Abstract
Introduction:
Despite high rates of morbidity and mortality in patients with contrast-induced nephropathy (CIN), there is no consensus regarding prevention of this well-known complication of contrast media use. One agent that has been widely used in this regard is N-acetyl cysteine (NAC). Nevertheless, its efficacy is still controversial. The aim of this study was to assess the efficacy of NAC, both in the oral and intravenous forms, for the prevention of CIN.
Methods:
This study is a double-blind randomized placebo controlled clinical trial. We randomized 434 adult patients with chronic kidney disease (constant serum creatinine ≥1.5 mg/dL) who were candidates for coronary angiography/plasty. The patients were categorized into three groups. One group received 1,200 mg NAC intravenously half an hour before the procedure and oral placebo starting 3 days before angiography. The second group received oral NAC 600 mg twice daily for 3 days, starting the day before the intervention and intravenous placebo half an hour before intervention. The third group received both oral and intravenous placebo. CIN was defined as a 25% relative increase in serum creatinine from baseline value, 48 h after use of contrast medium.
Results:
Of the 434 patients, 149 received intravenous NAC, 145 received oral NAC, and the remaining 140 received placebo. The incidence of CIN in the three groups was 6.1%, 7.6%, and 10.8%, respectively (p = 0.34).
Conclusion:
In patients with chronic kidney disease, neither intravenous nor oral NAC is superior to placebo for preventing CIN.
Keywords: Chronic kidney disease, contrast nephropathy, coronary angiography, N-acetyl cysteine, prevention
Introduction
Due to the widespread use of contrast media (CM) in diagnostic and therapeutic procedures, the rate of contrast-induced nephropathy (CIN) is increasing. Although our understanding in pathophysiology of CIN is impressive, but unfortunately there is no option to treat this side effect. The most important side effect of CM is CIN. It is the 3rd cause of acute kidney disease (AKD) in hospital and is associated with high rate of mortality, increase in hospital stay, and high cost.[1]
Among different procedures using CM, coronary procedures are associated with more prevalence of CIN, meanwhile previous chronic kidney disease and coadministration of other nephrotoxic agents increase the rate of CIN.[2]
Difference studies showed that the occurrence of CIN in CKD patients with glomerular filtration rate (GFR) of more than 45 ml/min is rare while using iso or low-osmolal CM.[2,3,4]
But in GFR less than 30ml/min the risk is significantly increased.[2,3] The patients with GFR = 30-44ml/min is at median risk.[4]
While the real incidence of CIN is not known, it is difficult to assess and compare the success of different strategies in preventing CIN. Based on different mechanisms of CIN, a lot of strategies are implemented with contradictory results. The only successful measures are well hydration before procedure and the use of the lowest dose of low/isosmolal CM.[5] The agent was mostly used in this manner is N-Acetyl Cysteine (NAC). NAC is a potent anti-oxidant. It scavenges many free radical oxygen species, it has direct vasodilator effect on renal vasculature bed and decreases oxidative stress. Many studies regarding its role to prevent CIN have been done with contradictory and inconsistent results.
Overall, there is no consensus in use of NAC in preventing CIN. In addition, there is no agreement regarding route and dose and time of administration. We designed this study by considering all limitations and heterogeneity of previous studies and tried to include high risk patients in good numbers and used both oral and IV NAC.
Methods
Trial design
This study is a prospective, randomized, double-blinded, placebo-controlled clinical trial. It was run between 2014 and 2017 in Tehran Heart Center. The study started after it was approved by institutional review board at Tehran University of medical sciences. It registered at Iranian Registry of Clinical Trials (IRCT201205305113N3).
Study population
All elective patients referred for angiography/plasty were evaluated. Eligible patients were 18 years or older who had serum Cr ≥1.5 mg/dl and had clear history of CKD defined as having serum creatinine more than 1.5 mg/dL for at least 3 months. Other inclusion criteria were stable renal function (changes in serum Cr less than 25% from the last Cr measured before the study to that of the day of procedure), and CKD stage of 3–4 [as estimated glomerular filtration rate (eGFR) was measured by four variables Modification of Diet in Renal disease study equation]. After description of study all of those who agreed to enter the study and signed the written consent were recruited.
