Abstract
Background
The COVID-19 pandemic has strained the healthcare systems across the world but its impact on acute stroke care is just being elucidated. We hypothesized a major global impact of COVID-19 not only on stroke volumes but also on various aspects of thrombectomy systems.
Aims
We conducted a convenience electronic survey with a 21-item questionnaire aimed to identify the changes in stroke admission volumes and thrombectomy treatment practices seen during a specified time period of the COVID-19 pandemic.
Methods
The survey was designed using Qualtrics software and sent to stroke and neuro-interventional physicians around the world who are part of the Global Executive Committee (GEC) of Mission Thrombectomy 2020, a global coalition under the aegis of Society of Vascular and Interventional Neurology, between April 5th and May 15th, 2020.
Results
There were 113 responses to the survey across 25 countries with a response rate of 31% among the GEC members. Globally there was a median 33% decrease in stroke admissions and a 25% decrease in mechanical thrombectomy (MT) procedures during the COVID-19 pandemic period until May 15th, 2020 compared to pre-pandemic months. The intubation policy for MT procedures during the pandemic was highly variable across participating centers: 44% preferred intubating all patients, including 25% of centers that changed their policy to preferred-intubation (PI) from preferred non-intubation (PNI). On the other hand, 56% centers preferred not intubating patients undergoing MT, which included 27% centers that changed their policy from PI to PNI. There was no significant difference in rate of COVID-19 infection between PI versus PNI centers (p=0.60) or if intubation policy was changed in either direction (p=1.00). Low-volume (<10 stroke/month) compared with high-volume stroke centers (>20 strokes/month) were less likely to have neurointerventional suite specific written personal protective equipment protocols (74% vs 88%) and if present, these centers were more likely to report them to be inadequate (58% vs 92%).
Conclusion
Our data provides a comprehensive snapshot of the impact on acute stroke care observed worldwide during the pandemic. Overall, respondents reported decreased stroke admissions as well as decreased cases of MT with no clear preponderance in intubation policy during MT.
Data access statement
The corresponding author will consider requests for sharing survey data. The study was exempt from institutional review board approval as it did not involve patient level data.
Key Words: Stroke, Mechanical thrombectomy, Intubation, Personal protective equipment, COVID-19, Large vessel occlusion, Coronavirus
Introduction
On March 11th 2020, the World Health Organization declared Coronavirus disease-2019 (COVID-19) a global pandemic which has burdened the healthcare systems worldwide. Globally, as of 28 November 2020, there have been 61,036,793 confirmed cases of COVID-19, including 1,433,316 deaths, reported to WHO.1 Pre-hospital and in-hospital protocols during COVID-19 have been highly variable within and between different countries, ranging from changes in pre-hospital triage policy by designating certain hospitals as COVID-19 centers, protocols for testing patients based on symptomatology or exposure, to cancellation of elective procedures and postponement of semi-elective procedures. By mid-April 2020, various neurointerventional societies such as Society of Vascular and Interventional Neurologists (SVIN),2 Society of Neurointerventional Surgery (SNIS)3 and European Society of Minimally Invasive Neurological Therapy (ESMINT)4 provided guidance statements for the care of patients requiring emergent neurointerventional procedures during COVID-19 pandemic. Availability and adequacy of personal protective equipment (PPE) is uniformly stressed to be of utmost importance to protect the frontline healthcare workers as evident by a large case series from Wuhan, China showing hospital-associated transmission as the presumed mechanism of infection in 29% of affected healthcare workers.5 There is a consensus amongst the international medical community that presence of COVID-19 as a public health emergency should not alter the inclusion or exclusion criteria for Mechanical Thrombectomy (MT),6 though the recommendations on criteria and timing of intubation for patients undergoing MT is unclear and more heavily contingent on institutional resources available. Also, while expert recommendations have been published there is no consensus on appropriate changes in practice in the management of non-COVID-19 emergencies during the pandemic. Different countries or even different healthcare systems within a country responded with a varied spectrum of policy changes trying to balance the safety of its healthcare workers and uphold the continued quality of care for the patients presenting with emergencies including stroke. This cross-sectional convenience survey by the MT2020+ global alliance reports an international snapshot of the significant changes in acute stroke care with an emphasis on mechanical thrombectomy.
