Abstract
Objectives:
Most patients can tolerate a hemoglobin (Hgb) > 8 g per deciliter. In some cases, however, transfusion will delay physical therapy and hospital discharge. This study aims to review Hgb and transfusion data for a large volume of recent hip fracture patients in order to identify new opportunities for decreasing the length of hospital stay. Our hypotheses are that in some cases, earlier transfusion of more blood will be associated with shorter hospital stays, and that Hgb levels consistently decrease for more than 3 days postoperatively.
Design:
Retrospective chart review.
Setting:
Two academic medical centers with Geriatric Fracture Programs.
Patients:
Data was collected from patients 50 years and older with hip fractures April 2015 and October 2017.
Intervention:
Operative stabilization of the hip fractures according to standard of care for the fracture type and patient characteristics. Transfusion according to established standards.
Main Outcome Measurements:
Electronic records were retrospectively reviewed for demographic information, Hgb levels, and transfusion events.
Results:
One thousand fifteen patients with femoral neck or intertrochanteric hip fractures were identified. Eight hundred sixty met the inclusion criteria. The average length of hospital stay was 6.7 days. The mean patient age was 82 years. The average American Society of Anesthesiologists score was 2.9. The average Hgb level consistently decreased for 5 days postoperatively before beginning to increase on day 6. There was poor consistency between intraoperative Hgb levels and preoperative or postoperative Hgb levels. Three hundred sixty-eight (42.8%) patients were transfused an average of 1.9 (range 1–6) units. One hundred five patients required a transfusion on postoperative day (POD) 1: 72 received only 1 unit of blood: 36 (50%) of the 72 required a second transfusion in the following days, compared to 9 of 33 (27%) who received 2 units on POD 1 (χ2 = 3.8898; P < .05). Patients who received transfusions on POD 3 or later had an average length of stay >2.5 days longer than those who received a transfusion earlier (P = 0.005).
Conclusions:
Our findings do not support earlier transfusion of more blood. Although in some cases, there is an association between earlier transfusion of more blood and shorter hospital stay, routine transfusion of more blood would incur higher transfusion risks in some patients who would not otherwise meet criteria for transfusion. After hip fracture surgery, the Hgb usually decreases for 5 days and does not begin to increase until POD 6. This information will provide utility in the population health management of hip fracture patients.
Level of Evidence:
Level III, Retrospective Cohort Study
Keywords: hemoglobin, hip fractures, population health, transfusions
1. Introduction
Hip fractures in elderly patients are an increasingly important component of health care delivery worldwide. Multiple advancements in the care of these patients have led to reduction in complications, improved outcomes, and better efficiency in costs.[1]
Many hip fracture patients have significant (i.e., Hgb <8 g/dl) anemia or symptomatic anemia and require transfusion of red blood cells (rbc's) in the perioperative period. However, growing concerns about safety, necessity, and cost of rbc transfusions have motivated efforts toward more restrictive transfusion practices.[2–5] It is established that using a hemoglobin (Hgb) level of 8 g per deciliter (g/dl) as a threshold for transfusion in healthy patients will result in fewer transfusions than if a threshold of 10 g/dl is used.[6] The consensus on whether or not it is safe to use restrictive transfusion strategies in hip fracture patients with cardiopulmonary disease continues to evolve.[7]
It is possible that restricting transfusion until a threshold of <8 g/dl is reached will result in more patients with symptomatic anemia and transfusions later in the hospital course, both of which may result in delay of patient discharge. This study aims to review Hgb and transfusion data in a large volume of recent hip fracture patients to determine if earlier transfusion can decrease the length of hospital stay. Our hypotheses are that in some cases, earlier transfusion of more blood is associated with shorter hospital stays, and that Hgb levels continue to fall for more than 3 days postoperatively.
