Abstract
Objective:
Understanding the distal (≤ 6 years of age) and proximal (between 6 years of age and early adolescence) factors in adolescent risk behavior is important for preventing and reducing morbidity and mortality in this population. This study sought to investigate the factors associated with the following adolescent risk behaviors: i) aggressiveness and violence, ii) tobacco, alcohol, and illicit substance use, iii) depressive behavior and self-harm (including suicidal ideation and attempts), iv) sexual risk behavior, and v) multiple risk behavior.
Methods:
A systematic review was conducted to identify longitudinal studies that examined factors associated with adolescent risk behaviors. The PubMed, PsycINFO, and LILACS databases were searched.
Results:
Of the 249 included studies, 23% reported distal risk factors, while the remaining reported proximal risk factors. Risk factors were related to sociodemographic characteristics (neighborhood, school, and peers), family patterns, and the presence of other adolescent risk behaviors.
Conclusion:
Distal and proximal factors in adolescent risk behavior that are not exclusively socioeconomic, familial, environmental, or social should be explored more thoroughly.
Keywords: Adolescent behavior, risk factors, risk behavior
Introduction
Adolescent risk behavior is participation in activities that may cause physical or mental harm, such as unintentional injuries and exposure to violence, sexual risk behavior (unsafe sexual behavior that may result in health consequences, such as unintended pregnancy and sexually transmitted diseases), and tobacco, alcohol, and illicit substance use.1 Although such activities are often sporadic, if a consolidated pattern of risky behavior is not identified early and effectively monitored, the individual's health, as well as his or her social and family ties, may be severely harmed.1
There is an increased interest in studying risk behavior in adolescents due to its high correlation with morbidity and mortality.1-3 These behaviors may also directly affect an individual’s human capital, i.e., the set of educational and cultural assets that determine his or her well-being over time.2,3 Thus, a better understanding of the factors in adolescent risk behavior is important for interventions to prevent this pattern of behavior in adult life. In addition, those who engage in any one risk behavior are likely to engage in others, and the behaviors may have common factors that predict their development. Hence, a growing body of research suggests that health risk behaviors often do not occur in isolation. Smoking, drinking, illicit drug use, sexual risk taking, and aggression are all mutually predictive.4
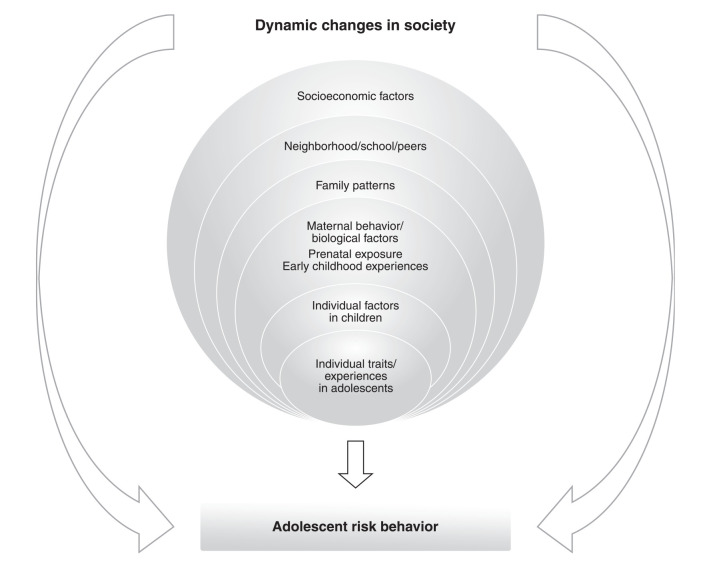
Theoretical models can clarify the dynamics of factors that influence the onset and perpetuation of risk behaviors. The Developmental-Ecological Framework, for example, posits that individual development and behaviors are influenced by the adolescent’s social environment (e.g., family, school, and neighborhood).5 Some health programs,6 designed to prevent and treat specific risk behaviors in adolescence, are guided by the Social Development Model,7 which postulates that children and adolescents shape their attitudes from four socializing units: family, school, religious and community institutions, and peers. There is also evidence that individual personality traits and temperament are determinants of specific behaviors.8 A theoretical model is shown in Figure 1.
Figure 1. Theoretical model of risk behavior factors.
The majority of studies on the factors involved in adolescent risk behaviors are cross-sectional or focused on proximal factors, i.e., those that occur after early childhood (before age 6, a critical and sensitive period of development).9,10 In addition, few studies have established a direct causal relationship between exposure (risk factor) and outcome (risk behavior). This systematic review will allow a description of the factors associated with adolescent risk behavior in the literature, as well as those that still require investigation. In-depth knowledge of the factors associated with adolescent risk behaviors could help prevent them, consequently reducing morbidity and mortality in this age group.
Although many systematic reviews have been conducted on adolescent risk behavior and its associated factors, they have generally studied the factors associated with a single behavior or the association between several behaviors and a single factor.11-15 Furthermore, no systematic review has used only longitudinal studies to assess the main adolescent risk behaviors and all associated factors. Hence, the aim of this report is to review the literature on distal and proximal factors associated with adolescent risk behaviors (sexual risk behavior, violent/aggressive behavior, substance use or abuse, depressive/suicidal behavior and self-harm, and multiple risk behavior – i.e., two or more of the aforementioned risk behaviors) and to provide an overview of the subject.
Methods
Protocol and registration
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.16 The study protocol has been published in the PROSPERO registry (CRD42018092963).
Information sources
A comprehensive literature search of the electronic databases PubMed, PsycINFO, and Lilacs was conducted from February 16, 2018 to August 9, 2018.
Search strategy and study eligibility
The articles were retrieved through the following search strategies: 1) on PubMed: (Adolescent Behavior OR Behavior, Adolescent OR Adolescent Behaviors OR Behaviors, Adolescent) AND (Risk Factors OR Factor, Risk OR Factors, Risk OR Risk Factor OR Population at Risk OR Risk, Population at OR Populations at Risk OR Risk, Populations at OR Pregnancy in Adolescence OR Alcohol Drinking OR Alcohol Drinking in College OR Binge Drinking OR Underage Drinking OR Aggression OR Substance-Related Disorders OR Tobacco Use OR Depressive Disorder OR Suicidal Ideation); 2) on Lilacs: Adolescent behavior AND Risk Factors; and 3) on PsycINFO: Adolescent behavior AND Risk factors.
The articles were grouped and structured according to the PICOS strategy: P (population) people between 10-19 years old, defined as adolescents by the World Health Organization17; I (intervention/exposure) related to factors associated with risk behaviors; C (comparison) for absence of risk behavior; O (outcome) risk behaviors, such as substances use, including alcohol and smoking tobacco, sexual risk behavior, aggressiveness and violence, self-harm, depressive and suicidal behavior; multiple risk behavior; and S (study design) longitudinal studies. These outcomes have been described as the most prevalent risk behaviors in adolescence. For instance, the prevalence of hazardous drinking is 34% among 15- to 16-year olds.18 In addition, smoking, aggression, and, depression affect an individual’s entire life cycle and negatively impact health in adulthood.19 Although a mental health problem, we included depressive symptoms due to their strong association with other risk behaviors, such as self-harm, suicidal ideation, substance use, and sexual risk behavior.20 The exclusive selection of longitudinal studies enabled us to examine factors that predict risk behaviors in adolescence, and also allowed us to ensure that the exposure occurred before the outcome, even for studies focusing on proximal risk factors, whose follow-up period is shorter than that of studies focusing on distal factors (i.e., those occurring in the first 6 years of life).21 Proximal risk factors were considered those that occurred prior to the outcome but after early childhood, and they can be described in retrospective or prospective studies.
Study selection
The search strategy we used for each database covered the maximum number of articles, and the selection process included several steps. First, the titles and abstracts were screened. Next, we excluded articles that did not fit the selection criteria or were duplicates; two investigators independently screened the article titles and abstracts. Potentially relevant articles were then retrieved, and two investigators independently assessed the full texts to determine which ones met the eligibility criteria. Further information about which authors performed each step is available in the online-only supplementary material (author contributions (132KB, pdf) ).
Risk of bias in individual studies
Two investigators independently assessed the risk of bias of the included studies with the Newcastle-Ottawa Scale (NOS) for cohort studies.22 The NOS uses eight criteria to evaluate selection bias, cohort comparability, and outcome assessment, and has been used in another risk behavior-related review.23,24 The NOS quality assessment form for cohort studies classifies them as good quality, fair quality, or poor quality. NOS classification considers the quality of the following criteria: population selection, comparability, and outcome assessment. Poor quality means zero points in any one of these three criteria. Of note, according to the PRISMA statement, NOS quality should not be considered as an exclusion or inclusion criterion for a systematic review. Thus, no studies were excluded exclusively on NOS quality classification.