Methods
A survey comprising of 21-questions (supplemental item 1) was distributed to the members of Global Executive Committee of the Mission Thrombectomy 2020+ alliance7 supported by the Society of Vascular and Interventional Neurologists (SVIN). The survey was sent by electronic mail and answered online. The GEC members were encouraged to further disseminate the survey to practicing stroke physicians and or neuro-interventionalists in their region. The questionnaire was designed to collect responses on four main categories: (I) Stroke and (II) MT volume pre and during-COVID-19; (III) Intubation policy changes due to COVID-19 for patients undergoing MT; (IV) Availability and adequacy of PPE and COVID-19 infections amongst neuroendovascular and stroke physicians, and ancillary staff. The survey responses were recorded between April 5th and May 15th, 2020. Participation was voluntary and responses were anonymized. Respondents from each country were allowed to choose the start of the COVID-19 timeline based on first COVID-19 cases documented in their respective countries.
Descriptive statistics were used to calculate the median stroke admissions and MT performed per month pre (A) and during (B) COVID-19, and then, the median of the stroke volume change reported by each respondent was calculated (i.e. median of B1-A1, B2-A2, B3-A3…). Two separate analysis of the data were performed: in the first analysis, countries with three or more responses were included in order to have a better representation of a country. Of note, respondents from all 19 centers from Germany, Poland, Italy and France reported a change in their local pre-hospital stroke triage policy (STP) diverting stroke patients to pre-specified centers. This had a direct effect on the descriptive statistics. Hence, these results were dichotomized by countries with and without change in pre-hospital triage policies for stroke admission during COVID-19. In the second analysis, we included responses from all the countries which were grouped into low, medium and high-volume centers based on their pre-COVID-19 stroke admissions representing < 10, 10–20 and > 20 average strokes per month respectively. The reported rate of COVID-19 infection amongst the physicians and ancillary staff was standardized based on pre-COVID-19 stroke admission volume because we lacked information on the denominator for the number of physicians and staff at risk.
Statistical analysis was performed using SPSS statistics software, version 25 (IBM Corp., Armonk, N.Y., USA). Fisher's exact test or Chi-square test, as appropriate, was used for categorical variables and p-value < 0.05 was considered significant.
Results
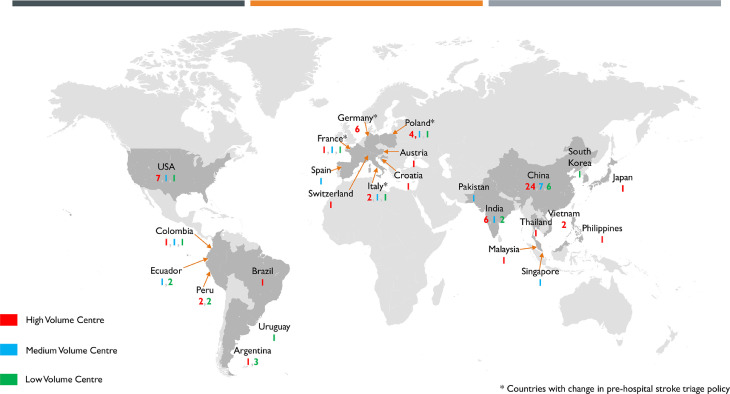
During the survey period from April 5th, 2020 to May 15th, 2020, we received 113 responses across 25 countries (Fig. 1 ), with a response rate of 31% among the GEC members. The response rate of the non-GEC members is not known. 12/25 (48%) countries had three or more respondents (n=99).
Fig. 1.