2. Materials and methods
Hospital billing records were used to identify all patients aged 50 years and older[6] with hip fractures (AO/OTA 31-A and 31-B) treated between April 2015 and October 2017 at 2 university-affiliated teaching hospitals. Electronic records were reviewed retrospectively for demographic information, American Society of Anesthesiologists (ASA) score, Hgb levels, transfusion events, indications for transfusion, the time of transfusion, and length of hospital stay. Patients with high-energy injuries (e.g., motor vehicle accidents or falls from a height), polytrauma, pathologic fractures, and pre-existing blood dyscrasias were excluded from analysis.
All patients were comanaged with the Geriatric Fracture Hospitalists with efforts toward early optimization of medical status and early operative stabilization. Patients with intertrochanteric femur fractures were treated with either compression screw and side plate (CPT 27244) or cephalomedullary nailing (CPT 27245) depending on the fracture pattern (e.g., lateral cortical fracture was an indication for cephalomedullary nailing) and on surgeon preference. Nondisplaced or impacted femoral neck fractures were treated with percutaneous screw fixation in situ (CPT 27235). Displaced femoral neck fractures were treated according to patient age and activity level: young healthy patients were treated with closed reduction and fixation (CPT 27235) or open reduction and internal fixation (CPT27236), while less active, older patients were treated with femoral hemiarthroplasty (CPT 27236). Active older patients with displaced femoral neck fractures were treated with total hip arthroplasty, and were not included in this analysis due to the propensity for higher blood loss with reaming of the acetabulum.
All patients received transfusion when their measured Hgb was < 8, or when any signs or symptoms indicative of anemia were present, such as tachycardia, hypotension, mental status changes, dizziness, and postural hypotension. In some cases, the treating surgeon ordered transfusion of more than 1 unit of rbc's based on their assessment of Hgb level, blood loss, and time course, rather than transfusing a single unit and assessing the patient response before deciding to transfuse a second unit. Additionally, patients with borderline preoperative Hgb levels (i.e., Hgb between 8 and 9 g/dl) who had intraoperative hemorrhage that was considered significant in the judgment of the treating surgeon were sometimes transfused intraoperatively.
One thousand fifteen patients with femoral neck or intertrochanteric femur fractures who underwent surgical management were identified during the 31-month period. One hundred fifty-five patients were excluded due to pathologic fracture (47), age <50 years (37), high-energy injury (36), pre-existing blood dyscrasias (15), additional unrelated surgery during same hospitalization (10), significant gastrointestinal hemorrhage during hospital stay (7), and hip fracture that occurred during hospitalization for another problem (3), leaving 860 patients who met the inclusion criteria for the study. There were 363 femoral neck fractures and 497 intertrochanteric femur fractures. The mean patient age was 82 years.
This study has been approved by the University of Rochester Office of Human Subject Protection Research Subjects Review Board, RSRB00069635, Principal Investigator John T. Gorczyca. The use of patient data for research purposes was approved by this committee in accordance with the Declaration of the World Medical Association (www.wma.net) and informed consent from human subjects was not required.
2.1. Statistical Summary
A variety of statistical techniques were used to address the following questions related to the main hypotheses. Welch t test was used to assess: whether or not a patient's ASA scores influenced the number of transfusions received, whether or not a patient's immediate preoperative Hgb levels influenced the number of transfusions needed, whether or not the time (in days) at which a patient received their initial transfusion influenced their length of stay (LOS), and whether or not there was an association between the number of transfusions a patient received and their estimated blood loss. For patients who had intraoperative Hgb levels recorded, Welch t test was used to assess whether or not there was a difference in intraoperative Hgb levels between patient who received and did not receive a transfusion following an operation.
A chi-square test was performed to determine whether or not the number of transfusions a patient received on the first postoperative day influenced that patient's need for future transfusions.
Multivariate regression analysis (Cox regression) was performed to evaluate the effect of patient age, ASA score, procedure, and transfusion on length of stay.
3. Results
3.1. Initial management
Out of 860 patients, 181 (21%) patients had surgery on the calendar day they were admitted. Five hundred sixty-eight (66%) patients had surgery the day after admission. Eighty-two (9.5%) patients had surgery the second day after admission. Chart review of the 29 (3.4%) patients who had surgery after their second day of admission revealed that surgery was delayed due to complex medical issues and slower optimization of their perioperative risk. The average ASA score was 2.94 (Table 1).