Data collection process
Two investigators extracted the data (study design, setting, population, risk behavior, associated risk factors, follow-up period, results, adjustment variables, covariates, and NOS score) from the articles. The data obtained from the selected studies were included in a summary table, and a descriptive analysis was performed. Adjusted results were reported when possible. Due to the studies’ heterogeneity, such as different populations, the number of risk behaviors, and risk factors, no meta-analysis was attempted.
Results
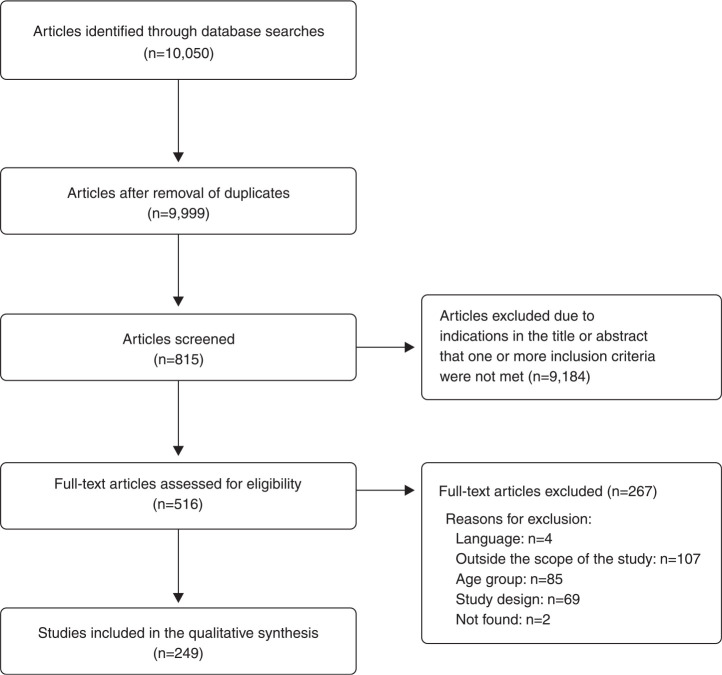
The database searches identified 10,050 article titles and, after removing duplicates, 815 titles and abstracts were screened. The full text of 516 articles was assessed for eligibility and 249 studies met the inclusion criteria. The complete flowchart is shown in Figure 2.
Figure 2. Study selection flowchart.
Descriptive analysis
A summary of the results is described in Table 1. The detailed results are presented in Table S1 (132KB, pdf) , available as online-only supplementary material.
Table 1. Summary of the 249 eligible studies.
| Risk behavior | ||||||
|---|---|---|---|---|---|---|
| Characteristic | All studies (n=249) | Substance use (n=113) | Aggressiveness and violence (n=35) | Self-harm, depressive, suicidal behavior (n=54) | Multiple risk behavior (n=21) | Sexual risk behavior (n=26) |
| Country | ||||||
| United States | 112 (45.0) | 48 (42.0) | 23 (65.7) | 19 (35.0) | 7 (33.0) | 15 (57.6) |
| United Kingdom | 37 (15.0) | 14 (12.0) | 2 (5.7) | 16 (29.6) | 2 (9.5) | 3 (11.5) |
| Australia | 24 (10.0) | 13 (12.0) | 3 (8.6) | 4 (7.4) | 2 (9.5) | 2 (7.9) |
| Other | 76 (30.0) | 38 (34.0) | 7 (20.0) | 15 (28.0) | 10 (48.0) | 6 (23.0) |
| Sample age (years) | ||||||
| 10-14 | 96 (38.5) | 51 (45.1) | 14 (40.0) | 18 (33.4) | 8 (38.0) | 5 (19.0) |
| 15-19 | 78 (31.4) | 29 (25.7) | 9 (25.7) | 19 (35.1) | 6 (28.5) | 15 (58.0) |
| Other | 75 (30.1) | 33 (29.2) | 12 (34.3) | 17 (31.5) | 7 (33.5) | 6 (23.0) |
| Years of follow-up | ||||||
| ≤ 10 | 193 (77.5) | 90 (79.6) | 22 (63.0) | 44 (81.5) | 13 (62.0) | 24 (92.3) |
| > 10 | 56 (22.5) | 23 (20.4) | 13 (37.0) | 10 (18.5) | 8 (38.0) | 2 (7.7) |
| Exposure | ||||||
| Distal risk factor | 56 (22.5) | 24 (21.2) | 15 (43.0) | 8 (14.8) | 7 (33.0) | 2 (7.7) |
| Distal protective factor | 3 (1.2) | 2 (1.8) | - | - | - | - |
| Proximal risk factor | 191 (76.0) | 88 (78.0) | 20 (57.0) | 44 (81.5) | 14 (67.0) | 25 (96.2) |
| Proximal protective factor | 5 (2.0) | 2 (1.8) | 1 (3.0) | 2 (3.7) | - | - |
| Study design | ||||||
| Prospective | 237 (95.0) | 109 (96.5) | 31 (88.5) | 53 (98.0) | 20 (95.0) | 24 (92.3) |
| Retrospective | 12 (5.0) | 4 (3.5) | 4 (11.5) | 1 (2.0) | 1 (5.0) | 2 (7.7) |
Data presented as n (%).
Sample characteristics
The majority (90%) of the studies included in this review analyzed both boys and girls, although approximately 7% included only girls, particularly studies on sexual risk behavior such as pregnancy in adolescence. In almost 40% of the studies, the sample included adolescents aged 10 to 14 years at outcome, while 62.2% used self-report questionnaires as a survey method.
Source/country
Of the 249 included longitudinal studies, 45% (112) were conducted in the United States, followed by the United Kingdom (15%) and Australia (10%). Only eight studies were included from South America (3%): four from Brazil, two from Mexico, and two from Chile. The other studies were conducted in Canada, Malaysia, Finland, Sweden, Denmark, Germany, Taiwan, Korea, China, South Africa, Tunisia, and Mauritius. Four studies were multicenter, three of which were conducted in Europe.
Newcastle-Ottawa Scale quality
Of the 249 studies, 151 (60.6%) were classified as good quality, 64 (25.7%) as fair quality, and a minority (13.7%) as poor quality.
Prospective vs. retrospective cohort studies
Regarding study design, 12 of the included studies (5%) were retrospective cohort studies and 237 (95%) were prospective cohort studies.
Year of publication
The minority (12.5%) of the studies were published between 1994 and 1999, whereas the majority were published between 2000 and 2018.
Risk behavior and its associated factors
The most frequent main outcome (risk behavior) was substance use, including alcohol and tobacco (45%), followed by depressive/suicidal/self-harm behavior (21.6%), violent or aggressive behavior (14%), sexual risk behavior (11%), and two or more risk behaviors (8.4%).
Only 23% (56) of the studies reported early childhood factors (including intrauterine factors) associated with adolescent risk behavior, mainly those related to aggressive behavior, and the majority were prospective cohort studies. Almost 80% of the included studies were restricted to proximal exposure (after the first 6 years of life), which involved shorter follow-up times.
The main early childhood factors associated with adolescent risk behavior were nicotine exposure during pregnancy, low socioeconomic status at birth, and adverse childhood experiences, such as prenatal exposure to drugs and poverty.8,25-28 Individual traits, such as internalizing and externalizing symptoms in the first 6 years of life, were also addressed in some studies as predictors or mediators of adolescent risk behaviors.29-32 Intrauterine exposure to alcohol, cocaine, lead, caffeine, and dexamethasone were also addressed in a few studies.33-37 Birth conditions (low birth weight, prematurity, delivery complications),38-40 family emotional expressiveness (such as maternal attitudes to pregnancy and postpartum care),41 and maternal depression in the child’s early life were rarely described as risk factors for adolescent risk behavior.42
The included studies examined 44 different (distal and proximal) types of factors. The following sections describe the factors significantly associated with each adolescent risk behavior in the majority of the articles.
Alcohol and other substance use
The distal risk factors for adolescent alcohol use were: intrauterine alcohol exposure (in one study it was only significant for girls,35 while in another it was significant for both sexes),43 maternal depression in early childhood, low maternal age at birth, cumulative adverse experiences in early childhood, externalizing symptoms, and low family income at birth.44 However, Melotti et al.45 reported a higher family income at birth as a risk factor for adolescent drinking. The mother’s negative feelings about being pregnant and having an unwanted/unplanned pregnancy predicted alcohol initiation by age 14.41 Edwards et al.29 found that internalizing symptoms in childhood were distal protective factors against adolescent drinking.
