Abstract
Background and aim:
The COVID-19 pandemic has upended the global healthcare systems. The surge in infections and sick critically ill patients has tested the resilience of healthcare infrastructures and facilities forcing organizations to quickly adapt and embrace emergency solutions. The paper proposes a decalogue of design strategies applicable both to new hospitals and to the refurbishment of existing hospitals.
Methods:
The authors conducted observations at hospitals, during public health webinars and through experts working groups from March to May 2020.
Results:
In this commentary, the authors present a list of strategies for creating critical care surge capacity and exploring design strategies for healthcare design for resilient hospital facilities. The strategies are organized into two tiers: I) design and II) operations. The (I) Design phase strategies are: 1) Strategic Site Location; 2) Typology Configuration; 3) Flexibility; 4) Functional program; 5) User-centerdness. The (II) Operation phase strategies are: 6) Healthcare network on the territory; 7) Patient safety; 8) HVAC and indoor air quality; 9) Innovative finishing materials and furniture; 10) Healthcare digital innovation.
Conclusions:
Hospitals, health care systems, and institutions urgently need to assess their resources, identify potential bottlenecks, and create strategies for increasing critical care surge capacity. The COVID-19 pandemic disrupted healthcare operations and accelerated the processes of innovation and transformation. The design and operational strategies can enable the achievement of resilient hospital facilities. Further multidisciplinary researches is needed to validate the strategies empirically. (www.actabiomedica.it)
Keywords: COVID19, Hospital, Healthcare facilities, Built Environment, flexibility, resilience, evidence based design, user centerdness, digital innovation, patient safety
COVID-19 impact on healthcare systems
The coronavirus disease 2019 (COVID-19) virus is creating unprecedented stresses on healthcare facilities and critical care systems. The rate of infections and critically ill hospitalized patients reached unprecedented levels. Hospitals play a crucial role within the health system in providing essential medical care to the community, particularly during a crisis. They are complex and vulnerable institutions, dependent on critical external support and supply lines which operate with limited margin of error, at a very high rate and capacity. Even a modest rise in admission volume can overwhelm a hospital beyond its functional reserve. The COVID-19 pandemic has stressed critical support services and interrupted supply chains along with staff shortages and communications have also been challenging topics (1). Hospitals struggled to adequately respond to an unprecedented and sudden demand for emergency care and Intensive Care Unit (ICU) beds for infectious diseases in a very short span of time. The demand for COVID-19 beds in acute care departments globally surged, forcing healthcare settings to adopt contingency capacity strategies including: adaptations to medical care spaces, staffing constraints, and supply shortages in a way that could increase capacities without significant impact on medical care delivery. The COVID-19 pandemic highlighted all the existing structural, organizational and technological challenges of worn-out and obsolete healthcare facilities. These facilities were seen to undermine flexibility and efficiency in tackling rapid epidemiological, social and economic changes that was required to address the COVID-19 surge. Additionally, in the near term, healthcare systems will face two major, “collateral” issues: the physical and mental exhaustion of the healthcare workforce and the growing “backlog” of healthcare procedures (i.e. delay in cancer procedures, operations, etc.) (2,3).
In order to overcome the saturation of spaces in existing hospitals, two main strategies have been adopted.
In order to overcome the saturation of spaces within existing hospitals, two main strategies have been adopted.
First, in following the example of Wuhan, China, who scrambled to build an emergency hospital in 10 days, the whole world has taken the challenge to build as many temporary facilities to help support the great demand for beds for coronavirus patients. Facilities designed to support the care of 1000 patients , on a 25 thousand square meters of prefabricated blocks were undertaken as the symbol of how innovation in construction sector can impact healthcare processes. Countless temporary solutions such as containers, inflatable systems, tent structures, modules, partition panels, ships have been proposed by designers around the world such as the CURA (Connected Units for Respiratory Aliments), the open source project by Carlo Ratti Associates and colleagues or the 68 beds and 10 ICU beds at the East Meadow in Central Park in New York City.
The second strategy regarded the transformation of non-sanitary building typologies, unused during the pandemic, such as re-tooled trade centers, airports or schools. Several studies developed by Architecture, Engineering and Construction (AEC) firms such as HKS Architects, resulted in conceptual documents to convert schools or hotels into temporary healthcare spaces in 14 days or less. In addition, a taskforce set up by the American Institute of Architects (AIA) (4) provided a planning tool to quickly identify suitable buildings for patient care. Examples can be found in the transformation of the ExCel Center in London (UK) and the Exibition Center “Fiera Milano”, Milan (Italy) where also important transformations for improving the mechanical systems were done. Naturally, these examples have several limitations such as a limited capacity for surgery or high level diagnostics, lack of specialized support services and being distant from the core hospital.
The challenge of COVID-19 for healthcare facilities and the built environment
While outside the hospital pop-up structures emerged, within the existing healthcare facilities the organizations had to deal with two major aspects. The first, treating patients with severe symptoms while stemming the spread of the virus among patients, visitors and healthcare workers. In order to deal with the first aspect, there was a rapid conversion of hotels, trade centers, city parks into new hospital spaces, revealing a series of operational and safety difficulties that can be summarized in the structural impossibility of “detaching” a component such as ICUs from the rest of the hospital. Therefore, a large part of the COVID-19’s related activities have been designed “on-site” with ad-hoc and extremely varied solutions according to the needs of the individual hospital, department or ward. The lack of a national or regional comprehensive strategy is not only linked to the complexity of the emergency, but especially to the high complexity and highly variable hospital infrastructures. In fact, in terms of size, number of users and volume of activity, the hospital is more similar to a city within a city characterized by stratifications of service networks distributed in internal and external areas. For example, the state of conservation of Italian hospitals are in a critical. In fact, it is estimated that more than two thirds of the healthcare real estate has reached the end of its life cycle and more than half is not adapted to the new organizational models and epidemiological demands (3). This general state of obsolescence and rigidity has greatly contributed to the management challenges of this particular pandemic.
