-level, challenges include removing clothing among those with functional limitations or arthritis, bladder emptying among those with prostate or bladder dysfunction, and following instructions for those with cognitive limitations. These challenges may explain the recent report showing higher SBP in the electronic health record compared with BP obtained under a standardized research protocol.30 Despite these challenges, there are several examples of how outpatient clinics can overcome clinic- and patient-level barriers to care (e.g., blood draws, laboratory calibration, crash cart maintenance) when standardized policies are put into place. This might also involve an expanded use of home blood pressure monitoring following AHA Scientific Statement recommendations for proper technique.29 While this approach may overcome the clinic-level deficiencies, some patient-level challenges remain. Concerns about device validation have also been reported.31
Research has shown differences based on the setting in which BP is measured, an important example being the higher prevalence of white coat hypertension with aging.8,32 One way to identify white coat hypertension is by using ambulatory blood pressure monitoring (ABPM). In ABPM, a BP monitor is worn for 24 hours and obtains automatic readings in the out-of-office setting.8 ABPM has been shown to have similarly feasible in older and younger adults.33 Using ABPM, white coat hypertension is defined as having elevated clinic BP without elevated daytime BP on ABPM. The term “treated white coat hypertension” has been used to describe elevated clinic BP without elevated daytime BP on ABPM among those on antihypertensive medications.8 Prior studies have shown that among older adults, clinic BP is higher in relationship to daytime BP resulting in a higher prevalence of treated white coat hypertension at older age. For example, an analysis of data from the Jackson Heart Study, compared the difference in clinic and daytime SBP among Black US adults with hypertension <60 vs. ≥60 years old.34 The difference between clinic SBP and daytime SBP was on average higher among those ≥60 years old compared with <60 years old (12 mm Hg higher vs. 8 mm Hg higher). The prevalence of white coat hypertension may be greater among special populations of adults. The prevalence of treated white coat hypertension among participants who were all 80 years and older in the HYVET study was 50%.35 Among nursing home residents, 1 study found that 70% of all nursing home residents with high BP were found to have white coat hypertension when ABPM was conducted.36 Taken together, these findings suggest that clinic BP obtained as part of routine care may not always reflect the out-of-clinic BP and should be considered when addressing BP control in older adults.
Plan
In the proposed framework, the plan refers to setting goals for BP control levels. As described above, the guideline recommended goal BP for the vast majority of older adults is <130 mm Hg/<80 mm Hg. This recommendation is supported by clinical trial evidence including findings from the Systolic Blood Pressure Intervention Trial (SPRINT) which tested intensive vs. standard control.27 While the results of SPRINT have been extensively reported,37 it is worth reviewing 3 findings that are relevant to older adults. First, among the prespecified subgroup of participants ≥75 years old, treating to an SBP goal of <120 mm Hg (intensive control) vs. <140 mm Hg (standard control) resulted in lower rates of fatal and nonfatal CVD events and death.28 This was true in exploratory subgroups in which participants were categorized as fit, less fit, or frail or had a low gait speed and among those ≥80 years old.38 Second, findings from SPRINT maybe generalizable to a large number of ambulatory older adults, including those with frailty. In SPRINT, 31% of participants ≥75 years old were frail, a similar prevalence seen in community-dwelling older adults.39 Third, findings from the SPRINT MIND study found a lower incidence of mild cognitive impairment and the combination of mild cognitive impairment or probable dementia with intensive SBP control.40 There was no difference seen in the primary outcome of probable dementia, perhaps due to the intervention being terminated early and inadequate follow-up time. However, because maintaining cognitive function is such an important goal in aging, findings of lower risk of mild cognitive impairment are clinically relevant for older adults.