World map representing the distribution of 113 responses across 25 countries and 103 centers which are further grouped into high, medium or low-volume based on pre-COVID stroke admissions per month
Stroke volume
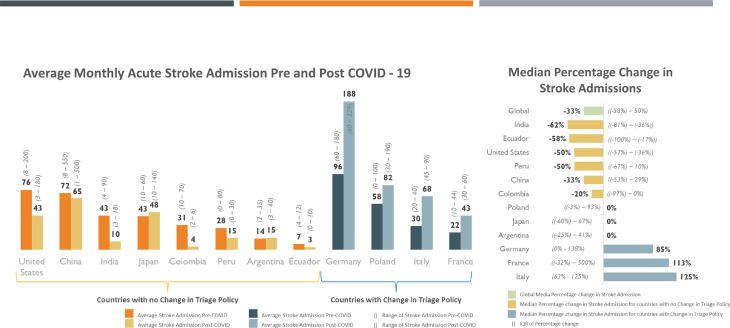
The overall group of respondents, with 3 or more responses from a country, reported a median 33% (IQR -60 – 50) decrease in stroke admissions during COVID-19 pandemic. Among this group, respondent in countries without STP change, reported a median percentage decrease in stroke admissions by 43% ranging from a decrease of 62% in India to 20% in Columbia. (Fig. 2 ). High, medium and low-volume stroke centers without a change in STP reported a median percentage decrease of 50% (IQR -71 – -10), 17% (IQR -51 – 13) and no change respectively during COVID-19 (Fig. 3 ).
Fig. 2.
Average monthly stroke admissions (2A) and median percentage change in stroke admissions (2B) pre- and during-COVID-19 globally and amongst countries with at least 3 or more responses with or without change in pre-hospital stroke triage policy.
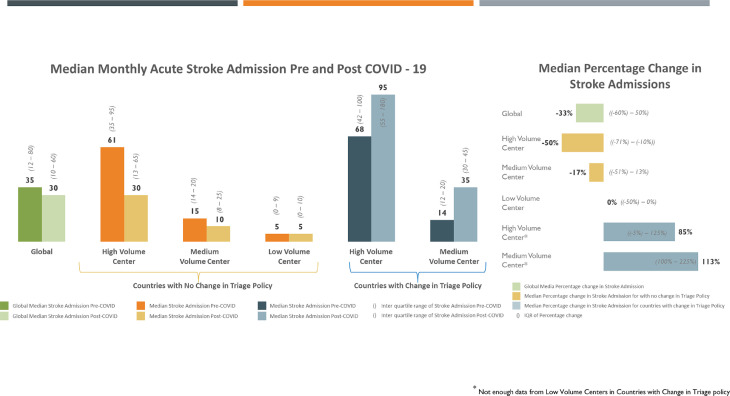
Fig. 3.
Average monthly stroke admissions (3A) and median percentage change in stroke admissions (3B) in high, medium and low-volume stroke centers pre- and during-COVID-19 globally with or without change in pre-hospital stroke triage policy
For STP countries, Germany, France, Italy and Poland reported a median percentage increase of 85% (IQR 0-138), 113% (IQR -32 – 500), 125% (IQR 63-125) and 0% (IQR -3 – 93) stroke admissions during COVID-19 respectively (Fig. 2). Amongst STP countries, high and medium volume centers reported a median percentage increase of 85% (IQR -5 – 125) and 113% (IQR 100 – 225), respectively. Not enough data was reported from low volume centers in countries with STP change (Fig. 3).
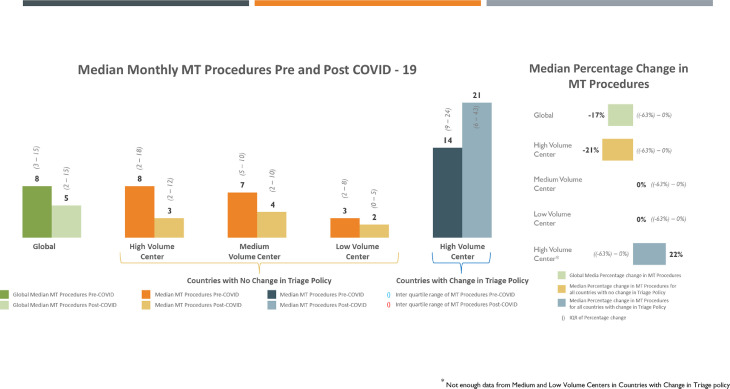
Mechanical thrombectomy volume
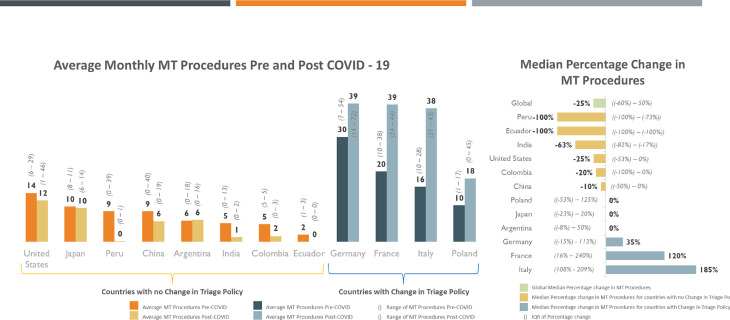
Globally our survey reported a 25% (IQR -60 – 50) median percentage decrease in MT performed during COVID-19. This rose to 33% median percentage decrease after excluding countries with STP change ranging from -100% in Peru and Ecuador, to -10% in China (Fig. 4 ). Similarly, high volume centers in countries without change in their local triage policy showed a median decrease of 21% (IQR -63 – 0) in MTs performed during COVID-19. Medium and low volume centers without change in local triage policy showed no change in MTs performed during COVID-19 (Fig. 5 ).