Hospitals were forced to adopt several cross-cutting strategies including the creation of: buffer areas between wards, the division between contaminated and non-contaminated areas, the transformation of acute care spaces (i.e. already equipped with advanced systems such suction, oxygen, negative pressure, etc.) starting from operating theatres; creating dedicated spaces for donning and doffing of personal protective equipment (PPE) decontamination areas for healthcare workers; new spaces with prefabricated technologies; core and shell empty environments at disposal (so-called “lung” spaces) to be equipped for emergencies or also unused area, gyms, car parks or congress centers.
The second challenge faced by hospitals is the virus containment. The lack of scientifically validated data and evidence-based protocols forced each hospital to develop ad hoc solutions sometimes based on models of prior epidemics caused by viruses such as Ebola (2013) and SARS (2003) or bacterial epidemics such as Tuberculosis. Coping with these highly contagious events required applying strict infection control protocols in the corridors, at key thresholds such as entrances to better manage the flows of staff who can infect themselves, colleagues and patients.
The aim is to propose strategies for hospitals to meet the needs for critical care capacity applicable both to new hospitals and to the refurbishment of existing hospitals to support a response for future health emergencies. What are the bottlenecks in critical care resources that might create a mismatch with the projected demand posed by the COVID-19 pandemic?
A decalogue for resilient hospital design
The aim of this commentary is to suggest a decalogue of strategies that are applicable both to new hospitals and to the re-furburishment of existing hospitals in order to respond rapidly and in the best possible way to the emergent needs that future health emergencies may bring to light. The hospitals of the future will have to be resilient to changes and capable of protecting different users’ health and tackle the transforming social, economic, environmental and epidemiological needs of the context in which they are located. We made a series of observation from March to May 2020 during public health webinars and through experts working groups. In particular, we built on the extensive expertise of the author’s in healthcare design and research. The observations were conducted in the following settings:
Participation in webinars organized by Public Health and Healthcare Design Associations at national and international level (Accademia Lombarda di Sanità Pubblica, Società Italiana di Igiene e Medicina Preventiva, Centro Nazionale Edilizia e Tecnica Ospedaliera, Design in Mental Health Network, Center for Health Design, International Academy for Design & Health);
Participation in institutional working groups such as Department of Architecture Built environment Construction engineering Observatories (Osservatori DABC) founded in response to need for institutional best practices formulation to face the so-called “Phase 2” in Italy;
Data was collected and reviewed from the gray literature and technical website, combining the following keywords: hospital; COVID-19; hospital planning; hospital refurbishment; design strategies;
Interaction with keynote speakers at the XI edition of the postgraduate Master “Planning, Programming Design of Healthcare and Socio-sanitary systems” Politecnico di Milano, Università degli Studi di Milano and Università Cattolica del Sacro Cuore di Roma.
According to previous statement and scenario a comparative matrix has been structured in order to merge the strategies derived from the data and case studies collection. Two areas of improvement have been highlighted: (I) strategies that can be implemented during the design phase and (II) strategies that can instead be achieved during the operation phase. We present a decalogue (5+5) of healthcare design strategies for resilient hospital facilities (Figure 1).
Figure 1.
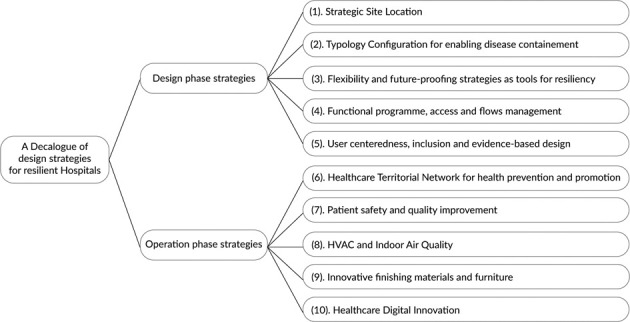
Flowchart of the decalogue of design strategies for resilient hospitals
(I) Design Phase strategies
1. Strategic Site Location
In the urban context, the hospital represents an important element for different factors, such as: the accommodation of a wide amount of users and visitors, the relevant building dimension and the economic supply chain. For this reason, hospitals’ site selection is a crucial topic in planning decision processes that affects the environmental, social and economic sustainability of healthcare structures and the efficiency of the health service (5,6)
In recent years, hospital trends have highlighted the importance of localization in central areas of the city, however past and ongoing experiences, especially in relation to an infectious epidemic, are challenging this tendence. Indeed, the capability of changing hospital’s areas or spreading them outside, has been often limited due to the lack of flexibility expansion related to the facilities’ location in dense city center. Learning from the management of previous pandemics, the localization of the post-COVID hospital to the city boundaries, can guarantee both the limitation of flows outside urban areas, containing possible risks of contagion in large high density city centers and the accessibility from the urban areas (7). At the same time, a correct strategic location represents an opportunity for spreading in areas close to the healthcare facility. On the other hand, central areas must host territorial facilities able to provide: health services at the first level, prevention and health promotion at the neighborhood scale(8).