While SPRINT is a landmark study and representative of a large percentage of older adults with hypertension, it is not possible for a randomized trial to be generalizable to all older adults. Therefore, it is important to consider the study exclusions most relevant to older adults when planning BP goals. For example, SPRINT excluded adults residing in nursing homes and those with standing hypotension of <110 mm Hg, type 2 diabetes, prior history of stroke, estimated glomerular filtration rate <20 ml/min/1.73 m2, dementia, unintentional weight loss, or symptomatic heart failure.27 As these conditions are common at older age and may be associated with risk for adverse events, it is not known if intensive SBP control would confer the same benefits for some subgroups of older adults. In addition to the exclusion criteria, it has been well documented that barriers exist to inclusion of older adults in research.41 For example, older adults with functional limitations and limited social support face additional barriers to participation even when not explicitly excluded, reinforcing the need to consider the aging context when making plans for BP treatment goals.41
Treat
After making plans for BP goals, the next step is to choose a management strategy. This includes both nonpharmacological interventions, such as low sodium diets and weight loss, as well as the use of BP-lowering medications. Several nonpharmacological interventions have additional benefits such as improvement of function and should be considered regardless of the need for antihypertensive medication. The clinician and patient should have an understanding of the expected benefits and potential for risk for adverse events when considering antihypertensive medication initiation or intensification. In general, guideline recommendations for specific antihypertensive medications do not differ by age.4 As the majority of older adults with hypertension are on treatment, treatment decisions less often focus on which antihypertensive medication to initiate, but more on when to intensify treatment by adding medications from other classes. For example, among adults ≥75 years old in SPRINT, 85% of participants in the intensive treatment group and 57% in the standard treatment group required 2 or more antihypertensive medication classes to achieve the targeted BP goals (mean number 2.6 vs. 1.8).28 The most commonly used antihypertensive medications for both randomization groups were angiotensin-converting enzyme inhibitors/ARBs followed by diuretics and calcium channel blockers. Therefore, in this population it is important to anticipate and manage polypharmacy, specifically antihypertensive polypharmacy, when treating hypertension.
Another aspect of treatment to consider is the risk for adverse events. Falls are leading cause of injury and death among older adults.42 Although concerns about fall risk likely lead to less intensive hypertension treatment, evidence on the association between hypertension treatment and falls is mixed. Clinical trials, including SPRINT, have not shown intensive BP treatment to be associated with a higher risk of injurious falls.27,43 However, rates of falls have been shown to be lower in trial populations than in observational studies.44,45 Among Medicare beneficiaries ≥70 years old with hypertension, antihypertensive medications use was shown to be associated with a higher risk of serious fall injuries.44 In a separate study of over 90,000 Medicare beneficiaries, antihypertensive medication initiation or intensification was associated with risk for serious fall injuries within 14 days, but not longer-term risk.46 In an analysis of data from the REasons for Geographic and Racial Differences in Stroke (REGARDS) study participants on antihypertensive medication, indicators of frailty, but not BP levels or number of antihypertensive medications, was shown to be associated with risk for serious fall injuries.47 These findings suggest that the risk for falls should not preclude hypertension treatment for most older adults, but careful titration, short-term monitoring, and addressing multiple fall risk factors should be part of comprehensive hypertension treatment.
Monitor
Population level reports on BP control provide a snapshot in time. However, in practice, clinicians diagnose and treat individuals with hypertension over many visits and patients live with hypertension over many years. Older adults often experience intermittent health events, many unrelated to hypertension, that may affect their ability to achieve BP control. Therefore, monitoring BP control over time with the goal of sustaining BP control is an important step in hypertension management. Recent studies have shown that sustained BP control is associated with better health outcomes.48 For example, an analysis of the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) linked to Medicare health insurance claims examined the association between sustained SBP control and the progression of multimorbidity, defined by the co-occurrence of up to 14 separate chronic conditions.49 SBP control was categorized as <140 mm Hg at <50%, 50% to <75%, 75% to <100%, and 100% of visits over a 48-month assessment period. Participants with sustained SBP control at a higher percentage of visits had a slower rate of multimorbidity progression and developed multimorbidity when they were 5–10 years older than their counterparts without sustained SBP control. As older adults often consider their overall health when assessing the risks and benefits of treatment, not just the disease-specific outcomes, evidence on reducing multimorbidity could be used to guide patient-centered discussions about monitoring and improving BP control over time.
Implementation needs
Understanding the unique challenges and opportunities for BP control in older adults may facilitate better implementation of hypertension guidelines in this population. In Table 2, we describe some differences between clinical trials and routine care related to measuring, planning, treating, and monitoring BP control among older adults. Recognizing these differences can be used to identify implementation opportunities. For example, in clinical trials, strict inclusion criteria are applied to populations to identify eligible participants before any plan for BP treatment is initiated. In clinical practice, identifying patients who might benefit is not done in a coordinated way. Therefore, implementation strategies that include risk stratification tools to identify patients for whom guideline recommended BP is appropriate are needed.
Table 2.