Excluding criteria were unstable hemodynamic patients, administration of diuretics, vasoactive agents, mannitol, fenoldopam, and use of nephrotoxins including CM in 5 days before or after the procedure. We also excluded the patients with uncontrolled hypertension (defined as blood pressure more than 160/110 mm Hg), and who needed surgery less than 5 days after procedure.
Interventions
All patients received normal saline 1cc/kg/h 12 h before procedure and continued 12 h thereafter. The diuretics were discontinued 24 h before procedure. The patients continued their regular medications like angiotensin converting enzyme inhibitors or angiotensin receptor blockers and statins. The CM was Iodixanol (Visipaque 320mg I/ml, GE healthcare, Norway). The dose of CM was according to weight × 5/Serum Cr formula. All patients were followed for 48 h and serum Cr was checked. In this period all patients were evaluated for hemodynamic status, use of possible nephrotoxic agents and other medical conditions.
Randomization
The patients were allocated randomly to three groups. The first group was on 1,200 mg NAC IV, infused half an hour before procedure. They were on oral placebo too (group A). The second group was on 600mg NAC bid orally, started the day before procedure and continued for 3 days. They were also on IV placebo (group B). The last group was on both oral an IV placebo (group C).
End point and definitions
The primary end point was defined according to different definition of AKI. Basically, we analyzed the results according to CIN definition of relative 25% increase of serum Cr from baseline. The results were also examined based on two other definitions of AKI-CIN which are absolute increase of 0.3 mg/dL serum creatinine or 0.5 mg/dL from baseline.
Statistical analysis
Continuous variables are summarized as mean ± SD. Categorical variables are shown as frequency and percentage. Comparison of continuous variables was performed by Student independent t-test and categorical data were compared by using X2 test. When it was necessary, Mann–Whitney U test and Fisher exact test were used. Odds ratio of CIN development with 95% confidence interval were calculated. The sample size was calculated according to X2 analysis for the primary endpoint. Assuming the development of CIN in 12% of placebo group and 3% in NAC group on the basis of previous studies, the power of this study in detecting statistically significant difference of 5% level is 80%.
The confidence level of the study is 95% and P < 0.05 is considered significant.
Results
In period of our study, 29,145 patients had coronary angiography/plasty in our center. According to inclusion/exclusion criteria 434 patients were elected [Figure 1]. The characteristic data of patients are shown in Table 1. It shows that there is no difference among the three groups in terms of type of angiography, hemodynamic status, complication, and short-term mortality and other factors that are known to impact the risk of CIN.
Figure 1.
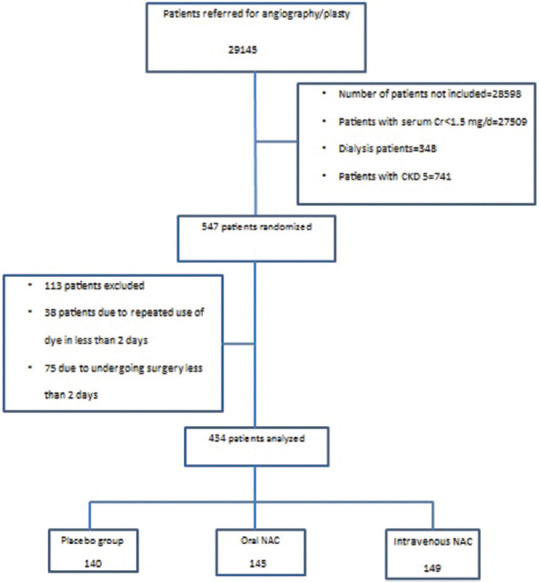
Patients' flow chart
Table 1.