2. Typology Configuration for Enabling Disease Containement
Currently, trends of hospital design typology are mainly characterized by horizontal configurations. This setting ensures, in emergency situations, the possibility to organize areas of the facility without constraining the entire flows and routes system (9). In order to provide an effective emergency management, treatment areas for infectious patients should be isolated through a clear routes separations, limiting cross-contaminations by avoiding the use of vertical and horizontal connections for multiple areas. Therefore, a hybrid typological configuration, characterized by a main body connected to support pavilions, might represent a strategic solution, with dedicated accesses for emergency and logistics vehicles. In case of infectious emergency, the independence of the buildings or the availability of autonomous internal units, allow to separate different functional areas from the rest of the hospital system, without ordinary activities interruption. Providing outdoor spaces around the hospital area is also suitable for hosting possible temporary structures such as tents, tensile structures or other modular solutions, which guarantee the connection to the hospital and the relationship to driveways for ambulances and logistics vehicles.
3. Flexibility and Future-Proofing Strategies as Tools for Resiliency
Resilience is one of the most important challenges that hospital structures must tackle according to healthcare emergency needs that might arise or disappear at a very fast rate. In order to ensure effective emergency management, flexibility represents a fundamental aspect to consider in the hospital design process, from the overall building system to the single functional and environmental units (10). The Rush University Medical Center in Chicago was a relevant example during COVID-19 pandemic. The hospital can expand both the emergency department capacity and the number of isolation rooms when needed. During ordinary operations, the Rush hospital has 40 negative pressure rooms that help prevent the spread of potentially infectious diseases in the air. Each room has a negative pressure with respect to the external corridor, in order to let the air flow from the corridor into the room, leaving the hospital through the introduction of HEPA filters. All the interventions that can guarantee a fast reconfiguration are therefore strategic in emergency situations, such as:
the presence of “lung” spaces, empty and support areas among different lots and departments to accommodate expansions, reconfigurations or isolation areas;
non-sanitary hospitals areas easily transformable and to be equipped with low investments. For instance, the underground parking of the Rambam hospital in Haifa (Israel) can be converted into a hospital with 2.000 beds in wartime or flexible sports facilities ca be reconfigured. Therefore, these areas must be supported by direct internal connections with the rest of the hospital and outside for ambulances;
functional areas that can be easily reconverted, such as common hospital ward that are provided of the proper amount of technical installations.
4. Functional Programme, Access and Flows Management
Functional program is fundamental in complex facilities such as hospital. In case of emergency the design should consider some transversal issues:
Distribution is one of the main aspects to consider within the functional programme in relation to emergencies. The access for staff must be unique, as well as that one for visitors who are not directed to the emergency department. In case of an infectious emergency, flows that are normally differentiated between users and health workers, must be able to be further separated, in order to divide the flows of patients with suspected or known infection by other users. In this regard, recognizable signage must effectively indicate temporary changes in hospital routes.
The strong relation between the emergency department and infectious wards requires a fast connection for the movement of patients and healthcare workers. These spaces should be therefore placed at the same level promoting short and horizontal connections.
The presence of storage areas is also required, which in case of infective emergency can host the wide amount of sanitary material, PPE and contaminated waste. Furthermore, there is a need of solutions for the extraordinary placement of corpses in low temperature environments, in close communication with the external driveways for their transport.
In order to decrease the risk of nosocomial diffusion of any infectious agent, all ordinary hospital wards must maximize the number of single rooms. This can be reached with a set of bed head beams and engineering plant equipment that allow to transform rooms into double rooms in case of hyper flow of patients.
In addition, a resilient hospital design must consider some organizational aspects of both high and low care areas mostly interested by the infectious emergency, such as:
The intensive care department results as the one of the most affected, so additional filter areas are needed for the dressing/undressing of the healthcare workers. Separated working areas from the main care area are suggested, in order to reduce the staff exposure and the use of mobile diagnostic equipment (i.e. mobile ultrasound scanner, Point-Of-Care Testing POCT machines, X-ray diagnostics and mobile Computed Tomography CT).
The emergency department must at the same time host patients with suspected infection and continue to manage all non-infectious cases, separating them from their entrance. Therefore two separate entrances are recommended to distinguish sick people through dedicated triage, with separate paths and waiting and treatment spaces. External multiple decontamination areas for ambulances and areas for the preparation of pre-triage tents must be provided.
The sanitary hotel, which usually welcomes outpatients, relatives or visitors, in emergency conditions must have a flexible configuration that allows to accommodate ordinary and additional healthcare workers, reducing the infectious risk for their families and ensuring them an effective rest in situations of high work stress. Similarly, it could be transformed to accommodate infectious patients of lower gravity or patient who need rehabilitation.
5. User Centerdness. Inclusion and Evidence Based Design
Studies on User-Centered Design and more in general Universal Design (11), confirm that during all the different phases of the design process, attention must be focused to the physical, psychological and social needs of all users to avoid future disabling situations generated due to COVID-like overwhelming conditions (12). This is especially true in hospital environments, where aspects as accessibility, wayfinding and comfort, directly impact on different users (patients, healthcare workers, visitors) during emergency situations. In particular, healthcare workers show symptoms of anxiety, depression, insomnia and stress higher than normal within hospital facilities. In this regard, during the COVID-19 pandemic, the design firm Studio Elsewhere develops “recharge rooms” for hospitals characterized by natural design elements that support medical workers recover from a physically and mentally taxing shift. These spaces are designed to be customized according to the users’ needs, such as sounds, sights, and smells. The rooms use bringing the outdoors into built environments - to create spaces with nature (real and on a screen) out of underused hospital spaces near intensive care departments. Researches, in fact, have demonstrated that looking at nature can improve recovery patient time and reduce nursing stress levels (13-15).