Identifying implementation opportunities that address differences in clinical trials and routine care
| Clinical trials | Routine care | Implementation opportunities | |
|---|---|---|---|
| Measure | • Standardized technique • Calibrated equipment • Certified research staff • Multiple measures • Routine orthostatic BP |
• Multiple techniques • Available equipment • Busy clinical staff • Single measure • Additional measures when clinically indicated/symptoms |
Develop practical approaches to BP measurement that can be achieved in busy clinic settings or accurately obtained outside of the clinic. |
| Plan | • Eligibility screening prior to enrollment • BP goals determined by protocol or randomization group |
• All comers • Provider variability in knowledge and comfort with guideline recommended goals • Variability in patient and family goals |
Use risk stratification tools to identify patients for whom guideline recommended BP is appropriate. Incorporate shared decision-making tools to help align patient goals with BP treatment goals. |
| Treat | • Determined by standardized protocols or by randomization group • Frequent assessment for study specific adverse events including minor events |
• Provider, patient, and clinic variability in drug choice and timing of initiation/intensification • Adverse events are multifactorial in etiology • Adverse events may not be identified unless they result in acute or emergent care |
Develop treatment protocols that address polypharmacy, drug–drug, and drug–condition interactions that are common among older adults with multimorbidity. Following existing guidelines for addressing multifactorial geriatric conditions such as falls. |
| Monitor | • Standard device and setting • Routine interval • Set study endpoint |
• Multiple devices and settings • As needed or when acute events occur • No endpoint |
Report meaningful metrics for sustained BP control that support patient–provider communication and quality improvement. Follow flexible monitoring schedules that respond to changes in BP control, acute health events, or health goals. |
Abbreviation: BP, blood pressure.
Despite effective and inexpensive treatments, clinical trial evidence on the benefits of treatment, and guideline recommendations, a large percentage of older adults do not have adequately controlled BP. A framework that recognizes both the broader aging context and the specific challenges and opportunities in BP management may be helpful for improving BP control. Implementation of current guidelines in populations of older adults may be improved when barriers to BP measurement, planning, treating, and monitoring are addressed.
FUNDING
Support was provided through the National Heart, Lung, and Blood Institute (R01HL133618) and the National Institute on Aging (R01AG062502) to C.B.B. This work was also supported by the Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) (CIN 13-410) at the Durham VA Health Care System. The views expressed here/in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the Department of Health and Human Services.
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1. Muntner P, Carey RM, Gidding S, Jones DW, Taler SJ, Wright JT Jr, Whelton PK. Potential US population impact of the 2017 ACC/AHA High Blood Pressure Guideline. Circulation 2018; 137:109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 2019; 139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 3. Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA 2020; 324:1190–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018; 138:e426–e483. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. Towards a Common Language for Functioning, Disability, and Health, ICF, The International Classification of Functioning, Disability and Health. World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- 6. Boyd C, Smith CD, Masoudi FA, Blaum CS, Dodson JA, Green AR, Kelley A, Matlock D, Ouellet J, Rich MW, Schoenborn NL, Tinetti ME. Decision making for older adults with multiple chronic conditions: executive summary for the American Geriatrics Society Guiding Principles on the Care of Older Adults With Multimorbidity. J Am Geriatr Soc 2019; 67:665–673. [DOI] [PubMed] [Google Scholar]
- 7. Tinetti ME, Fried T. The end of the disease era. Am J Med 2004; 116:179–185. [DOI] [PubMed] [Google Scholar]