Proximal risk factors for adolescent alcohol use included: sibling and peer alcohol use, residing in an urban area, parental alcohol use or abuse, parental separation, and a single mother family. Parental style (overprotection) was associated with regular alcohol use in adolescence.46-48 Prior behavior problems predicted alcohol initiation by age 11-13.49 Smoking, easy access to alcohol, and truancy were associated with alcohol consumption by age 14.50 Bullying victimization was positively associated with drinking and risky drinking. Externalizing symptoms (maladaptive behaviors directed toward one’s environment) by age 8 (after early childhood), low locus of control, depressive symptoms, poor parental attachment, and low school connectedness were significantly associated with alcohol use. Early puberty and low sports participation increased the risk of binge drinking.51-54 An important proximal protective factor for alcohol use was more family meals and a secure adolescent-parent attachment.47 High socioeconomic status and an authoritarian parental style were also protective factors against binge drinking.55
No distal risk factors were described regarding onset of cannabis use. Proximal factors, such as knowing slang words for cannabis, signaled a markedly increased risk for subsequent cannabis use.56 Prior history of smoking, alcohol consumption, antisocial behavior, intention to use drugs, drug use among friends, and spending leisure time in bars were independent risk factors for cannabis use in both sexes.56 Maternal smoking, friends who smoke tobacco, low parental monitoring, and having smoked tobacco by age 11 were risk factors for cannabis use by age 17-18.57,58 Regarding the use of other substances, males with conduct problems were at higher risk of using multiple substances (cocaine, alcohol, cannabis), and early puberty was positively associated with substance use in middle adolescence for both sexes.49
Smoking tobacco
The distal risk factors for smoking in adolescence were: behavioral and emotional problems during infancy, maternal smoking during pregnancy (in several good quality studies), boys born to single mothers, girls with high stress at age 3, and exposure to maternal depression at 4-5 years old.25,28,59
The proximal risk factors for smoking in adolescence were: child depression, maternal depression, current maternal smoking, peer drug use, parental separation, thrill seeking behavior, stress, other risk behaviors, and the father’s use of snus (Swedish snuff).60,61 In addition, exposure to tobacco advertising was associated with smoking in adolescence, even after controlling for socioeconomic factors. Low self-esteem in girls was a predictor of smoking.62 Poor academic performance, parental smoking, and having friends who smoke all independently predicted heavy smoking.61,63,64 Depression and prior cigarette consumption were associated with smoking in adolescence.65 Fights, previous experience with alcohol, an absent father, male gender, a poor relationship with the mother, corporal punishment by parents, and family conflict were associated with smoking in adolescence (by 11.3 years of age).66,67 Early puberty in both sexes was an independent risk factor for regular smoking in adolescence. Although attention deficit and hyperactivity disorder symptoms were associated with smoking in adolescence, this relationship was mediated by school adjustment.68 Using e-cigarettes in the past 30 days was associated with initiation of smoking and daily smoking.69 Water-pipe smoking increased the risk of conventional smoking.70 Barriers to smoking in public places, negative perception of the tobacco industry, and nonsmoking policies were described as proximal protective factors against smoking in adolescence.71 Unlike the majority of literature, De Vries et al.72 concluded that peer smoking was not a predictor of smoking in adolescence, and justified the result as a selection paradigm: adolescents choose friends with similar tobacco-related behaviors.
Depressive/suicidal/self-harm behavior
The distal risk factors for depressive behavior in adolescence were: shyness at age 6, child abuse or neglect in early childhood, low birth weight, number/frequency of real and/or perceived physical issues, and internalizing problems.73,74 Prematurity (less than 26 weeks) was a risk factor for depressive symptoms at age 11.38 Prenatal maternal depression was a predictor of adolescent depressive symptoms, after controlling for variables such as maternal education, maternal age at delivery, gender, smoking, and alcohol use during pregnancy.42 Maternal consumption of more than eight cups of tea or coffee per day during pregnancy was associated with depressive disorder at age 11, even after adjusting for covariates.37 Locus of control mediated the association between socioeconomic adversity in infancy and depression in adolescence.75 Compared to hydrocortisone or nothing, dexamethasone exposure at birth was reported as a risk factor for depressive behavior in adolescence.74 No distal protective factors against depressive behavior in adolescence were described.
The proximal risk factors for depressive symptoms in adolescence were a socioeconomically disadvantaged neighborhood and having experimented with drugs. Having engaged in two or more health risk behaviors predicted depressive symptoms (adjusted for age, ethnicity, obesity, and general health status).76 Low school connectedness, lack of parental affection, parental conflict, parental separation, cyberbullying victimization, bullying victimization by age 15, female gender, low income, low levels of religious activity, and no suicidal self-injury were risk factors for depressive behavior during adolescence.77,78 Self-identification as a goth at age 15 was associated with depression at age 18.79 Family connectedness, parental warmth, peer acceptance, better school performance, and religious activity were reported as proximal protective factors for depression.77 Maternal depression and ongoing anxiety were not associated with depression in adolescence.42
Concerning the distal risk factors for self-injury and suicidal behavior: emotional disorders in early childhood were cited as a risk for later suicidal ideation and suicide attempts, adoption was an independent risk factor for attempted suicide in adolescence, and low socioeconomic status at birth was also associated with self-harm without suicide attempt at age 16.80 No distal protective factors were described.
The proximal risk factors for self-injury included: involvement in violence at age 14 (associated with suicidal ideation one year later),81 health problems (e.g., muscle pain and tension, overweight), and conduct problems at age 9 (associated with suicidal ideation at age 15).82 Depression, parental conflict, other risk behaviors (e.g., smoking), anxiety at age 9, being a male bullying victim, and being a female bully were risk factors for posterior suicidal ideation.83 Exposure to frequent bullying, poor school connectedness, poor neighborhood safety and cohesion, and maternal suicidal intent were associated with self-harm.84,85 Being adopted was an independent risk factor for attempted suicide in adolescence. Self-identification as a goth at age 15 was associated with self-harm at age 18.77 Violent methods of self-harm were independently associated with attempted suicide.86
Aggressive/violent behavior
The distal risk factors for aggressive behavior in adolescents were: prenatal exposure to lead,33 early childhood exposure to family violence and alcohol abuse, and child abuse (regardless of whether it occurred at home or in foster care).87 In addition, intrauterine exposure to tobacco was associated with delinquency at age 12.88 Maternal alcohol consumption during pregnancy was associated with antisocial behavior in adolescence. Gestational hypertension and preeclampsia were positively associated with aggressive behavior at age 14.38 Birth complications, psychosocial adversity, abuse, maladaptive parental behavior, socioeconomic disadvantage, and malnutrition were distal risk factors for aggressive behavior and delinquency, and externalizing symptoms in infancy were described as a mediator.89 Other early factors included: exposure to maternal depressive symptoms at 4-5 years of age, unplanned pregnancy, maternal urinary tract infection during pregnancy, low maternal education, and being born to a single mother. Low maternal age and having three or more siblings (associated with aggressive behavior at age 11).90 Childhood exposure to violence and parental rejection were associated with violent behavior at age 16.91 Maternal consumption of more than eight cups of tea or coffee per day during pregnancy was associated with conduct/oppositional disorder at age 11, even after adjusting for a number of covariates.37
The proximal risk factors for aggressive behavior in adolescence described in the included studies included neighborhood socioeconomic disadvantage, current access to guns, male gender, depression, tobacco use, substance use, disruptive behavior in early adolescence, early substance use, early puberty, hyperactivity, poor academic performance, peer delinquency, availability of drugs in the neighborhood, perceived discrimination, and parental separation in early adolescence.92-96
Sexual risk behavior
The distal risk factors for sexual risk behavior in adolescence were childhood sexual abuse,95,97 persistent conduct problems during childhood, low income, and low maternal education. Low maternal age at delivery and behavioral and emotional problems at age 5 were risk factors for early sexual activity (before 16 years of age).31,32,92,98 Externalizing problems at age 2 increased the risk of unwanted sex (not forced but not spontaneously desired) at age 15 for girls, and the risk of multiple sexual partners for boys.32 Attention deficit and hyperactivity disorder, oppositional defiant disorder, and conduct disorder were associated with sexual intercourse before 16 years of age.99 The proximal risk factors for sexual risk behavior in adolescence were: lack of interests outside the home at age 13 and no religious activity at age 11. Low school connectedness at age 15 and a diagnosis of conduct disorder were described as risk factors for sexual activity before 16 years of age in males.100 For females, high self-esteem, early menarche, planning to quit school, and low school connectedness were risk factors for early sexual activity.100 Low maternal monitoring, high older sister power, and low sibling conflict were factors for sexual risk behavior 3 years later.101 Having a previous sexually transmitted disease was a risk factor for contracting a new one in adolescence.102 Marijuana use by one of the partners was found to be a risk factor for not using condoms.103 Risk factors for adolescent pregnancy included: a positive desire to become pregnant, early conduct problems, less than 8 years of education, multiple sexual partners, and being single.104,105 Finally, a higher level of parental monitoring and good grades were proximal protective factors for sexually transmitted diseases such as gonorrhea and chlamydia.102