Evidence Based Design (EBD) studies demonstrate that the presence of spaces for the physical and psychological well-being is strategic for all users and it also positively influence the work performance of the healthcare staff. Such spaces, in fact, in case of emergency, could guarantee users environments to relax from psychological stress and daily pressures. They can be both areas inside the structure - close to the functional areas - or green areas of the hospital (i.e. garden and terraces), preferably with a variety of spaces, different seats and isolation points to ensure user’s privacy (17).
(II) Operation phase strategies
6. Healthcare Territorial Network for Health Prevention and Promotion
The synergy between territorial services and hospital organizations plays a crucial role for health promotion (18,19). In particular, starting from the recent experience, the adoption of Hub & Spoke model could turn out particularly efficient in cases of high emergencies, avoiding the overflow of users in the hospital thanks to health home care management or low and medium-care facilities (20).
The creation of community health centers in the territory for guaranteeing the primary care services and triage activities could ensure a better management of low and medium-care services, as well as to favor the use of smart diagnostics and to support the outpatients management on the territory (21). This capillary model encourages access to care for the population (6), reducing the patients’ transfer across the territory, decreasing the overcrowding of the emergency departments, and minimizing hospital-based cross-contamination among users and healthcare staff. These healthcare facilities should be configured as integrated hub between healthcare professionals and healthcare and social services, also for NGOs and voluntary associations for addressing fragile users needs (22-24). In addition, the use and application of healthcare devices for the smart hospital, as well as telemedicine programs, can easily support and strengthen the health network and the monitoring of the users’ health status, even in the presence of healthcare emergencies (18,25).
7. Patient Safety and Quality Improvement
It is well-known that healthcare organizations regularly give rise to protocols for risk control and patient safety in hospital settings. In particular, during the pandemic, the healthcare leadership need to reorganized the users’ behaviors and healthcare protocols in line with the best practices for the COVID-19 control. Healthcare design should give rise to physical environments that support providers to act in a professional, trustful and respectful manner for all the community (26). Facility design affects how people work, and what processes, systems and technologies they will require to support the functioning of a learning work environment. In addition it is necessary to take into consideration design strategies aimed at responding to possible emergencies and medical needs for guaranteeing patient safety. For example, among them, several healthcare facilities have included visual cues for visitors and users for highlighting the proximity of risk functional areas and infectious impatient wards. Others have adopted protocols for bringing healthcare devices and materials, as well as the medical waste, through dedicated elevators in an attempt to minimize cross-contamination. Moreover, for guaranteeing the regular disinfection activities, some hospitals adopted spaces called “pods” for low-acuity patients. They were designed to reduce possible infection by separating the patient from the equipment to be cleaned, thus reducing the possibility of contaminating them (27). Several hospitals adopted strategies, such as adhesive tape on the floor, signage and signs boards on door used for annotations with special markers, intentionally positioned. Stations for accessing the PPE were provided in key positions, which in turn influenced the way and the place in which the hospital staff used the equipment. The ability to interpret and understand the configuration of the space can be a powerful tool to support healthcare professionals within unfamiliar and rapidly evolving COVID-19 care environments. Simple visual devices, wayfinding strategies and design-nudges can help to mitigate the transmission of infections by clearly defining risk areas, creating “mental anchors” for specific activities (28,29) and consequently reducing mental fatigue and helping to align the behavior with the protocols to be followed.
8. HVAC and Indoor Air Quality
It is well known that air quality in confined spaces plays a direct or indirect leading role in prevention, especially in environments with vulnerable users. The quality of the indoor air (IAQ) depends not only on the outdoor air but also on the presence of indoor sources that emit pollutants that can affect its composition (30,31). It is therefore necessary to ensure adequate air exchange in all environments through mechanical and, where possible, mixed ventilation. To ensure efficient management in case of emergency, such as infectious epidemics the ventilation systems have a strategic role, but its functioning must be able to respond to different healthcare needs, in all the conditions and especially in emergency situations where air could be a possible means of infection diffusions (32,33). The heating, ventilation, and air conditioning (HVAC) must be flexible and their operation must be able to be modified in terms of the air used, from recirculation to all-air systems, and pressure, from positive to negative (34,35). In addition, their regular and constant maintenance, cleaning and disinfection also become strategic through the use of innovative materials. As a consequence new generation systems must be designed with solutions that guarantee easy inspection, and the possibility of intervention (36).
9. Innovative Finishing Materials and Furniture
Healthcare Acquired Infections (HAIs) have a relevant strategic role in the light of the management of the COVID pandemic. In synergy with monitoring and risk management activities, it is necessary to use high-performance, long-lasting and easy to clean materials in relation to the medical needs. In particular, innovative materials must be introduced to reduce the bacterial (and viral) load on the finishing surfaces (37) among which also eco-active ones and photocatalytic paints (30,38), as well as characterized by high performances and flexibility-in-use. It is necessary to investigate and take into consideration, also, solutions used in emergency contexts such as, for example, washable textile materials (39). Their application could be extended in different sanitary areas for social distancing, and which in case of need can be easily clean and replaced, and/or removed for guaranteeing the adaptability and resilience of the spaces (40,41). Together with the application of best practices of ventilation, the choice of cleaning products must be defined in relation to the finishing materials and furnishings in the environmental unit, considering the peculiarities and features of each surface (42). In addition, detergents (such as hydrogen peroxide, alcohols, sodium hypochlorite or benzenzonium chloride) have chemical compositions that kill the bacterial and antiviral load but, at the same time, they can present volatile organic compounds (VOCs) toxic to humans (30), and require paying attention to environmental sustainability (43).