- 8. Reynolds K, Bowling CB, Sim JJ, Sridharan L, Harrison TN, Shimbo D. The utility of ambulatory blood pressure monitoring for diagnosing white coat hypertension in older adults. Curr Hypertens Rep 2015; 17:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee . The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 10. Bromfield SG, Bowling CB, Tanner RM, Peralta CA, Odden MC, Oparil S, Muntner P. Trends in hypertension prevalence, awareness, treatment, and control among US adults 80 years and older, 1988–2010. J Clin Hypertens (Greenwich) 2014; 16:270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moore KL, Boscardin WJ, Steinman MA, Schwartz JB. Patterns of chronic co-morbid medical conditions in older residents of U.S. nursing homes: differences between the sexes and across the agespan. J Nutr Health Aging 2014; 18:429–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boockvar KS, Song W, Lee S, Intrator O. Hypertension treatment in US long-term nursing home residents with and without dementia. J Am Geriatr Soc 2019; 67:2058–2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hajjar I, Lackland DT, Cupples LA, Lipsitz LA. Association between concurrent and remote blood pressure and disability in older adults. Hypertension 2007; 50:1026–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gottesman RF, Albert MS, Alonso A, Coker LH, Coresh J, Davis SM, Deal JA, McKhann GM, Mosley TH, Sharrett AR, Schneider ALC, Windham BG, Wruck LM, Knopman DS. Associations between midlife vascular risk factors and 25-year incident dementia in the Atherosclerosis Risk in Communities (ARIC) cohort. JAMA Neurol 2017; 74:1246–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yano Y, Ning H, Allen N, Reis JP, Launer LJ, Liu K, Yaffe K, Greenland P, Lloyd-Jones DM. Long-term blood pressure variability throughout young adulthood and cognitive function in midlife: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Hypertension 2014; 64:983–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jette AM. Toward a common language for function, disability, and health. Phys Ther 2006; 86:726–734. [PubMed] [Google Scholar]
- 17. Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380:37–43. [DOI] [PubMed] [Google Scholar]
- 18. Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA 2012; 307:2493–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bowling CB, Deng L, Sakhuja S, Morey MC, Jaeger BC, Muntner P. Prevalence of activity limitations and association with multimorbidity among US adults 50 to 64 years old. J Gen Intern Med 2019; 34:2390–2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Szanton SL, Wolff JW, Leff B, Thorpe RJ, Tanner EK, Boyd C, Xue Q, Guralnik J, Bishai D, Gitlin LN. CAPABLE trial: a randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: rationale and design. Contemp Clin Trials 2014; 38:102–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Boyd CM, Wolff JL, Giovannetti E, Reider L, Weiss C, Xue QL, Leff B, Boult C, Hughes T, Rand C. Healthcare task difficulty among older adults with multimorbidity. Med Care 2014; 52(Suppl 3):S118–S125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bowling CB, Plantinga L, Phillips LS, McClellan W, Echt K, Chumbler N, McGwin G, Vandenberg A, Allman RM, Johnson TM II. Association of multimorbidity with mortality and healthcare utilization in chronic kidney disease. J Am Geriatr Soc 2017; 65:704–711. [DOI] [PubMed] [Google Scholar]
- 23. Hall RK, Zhou H, Reynolds K, Harrison TN, Bowling CB. A novel approach to developing a Discordance Index for older adults with chronic kidney disease. J Gerontol A Biol Sci Med Sci 2020; 75:522–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bowling CB, Vandenberg AE, Phillips LS, McClellan WM, Johnson TM II, Echt KV. Older patients’ perspectives on managing complexity in CKD self-management. Clin J Am Soc Nephrol 2017; 12:635–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care 2006; 29:725–731. [DOI] [PubMed] [Google Scholar]
- 26. Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA 2012; 307:182–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT; SPRINT Research Group . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, Fine LJ, Haley WE, Hawfield AT, Ix JH, Kitzman DW, Kostis JB, Krousel-Wood MA, Launer LJ, Oparil S, Rodriguez CJ, Roumie CL, Shorr RI, Sink KM, Wadley VG, Whelton PK, Whittle J, Woolard NF, Wright JT Jr, Pajewski NM; SPRINT Research Group . Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA 2016; 315:2673–2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, Myers MG, Ogedegbe G, Schwartz JE, Townsend RR, Urbina EM, Viera AJ, White WB, Wright JT Jr. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019; 73:e35–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Drawz PE, Agarwal A, Dwyer JP, Horwitz E, Lash J, Lenoir K, McWilliams A, Oparil S, Rahbari-Oskoui F, Rahman M, Parkulo MA, Pemu P, Raj DS, Rocco M, Soman S, Thomas G, Tuot DS, Whelton PK, Pajewski NM. Concordance between blood pressure in the Systolic Blood Pressure Intervention Trial and in routine clinical practice. JAMA Intern Med 2020; 180:1655–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Cohen JB, Padwal RS, Gutkin M, Green BB, Bloch MJ, Germino FW, Sica DA, Viera AJ, Bluml BM, White WB, Taler SJ, Yarows S, Shimbo D, Townsend RR. History and justification of a national blood pressure measurement validated device listing. Hypertension 2019; 73:258–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ishikawa J, Ishikawa Y, Edmondson D, Pickering TG, Schwartz JE. Age and the difference between awake ambulatory blood pressure and office blood pressure: a meta-analysis. Blood Press Monit 2011; 16:159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nesti N, Pieraccioli M, Mossello E, Sgrilli F, Bulgaresi M, Crescioli E, Biagini F, Caleri V, Tonon E, Cantini C, Biagini CA, Marchionni N, Ungar A. Tolerability of ambulatory blood pressure monitoring (ABPM) in cognitively impaired elderly. Blood Press 2014; 23:377–380. [DOI] [PubMed] [Google Scholar]