Characteristic date
| Total n=434 | Group A n=149 | Group B n=145 | Group C n=140 | P | |
|---|---|---|---|---|---|
| Age (mean±SD) | 67.42±10.00 | 67.70±10.41 | 66.12±9.59 | 68.49±9.88 | 0.12 |
| Male | 73.5% (319) | 70.5% (105) | 75.2% (109) | 75% (105) | 0.58 |
| BMI (mean±SD) | 28.14±5.29 | 28.37±5.37 | 27.82±4.95 | 28.23±5.57 | 0.64 |
| Diabetes | 53% (230) | 52.3% (78) | 54.5% (79) | 52.1% (73) | 0.90 |
| Hypertension | 84.3% (366) | 84.6% (126) | 82.1% (119) | 86.4% (121) | 0.59 |
| Hyperlipidemia | 68% (295) | 70.5% (105) | 70.3% (102) | 62.9% (88) | 0.28 |
| Renal failure eGFR <60 ml/min) | 100% (434) | 34.4% (149) | 33.4% (145) | 32.2% (140) | 0.48 |
| Recent MI | 50.9% (219) | 50.3% (74) | 56.2% (81) | 46% (64) | 0.22 |
| Heart failure (EF <50%) | 33.3% (140) | 32.6% (47) | 34.8% (48) | 32.6% (45) | 0.90 |
| Hb level (g/L) | 12.75±2.21 | 12.57±2.14 | 12.76±2.20 | 12.91±2.29 | 0.42 |
| EF | 42.21±11.08 | 43.36±10.22 | 41.53±11.36 | 41.73±11.62 | 0.32 |
| GFR (ml/min) | 38.98±14.35 | 37.54±13.76 | 40.99±15.33 | 38.37±13.75 | 0.102 |
| Contrast Volume (ml) | 116.3±38.8 | 111.67±33.92 | 119.35±44.61 | 118.19±37.31 | 0.19 |
BMI=Body mass index, Hb=Hemoglobin, EF=Ejection fraction, GFR=Glomerular filtration rate
By definition of 25% relative increase in serum Cr a total of 35 patients (8.1%) had CIN. Of them nine patients were in group A (6.1%), 11 patients in group B (7.6%), and 15 patients in group C (10.8%). Although the trend of CIN is increased in placebo group but there is no statistically difference among groups (P = 0.34). We also examined the results according to two other definitions of AKI-CIN.
Based on 0.3mg/dL or 0.5 mg/dL increase of serum Cr [Table 2], once again we found no statistical difference among groups (P = 0.44 and 0.38, respectively). All patients in all groups did not require dialysis and were discharged from hospital in good condition with stable or reduced serum creatinine. We are following these patients for long-term outcome for which the results will be published in future.
Table 2.
Incidence of CIN in different groups according to different definitions of CIN
| Groups | Total n=434 | Group A* n=149 | Group B† n=145 | Group C‡ n=140 | P |
|---|---|---|---|---|---|
| Cr after 48 h | 1.99±0.77 | 2.05±0.81 | 1.90±0.63 | 2.00±0.85 | 0.27 |
| CIN0.5§ | 8.1% (35) | 6.8% (10) | 6.9% (10) | 10.8% (15) | 0.38 |
| CIN0.3|| | 12.4% (53) | 9.7% (14) | 13.3% (19) | 14.4% (20) | 0.44 |
| CIN25%# | 8.1% (35) | 6.1% (9) | 7.6% (11) | 10.8% (15) | 0.34 |
*Group A=IV NAC, †Group B=Oral NAC, ‡Group C=Placebo group, §CIN0.5=CIN defined by absolute 0.5 mg/dL increase of serum Cr from baseline, ||CIN0.3=CIN defined by absolute 0.3 mg/dL increase of serum Cr from baseline, #CIN25% = CIN defined by relative 25% increase of serum Cr from baseline
Discussion
Our study revealed no effect of oral or IV NAC on preventing CIN. While the half-life of NAC after IV injection is 40 min, it effects maybe due to its metabolites by inhibition of free oxygen radical activity. It may also have a role in releasing nitric oxide and N-Nitozitole which have vasodilator effects,[2] while free oxygen radicals have a known role in pathogenesis of CIN, so it is rational to use such anti-oxidants in preventing CIN.