Fig. 4.
Average monthly Mechanical Thrombectomies performed (4A) and median percentage change in Mechanical Thrombectomies (4B) pre- and during-COVID-19 globally and amongst countries with at least 3 or more responses with or without change in pre-hospital stroke triage policy
Fig. 5.
A-B: Average monthly Mechanical Thrombectomies (5A) and median percentage change in Mechanical Thrombectomies (2B) pre- and during-COVID-19 globally with or without change in pre-hospital stroke triage policy
Countries with STP, Germany, France, Italy and Poland reported a median increase of 35% (IQR -15 – 113), 120% (IQR -16 – 240), 185% (IQR 108 – 209) and 0% (IQR -53 – 125) respectively (Fig. 4). All the centers that responded from countries with STP change were high-volume MT centers, reporting a 22% median percentage increase in MT during COVID-19 (Fig. 5).
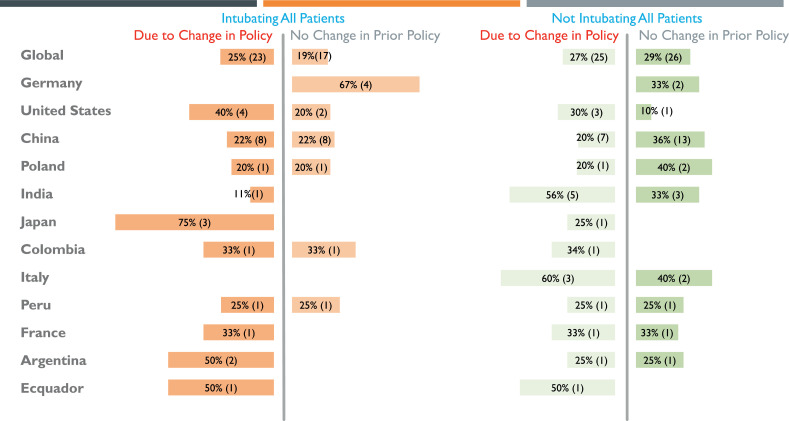
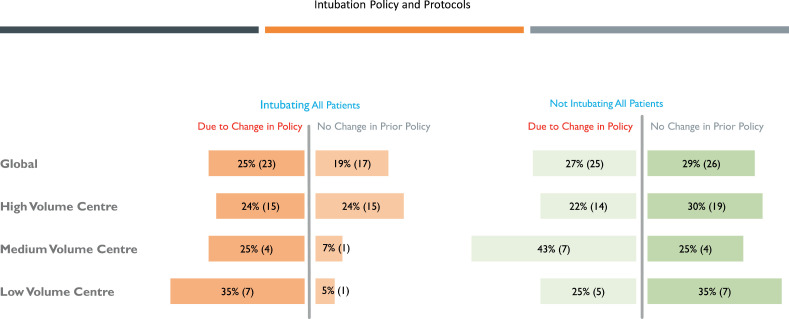
Intubation policy
Intubation policy for during the performance MT was variable across countries and centers pre and during COVID-19 pandemic. Also, any change of policy due to the pandemic did not have preponderance in one direction (Fig. 6 ). During COVID-19, 44% centers preferred intubation (PI) during MT, including 25% centers that changed their policy to PI during-COVID-19 from preferred non-intubation (PNI) pre-COVID-19. On the other hand, 56% centers PNI which included 27% centers that changed their policy from PI to PNI (Fig. 6). Based on volume, 48% high, 32% medium and 40% low volume centers preferred intubation during MT, which included 24%, 25% and 35% centers respectively that reported a change in policy to PI from PCS during COVID-19 (Fig. 7 ).