10. Healthcare Digital Innovation
The new digital technologies can support the patients’ treatment and care processes both in the hospital and on the territorial healthcare network (20). It can be considered not only for ordinary medical activities, but also in case of emergency. In fact, the continuous control of the health status and vital parameters through IT systems, such as smartphone or wearable devices, can guarantee a better management of hospitalization, and consequently an efficient organization of hospital settings (44). Moreover, the modular planning and forecasting of the occupation of Intensive Care Unit (ICU) and ordinary beds, both in the same hospital and within the territorial hospital network, can support - in real time - the possible directing of the ambulances to the more appropriate healthcare facility. In addition, the constant monitoring and technological advancement allows the use of some electro-medical equipment remotely, decreasing the contacts between (infected) patients and hospital staff, and guaranteeing an overall control and a more efficient use of the resources (45). As well the use of sensors and devices through the Internet of Things allows the hospital to guarantee a personalized and dedicated experience for each user, monitoring the degree of comfort and satisfaction (27). In conclusion, the substantial reduction of paper-based health and administrative documentation through the digital innovation allows the reuse of storage spaces and archives for other functions, including server rooms (41). In the close future all medical procedures that can be treated without physical presence, will be carried out through digital systems and healthcare organizations will also be able to better manage patients’ clinical information and therefore users at risk will be more protected through tailored medical paths. Nowadays more than ever, digital healthcare system represents a ‘life saver’, an accelerator of health and an evident reduction in the costs of healthcare services.
Preliminary conclusions and future perspectives
As in many other spheres and economic activities, this pandemic has accelerated all those processes of innovation and digitization that had somehow already been activated. The home care issue, the use of smart devices for a dialogue between the healthcare professionals and the pervasive use of apps to monitor certain health parameters, are just some of the megatrends that were being observed and which have now necessarily entered into everyday life. In the same way, the hospital, which in the face of this gradual process of dematerialization and relocation of ‘softer’ clinical-diagnostic activities, reaffirms itself as a centre of the highest specialty for the treatment and care of acute patients, for high-level clinical and experimental research, for diagnostics and more complex operations (Figure 2).
Figure 2.
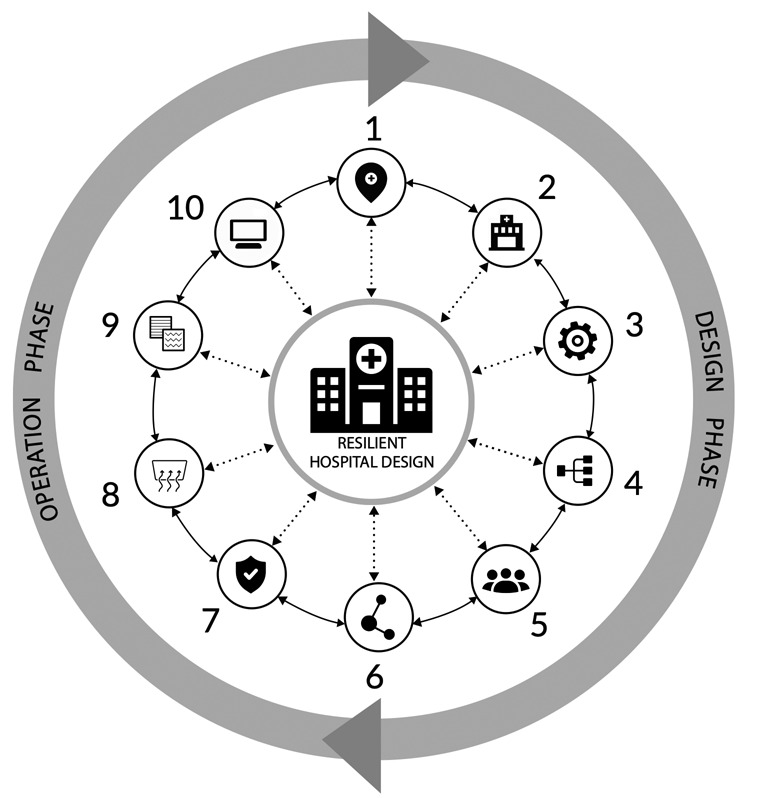
A graphical diagram that describe the 10 strategies proposed in the commentary
Antimicrobial resistance has been recently highlighted by several institutions due to the mis-use and/or overuse of antibiotics in human medicine, specific facilities for infectious diseases treatment and containments emerged (46-51). The COVID pandemic highlighted that a post-antibiotic era can be very difficult to tackle and the role of built environment is of increasing importance. Indeed, due to the high diffusion and infectious rates of COVID and in the absence of reliable drugs or specific vaccinations, the pandemic containment has been mainly performed through physical and social tool such as the confinement practices and hand washing. The hospital will have to increasingly reflect on its role of health promotion and protection, especially towards the most fragile users.
It is essential to promote multidisciplinary actions and monitoring programs for quality improvement through evidence-based evaluation tools in order to develop a new design for the hospital of the near future (52). Further multidisciplinary researches is encouraged to validate the presented strategies in case studies and in empirical settings.
The decalogue of strategie aims to briefly indicate the key strategies to be considered in the design of new resilient hospitals and in the re-functionalization of existing structures.
Acknowledgements
We thank Prof. Mario Claudio Dejaco for his participation in the project.