Multiple risk behavior
The distal factors of multiple risk behavior were adverse childhood experiences, including low family income (assessed when the child was 2-4 years of age), and other social determinants, such as low maternal education level.18 In relation to proximal factors in multiple risk behavior, low parental social class, low maternal education, and low household income were directly and significantly associated with more risk behaviors at age 15.18
Discussion
Distal risk factors
In this review we have described three basic ways in which the lifelong effects of distal factors impact a child’s future health and behavior: i) prenatal factors, such as maternal depression, tobacco, alcohol, caffeine, and other substance use during pregnancy; ii) birth conditions, such as prematurity and low birth weight; iii) experiences during early life, such as adverse experiences (abuse, neglect, family violence, adoption), low family income, and maternal or caregiver emotional problems.35,41,43,44
Hence, the majority of the distal factors in adolescent risk behavior described in this study could be considered social determinants of health, i.e. the nonmedical conditions in which people are born, mature, work, live, and age, and the broader set of forces and systems that shape the conditions of daily life.106 These nonmedical conditions, such as sustained poverty, low parental education, and family violence, determine patterns that can negatively impact the environment in which children are born, live, and mature, thereby influencing their health, development, and well-being.107-109
Distal protective factors
Protective factors mediate or moderate the effect of exposure to risk factors, resulting in a reduced incidence of the problem behavior.110 These protective factors for behavior outcomes in adolescence fall into three basic categories: individual traits (positive social orientation, high intelligence, and a resilient temperament), social bonding (warmth, affective relationships, and commitment), and healthy behavior patterns. There is a consensus that during early childhood, having good affective experiences and bonds, as well as growing in a stable and safe environment, improves emotional development and, consequently, has a positive impact on mental health and behavior during adolescence and adulthood.111
However, in this systematic review, few studies reported on distal protective factors for risk behaviors in adolescence; only two reports (both concerning substance use) described distal protective factors. No studies investigated distal protective factors, such as the quality of the mother-child bond or breastfeeding duration, for instance. The literature found in this review was more focused on the factors involved in risk behaviors. Perhaps this finding could be explained by evidence from previous epidemiological studies indicating that health programs and policies for children and youth should focus only on risk factors to reduce the prevalence of problem behavior in adolescence.112,113 Nevertheless, some authors have advocated focusing exclusively on protective factors associated with resilience, rather than trying to reduce risk factors, i.e., emphasizing “prevention” rather than the “problem.”114,115 Other authors have argued that focusing solely on protective factors ignores the importance of social and contextual risk factors, which should also be considered in prevention policies and interventions.116
Proximal risk factors
The proximal factors for adolescent risk behavior described in this systematic review are well established in the literature, and are basically synonymous with social determinants of health. They could be divided into structural determinants, which are the fundamental structures of society that create social stratification (such as national wealth, income inequality, educational status, gender, and ethnicity), and proximal or intermediate determinants, which are considered the circumstances of daily life (such as the quality of the family environment, peer relationships, the availability of food, housing, recreation, and access to education).117 Proximal factors are created by social stratification (i.e., structural determinants), as well as by cultural, religious, and community factors. There is strong evidence that these proximal social and educational factors affect the vulnerability and exposure of young people to health risk behaviors and conditions. This evidence is derived from traditional efforts to prevent substance abuse, sexual risk behavior, violence, delinquency, and poor mental health in adolescence.118,119
The family has an important role in proximal factors: low parental monitoring, parental conflict, and sibling conflict are factors in several risk behaviors.77,78,101 In high-income countries, disadvantaged neighborhoods have been associated with poor educational attainment,120 teenage pregnancy,121 poor mental health,122 and violence in adolescence. Peers also play a crucial role: the emergence of strong peer relationships is one of the key developmental changes of early adolescence, and peers can have a positive or negative influence on behavior.123 Finally, individual traits, such as other risk behaviors or a mental disorder, are frequently described as factors for risk behaviors.76,102
Thus, sociodemographic factors, family patterns, neighborhood, peers, risk behavior, and mental disorders are currently the most studied determinants of adolescent risk behavior. Health policies must combine interventions at the individual, school, and family levels. Individual traits, such as low self-esteem,62 early puberty,49 and other physical problems,82 were rarely described as factors associated with risk behaviors. These individual risk factors require further investigation since, given the difficulty of intervening in environmental, neighborhood, and family structures, health professionals could work directly with adolescents.
Proximal protective factors
According to Rutter,124 protective factors and risk factors should be treated as conceptually distinct rather than as opposite ends of a single dimension. Thus, protective factors are considered independent variables that can have their own effects on behavior but can also moderate the relation between risk factors and behaviors.125 Hence, protective factors could play a key role when exposure to risk is unavoidable and essentially constant. Several protective factors for behavioral outcomes have been explored. The literature reports125,126 three categories of protective variables:
i) dispositional attributes, that is, individual differences, such as high self-efficacy; ii) family attributes, such as parental support and affection; and iii) extrafamilial circumstances, such as support from other adults or strong community integration.
In this review, proximal protective factors for risk behaviors were poorly reported, and no proximal protective factors were described for multiple risk behavior or sexual risk behavior. Furthermore, the majority of the reported proximal protective factors were either “extrafamilial circumstances” (e.g., nonsmoking policies, peer acceptance, better school performance, religious activity) or “family attributes” (e.g. parental warmth and parental style). It has become evident that adolescents whose parents are highly knowledgeable about their activities are less likely to engage in problem behavior, including sexual risk behaviors,101 violence,96 and substance abuse.47 In the present review, we found that individual protective factors for risk behaviors have been poorly explored. These should be more thoroughly investigated, since they could be used to promote resilience and reduce risk behavior in adolescents.
Strengths and limitations
This review followed the recommended procedures for rigorous systematic reviews. To identify as many relevant studies as possible and reduce the risk of publication bias, a highly sensitive search strategy was used and an extensive range of resources were searched, including electronic databases, guidelines, and systematic reviews. Another important strength was the fact that only longitudinal studies were included. This has enabled us to examine factors that predict risk behaviors in adolescence and ensured that exposure occurred before the outcome. Furthermore, our results align with previous findings, and the majority (almost 80%) of the included studies presented an adjusted analysis for covariates, which reduces confounding and strengthens the causal inference between exposure and outcome. Another advantage is the high number of included studies from a broad variety of locations and populations, amplifying consistency and also contributing to causal inference.127
Despite the selection and information biases implicit in cohort studies, the NOS criteria were applied to each included study, ensuring the quality of the results and an awareness of bias. Although the majority of the included studies (60%) were classified as good quality with low risk of bias, almost half (40%) were classified as fair or poor quality, which indicates an increased risk of selection and information biases. This could be considered a limitation.
Conclusions
This systematic review found few reports on distal factors in adolescent risk behavior, particularly medical factors, such as gestational and delivery complications, and emotional and/or psychological problems during early childhood. We also found that distal protective factors for risk behavior in adolescence were poorly explored, since only two reports described distal protective factors for substance use (both related to socioeconomic status at birth). No reports were found on distal risk factors for other risk behaviors, such as aggressiveness, sexual risk behavior, depressive and suicidal behavior, or self-harm, and no studies investigated an association of factors (such as mother-child bond, breastfeeding duration, maternal emotional status during and after pregnancy, and maternal emotional support during and after pregnancy) with risk behaviors in adolescence, for instance. Finally, the physical and psychological traits of individual adolescents were rarely investigated as proximal factors for risk behaviors. The literature focuses much more on social, environmental, school, neighborhood, and family factors. Individual traits should be better explored, since they could be an easier and proximal target for intervention by health professionals.