Fig. 6.
A global representation of intubation policy and direction of change to or from preferred intubation for patients undergoing Mechanical Thrombectomy during COVID-19 pandemic amongst countries with at least 3 or more responses.
Fig. 7.
A global representation of intubation policy and direction of change to or from preferred intubation for patients undergoing Mechanical Thrombectomy during COVID-19 pandemic based on high, medium or low-volume stroke centers.
There is wide variation in preference for intubation policy within countries, none of the centers in Italy versus 67% centers in Germany preferred intubation during COVID-19. None of the centers in Germany changed their intubation policy during COVID-19, whereas all centers in Japan reported a change in intubation policy including 75% to PI and 25% to PNI (Fig. 6).
Anesthesia policy and reported Covid-19 infections in personnel
Amongst centers with PI, 20.9% (9/43) reported at least 1 or more stroke or neuroendovascular team personnel testing positive for COVID-19 versus 16.1% (9/56) centers with PNI (p=0.6). Furthermore 18.9% (10/53) centers with change in intubation policy during COVID-19 pandemic in either direction reported at least one COVID-19 infection amongst stroke or neuroendovascular team personnel versus 17.4% (8/46) centers with no change in policy (p=1) (supplemental item 2).
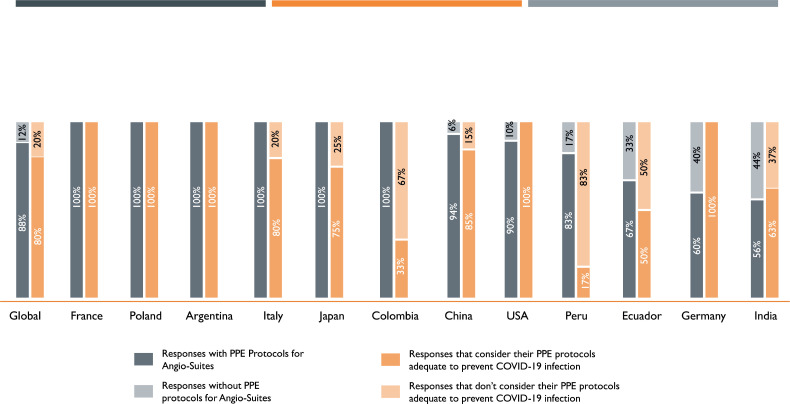
Personal protective equipment
Globally, 88% participating stroke centers reported neuroendovascular-specific written PPE protocols and 80% considered them to be adequate. Fig. 8 A shows responses from individual countries. Amongst centers based on volume, reportedly low-volume centers are less likely to have neuroendovascular specific written PPE protocols (74% versus 88% or 89% high or medium-volume respectively) and when present, less likely to report them to be adequate (58% vs. 92% or 81% high or medium-volume respectively) (p=0.25) (Fig. 8B).
Fig. 8.
A-B: A global representation of presence of established written personal-protective-equipment protocols specific for neuro-interventional suite and if these protocols were considered adequate to prevent SARS-CoV-2 infection amongst countries with at least 3 or more responses (8A), and amongst high, medium or low volume stroke centers (8B).
PPE and reported Covid-19 infections in personnel
Amongst centers with written neuroendovascular-specific PPE protocols, 19.1% (16/84) reported at least one or more stroke or neuroendovascular team personnel COVID-19 infection versus 14.3% (2/14) centers without these protocols (p=1.00). In centers where the respondents felt the neuroendovascular-specific PPE protocols were adequate, notably 20.5% (16/78) reported at least one or more COVID-19 infection amongst stroke or neuroendovascular team personnel versus 12.5% (2/16) respondents in centers that reported the PPE protocols to be inadequate (p=0.73).
Similarly, there was no statistically significant difference noted in availability of respective PPE equipment such as N95 masks (p=0.51), Surgical masks (p=1.00), Bunny suit (p=0.34) and Face shield (p=0.51), and COVID-19 infection amongst stroke or neuroendovascular team personnel (supplemental item 3).