Conflict of interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.WHO. Hospital Readiness Checklist for COVID-19. World Health Organization Regional Office for, 2020. Available from: https://www.euro.who.int/__data/assets/pdf_file/0010/430210/Hospital-Readiness-Checklist.pdf . [Google Scholar]
- 2.Impact of the Covid-19 pandemic on healthcare systems? Deloitte France. Available from: https://www2.deloitte.com/fr/fr/pages/covid-insights/articles/impact-covid19-healthcare-systems.html. [Accessed: 18th June 2020] [Google Scholar]
- 3.Barach P, Fisher SD, Adams MJ, et al. Disruption of healthcare: Will the COVID pandemic worsen non-COVID outcomes and disease outbreaks? Progress in Pediatric Cardiology. 2020;101254 doi: 10.1016/j.ppedcard.2020.101254. doi: 10.1016/j.ppedcard.2020.101254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AIA’s COVID-19 Task Force Creates Design Guide to Retrofit Buildings for Alternative Care. ArchDaily. Available from: https://www.archdaily.com/937331/aias-covid-19-task-force-creates-design-guide-to-retrofit-buildings-for-alternative-care. [Accessed: 21st June 2020] [Google Scholar]
- 5.Dell’Ovo M, Capolongo S, Oppio A. Combining spatial analysis with MCDA for the siting of healthcare facilities. Land Use Policy. 2018;76:634–644. Available from: doi:10.1016/j.landusepol.2018.02.044. [Google Scholar]
- 6.Dell’Ovo M, Frej EA, Oppio A, Capolongo S, Morais DC, de Almeida AT. FITradeoff Method for the Location of Healthcare Facilities Based on Multiple Stakeholders’ Preferences Group Decision and Negotiation in an Uncertain World. In: Chen Y, Kersten G, Vetschera R, Xu H, editors. Cham. Springer International Publishing; 2018. pp. 97–112. doi: 10.1007/978-3-319-92874-6_8. [Google Scholar]
- 7.Capasso L, Faggioli A, Rebecchi A, et al. Aspetti igienico-sanitari in ambito urbanistico: conflittualità nelle norme urbanistiche nazionali e locali in tema di sanità pubblica. Epidemiologia & Prevenzione. 2018;42(1):60–64. doi: 10.19191/EP18.1.P060.016. doi: 10.19191/EP18.1.P060.016. [DOI] [PubMed] [Google Scholar]
- 8.Miedema E, Lindahl G, Elf M. Conceptualizing Health Promotion in Relation to Outpatient Healthcare Building Design: A Scoping Review. HERD. Health Environments Research & Design Journal. 2019;12(1):69–86. doi: 10.1177/1937586718796651. Available from: doi:10.1177/1937586718796651. [DOI] [PubMed] [Google Scholar]
- 9.Capolongo S, Cocina G, Peretti G, Pollo R, Gola M. Horizontality and verticality in architectures for health. TECHNE - Journal of Technology for Architecture and Environment. 2019;17:152–160. Available from: doi:10.13128/Techne-24028. [Google Scholar]
- 10.Capolongo S, Buffoli M, Nachiero D, Tognolo C, Zanchi E, Gola M. Open building and flexibility in healthcare: strategies for shaping spaces for social aspects. Annali dell’Istituto Superiore di Sanità. 2016;52(1):63–69. doi: 10.4415/ANN_16_01_12. [DOI] [PubMed] [Google Scholar]
- 11.Mosca EI, Herssens J, Rebecchi A, Capolongo S. Inspiring architects in the application of design for all: knowledge transfer methods and tools. Journal of Accessibility and Design for All. 2019;9(1) doi: 10.17411/jacces.v9i1.147. [Google Scholar]
- 12.Mosca EI, Capolongo S. Towards a Universal Design Evaluation for Assessing the Performance of the Built Environment. Transforming our World Through Design, Diversity and Education. IOS Press Ebooks. 2018:771–779. [PubMed] [Google Scholar]
- 13.Brambilla A, Capolongo S. Healthy and Sustainable Hospital Evaluation—A Review of POE Tools for Hospital Assessment in an Evidence-Based Design Framework. Buildings. Multidisciplinary Digital Publishing Institute. 2019;9(4):76. doi: 10.3390/buildings9040076. [Google Scholar]
- 14.Ulrich RS, Zimring C, Zhu X, et al. A Review of the Research Literature on Evidence-Based Healthcare Design. HERD. Health Environments Research & Design Journal. 2008;1(3):61–125. doi: 10.1177/193758670800100306. doi: 10.1177/193758670800100306. [DOI] [PubMed] [Google Scholar]
- 15.Debajyoti P, Harvey T, Barach P. The impact of exterior views on nurse stress: An Exploratory Study. Health Environments Research and Design Journal. 2008;2:27–38. [Google Scholar]
- 16.Elf M, Anåker A, Marcheschi E, Sigurjónsson Á, Ulrich RS. The built environment and its impact on health outcomes and experiences of patients, significant others and staff—A protocol for a systematic review. Nursing Open. 2020 doi: 10.1002/nop2.452. doi:10.1002/nop2.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buffoli M, Rebecchi A, Gola M, Favotto A, Procopio GP, Capolongo S. Green SOAP. A Calculation Model for Improving Outdoor Air Quality in Urban Contexts and Evaluating the Benefits to the Population’s Health Status Integrated Evaluation for the Management of Contemporary Cities. In: Mondini G, Fattinnanzi E, Oppio A, Bottero M, Stanghellini S, editors. Cham. Springer International Publishing; 2018. pp. 453–467. doi: 10.1007/978-3-319-78271-3_36. [Google Scholar]