After first report of Tepel et al.[6] that showed dramatic decrease of CIN with NAC, use of this drug was staggeringly growing. Since then although many studies have been run, but the controversies remain in use of NAC to prevent CIN.
Many studies have used oral NAC to prevent CIN. Some reported positive results,[7,8,9] while some showed negative results.[10,11,12] In the largest multicenter RCT,[13] 2,303 patients with at least one risk factor were enrolled. The researchers found no difference between oral NAC and placebo. Recently, Weisbord et al. published the results of PRESERVE trial.[14] In their large scale trial, they found no differences between patients who received saline versus bicarbonate and patients who received NAC versus placebo in the primary outcome (composite of death, need for dialysis, or persistent increase of 50% or > in baseline Cr at 90-104 days post-angiography). There were also no differences in CIN between patients who got NAC or placebo (2,500 patients in each group). A subgroup analysis of 2,615 patients with eGFR <45 ml/min also showed no difference in CIN incidence between placebo and NAC. But in their study oral NAC was used while in our study both oral and IV NAC were compared.
When studies with oral NAC didn't solve the problem, some researchers thought about IV NAC. Because the NAC has poor bioavailability, they thought that IV NAC maybe more effective than oral one. But, again IV NAC studies have also shown contradictory results. While some report good results,[8,15,16] the other founds no difference.[17,18,19,20,21]
The first study that compared IV NAC and placebo in 2006 showed that the higher doses of IV NAC is more effective than standard IV dose.[7] This study was on patients with Non ST- Elevation Acute Myocardial Infarction with normal renal function. The largest randomized trial of IV NAC was performed on 487 patients.[17] In this trial only 500mg IV NAC was used before procedure. This study was terminated early due to a determination of futility by the data safety monitoring committee. Nevertheless, this study showed no beneficial effect of NAC. Carbolell et al.[18] showed that in 216 patients with normal renal function 600mg IV NAC is not effective in preventing CIN. But this group in their next study on 81 patients with serum Cr ≥1.4 showed that NAC is more effective than placebo.[16]
Thiele et al.[19] showed IV NAC, 1,200mg bid for 48 h, cannot prevent CIN in patients with normal renal function. Kotlayar et al.[21] used 300 or 600 mg IV NAC and reported no benefit.
Study of Sochman et al. after first bolus[8] is interesting. They only studied 20 patients with serum Cr >1.5. The patients were divided in two groups. Both received 100mg/kg IV NAC but only one group received CM. This pilot study showed no increase in serum Cr in both groups.
Jaffary et al.[20] in a paper published recently, studied 398 patients. Their patients had non-ST elevation acute myocardial infarction with normal renal function. After first bolus of NAC before CM exposure they continued IV NAC infusion for 24 h. They also measured cystatin C in addition to serum Cr. They were also assessed for 1 month morbidity and mortality. They showed that there is no statistical difference between patients received NAC or placebo.
We found 22 meta-analyses between 2003 and 2016. These meta-analyses have also reported different results. Among them, 13 meta-analyses included at least one IV NAC study.[1,22,23,24,25,26,27,28,29,30,31,32,33] Some of them reported positive results.[1,22,25,26,27,28,29,31] There are only 2 meta-analyses that contain IV NAC studies. None of them showed any advantage in use of NAC.[33,34] These huge differences in results of these studies may be due to differences in sample size of studies, patient's condition (age, sex, associated conditions like CKD, diabetes and CHF), angiographic procedure (coroner, peripheral, CT Scan) contrast related issues, definition of end points, and many other factors. The type of hydration is another heterogeneous factor. One important limitation in these studies is difference in time of NAC administration[10] and finally bias in publishing studies with positive results.
So, taken together, despite many studies about the role of NAC in preventing CIN there are a lot of arguments regarding this cheap and relatively safe agent.[11,32,33]
The power of our study is sample size, including CKD patients, comparing both IV and oral NAC in same settings, and relatively high IV NAC dose. The limitations are like others; we define serum Cr as a surrogate of renal function which has many pitfalls.