Recommendations
Public policies that aim to prevent risk behaviors in adolescence should intervene in the social determinants of health, since they are significantly associated with several risk behaviors in adolescence. Nevertheless, the distal and proximal risk and protective factors for risk behaviors in adolescence, whether medical, psychological, or individual, cannot be forgotten by researchers, since interventions in these determinants could be promoted not only through public health policies, but also by pediatricians, obstetricians, and other health professionals in the primary care system.
Disclosure
The authors report no conflicts of interest.
Acknowledgements
This study was funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) scholarship.
Footnotes
How to cite this article: Bozzini AB, Bauer A, Maruyama J, Simões R, Matijasevich A. Factors associated with risk behaviors in adolescence: a systematic review. Braz J Psychiatry. 2021;43:210-221. http://dx.doi.org/10.1590/1516-4446-2019-0835
References
- 1.Kipping RR, Campbell RM, MacArthur GJ, Gunnell DJ, Hickman M. Multiple risk behaviour in adolescence. J Public Health. 2012;34(Suppl 1):i1–2. doi: 10.1093/pubmed/fdr122. [DOI] [PubMed] [Google Scholar]
- 2.Feijó RB, Oliveira EA. [Risk behavior in adolescence] J Pediatr (Rio J) 2001;77(Suppl 2):S125–34. doi: 10.2223/jped.300. [DOI] [PubMed] [Google Scholar]
- 3.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth risk behavior surveillance - United States, 2007. MMWR Surveill Summ. 2008;57:1–131. [PubMed] [Google Scholar]
- 4.Guilamo-Ramos V, Litardo HA, Jaccard J. Prevention programs for reducing adolescent problem behaviors: implications of the co-occurrence of problem behaviors in adolescence. J Adolesc Health. 2005;36:82–6. doi: 10.1016/j.jadohealth.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 5.Bronfenbrenner U. The ecology of human development. Cambridge:: Harvard University;; 1979. [Google Scholar]
- 6.Hawkins JD, Brown EC, Oesterle S, Arthur MW, Abbott RD, Catalano RF. Early effects of communities that care on targeted risks and initiation of delinquent behavior and substance use. J Adolesc Health. 2008;43:15–22. doi: 10.1016/j.jadohealth.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Catalano RF, Hawkins JD. The social development model: a theory of antisocial behavior. In: Hawkins JD, editor. Delinquency and crime: current theories. Cambridge: Cambridge University; 1996. pp. 149–97. p. [Google Scholar]
- 8.Mason WA, Patwardhan I, Smith GL, Chmelka MB, Savolainen J, January SA, Järvelin MR. Cumulative contextual risk at birth and adolescent substance initiation: peer mediation tests. Drug Alcohol Depend. 2017;177:291–8. doi: 10.1016/j.drugalcdep.2017.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bird Y, Moraros J, Olsen LK, Coronado GD, Thompson B. Adolescents' smoking behaviors, beliefs on the risks of smoking, and exposure to ETS in Juarez, Mexico. Am J Health Behav. 2006;30:435–46. doi: 10.5555/ajhb.2006.30.4.435. [DOI] [PubMed] [Google Scholar]
- 10.Hockenberry JM, Edward JT, Weg MK. Smoking, parent smoking, depressed mood, and suicidal ideation in teens. Nicotine Tob Res. 2010;12:235–42. doi: 10.1093/ntr/ntp199. [DOI] [PubMed] [Google Scholar]
- 11.Buhi ER, Goodson P. Predictors of adolescent sexual behavior and intention: a theory-guided systematic review. J Adolesc Health. 2007;40:4–21. doi: 10.1016/j.jadohealth.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 12.Rew L, Wong YJ. A systematic review of associations among religiosity/spirituality and adolescent health attitudes and behaviors. J Adolesc Health. 2006;38:433–42. doi: 10.1016/j.jadohealth.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Ryan SM, Jorm AF, Lubman DI. Parenting factors associated with reduced adolescent alcohol use: a systematic review of longitudinal studies. Aust N Z J Psychiatry. 2010;44:774–83. doi: 10.1080/00048674.2010.501759. [DOI] [PubMed] [Google Scholar]
- 14.Evans E, Hawton K, Rodham K. Factors associated with suicidal phenomena in adolescents: a systematic review of population-based studies. Clin Psychol Rev. 2004;24:957–79. doi: 10.1016/j.cpr.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Fliege H, Lee JR, Grimm A, Klap BF. Risk factors and correlates of deliberate self-harm behavior: a systematic review. J Psychosom Res. 2009;66:477–93. doi: 10.1016/j.jpsychores.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization (WHO) Adolescent health [Internet] 2019. [cited 2019 Jan 21] http://www.who.int/maternal_child_adolescent/adolescence/en/ [Google Scholar]
- 18.Kipping RR, Smith M, Heron J, Hickman M, Campbell R. Multiple risk behaviour in adolescence and socio-economic status: findings from a UK birth cohort. Eur J Public Health. 2015;25:44–9. doi: 10.1093/eurpub/cku078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berg N, Kiviruusu O, Karvonen S, Kestilä L, Lintonen T, Rahkonen O, et al. A 26-year follow-up study of heavy drinking trajectories from adolescence to mid-adulthood and adult disadvantage. Alcohol Alcohol. 2013;48:452–7. doi: 10.1093/alcalc/agt026. [DOI] [PubMed] [Google Scholar]
- 20.Hallfors DD, Waller MW, Ford CA, Halpern CT, Brodish BH, Iritani B. Adolescent depression and suicide risk: association with sex and drug behavior. Am J Prev Med. 2004;27:224–31. doi: 10.1016/j.amepre.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 21.Núcleo Ciência Pela Infância (NCPI) Early child [Internet] [cited 2020 Mar 23]. http://ncpi.org.br/en-us/early-childhood/ [Google Scholar]
- 22.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale for assessing the quality of nonrandomised studies in meta-analyses [Internet] [cited 2014 Mar 11]. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- 23.Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171:788–97. doi: 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Embree TE, Romanow NT, Djerboua MS, Morgunov NJ, Bourdeaux JJ, Hagel BE. Risk factors for bicycling injuries in children and adolescents: a systematic review. Pediatrics. 2016;138:e20160282. doi: 10.1542/peds.2016-0282. [DOI] [PubMed] [Google Scholar]
- 25.Kandel DB, Wu P, Davies M. Maternal smoking during pregnancy and smoking by adolescent daughters. Am J Public Health. 1994;84:1407–13. doi: 10.2105/ajph.84.9.1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Isohanni M, Oja H, Moilanen I, Rantakallio P, Koiranen M. The relation between teenage smoking and drinking, with special reference to non-standard family background. Scand J Soc Med. 1993;21:24–30. doi: 10.1177/140349489302100105. [DOI] [PubMed] [Google Scholar]
- 27.Roberts KH, Munafò MR, Rodriguez D, Drury M, Murphy MF, Neale RE, et al. Longitudinal analysis of the effect of prenatal nicotine exposure on subsequent smoking behavior of offspring. Nicotine Tob Res. 2005;7:801–8. doi: 10.1080/14622200500262840. [DOI] [PubMed] [Google Scholar]
- 28.Lawlor DA, O'Callaghan MJ, Mamun AA, Williams GM, Bor W, Najman JM. Early life predictors of adolescent smoking: findings from the Mater‐University study of pregnancy and its outcomes. Paediatr Perinat Epidemiol. 2005;19:377–87. doi: 10.1111/j.1365-3016.2005.00674.x. [DOI] [PubMed] [Google Scholar]
- 29.Edwards AC, Latendresse SJ, Heron J, Cho SB, Hickman M, Lewis G, et al. Childhood internalizing symptoms are negatively associated with early adolescent alcohol use. Alcohol Clin Exp Res. 2014;38:1680–8. doi: 10.1111/acer.12402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Farooqi A, Hägglöf B, Sedin G, Gothefors L, Serenius F. Mental health and social competencies of 10-to 12-year-old children born at 23 to 25 weeks of gestation in the 1990s: a Swedish national prospective follow-up study. Pediatrics. 2007;120:118–33. doi: 10.1542/peds.2006-2988. [DOI] [PubMed] [Google Scholar]