- 18.Capolongo S, Mauri M, Peretti G, Pollo R, Tognolo C. Facilities for Territorial Medicine: the experiences of Piedmont and Lombardy Regions. TECHNE - Journal of Technology for Architecture and Environment. TECHNE - Journal of Technology for Architecture and Environment. 2015:230–236. Pages. doi: 10.13128/TECHNE-16128. [Google Scholar]
- 19.Odone A, Saccani E, Chiesa V, et al. The implementation of a Community Health Centre-based primary care model in Italy. The experience of the Case della Salute in the Emilia-Romagna Region. Annali dell’Istituto Superiore Di Sanita. 2016;52(1):70–77. doi: 10.4415/ANN_16_01_13. doi: 10.4415/ANN_16_01_13. [DOI] [PubMed] [Google Scholar]
- 20.Mauri M. The future of the hospital and the structures of the NHS. TECHNE - Journal of Technology for Architecture and Environment. 2015:27–34. doi: 10.13128/Techne-16100. [Google Scholar]
- 21.Oppio A, Buffoli M, Dell’Ovo M, Capolongo S. Addressing Decisions About New Hospitals’ Siting: A Multidimensional Evaluation Approach. Ann Ist Super Sanita. 2016;52(1):78–87. doi: 10.4415/ANN_16_01_14. [DOI] [PubMed] [Google Scholar]
- 22.Gola M, Fugazzola E, Rebecchi A. Mapping and Programming Healthcare Services for New Health Perspectives Healthcare Facilities in Emerging Countries. In: Capolongo S, Gola M, Rebecchi A, editors. Cham. Springer International Publishing; 2018. pp. 89–111. doi: 10.1007/978-3-319-72398-3_6. [Google Scholar]
- 23.Faroldi E, Fabi V, Vettori MP, Gola M, Brambilla A, Capolongo S. Health Tourism and Thermal Heritage: Assessing Italian Spas with Innovative Multidisciplinary Tools. Tourism Analysis. 2019;24(3):405–419. doi: 10.3727/108354219X15511865533121. [Google Scholar]
- 24.Brambilla A, Maino R, Mangili S, Capolongo S. Built Environment and Alzheimer. Quality Evaluation of Territorial Structures for Patients with Dementia. In: Bevilacqua C, Calabrò F, Della Spina, editors. New Metropolitan Perspectives. Knowledge Dynamics and Innovation-driven Policies Towards Urban and Regional Transition. Switzerland: Springer International Publishing; in press) [Google Scholar]
- 25.Capolongo S, Rebecchi A, Buffoli M, et al. COVID-19 and Cities: from Urban Health strategies to the pandemic challenge. A Decalogue of Public Health opportunities. Acta Bio Medica Atenei Parmensis. 2020;91(2):13–22. doi: 10.23750/abm.v91i2.9515. doi: 10.23750/abm.v91i2.9615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brambilla A, Rebecchi A, Capolongo S. Evidence Based Hospital Design. A literature review of the recent publications about the EBD impact of built environment on hospital occupants’ and organizational outcomes. annali di igiene medicina preventiva e di comunità. 2019;2:165–180. doi: 10.7416/ai.2019.2269. doi: 10.7416/ai.2019.2269. [DOI] [PubMed] [Google Scholar]
- 27.Marsilio M, Prenestini A. Making it happen: Challenges and transformations in health care processes, people management, and decision-making. Health Services Management Research. 2020;33(2):53–54. doi: 10.1177/0951484820906314. doi: 10.1177/0951484820906314. [DOI] [PubMed] [Google Scholar]
- 28.Mosca EI, Herssens J, Rebecchi A, Strickfaden M, Capolongo S. Cham. Springer International Publishing; 2019. Evaluating a Proposed Design for All (DfA) Manual for Architecture. In: Di Bucchianico G (ed.) Advances in Design for Inclusion; pp. 54–64. doi: 10.1007/978-3-319-94622-1_6. [Google Scholar]
- 29.Jamshidi S, Pati D. A Narrative Review of Theories of Wayfinding Within the Interior Environment. HERD. Health Environments Research & Design Journal. 2020;193758672093227 doi: 10.1177/1937586720932276. doi: 10.1177/1937586720932276. [DOI] [PubMed] [Google Scholar]
- 30.Gola M, Settimo G, Capolongo S. Indoor Air Quality in Inpatient Environments: A Systematic Review on Factors that Influence Chemical Pollution in Inpatient Wards. Journal of Healthcare Engineering. 2019;2019:1–20. doi: 10.1155/2019/8358306. doi: 10.1155/2019/8358306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Settimo G. Existing Guidelines for Indoor Air Quality: The Case Study of Hospital Environments. In: Capolongo S, Settimo G, Gola M, editors. Indoor Air Quality in Healthcare Facilities. Cham: Springer International Publishing; 2017. pp. 13–26. Available from: doi:10.1007/978-3-319-49160-8_2. [Google Scholar]
- 32.Correia G, Rodrigues L, Gameiro da Silva M, Gonçalves T. Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Medical Hypotheses. 2020;141:109781. doi: 10.1016/j.mehy.2020.109781. doi: 10.1016/j.mehy.2020.109781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Y, Leung GM, Tang JW, et al. Role of ventilation in airborne transmission of infectious agents in the built environment? a multidisciplinary systematic review. Indoor Air. 2007;17(1):2–18. doi: 10.1111/j.1600-0668.2006.00445.x. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- 34.Moscato U, Borghini A, Teleman AA. HVAC Management in Health Facilities Indoor Air Quality in Healthcare Facilities. In: Capolongo S, Settimo G, Gola M, editors. Cham. Springer International Publishing; 2017. pp. 95–106. doi: 10.1007/978-3-319-49160-8_9. [Google Scholar]