The other limitation is short term follow-up of patients. We hope to continue following up these patients to show the difference in progression of CKD or need for dialysis or mortality.
Conclusion
NAC neither in oral form nor in IV form is not more effective than placebo in preventing CIN.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Tehran University of Medical Sciences code: 18043-146-02-91.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This work has been supported by Tehran University of Medical Sciences & Health services grant No 18043. We also would like acknowledge gratefully the members of the nursing staff of the different wards and cath. lab that participated in this study for their cooperation. Special thanks to Mrs. Shokooei for her hard work in data acquisition.
References
- 1.Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: Effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148:284–94. doi: 10.7326/0003-4819-148-4-200802190-00007. [DOI] [PubMed] [Google Scholar]
- 2.McDonald JS, McDonald RJ, Carter RE, Katzberg RW, Kallmes DF, Williamson EE. Risk of intravenous contrast material-mediated acute kidney injury: A propensity score-matched study stratified by baseline-estimated glomerular filtration rate. Radiology. 2014;271:65–73. doi: 10.1148/radiol.13130775. [DOI] [PubMed] [Google Scholar]
- 3.Afennas M, Bonnier H, Schoors D. Takotsubo cardiomyopathy after microwave ablation for metastatic liver lesions. Cardiovasc Revasc Med. 2017;18:526–7. doi: 10.1016/j.carrev.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 4.Davenport MS, Khalatbari S, Cohan RH, Dillman JR, Myles JD, Ellis JH. Contrast material–induced nephrotoxicity and intravenous low-osmolality iodinated contrast material: Risk stratification by using estimated glomerular filtration rate. Radiology. 2013;268:719–28. doi: 10.1148/radiol.13122276. [DOI] [PubMed] [Google Scholar]
- 5.Fahling M, Seeliger E, Patzak A, Persson PB. Understanding and preventing contrast-induced acute kidney injury. Nat Rev Nephrol. 2017;13:169–80. doi: 10.1038/nrneph.2016.196. [DOI] [PubMed] [Google Scholar]
- 6.Tepel M, van der Giet M, Schwarzfeld C, Laufer U, Liermann D, Zidek W. Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med. 2000;343:180–4. doi: 10.1056/NEJM200007203430304. [DOI] [PubMed] [Google Scholar]
- 7.Marenzi G, Assanelli E, Marana I, Lauri G, Campodonico J, Grazi M, et al. N-acetylcysteine and contrast-induced nephropathy in primary angioplasty. N Engl J Med. 2006;354:2773–82. doi: 10.1056/NEJMoa054209. [DOI] [PubMed] [Google Scholar]
- 8.Sochman J, Krizova B. Prevention of contrast agent-induced renal impairment in patients with chronic renal insufficiency and heart disease by high-dose intravenous N-acetylcysteine: A pilot-ministudy. Kardiol Pol. 2006;64:559–64. [PubMed] [Google Scholar]
- 9.Habib M, Hillis A, Hammad A. N-acetylcysteine and/or ascorbic acid versus placebo to prevent contrast-induced nephropathy in patients undergoing elective cardiac catheterization: The NAPCIN trial; A single-center, prospective, randomized trial. Saudi J Kidney Dis Transpl. 2016;27:55–61. doi: 10.4103/1319-2442.174072. [DOI] [PubMed] [Google Scholar]
- 10.Shabbir A, Kitt J, Alia O. Contrast-induced nephropathy in PCI: An evidence-based approach to prevention. Br J Cardiol. 2015;22:34–5. [Google Scholar]