- 31.Skinner SR, Robinson M, Smith MA, Robbins SC, Mattes E, Cannon J, et al. Childhood behavior problems and age at first sexual intercourse: a prospective birth cohort study. Pediatrics. 2015;135:255–63. doi: 10.1542/peds.2014-1579. [DOI] [PubMed] [Google Scholar]
- 32.Skinner SR, Marino J, Rosenthal SL, Cannon J, Doherty DA, Hickey M. Prospective cohort study of childhood behaviour problems and adolescent sexual risk-taking: gender matters. Sex Health. 2017;14:492–501. doi: 10.1071/SH16240. [DOI] [PubMed] [Google Scholar]
- 33.Dietrich KN, Ris MD, Succop PA, Berger OG, Bornschein RL. Early exposure to lead and juvenile delinquency. Neurotoxicol Teratol. 2001;23:511–8. doi: 10.1016/s0892-0362(01)00184-2. [DOI] [PubMed] [Google Scholar]
- 34.Delaney-Black V, Chiodo LM, Hannigan JH, Greenwald MK, Janisse J, Patterson G, et al. Prenatal and postnatal cocaine exposure predict teen cocaine use. Neurotoxicol Teratol. 2011;33:110–9. doi: 10.1016/j.ntt.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Griesler PC, Kandel DB. The impact of maternal drinking during and after pregnancy on the drinking of adolescent offspring. J Stud Alcohol. 1998;59:292–304. doi: 10.15288/jsa.1998.59.292. [DOI] [PubMed] [Google Scholar]
- 36.Ter Wolbeek M, Kavelaars A, de Vries WB, Tersteeg-Kamperman M, Veen S, Kornelisse RF, et al. Neonatal glucocorticoid treatment: Long-term effects on the hypothalamus-pituitary-adrenal axis, immune system, and problem behavior in 14-17 year old adolescents. Brain Behav Immun. 2015;45:128–38. doi: 10.1016/j.bbi.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 37.Mikkelsen SH, Obel C, Olsen J, Niclasen J, Bech BH. Maternal caffeine consumption during pregnancy and behavioral disorders in 11-year-old offspring: a Danish National Birth Cohort Study. J Pediatr. 2017;189:120–7. doi: 10.1016/j.jpeds.2017.06.051. [DOI] [PubMed] [Google Scholar]
- 38.Robinson M, Mattes E, Oddy WH, de Klerk NH, Li J, McLean NJ, et al. Hypertensive diseases of pregnancy and the development of behavioral problems in childhood and adolescence: the Western Australian Pregnancy Cohort Study. J Pediatr. 2009;154:218–24. doi: 10.1016/j.jpeds.2008.07.061. [DOI] [PubMed] [Google Scholar]
- 39.Alati R, Najman JM, O’Callaghan M, Bor W, Williams GM, Clavarino A. Fetal growth and behaviour problems in early adolescence: findings from the Mater University Study of Pregnancy. Int J Epidemiol. 2009;38:1390–400. doi: 10.1093/ije/dyp252. [DOI] [PubMed] [Google Scholar]
- 40.Farooqi A, Hägglöf B, Sedin G, Gothefors L, Serenius F. Mental health and social competencies of 10-to 12-year-old children born at 23 to 25 weeks of gestation in the 1990s: a Swedish national prospective follow-up study. Pediatrics. 2007;120:118–33. doi: 10.1542/peds.2006-2988. [DOI] [PubMed] [Google Scholar]
- 41.Hutchinson DM, Alati R, Najman JM, Mattick RP, Bor W, O'Callaghan M, et al. Maternal attitudes in pregnancy predict drinking initiation in adolescence. Aust N Z J Psychiatry. 2008;42:324–34. doi: 10.1080/00048670701881512. [DOI] [PubMed] [Google Scholar]
- 42.Betts KS, Williams GM, Najman JM, Alati R. Maternal depressive, anxious, and stress symptoms during pregnancy predict internalizing problems in adolescence. Depress Anxiety. 2014;31:9–18. doi: 10.1002/da.22210. [DOI] [PubMed] [Google Scholar]
- 43.Baer JS, Barr HM, Bookstein FL, Sampson PD, Streissguth AP. Prenatal alcohol exposure and family history of alcoholism in the etiology of adolescent alcohol problems. J Stud Alcohol. 1998;59:533–43. doi: 10.15288/jsa.1998.59.533. [DOI] [PubMed] [Google Scholar]
- 44.Dube SR, Miller JW, Brown DW, Giles WH, Felitti VJ, Dong M, et al. Adverse childhood experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006;38:444.e1–10. doi: 10.1016/j.jadohealth.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 45.Melotti R, Heron J, Hickman M, Macleod J, Araya R, Lewis G, et al. Adolescent alcohol and tobacco use and early socioeconomic position: the ALSPAC birth cohort. Pediatrics. 2011;127:e948–55. doi: 10.1542/peds.2009-3450. [DOI] [PubMed] [Google Scholar]
- 46.Isohanni M, Oja H, Moilanen I, Koiranen M. Teenage alcohol drinking and non-standard family background. Soc Sci Med. 1994;38:1565–74. doi: 10.1016/0277-9536(94)90118-x. [DOI] [PubMed] [Google Scholar]
- 47.Fisher LB, Miles IW, Austin SB, Camargo CA, Jr, Colditz GA. Predictors of initiation of alcohol use among US adolescents: findings from a prospective cohort study. Arch Pediatr Adolesc Med. 2007;161:959–66. doi: 10.1001/archpedi.161.10.959. [DOI] [PubMed] [Google Scholar]
- 48.Livaudais JC, Napoles-Springer A, Stewart S, Kaplan CP. Understanding Latino adolescent risk behaviors: parental and peer influences. Ethn Dis. 2007;17:298–304. [PubMed] [Google Scholar]
- 49.Boyle MH, Offord DR, Racine YA, Szatmari P, Fleming JE, Links PS. Predicting substance use in late adolescence: results from the Ontario Child Health Study follow-up. Am J Psychiatry. 1992;149:761–7. doi: 10.1176/ajp.149.6.761. [DOI] [PubMed] [Google Scholar]
- 50.Danielsson AK, Wennberg P, Tensgtröm A, Romelsjö A. Adolescent alcohol use trajectories: predictors and subsequent problems. Addict Behav. 2010;35:848–52. doi: 10.1016/j.addbeh.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 51.McCarty CA, Wymbs BT, King KM, Mason WA, Vander Stoep A, McCauley E, et al. Developmental consistency in associations between depressive symptoms and alcohol use in early adolescence. J Stud Alcohol Drugs. 2012;73:444–53. doi: 10.15288/jsad.2012.73.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Monshouwer K, Harakeh Z, Lugtig P, Huizink A, Creemers HE, Reijneveld SA, et al. Predicting transitions in low and high levels of risk behavior from early to middle adolescence: the TRAILS study. J Abnorm Child Psychol. 2012;40:923–31. doi: 10.1007/s10802-012-9624-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Modecki KL, Bonnie BL, Eccles JS. Binge drinking trajectories across adolescence: for early maturing youth, extra-curricular activities are protective. J Adolesc Health. 2014;54:61–6. doi: 10.1016/j.jadohealth.2013.07.032. [DOI] [PubMed] [Google Scholar]
- 54.Bearinger LH, Blum RW. The utility of locus of control for predicting adolescent substance use. Res Nurs Health. 1997;20:229–45. doi: 10.1002/(sici)1098-240x(199706)20:3<229::aid-nur6>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 55.McCann M, Perra O, McLaughlin A, McCartan C, Higgins K. Assessing elements of a family approach to reduce adolescent drinking frequency: parent-adolescent relationship, knowledge management and keeping secrets. Addiction. 2015;111:843–53. doi: 10.1111/add.13258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wilcox HC, Storr CL, Benoit MZ, Anthony JC. Ethnicity as manifest in drug-specific vocabulary and subsequent risk of starting cannabis use in early adolescence. Ethn Dis. 2005;15:485–91. [PubMed] [Google Scholar]
- 57.Bohnert KM, Anthony JC, Breslau N. Parental monitoring at age 11 and subsequent onset of cannabis use up to age 17: results from a prospective study. J Stud Alcohol Drugs. 2012;73:173–7. doi: 10.15288/jsad.2012.73.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brown J, Cohen P, Johnson JG, Smailes EM. Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry. 1999;38:1490–6. doi: 10.1097/00004583-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 59.Cornelius MD, Leech SL, Goldschmidt L, Day NL. Prenatal tobacco exposure: is it a risk factor for early tobacco experimentation? Nicotine Tob Res. 2000;2:45–52. doi: 10.1080/14622200050011295. [DOI] [PubMed] [Google Scholar]
- 60.Skara S, Sussman S, Dent CW. Predicting regular cigarette use among continuation high school students. Am J Health Behav. 2001;25:147–56. doi: 10.5993/ajhb.25.2.7. [DOI] [PubMed] [Google Scholar]
- 61.Menezes AM, Gonçalves H, Anselmi L, Hallal PC, Araujo CL. Smoking in early adolescence: evidence from the 1993 Pelotas (Brazil) birth cohort study. J Adolesc Health. 2006;39:669–77. doi: 10.1016/j.jadohealth.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 62.Abernathy TJ, Massad L, Romano-Dwyer L. The relationship between smoking and self-esteem. Adolescence. 1995;30:899–907. [PubMed] [Google Scholar]