Discussion
The COVID-19 pandemic has a significantly impacted the emergency response mechanisms of the healthcare systems worldwide. This cross-sectional convenience survey by the MT2020+ global alliance reports an international snapshot of the significant changes in acute stroke care with an emphasis on mechanical thrombectomy systems of care. Our study shows that worldwide, stroke specialists report an overall median percentage decrease of 33% in stroke admissions and 25% in MT procedures performed during COVID-19 pandemic. A similar trend of reduced stroke admissions and about 25% decrease in acute stroke interventions such as intravenous thrombolysis (IVT) and MT was reported in a survey completed by members of World Stroke Organization.8 Our results are also consistent with the literature showing reduced admissions of patients presenting with more life threatening emergencies such as myocardial infarction9 , 10 and large vessel occlusion (LVO) strokes or delays in arrival to hospitals during COVID-19 pandemic.11 The department of Veteran Affairs, the largest healthcare system in the US, reported a decrease of 41.9% inpatient admissions starting mid-March to April compared to beginning of the year 2020.12 A large population based study from Joinville, Brazil reported a 36.4% reduction in TIA, mild and moderate stroke admissions but no difference in admissions for severe stroke (NIHSS >8) during 30 days immediately post the pandemic restrictions were imposed on March 17th 202013 Another large study from North Spain reported statistically significant decrease in mean weekly stroke admissions to the tertiary referral hospitals but no difference in proportion of IVT or MT performed from December 30th 2019 to May 3rd 2020.14 Similarly, a large national survey in China that included participants from 280 stroke centers reported approximately 40% drop in stroke admissions and about 25% reduction in thrombolysis and thrombectomy cases during the month of February 2020 compared to the same in 2019.15 In addition, a multicenter observational study across 8 states in the US reported significant decline in weekly stroke admissions, but the proportion of patients receiving IVT and MT remained the same during the months of March, April and May 2020 compared to the same period in 2019.16
In the subgroup of countries of Germany, France, Italy and Poland, there was a median percentage increase of 85% and 113% in stroke admissions in medium and high-volume centers respectively and 22% increase in MT performed in high-volume centers due to a pandemic-related change in their pre-hospital stroke triage policy to direct all strokes to designated centers only during the pandemic. As such, this reported increase in stroke admissions and MT performed in countries with STP change is unlikely to represent a true measure of the overall change in the stroke admission and MT during COVID-19 pandemic. On the other hand, countries without change in STP provide a better snapshot of the direction of change in stroke admissions and MT performed. High and medium-volume centers in countries without STP change reported a median percentage decrease of 50% and 17% respectively in stroke admissions and a median decrease of 21% in MT performed in high-volume centers.
While our survey could not address the specific reasons for the decrease in stroke admissions and MT volumes, it is consistent with other reports of indirect effects of social distancing, delaying detection of neurological changes in independently living elderly patients and increased out-of-hospital mortality during mid-March to April compared to pre-pandemic months.17
A prospective international study during COVID-19 surge reported longer door-to-reperfusion times (138 vs. 100 min) and higher in-patient mortality (RR 1.87) in patients undergoing preferred intubation for MT,18 though details about direction of institutional intubation policy change in respective centers due to COVID-19 was not detailed. While there is no consensus regarding the optimal intubation policy for MT, our survey was able to capture the magnitude of any change in the intubation policy at centers in response to the pandemic. Our study shows that 52% stroke centers instituted intubation policy change for patients undergoing MT with an almost equal change in either direction: 25% changed their policy to PI from PNI and 27% centers changed their policy to PNI from PI. Interventional cardiology expert consensus guidelines recommended a low threshold for intubating patients prior to transfer to catheterization suite to avoid emergent intubation and reduce potential transmission risk to catheterization staff.19 Similarly, the neuroendovascular expert consensus statements encouraged adequate PPE precautions, and lower threshold for intubation when adequate negative pressure rooms are available to reduce the possible risk of infection. This is supported by the evidence that about 6 – 14% patients undergoing MT require emergent intubation during procedure,20 therefore reducing the threshold for intubating all patients undergoing MT with unknown COVID-19 status preemptively in a more controlled environment such as negative pressure room prior to the procedure has the potential in reducing the risk of transmission of COVID-19 infection to neuroendovascular staff. Our data did not show a significant difference in infection rates amongst stroke or neuroendovascular staff with PI versus PNI or change in intubation policy in either direction, though it's important to note that the study was not powered to make these associations.