- 11.Gurm HS, Smith DE, Berwanger O, Share D, Schreiber T, Moscucci M, et al. Contemporary Use use and effectiveness of N-acetylcysteine in preventing contrast-induced nephropathy among patients undergoing percutaneous coronary intervention. JACC Cardiovasc Interv. 2012;5:98–104. doi: 10.1016/j.jcin.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 12.Chong E, Poh K-K, Lu Q, Zhang JJ-J, Tan N, Hou XM, et al. Comparison of combination therapy of high-dose oral N-acetylcysteine and intravenous sodium bicarbonate hydration with individual therapies in the reduction of contrast-induced nephropathy during cardiac catheterisation and percutaneous coronary intervention (CONTRAST): A multi-centre, randomised, controlled trial. Int J Cardiol. 2015;201:237–42. doi: 10.1016/j.ijcard.2015.07.108. [DOI] [PubMed] [Google Scholar]
- 13.ACT Investigators. Acetylcysteine for prevention of renal outcomes in patients undergoing coronary and peripheral vascular angiography main results From the randomized Acetylcysteine for contrast-induced nephropathy trial (ACT) Circulation. 2011;124:1250–9. doi: 10.1161/CIRCULATIONAHA.111.038943. [DOI] [PubMed] [Google Scholar]
- 14.Weisbord SD, Gallagher M, Jneid H, Garcia S, Cass A, Thwin SS, et al. Outcomes after angiography with sodium bicarbonate and acetylcysteine. N Engl J Med. 2018;378:603–14. doi: 10.1056/NEJMoa1710933. [DOI] [PubMed] [Google Scholar]
- 15.Baker CSR, Wragg A, Kumar S, De Palma R, Baker LRI, Knight CJ. A rapid protocol for the prevention of contrast-induced renal dysfunction: The RAPPID study. J Am Coll Cardiol. 2003;41:2114–8. doi: 10.1016/s0735-1097(03)00487-x. [DOI] [PubMed] [Google Scholar]
- 16.Carbonell N, Sanjuan R, Blasco M, Jorda A, Miguel A. N-acetylcysteine: Short-term clinical benefits after coronary angiography in high-risk renal patients. Rev Esp Cardiol. 2010;63:12–9. doi: 10.1016/s1885-5857(10)70004-9. [DOI] [PubMed] [Google Scholar]
- 17.Webb JG, Pate GE, Humphries KH, Buller CE, Shalansky S, Al Shamari A, et al. A randomized controlled trial of intravenous N-acetylcysteine for the prevention of contrast-induced nephropathy after cardiac catheterization: Lack of effect. Am Heart J. 2004;148:422–9. doi: 10.1016/j.ahj.2004.03.041. [DOI] [PubMed] [Google Scholar]
- 18.Carbonell N, Blasco M, Sanjuan R, Perez-Sancho E, Sanchis J, Insa L, et al. Intravenous N-acetylcysteine for preventing contrast-induced nephropathy: A randomised trial. Int J Cardiol. 2007;115:57–62. doi: 10.1016/j.ijcard.2006.04.023. [DOI] [PubMed] [Google Scholar]
- 19.Thiele H, Hildebrand L, Schirdewahn C, Eitel I, Adams V, Fuernau G, et al. Impact of high-dose N-acetylcysteine versus placebo on contrast-induced nephropathy and myocardial reperfusion injury in unselected patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention.The LIPSIA-N-ACC (Prospective, single-blind, placebo-controlled, randomized leipzig immediate percutaneouS coronary intervention acute myocardial infarction N-ACC) trial. J Am Coll Cardiol. 2010;55:2201–9. doi: 10.1016/j.jacc.2009.08.091. [DOI] [PubMed] [Google Scholar]
- 20.Jaffery Z, Verma A, White CJ, Grant AG, Collins TJ, Grise MA, et al. A randomized trial of intravenous N-acetylcysteine to prevent contrast induced nephropathy in acute coronary syndromes. Catheter Cardiovasc Interv. 2012;79:921–6. doi: 10.1002/ccd.23157. [DOI] [PubMed] [Google Scholar]
- 21.Kotlyar E, Keogh A, Thavapalachandran S, Allada C, Sharp J, Dias L, et al. Prehydration alone is sufficient to prevent contrast-induced nephropathy after day-only angiography procedures – Arandomised controlled trial. Heart Lung Circ. 2005;14:245–51. doi: 10.1016/j.hlc.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 22.Pannu N, Manns B, Lee H, Tonelli M. Systematic review of the impact of N-acetylcysteine on contrast nephropathy. Kidney Int. 2004;65:1366–74. doi: 10.1111/j.1523-1755.2004.00516.x. [DOI] [PubMed] [Google Scholar]