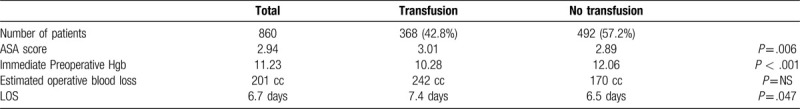
Table 1.
Patient data.
3.1.1. Rate of transfusions
Three hundred sixty-eight (42.8%) patients received at least 1 transfusion; the average units of blood transfused in these patients were 1.9 (range 1–6) units over an average of 1.5 (range 1–5) transfusion events. Forty-eight (5.6%) patients received a preoperative transfusion, 53 (6.2%) patients received an intraoperative transfusion, and 329 (38%) patients received a postoperative transfusion.
3.1.2. Natural history of postoperative hemoglobin levels
For the sample of patients who did not receive a transfusion (492 of 860 patients), the average Hgb level consistently decreased for 5 days postoperatively before beginning to increase on postoperative day 6 (Fig. 1). An analysis of Hgb data, including postdischarge Hgb levels when available, showed an exception—patients discharged on postoperative day 3 had a trend toward an increase in their Hgb on postoperative day 3 (Fig. 2). This was not true for patients discharged after postoperative day 3.
Figure 1.
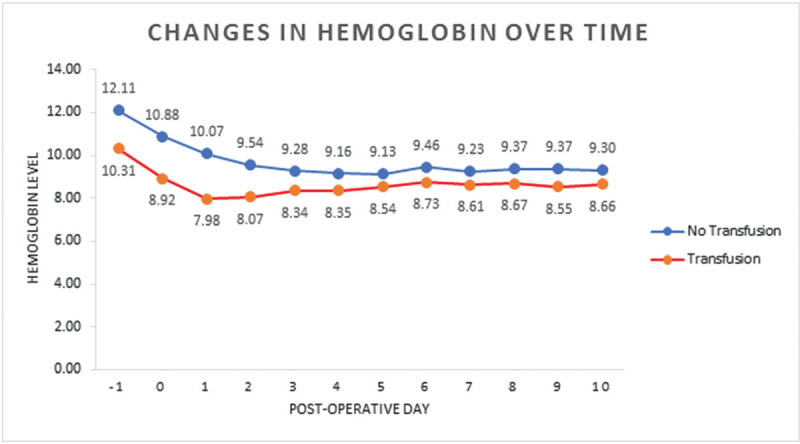
Graph demonstrates the average Hgb level in patients who received transfusion and in those who did not receive transfusion during the course of their hospital stay. In the patients who received transfusion, the average Hgb level began to increase on postoperative day 2, while in the patients who did not receive transfusion, the Hgb continued to decrease for 5 days.
Figure 2.
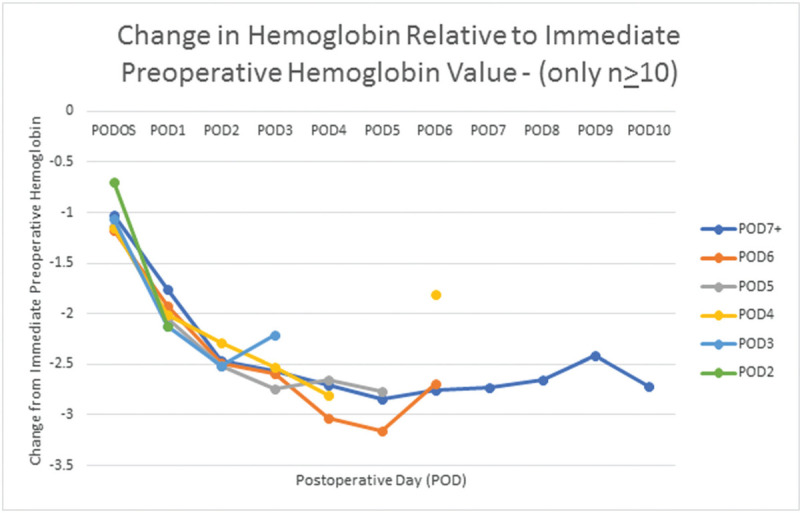
Graph depicts change in Hgb relative to immediate preoperative Hgb value for patients grouped by postoperative discharge date. Patients who were discharged on postoperative day 3 showed a trend toward an increase on that day, but available data shows that average Hgb of patients who were not discharged on postoperative day 3 had an overall progressive decline in Hgb for 5 days. (Postdischarge data is included when available. Points with fewer than 10 recordings were removed in order to simplify the graph).