- 63.Karp I, O'loughlin J, Paradis G, Hanley J, Difranza J. Smoking trajectories of adolescent novice smokers in a longitudinal study of tobacco use. Ann Epidemiol. 2005;15:445–52. doi: 10.1016/j.annepidem.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 64.O'Loughlin J, Karp I, Koulis T, Paradis G, Difranza J. Determinants of first puff and daily cigarette smoking in adolescents. Am J Epidemiol. 2009;170:585–97. doi: 10.1093/aje/kwp179. [DOI] [PubMed] [Google Scholar]
- 65.Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. Depression, anxiety, and smoking initiation: a prospective study over 3 years. Am J Public Health. 1998;88:1518–22. doi: 10.2105/ajph.88.10.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.O'Callaghan FV, O'Callaghan M, Najman JM, Williams GM, Bor W, Alati R. Prediction of adolescent smoking from family and social risk factors at 5 years, and maternal smoking in pregnancy and at 5 and 14 years. Addiction. 2006;101:282–90. doi: 10.1111/j.1360-0443.2006.01323.x. [DOI] [PubMed] [Google Scholar]
- 67.Paunesku D, Ellis J, Fogel J, Kuwabara SA, Gollan J, Gladstone T, et al. Clusters of behaviors and beliefs predicting adolescent depression: implications for prevention. J Cogn Behav Psychother. 2008;8:147–68. [PMC free article] [PubMed] [Google Scholar]
- 68.Flory K, Malone PS, Lamis DA. Childhood ADHD symptoms and risk for cigarette smoking during adolescence: school adjustment as a potential mediator. Psychol Addict Behav. 2011;25:320–9. doi: 10.1037/a0022633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hammond D, Reid JL, Cole AG, Leatherdale ST. Electronic cigarette use and smoking initiation among youth: a longitudinal cohort study. CMAJ. 2017;189:E1328–36. doi: 10.1503/cmaj.161002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jaber R, Madhivanan P, Veledar E, Khader Y, Mzayek F, Maziak W. Waterpipe a gateway to cigarette smoking initiation among adolescents in Irbid, Jordan: a longitudinal study. Int J Tuberc Lung Dis. 2015;19:481–7. doi: 10.5588/ijtld.14.0869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bernat DH, Erickson DJ, Widome R, Perry CL, Forster JL. Adolescent smoking trajectories: results from a population-based cohort study. J Adolesc Health. 2008;43:334–40. doi: 10.1016/j.jadohealth.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.de Vries H, Candel M, Engels R, Mercken L. Challenges to the peer influence paradigm: results for 12-13 year olds from six European countries from the European smoking prevention framework approach study. Tob Control. 2006;15:83–9. doi: 10.1136/tc.2003.007237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Alati R, Najman JM, O’Callaghan M, Bor W, Williams GM, Clavarino A. Fetal growth and behaviour problems in early adolescence: findings from the Mater university study of pregnancy. Int J Epidemiol. 2009;38:1390–400. doi: 10.1093/ije/dyp252. [DOI] [PubMed] [Google Scholar]
- 74.Ter Wolbeek M, Kavelaars A, de Vries WB, Tersteeg-Kamperman M, Veen S, Kornelisse RF, et al. Neonatal glucocorticoid treatment: long-term effects on the hypothalamus-pituitary-adrenal axis, immune system, and problem behavior in 14-17 year old adolescents. Brain Behav Immun. 2015;45:128–38. doi: 10.1016/j.bbi.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 75.Culpin I, Stapinski L, Miles ÖB, Araya R, Joinson C. Exposure to socioeconomic adversity in early life and risk of depression at 18 years: the mediating role of locus of control. J Affect Disord. 2015;183:269–78. doi: 10.1016/j.jad.2015.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Clark C, Haines MM, Head J, Klinberg E, Arephin M, Viner R, et al. Psychological symptoms and physical health and health behaviours in adolescents: a prospective 2‐year study in East London. Addiction. 2007;102:126–35. doi: 10.1111/j.1360-0443.2006.01621.x. [DOI] [PubMed] [Google Scholar]
- 77.Van Voorhees BW, Paunesku D, Kuwabara SA, Basu A, Gollan J, Hankin BL, et al. Protective and vulnerability factors predicting new-onset depressive episode in a representative of US adolescents. J Adolesc Health. 2008;42:605–16. doi: 10.1016/j.jadohealth.2007.11.135. [DOI] [PubMed] [Google Scholar]
- 78.Kaltiala-Heino R, Fröjd S, Marttunen M. Involvement in bullying and depression in a 2-year follow-up in middle adolescence. Eur Child Adolesc Psychiatry. 2010;19:45–55. doi: 10.1007/s00787-009-0039-2. [DOI] [PubMed] [Google Scholar]
- 79.Bowes L, Carnegie R, Pearson R, Mars B, Biddle L, Maughan B, et al. Risk of depression and self-harm in teenagers identifying with goth subculture: a longitudinal cohort study. Lancet Psychiatry. 2015;2:793–800. doi: 10.1016/S2215-0366(15)00164-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Page A, Lewis G, Kidger J, Heron J, Chittleborough C, Evans J, et al. Parental socio-economic position during childhood as a determinant of self-harm in adolescence. Soc Psychiatry Psychiatr Epidemiol. 2014;49:193–203. doi: 10.1007/s00127-013-0722-y. [DOI] [PubMed] [Google Scholar]
- 81.Nahapetyan L, Orpinas P, Song X, Holland K. Longitudinal association of suicidal ideation and physical dating violence among high school students. J Youth Adolesc. 2014;43:629–40. doi: 10.1007/s10964-013-0006-6. [DOI] [PubMed] [Google Scholar]
- 82.Strandheim A, Bjerkeset O, Gunnell D, Bjørnelv S, Holmen TL, Bentzen N. Risk factors for suicidal thoughts in adolescence-a prospective cohort study: the Young-HUNT study. BMJ Open. 2014;4:e005867. doi: 10.1136/bmjopen-2014-005867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kim YS, Leventhal BL, Koh YJ, Boyce WT. Bullying increased suicide risk: prospective study of Korean adolescents. Arch Suicide Res. 2009;13:15–30. doi: 10.1080/13811110802572098. [DOI] [PubMed] [Google Scholar]
- 84.Young R, Sweeting H, Ellaway A. Do schools differ in suicide risk? The influence of school and neighbourhood on attempted suicide, suicidal ideation and self-harm among secondary school pupils. BMC Public Health. 2011;11:874. doi: 10.1186/1471-2458-11-874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fisher HL, Moffitt TE, Houts RM, Belsky DW, Arseneault L, Caspi A. Bullying victimization and risk of self harm in early adolescence: longitudinal cohort study. BMJ. 2012;344:2683. doi: 10.1136/bmj.e2683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tidemalm D, Beckman K, Dahlin M, Vaez M, Lichtenstein P, Långström N, et al. Age-specific suicide mortality following non-fatal self-harm: national cohort study in Sweden. Psychol Med. 2015;45:1699–707. doi: 10.1017/S0033291714002827. [DOI] [PubMed] [Google Scholar]
- 87.Ritter J, Stewart M, Bernet C, Coe M, Brown SA. Effects of childhood exposure to familial alcoholism and family violence on adolescent substance use, conduct problems, and self‐esteem. J Trauma Stress. 2002;15:113–22. doi: 10.1023/A:1014803907234. [DOI] [PubMed] [Google Scholar]
- 88.Wakschlag LS, Pickett KE, Kasza KE, Loeber R. Is prenatal smoking associated with a developmental pattern of conduct problems in young boys? J Am Acad Child Adolesc Psychiatry. 2006;45:461–7. doi: 10.1097/01.chi.0000198597.53572.3e. [DOI] [PubMed] [Google Scholar]
- 89.Liu J, Raine A, Wuerker A, Venables PH, Mednick S. The association of birth complications and externalizing behavior in early adolescents: direct and mediating effects. J Res Adolesc. 2009;19:93–111. doi: 10.1111/j.1532-7795.2009.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Murray J, Maughan B, Menezes AM, Hickman M, MacLeod J, Matijasevich A, et al. Perinatal and sociodemographic factors at birth predicting conduct problems and violence to age 18 years: comparison of Brazilian and British birth cohorts. J Child Psychol Psychiatry. 2015;56:914–22. doi: 10.1111/jcpp.12369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Boden JM, Fergusson DM, Horwood LJ. Risk factors for conduct disorder and oppositional/defiant disorder: evidence from a New Zealand birth cohort. J Am Acad Child Adolesc Psychiatry. 2010;49:1125–33. doi: 10.1016/j.jaac.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 92.Fergusson DM, Horwood LJ, Lynskey MT. Parental separation, adolescent psychopathology, and problem behaviors. J Am Acad Child Adolesc Psychiatry. 1994;33:1122–31. doi: 10.1097/00004583-199410000-00008. discussion 1131-3. [DOI] [PubMed] [Google Scholar]