- 35.Astley P, Capolongo S, Gola M, Tartaglia A. Operative and design adaptability in healthcare facilities. TECHNE - Journal of Technology for Architecture and Environment. 2015:162–170. doi: 10.13128/Techne-16118. [Google Scholar]
- 36.Joppolo CM, Romano F. HVAC System Design in Healthcare Facilities and Control of Aerosol Contaminants: Issues, Tools, and Experiments Indoor Air Quality in Healthcare Facilities. In: Capolongo S, Settimo G, Gola M, editors. Cham. Springer International Publishing; 2017. pp. 83–94. doi: 10.1007/978-3-319-49160-8_8. [Google Scholar]
- 37.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. New England Journal of Medicine. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bianchi CL, Sacchi B, Capelli S, et al. Micro-sized TiO2 as photoactive catalyst coated on industrial porcelain grès tiles to photodegrade drugs in water. Environmental Science and Pollution Research. 2018;25(21):20348–20353. doi: 10.1007/s11356-017-9066-6. doi: 10.1007/s11356-017-9066-6. [DOI] [PubMed] [Google Scholar]
- 39.Capolongo S, Buffoli M, Riva MG, Tognolo C, Oppio A. Hygiene and emergency. Considerations and proposals for improving hygiene and health features of Advanced Medical Post. Annali Di Igiene. Medicina Preventiva E Di Comunita. 2012;24(5):389–396. [PubMed] [Google Scholar]
- 40.Zanelli A, Campioli A, Monticelli C, Viscuso S, Giabardo G. Novel Textile-Based Solutions of Emergency Shelters: Case Studies and Field Tests of S(P)EEDKITS Project Innovative Models for Sustainable Development in Emerging African Countries. In: Aste N, Della Torre S, Talamo C, Adhikari RS, Rossi C, editors. Cham. Springer International Publishing; 2020. pp. 111–122. doi: 10.1007/978-3-030-33323-2_10. [Google Scholar]
- 41.Buffoli M, Nachiero D, Capolongo S. Flexible Healthcare Structures: Analysis and Evaluation of Possible Strategies and Technologies. Annali di Igiene Medicina Preventiva e di Comunità. 2012;24(6):543–552. [PubMed] [Google Scholar]
- 42.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.01.022. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bassi A, Ottone C, Dell’Ovo M. Minimum environmental criteria in the architectural project. Trade-off between environmental, economic and social sustainability. Valori E Valutazioni. 2019;22:35–45. [Google Scholar]
- 44.Capolongo S, Buffoli M, di Noia M, Gola M, Rostagno M. Current Scenario Analysis Improving Sustainability During Hospital Design and Operation. In: Capolongo S, Bottero MC, Buffoli M, Lettieri E, editors. Cham. Springer International Publishing; 2015. pp. 11–22. doi: 10.1007/978-3-319-14036-0_2. [Google Scholar]
- 45.Settimo G, Bertinato L, Bonadonna L, D’Ancona P, Santarsiero A, Soggiu ME. Indicazioni ad interimper la prevenzione e gestione degli ambienti indoor in relazione alla trasmissione dell’infezione da virus SARS-CoV-2. Istituto Superiore di Sanità. Report number: Version of April 21, 2020. 2020 May Available from: https://www.iss.it/documents/20126/0/Rapporto+ISS+COVID-19+n.+5_2020+REV.pdf/2d27068f-6306-94ea-47e8-0539f0119b91?t=1588146889381 . [Google Scholar]
- 46.Lanbeck P, Ragnarson Tennvall G, Resman F. A cost analysis of introducing an infectious disease specialist-guided antimicrobial stewardship in an area with relatively low prevalence of antimicrobial resistance. BMC Health Services Research. 2016;16(1):311. doi: 10.1186/s12913-016-1565-5. doi: 10.1186/s12913-016-1565-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mellace L, Consonni D, Jacchetti G, et al. Epidemiology of Clostridiumdifficile-associated disease in internal medicine wards in northern Italy. Intern Emerg Med. 2013;8(8):717–723. doi: 10.1007/s11739-012-0752-6. [DOI] [PubMed] [Google Scholar]
- 48.Ardoino I, Zangirolami F, Iemmi D, et al. Riskfactors and epidemiology of Acinetobacter baumannii infections in auniversity hospital in Northern Italy: A case-control study. Am J InfectControl. 2016;44(12):1600–1605. doi: 10.1016/j.ajic.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 49.Capobussi M, Sabatino G, Donadini A, Tersalvi CA, Castaldi S. Control of scabies outbreaksin an Italian hospital: An information-centered management strategy. Am JInfect Control. 2014;42(3):316–320. doi: 10.1016/j.ajic.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 50.Prigitano A, Romano L, Auxilia F, Castaldi S, Tortorano AM. Antibiotic resistance: Italianawareness survey 2016. J Infect Public Health. 2018;11(1):30–34. doi: 10.1016/j.jiph.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 51.Montagna MT, Mascipinto S, Pousis C, et al. Knowledge, experiences, and attitudes toward Mantoux test among medical and health professional students in Italy: a cross sectional study. Ann Ig. 2018 Sep-Oct;30(5 Supple 2):86–98. doi: 10.7416/ai.2018.2253. doi: 10.7416/ai.2018.2253. [DOI] [PubMed] [Google Scholar]
- 52.Azzopardi-Muscat N, Brambilla A, Caracci F, Capolongo S. Synergies in Design and Health. The role of architects and urban health planners in tackling key contemporary public health challenges. Acta Bio Medica Atenei Parmensis. 2020;91(3-S):9–20. doi: 10.23750/abm.v91i3-S.9414. doi: 10.23750/abm.v91i3-S.9414. [DOI] [PMC free article] [PubMed] [Google Scholar]