One hundred seven patients who were not transfused had Hgb data available for both POD 1 and POD 5: 75 (70%) had Hgb that was higher on POD 1 than on POD 5; 26 (24.3%) had Hgb higher on POD 5; and 6 (5.6%) had the same Hgb on POD 1 and POD 5. Eighty-five patients who were not transfused had Hgb levels drawn on both POD 3 and on POD 5: 41 (48.2%) had higher Hgb on POD 3 than on POD 5; 41 (48.2%) had higher Hgb on POD 5; and 3 (3.6%) had the same Hgb on POD 3 and on POD 5.
3.1.3. Influence of procedure
The transfusion rate was 6.5% for CPT 27235; 25.8% for 27236; 36.4% for 27244; and 58.9% for 27245. Despite the difference in transfusion rates among the procedures, the Hgb consistently decreased for 5 days postoperatively for CPT 27235, 27236, and 27244. The Hgb for 27245 consistently decreased for 3 days postoperatively. The average hemoglobin on POD6 remained lower than the average Hgb on POD 1 for all of these procedures (Fig. 3).
Figure 3.
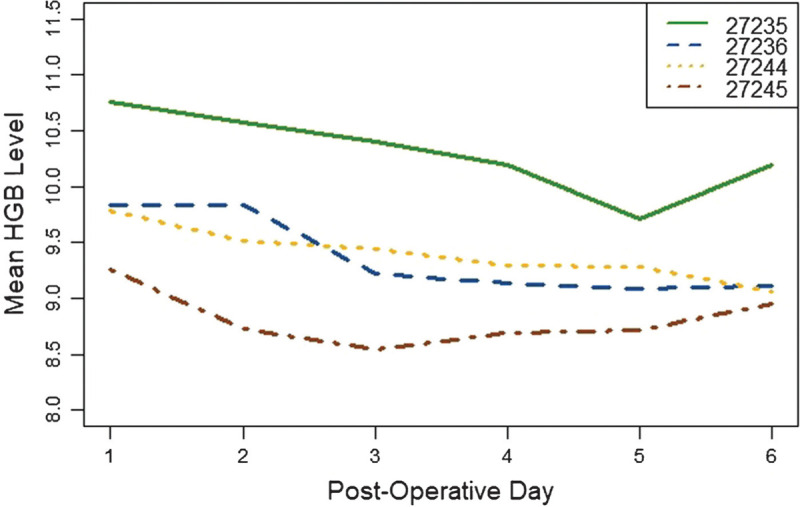
Graph demonstrates Hgb level according to postoperative day for each CPT code. Despite the difference in Hgb levels, 3 of the 4 codes are associated with a steady decline in average HGB for 5 days postoperatively, and the POD 6 average Hgb is lower than the POD 1 Hgb for all of the procedure codes.
3.1.4. Number of transfusions
One hundred five patients met the threshold for an initial transfusion (Hgb <8 or symptoms of anemia) on postoperative day 1: 72 of them were transfused only 1 unit of blood and had an average LOS of 8.1 days: 36 (50%) of these 72 patients required a second transfusion on a subsequent day, and 18 of these 36 (50%) patients required the second transfusion to treat symptomatic anemia. In contrast, 33 patients were transfused 2 or more units on POD 1 and had an average LOS of 6.4 days. Nine of these 33 (27.2%) required additional blood, chi-square = 3.8898 (P<.05).