- 23.Zagler A, Azadpour M, Mercado C, Hennekens CH. N-Acetylcysteine and contrast-induced nephropathy: A meta-analysis of 13 randomized trials. Am Heart J. 2006;151:140–5. doi: 10.1016/j.ahj.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 24.O'Sullivan S, Healy DA, Moloney MC, Grace PA, Walsh SR. The role of N--acetylcysteine in the prevention of contrast-induced nephropathy in patients undergoing peripheral angiography. Angiology. 2013;64:576–82. doi: 10.1177/0003319712467223. [DOI] [PubMed] [Google Scholar]
- 25.Alonso A, Lau J, Jaber B, Weintraub A, Sarnak M. Prevention of radiocontrast nephropathy with N-acetylcysteine in patients with chronic kidney disease: A meta-analysis of randomized, controlled trials. Am J Kidney Dis. 2004;43:1–9. doi: 10.1053/j.ajkd.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Trivedi H, Daram S, Szabo A, Bartorelli AL, Marenzi G. High-dose N-acetylcysteine for the prevention of contrast-induced nephropathy. Am J Med. 2009;122:874e879–15. doi: 10.1016/j.amjmed.2009.01.035. [DOI] [PubMed] [Google Scholar]
- 27.Wu MY, Hsiang HF, Wong CS, Yao MS, Li YW, Hsiang CY, et al. The effectiveness of N-acetylcysteine in preventing contrast-induced nephropathy in patients undergoing contrast-enhanced computed tomography: A meta-analysis of randomized controlled trials. IntUrol Nephrol. 2013;45:1309–18. doi: 10.1007/s11255-012-0363-1. [DOI] [PubMed] [Google Scholar]
- 28.Wang N, Qian P, Kumar S, Yan TD, Phan K. The effect of N-acetylcysteine on the incidence of contrast-induced kidney injury: A systematic review and trial sequential analysis. Int J Cardiol. 2016;209:319–27. doi: 10.1016/j.ijcard.2016.02.083. [DOI] [PubMed] [Google Scholar]
- 29.Xu R, Tao A, Bai Y, Deng Y, Chen G. Effectiveness ofN-acetylcysteine for the prevention of contrast-induced nephropathy: A systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc. 2016;5:pii: e003968. doi: 10.1161/JAHA.116.003968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bagshaw SM, Ghali WA. Acetylcysteine for prevention of contrast-induced nephropathy after intravascular angiography: A systematic review and meta-analysis. BMC Med. 2004;2:38. doi: 10.1186/1741-7015-2-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nallamothu BK, Shojania KG, Saint S, Hofer TP, Humes HD, Moscucci M, et al. Is acetylcysteine effective in preventing contrast-related nephropathy.A meta-analysis? Am J Med. 2004;117:938–47. doi: 10.1016/j.amjmed.2004.06.046. [DOI] [PubMed] [Google Scholar]
- 32.Biondi-Zoccai GG, Lotrionte M, Abbate A, Testa L, Remigi E, Burzotta F, et al. Compliance with QUOROM and quality of reporting of overlapping meta-analyses on the role of acetylcysteine in the prevention of contrast associated nephropathy: Case study. Br Med J. 2006;332:202–9. doi: 10.1136/bmj.38693.516782.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun Z, Fu Q, Cao L, Jin W, Cheng L, Li Z. Intravenous N-acetylcysteine for prevention of contrast-induced nephropathy: A meta-analysis of randomized, controlled trials. PloS One. 2013;8:e55124. doi: 10.1371/journal.pone.0055124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson SM, Park ZH, Patel RV. Intravenous N-acetylcysteine in the prevention of contrast media-induced nephropathy. Ann Pharmacother. 2011;45:101–7. doi: 10.1345/aph.1P275. [DOI] [PubMed] [Google Scholar]