- 34. Tanner RM, Shimbo D, Seals SR, Reynolds K, Bowling CB, Ogedegbe G, Muntner P. White-coat effect among older adults: data from the Jackson Heart Study. J Clin Hypertens (Greenwich) 2016; 18:139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Franklin SS, Thijs L, Hansen TW, Li Y, Boggia J, Kikuya M, Björklund-Bodegård K, Ohkubo T, Jeppesen J, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Imai Y, Wang J, Ibsen H, O’Brien E, Staessen JA; International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators . Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension 2012; 59:564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mossello E, Pieraccioli MC, Zanieri S, Fedeli A, Belladonna M, Nesti N, Marchionni N, Masotti G, Ungar A. Ambulatory blood pressure monitoring in older nursing home residents: diagnostic and prognostic role. J Am Med Dir Assoc 2012; 13:760.e1–760.e5. [DOI] [PubMed] [Google Scholar]
- 37. Supiano MA, Williamson JD. New guidelines and SPRINT results: implications for geriatric hypertension. Circulation 2019; 140:976–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pajewski NM, Berlowitz DR, Bress AP, Callahan KE, Cheung AK, Fine LJ, Gaussoin SA, Johnson KC, King J, Kitzman DW, Kostis JB, Lerner AJ, Lewis CE, Oparil S, Rahman M, Reboussin DM, Rocco MV, Snyder JK, Still C, Supiano MA, Wadley VG, Whelton PK, Wright JT Jr, Williamson JD. Intensive vs standard blood pressure control in adults 80 years or older: a secondary analysis of the Systolic Blood Pressure Intervention Trial. J Am Geriatr Soc 2020; 68:496–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pajewski NM, Williamson JD, Applegate WB, Berlowitz DR, Bolin LP, Chertow GM, Krousel-Wood MA, Lopez-Barrera N, Powell JR, Roumie CL, Still C, Sink KM, Tang R, Wright CB, Supiano MA; SPRINT Study Research Group . Characterizing frailty status in the Systolic Blood Pressure Intervention Trial. J Gerontol A Biol Sci Med Sci 2016; 71:649–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, Cleveland ML, Coker LH, Crowe MG, Cushman WC, Cutler JA, Davatzikos C, Desiderio L, Erus G, Fine LJ, Gaussoin SA, Harris D, Hsieh MK, Johnson KC, Kimmel PL, Tamura MK, Launer LJ, Lerner AJ, Lewis CE, Martindale-Adams J, Moy CS, Nasrallah IM, Nichols LO, Oparil S, Ogrocki PK, Rahman M, Rapp SR, Reboussin DM, Rocco MV, Sachs BC, Sink KM, Still CH, Supiano MA, Snyder JK, Wadley VG, Walker J, Weiner DE, Whelton PK, Wilson VM, Woolard N, Wright JT Jr, Wright CB; SPRINT MIND Investigators for the SPRINT Research Group . Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA 2019; 321:553–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bowling CB, Whitson HE, Johnson TM II. The 5Ts: preliminary development of a framework to support inclusion of older adults in research. J Am Geriatr Soc 2019; 67:342–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged ≥65 years—United States, 2014. MMWR Morb Mortal Wkly Rep 2016; 65:993–998. [DOI] [PubMed] [Google Scholar]
- 43. Margolis KL, Palermo L, Vittinghoff E, Evans GW, Atkinson HH, Hamilton BP, Josse RG, O’Connor PJ, Simmons DL, Tiktin M, Schwartz AV. Intensive blood pressure control, falls, and fractures in patients with type 2 diabetes: the ACCORD trial. J Gen Intern Med 2014; 29:1599–1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, Zhou B, Lin H. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med 2014; 174:588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology 2010; 21:658–668. [DOI] [PubMed] [Google Scholar]
- 46. Shimbo D, Barrett Bowling C, Levitan EB, Deng L, Sim JJ, Huang L, Reynolds K, Muntner P. Short-term risk of serious fall injuries in older adults initiating and intensifying treatment with antihypertensive medication. Circ Cardiovasc Qual Outcomes 2016; 9:222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bromfield SG, Ngameni CA, Colantonio LD, Bowling CB, Shimbo D, Reynolds K, Safford MM, Banach M, Toth PP, Muntner P. Blood pressure, antihypertensive polypharmacy, frailty, and risk for serious fall injuries among older treated adults with hypertension. Hypertension 2017; 70:259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bowling CB, Davis BR, Luciano A, Simpson LM, Sloane R, Pieper CF, Einhorn PT, Oparil S, Muntner P. Sustained blood pressure control and coronary heart disease, stroke, heart failure, and mortality: an observational analysis of ALLHAT. J Clin Hypertens (Greenwich) 2019; 21:451–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Bowling CB, Sloane R, Pieper C, Luciano A, Davis BR, Simpson LM, Einhorn PT, Oparil S, Muntner P. Association of sustained blood pressure control with multimorbidity progression among older adults. J Am Geriatr Soc 2020; 68:2059–2066. [DOI] [PMC free article] [PubMed] [Google Scholar]