3.1.5. Hemoglobin level on postoperative day 1 and its predictive value
Analysis of Hgb irrespective of symptoms showed that 178 patients had a Hgb <9 on POD 1, and 98 (55%) of the 178 were transfused on that day or a later date. Eighty-seven patients had a Hgb < 8.4 on postoperative day 1, and 55 (63%) were subsequently transfused.
3.1.6. Late transfusions
The average length of hospital stay was 6.7 days. Patients who received rbc transfusion on POD 3 or later had an average length of stay more than 2.5 days longer (9.1 vs 6.4) than those who received all transfusions earlier than POD3 (P=.005). Their average Hgb on POD 1 was 8.74 g/dL.
3.1.7. Intraoperative blood loss
Estimated blood loss (EBL) averaged 201 cc. For patients who received at least 1 transfusion, the average EBL was 242 cc; the average EBL for patients who did not receive a transfusion was 170 cc (P < .001). We did not find a correlation between estimated intraoperative blood loss and perioperative change in Hgb.
3.1.8. Intraoperative hemoglobin levels
Sixty-one patients had at least 1 Hgb level obtained intraoperatively. Some of these Hgb levels were obtained as part of an intraoperative arterial blood gas measurement that was ordered by the anesthesia team to monitor oxygenation status. Forty-two of these 61 patients did not receive a preoperative or intraoperative transfusion and had a Hgb recorded in the 24 hours before surgery; the average absolute value of the change from the immediate preoperative Hgb level to the intraoperative Hgb level was 1.23 g/dl. Nine (22%) of these 41 patients had an intraoperative Hgb that was higher than their preoperative Hgb. Of the 42 patients who did not receive preoperative and/or intraoperative transfusion, 18 (43%) had postoperative Hgb levels drawn later that same day: the average absolute value of the change was 1.74 g/dl. Six (33%) of these 18 patients had a postoperative Hgb higher than their intraoperative Hgb. Thus, the intraoperative Hgb may be inconsistent with preoperative or postoperative Hgb levels as much as 55% of the time.
3.1.9. Intraoperative transfusion
A total of 53 (6.2%) of 860 patients received transfusion intraoperatively. Most of these were patients with borderline preoperative Hgb levels (between 8 g/dl and 9 g/dl) and intraoperative hemorrhage that was considered significant. Twenty-seven (51%) of these 53 patients also required additional transfusion postoperatively.
3.1.10. Anemia and physical therapy
Three hundred sixty-eight patients (42.8%) received transfusion; 123 (33%) of them missed at least 1 day of physical therapy for various reasons. Fifty-three (16%) of 329 patients who were transfused postoperatively did not receive physical therapy on the date of transfusion. For 22 (7%) of these 329 patients, the anemia and the ongoing transfusion were entirely responsible for the fact that physical therapy did not occur that day. The other 31 (9%) patients had pain in addition to their anemia, and it is not possible to determine from reviewing the records which was more responsible for cancellation of the physical therapy session.
3.1.11. Hospital discharge data
Patients who received a transfusion stayed in the hospital for 7.4 days on average; patients who did not receive transfusion stayed in the hospital for 6.4 days on average (P = .047). Multivariate Cox regression analysis was performed to assess the association between age, ASA score, procedure, and whether or not the patient was transfused (effects) on LOS. There was a positive but clinically insignificant relationship between age and LOS; there were negative but clinically insignificant relationships between ASA and LOS, each procedure and LOS, and transfusion and LOS.
Seven hundred two (82%) of the 860 patients were discharged to a skilled nursing facility at an average of 6.7 days, 104 (12%) were discharged home at an average of 6.0 days, 13 (1.5%) were discharged to hospice at an average of 10 days, 12 (1.4%) were discharged to inpatient rehabilitation at an average of 8.5 days after admission, and 2 (0.2%) were discharged to palliative care at an average of 11 days after admission. Twenty-seven (3.1%) patients expired in the hospital on average at hospital day 12.