- 93.Wymbs BT, McCarty CA, Mason WA, King KM, Baer JS, Stoep AV, et al. Early adolescent substance use as a risk factor for developing conduct disorder and depression symptoms. J Stud Alcohol Drugs. 2014;75:279–89. [PMC free article] [PubMed] [Google Scholar]
- 94.Kretschmer T, Oliver BR, Maughan B. Pubertal development, spare time activities, and adolescent delinquency: testing the contextual amplification hypothesis. J Youth Adolesc. 2014;43:1346–60. doi: 10.1007/s10964-013-0074-7. [DOI] [PubMed] [Google Scholar]
- 95.Hipwell AE, Murray J, Xiong S, Stepp SD, Keenan KE. Effects of adolescent childbearing on maternal depression and problem behaviors: a prospective, population-based study using risk-set propensity scores. PloS One. 2016;11:e0155641. doi: 10.1371/journal.pone.0155641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tremblay RE, Masse B, Perron D, LeBlanc M, Schwartzman AE, Ledingham JE. Early disruptive behavior, poor school achievement, delinquent behavior, and delinquent personality: longitudinal analyses. J Consult Clin Psychol. 1992;60:64–72. doi: 10.1037//0022-006x.60.1.64. [DOI] [PubMed] [Google Scholar]
- 97.Fergusson DM, Horwood LJ, Lynskey MT. Childhood sexual abuse, adolescent sexual behaviors and sexual revictimization. Child Abuse Negl. 1997;21:789–803. doi: 10.1016/s0145-2134(97)00039-2. [DOI] [PubMed] [Google Scholar]
- 98.Parkes A, Waylen A, Sayal K, Heron J, Henderson M, Wight D, et al. Which behavioral, emotional and school problems in middle-childhood predict early sexual behavior? J Youth Adolesc. 2014;43:507–27. doi: 10.1007/s10964-013-9973-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Donahue KL, Lichtenstein P, Lundström S, Anckarsäter H, Gumpert CH, Långström N, et al. Childhood behavior problems and adolescent sexual risk behavior: Familial confounding in the Child and Adolescent Twin Study in Sweden (CATSS) J Adolesc Health. 2013;52:606–12. doi: 10.1016/j.jadohealth.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Paul C, Fitzjohn J, Herbison P, Dickson N. The determinants of sexual intercourse before age 16. J Adolesc Health. 2000;27:136–47. doi: 10.1016/s1054-139x(99)00095-6. [DOI] [PubMed] [Google Scholar]
- 101.Gambadauro P, Carli V, Hadlaczky G, Sarchiapone M, Apter A, Balazs J, et al. Correlates of sexual initiation among European adolescents. PloS One. 2018;13:e0191451. doi: 10.1371/journal.pone.0191451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Crosby R, Leichliter JS, Brackbill R. Longitudinal prediction of sexually transmitted diseases among adolescents: results from a national survey. Am J Prev Med. 2000;18:312–7. doi: 10.1016/s0749-3797(00)00122-7. [DOI] [PubMed] [Google Scholar]
- 103.Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: trajectories, risk factors, and event-level relationships. Dev Psychol. 2012;48:1429–42. doi: 10.1037/a0027547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Woodward LJ, Fergusson DM. Early conduct problems and later risk of teenage pregnancy in girls. Dev Psychopathol. 1999;11:127–41. doi: 10.1017/s0954579499001984. [DOI] [PubMed] [Google Scholar]
- 105.Bruno ZV, Feitosa FEL, Silveira KP, Morais IQ, Bezerra MF. Subsequent pregnancy among adolescents. Rev Bras Ginecol Obstet. 2009;31:480–4. doi: 10.1590/s0100-72032009001000002. [DOI] [PubMed] [Google Scholar]
- 106.World Health Organization (WHO) Social determinants of health [Internet] 2019. [cited 2020 Jan 22] http://www.who.int/social_determinants/sdh_definition/en/ [Google Scholar]
- 107.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 108.Short SE, Mollborn S. Social determinants and health behaviors: conceptual frames and empirical advances. Curr Opin Psychol. 2015;5:78–84. doi: 10.1016/j.copsyc.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Moore TG, McDonald M, Carlon L, O'Rourke K. Early childhood development and the social determinants of health inequities. Health Promot Int. 2015;30(Suppl 2):ii102–15. doi: 10.1093/heapro/dav031. [DOI] [PubMed] [Google Scholar]
- 110.Garmezy N. Stress-resistant children: the search for protective factors. In: Stevenson JE, editor. Recent research in developmental psychopathology (Child Psychology Psychiatry Supplement) Oxford: Pergamon; 1985. pp. 213–33. editor. p. [Google Scholar]
- 111.Conti G, Heckman JJ, Pinto R. The effects of two influential early childhood interventions on health and healthy behaviour. Econ J. 2016;126:F28–65. doi: 10.1111/ecoj.12420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Pollard JA, Hawkins JD, Arthur MW. Risk and protection: are both necessary to understand diverse behavioral outcomes in adolescence? Soc Work Res. 1999;23:145–58. [Google Scholar]
- 113.Beyers JM, Toumbourou JW, Catalano RF, Arthur MW, Hawkins JD. A cross-national comparison of risk and protective factors for adolescent substance use: the United States and Australia. J Adolesc Health. 2004;35:3–16. doi: 10.1016/j.jadohealth.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 114.Bernard B. Resiliency paradigm validates craft knowledge. Western Center News. 1993;6:6–7. [Google Scholar]
- 115.Benson PL. All kids are our kids: what communities must do to raise caring and responsible children and adolescents. 2nd ed. San Francisco:: Jossey-Bass;; 1997. [Google Scholar]
- 116.Tolan PH. How resilient is the concept of resilience? Community Psychol. 1996;29:12–5. [Google Scholar]
- 117.Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. Lancet. 2012;379:1641–52. doi: 10.1016/S0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
- 118.Herrenkohl TI, Maguin E, Hill KG, Hawkins JD, Abbott RD, Catalano RF. Developmental risk factors for youth violence. J Adolesc Health. 2000;26:176–86. doi: 10.1016/s1054-139x(99)00065-8. [DOI] [PubMed] [Google Scholar]
- 119.Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 120.Boyle MH, Georgiades K, Racine Y, Mustard C. Neighborhood and family influences on educational attainment: results from the Ontario child health study follow-up 2001. Child Dev. 2007;78:168–89. doi: 10.1111/j.1467-8624.2007.00991.x. [DOI] [PubMed] [Google Scholar]
- 121.Harding DJ. Counterfactual models of neighborhood effects: the effect of neighborhood poverty on dropping out and teenage pregnancy. Am J Sociol. 2003;109:676–719. [Google Scholar]
- 122.Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37:293–310. [PubMed] [Google Scholar]
- 123.Jaccard J, Blanton H, Dodge T. Peer influences on risk behavior: an analysis of the effects of a close friend. Dev Psychol. 2005;41:135–47. doi: 10.1037/0012-1649.41.1.135. [DOI] [PubMed] [Google Scholar]
- 124.Rutter M. Psychosocial resilience and protective mechanisms. Am J Orthopsychiatry. 1987;57:316–31. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 125.Jessor R, Van Den Bos J, Vanderryn J, Costa FM, Turbin MS. Protective factors in adolescent problem behavior: moderator effects and developmental change. Dev Psychol. 1995;31:923–33. [Google Scholar]
- 126.Garmezy N, Masten AS. Stress, competence, and resilience: common frontiers for therapist and psychopathologist. Behav Ther. 1986;17:500–21. [Google Scholar]
- 127.Fedak KM, Bernal A, Capshaw ZA, Gross S. Applying the Bradford Hill criteria in the 21st century: how data integration has changed causal inference in molecular epidemiology. Emerg Themes Epidemiol. 2015;12:14. doi: 10.1186/s12982-015-0037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]