4. Discussion
Hip fractures in older patients continue to pose challenges to our health care system due to the overall number of these fractures, the significant morbidity of the injury itself, the association of hip fracture to increasing medical complexity and declining patient health, the risk of complications, and the total economic cost to our society.[1] Ongoing efforts to streamline care and to improve quality are warranted.
The FOCUS study was a large prospective randomized study comparing liberal transfusion (a Hgb threshold of < 10 g/dl) to restrictive transfusion (symptoms of anemia or at physician discretion for Hgb level < 8 g/dl).[7] In the FOCUS study, Carson et al reported fewer postrandomization transfusions in the restrictive group (41%) than in the liberal group (97%), without a statistically significant difference in the risk of cardiopulmonary complications. It should be noted, however, that 28.6% of the patients in the restrictive group had received a transfusion prior to the randomization process. The study showed no difference in the ability of patients to independently walk 10 feet across a room at 60 days postoperatively. The mortality rate did not differ, but the study also showed a higher risk of cardiopulmonary complication in the restrictive group (this was not statistically significant). Other well-designed studies, albeit with fewer patients, have reported higher rates of cardiopulmonary complications in hip fracture patients treated with restrictive transfusion protocols than with liberal transfusion protocols.[8–11]
Despite these reports, several large medical associations, including the American Society of Anesthesiologists, the European Society of Anaesthesiology, the Association of Anaesthetists of Great Britain and Ireland, and the AABB (formerly known as the American Association of Blood Banks), have promoted guidelines advocating restrictive transfusion protocols (i.e., for asymptomatic anemia of Hgb < 8) in all orthopaedic patients.[12–15] However, it is our belief that hip fracture patients differ in many ways from other orthopaedic and nonorthopaedic patients: Hip fracture patients tend to be more frail; they arrive with acute hemorrhage from the fracture; they are often dehydrated or hypovolemic at admission, which can cause their Hgb concentration to appear misleadingly high; and they are more likely to benefit from active participation in physical therapy early in their postoperative course. These differences in patient characteristics and perioperative care plans may provide justification for treating these patients with a less restrictive transfusion strategy.
It is clear that most asymptomatic patients can tolerate a Hgb level as low as 8 g/dl without transfusion. But this study has raised other questions in the care of this population. For instance, if a patient has a preoperative Hgb < 9 g/dl, must the surgeon wait until there is a documented Hgb less than 8 g/dl before giving that patient a transfusion? Further, if a patient has a borderline Hgb level (between 8 g/dl and 9 g/dl) on POD 1, would a transfusion at that time streamline patient care, either by allowing the patient to participate in physical therapy without symptoms of anemia, or by enabling the patient to be safely discharged on an earlier date? We note that the cost of an additional day in the hospital ($2729)[16] is greater than 9 times the cost of a transfusion ($200–300).[17]
It is difficult to compare the risks and benefits of earlier transfusion in these situations. Certainly, cautious transfusion is encouraged within certain guidelines. But in an era in which both the surgeon and the health care delivery system are becoming increasingly responsible for the overall cost of patient care, any factor that may contribute to a shorter hospital stay, or improve active participation in physical therapy, should be evaluated closely.
Our retrospective analysis provides some interesting results. First, after hip fracture surgery, unless the patient receives a transfusion, the Hgb level can be expected to consistently decrease for of the first 5 days after surgery, and in most patients does not begin to increase until postoperative day 6. This supports the concept that asymptomatic patients with Hgb levels close to the transfusion threshold in the early postoperative period (i.e., postoperative day 1 or 2) could be transfused at that time in order to avoid transfusion for symptoms later in their hospital stay, at a time when they might otherwise benefit from participation in physical therapy or be ready for hospital discharge.
Superficial or anecdotal review of postoperative Hgb levels may not be as striking as our data shows because it is easy to mix the postoperative Hgb data from patients who received transfusion with data from patients who did not receive transfusion. This would cause the steady decrease in Hgb over 3 to 5 days postoperatively to be obscured by the increase in Hgb of those patients who received postoperative transfusion. It is only by isolating those patients who did not receive transfusion that the true natural course of Hgb correction in this older population can be understood. Figure 1 shows that, as expected, the average Hgb level begins to increase at an average of 2 days if patients who were transfused are included in the analysis. However, the average Hgb does not start to increase until 6 days postoperatively in the patients who have not received transfusion. Thus, the notion that a borderline low postoperative Hgb level will quickly autocorrect is repudiated.
For patients on whom intraoperative Hgb levels were obtained, we noted high variability when it was compared to preoperative and postoperative Hgb levels. While some variability is to be expected, it seems logical that the Hgb should steadily decrease from the preoperative to the intraoperative and to the postoperative periods. However, the intraoperative Hgb level was higher than the preoperative Hgb in 22% of patients and lower than the postoperative Hgb level in 33% of the patients, even though these patients were not transfused. This challenges the reliability of the intraoperative Hgb level and questions its utility in deciding whether or not to transfuse. This is especially true for intraoperative patients for whom clinical judgment would support transfusion based on relatively low preoperative Hgb and a relatively high estimated operative blood loss.
In our patients, the restrictive transfusion threshold (Hgb <8) advocated by the FOCUS study was strictly followed, and the transfusion rates were comparable if not better (42.8% in our study vs 41% postrandomization plus an additional 28% prerandomization in the FOCUS study); average 0.81 units per patient (all patients, whether or not transfused) in our series vs 1.17 units per patient in the FOCUS restrictive patients. But there were occasions in our series in which physician judgment seemed to have benefit. One example is patients who required transfusion on postoperative day 1—patients who were ordered to receive 2 units of blood instead of 1 unit had a 27% rate of later transfusion, compared with a 50% rate. It should be noted that 50% of the patients who required a later transfusion after receiving only 1 unit on POD1 developed symptoms of anemia. We believe that symptomatic anemia is risky and should be avoided if possible. How to compare higher rate of transfusion risks (i.e., blood borne infection, congestive heart failure, hemolytic reaction) that would be incurred by routinely transfusing all of these patients 2 units to the 25% lower risk of symptomatic anemia and the 23% lower risk of later transfusion is difficult and would require further study. Our study provides this data for physicians to consider when considering the risks and benefits of their transfusion-decisions.
There were 46 patients who did not receive a transfusion until POD 3 or later. These patients had a significantly longer hospital stay (8.23 days vs 6.02 days) than those patients who received their initial transfusion on POD1 (P<.05). These patients had an average Hgb of 8.6 on POD 1, and may have benefited from transfusion at that time, either by leaving the hospital sooner, or simply by having a higher Hgb level and oxygen-carrying capacity earlier. Our data shows that patients with a Hgb <9 on postoperative day 1 have a 55% risk of requiring a transfusion and patients with a Hgb < 8.4 have a 63% rate of subsequent transfusion when using restrictive transfusion criteria. Thus, a “watch and wait” approach to early postoperative anemia can have negative consequences and is not advocated.
Our study has several limitations. First, it is a retrospective study, and despite the large number of patients, the study is limited by this design. Second, we did not evaluate intraoperative crystalloid volume, which could impact the Hgb concentration perioperatively. Our belief is that crystalloid solution infusion rate was adjusted intraoperatively as needed to maintain hemodynamic stability, and that the volume of this fluid that made its way outside of the intravascular space was so highly variable that the measurement of infused crystalloid volume would not provide much useful information. We documented postoperative Hgb by the number of days postoperatively, which covered a span of 24 hours and was theoretically less accurate. It is likely that any inaccuracy in this large series of patients became insignificant with averaging. We recorded ASA score as an indication of patient overall health due to its ease of measurement, although other comorbidity scores may have provided information that is more useful. We did not control for ASA score in the evaluation of the Hgb levels over time. Also, we have limited data available for Hgb levels after patient discharge, so it is impossible to determine if there is a bias in our patients, and that the measured progressive decline in Hgb for 5 days occurred only in patients who are less healthy and thus who remained hospitalized for a longer period of time. It must be noted, however, that the average length of hospital stay was 6.7 days, and only 69 (8%) of the 860 patients were discharged on postoperative day 3, so the available data applies to the great majority of our patients.
Our findings do not support earlier transfusion of more blood. Although in some cases, there is an association between earlier transfusion of more blood and shorter hospital stay, routine transfusion of more blood would incur higher transfusion risks in some patients who would not otherwise meet criteria for transfusion. After hip fracture surgery, the Hgb usually decreases for 5 days and does not begin to increase until POD 6. This information will provide utility in the population health management of hip fracture patients.
References
- 1.Switzer JA, Bozic KJ, Kates SL. Geriatric fracture care: future trajectories: a 2015 AOA Critical Issues Symposium. J Bone Joint Surg Am. 2017;99:e40. [DOI] [PubMed] [Google Scholar]
- 2.Holst LB, Petersen MW, Haase N, et al. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomized trials with meta-analysis and trial sequential analysis. BMJ. 2015;350:h1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carson JL, Stanworth SJ, Roubinian N, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2016;10: CD002042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teng Z, Zhu Y, Liu Y, et al. Restrictive blood transfusion strategies and associated infection in orthopedic patients: a meta-analysis of 8 randomized controlled trials. Sci Rep. 2015;5:13421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brunskill SJ, Millette SL, Shokoohi A, et al. Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev. 2015;4:CD009699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carson JL, Terrin ML, Noveck H, et al. FOCUS Investigators. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gu W-J, Gu X-P, Wu X-D, et al. Restrictive versus liberal strategy for red blood-cell transfusion: a systematic review and meta-analysis in orthopaedic patients. J Bone Joint Surg. 2018;100A:686–695. [DOI] [PubMed] [Google Scholar]
- 8.Carson JL, Terrin ML, Barton FB, et al. A pilot randomized trial comparing symptomatic vs. Hgb-level-driven red blood cell transfusions following hip fracture. Transfusion. 1998;38:522–529. [DOI] [PubMed] [Google Scholar]
- 9.Grover M, Talwalkar S, Casbard A, et al. Silent myocardial ischaemia and haemoglobin concentration: a randomized controlled trial of transfusion strategy in lower limb arthroplasty. Vox Sang. 2006;90:105–112. [DOI] [PubMed] [Google Scholar]
- 10.Foss NB, Kristensen MT, Jensen PS, et al. The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion. 2009;49:227–234. [DOI] [PubMed] [Google Scholar]
- 11.Parker MJ. Randomised trial of blood transfusion versus a restrictive transfusion policy after hip fracture surgery. Injury. 2013;44:1916–1918. [DOI] [PubMed] [Google Scholar]
- 12.American Society of Anesthesiologists Task Force on Perioperative Blood Management Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology. 2015;122:241–275. [DOI] [PubMed] [Google Scholar]
- 13.Kozek-Langenecker SA, Afshari A, Albaladejo P, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2013;30:270–382. [DOI] [PubMed] [Google Scholar]
- 14.Klein AA, Arnold P, Bingham RM, et al. AAGBI guidelines: the use of blood components and their alternatives 2016. Anaesthesia. 2016;71:829–842. [DOI] [PubMed] [Google Scholar]
- 15.Carson JL, Guyatt G, Heddle NM, et al. Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA. 2016;316:2025–2035. [DOI] [PubMed] [Google Scholar]
- 16.KAISER FAMILY FOUNDATION. Hospital Adjusted Expenses per Inpatient Day, 2017, New York State. Available at: https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D accessed December 31, 2019.
- 17.CHOOSING WISELY. Blood Transfusions for Anemia in the Hospital. Available at: https://www.choosingwisely.org/patient-resources/blood-transfusions-for-anemia-in-the-hospital/ accessed December 31, 2019.