An international study across 35 centers with neuroendovascular units showed a strong positive correlation between number of quarantined providers (38%) and those testing positive for COVID-19 (12%), suggesting appropriate and effective implementation of quarantine measures though the details of these measures were not discussed.21 In addition, the elective interventions in these centers were reportedly canceled within median 14 days from first reported case of COVID-19 in their respective regions, which could explain the lower rates of infection amongst the providers compared to infection rates in their respective communities, thus allowing continued availability of emergency thrombectomy services.21 In our survey, majority of the centers reported establishing written neuroendovascular-specific PPE protocols (88%) and amongst the centers with these protocols, majority respondents considered them to be adequate (80%). Interestingly, we did not find any significant difference between the presence of established neuroendovascular-specific PPE protocols or reported adequacy of the same with rate of COVID-19 infections amongst stroke or neuroendovascular staff, but again our study was not powered to conclusively analyze these differences. Low-volume stroke centers in comparison to high or medium-volume centers are less likely to have established neuroendovascular-specific PPE protocols (74% versus 88% or 89%, respectively); and if established, only 58% respondents from these centers considered them to be adequate compared with large or medium-volume centers (92 or 81% respectively).
This study is based on a convenience cross-sectional survey and does not represent a random sample of global medical institutions, and therefore the results should be viewed considering this important limitation. Though separate analysis was conducted restricted to countries with three or more responses to provide a better representation of practices within a particular country, there is a potential for reporting bias which can skew the data for a given country. The actual time frame defining pre and during COVID-19 infection was left to the respondents and was therefore variable due to differences in first reported COVID-19 infection in their respective cities or countries. In addition, we analyzed and reported the countries with pandemic related change in pre-hospital STP separately. This is important as change in pre-hospital triage of stroke patients during the pandemic to designated tertiary care stroke centers lead to an increase in stroke admissions in these centers. Nevertheless, pertinent reason to include these countries with pre-hospital STP is to present a complete picture of the effects of the pandemic on stroke systems of care including effects of the STP change. A convenience survey is a useful tool to study physician practices and changes implemented due to unprecedented healthcare crisis during COVID-19 pandemic. Average survey response rates amongst healthcare professionals is about 53%,22 therefore the lower response rates in our survey can potentially lead to non-response bias and the survey results should be viewed keeping this limitation in mind.23
To conclude, our data provides a valuable snapshot of the impact of the first surge of the COVID-19 pandemic on global stroke systems of care and provides lessons for the future. It highlights the need to increase public awareness about seeking urgent medical care for focal neurological deficits. More studies are needed to shed light on whether PI versus PNI or avoiding adopting intubation policy changes in workflow helps curtail COVID-19 infection despite adequate PPE precautions or not. However, it's unclear at this juncture that changes in local healthcare policy varying from pre-hospital triage or preferred-intubation affected the long-term patient outcomes. These results can be useful to policymakers to anticipate and counter adverse stroke care changes during future public healthcare emergencies.
Funding
The survey was supported by funds from the Society of Vascular and Interventional Neurologists.
Declaration of Competing Interest
Dr. Yavagal is on the steering committee of TIGER clinical trial sponsored by Rapid Medical and steering committee of CALM-2 sponsored by Vascular Dynamics. He is a consultant to Medtronic, Cerenovus, Poseydon, Neurosave, and other Neuralanalytics. All of these relationships are outside of the current work.
All other co-authors declare that there are no conflicts of interest.
Acknowledgements
None
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jstrokecerebrovasdis.2021.105806.
Appendix. Supplementary materials
References
- 1.Organization WH. WHO Coronavirus Disease (COVID-19) Dashboard, https://covid19.who.int (2020, accessed 5th July 2020).
- 2.Nguyen TN, Abdalkader M, Jovin TG, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the society of vascular and interventional neurology. Stroke. 2020;51:1896–1901. doi: 10.1161/strokeaha.120.030100. 2020/04/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fraser JF, Arthur AS, Chen M, et al. Society of neuro interventional surgery recommendations for the care of emergent neurointerventional patients in the setting of COVID-19. J Neurointervent Surg. 2020;12:539–541. doi: 10.1136/neurintsurg-2020-016098. 2020/04/17. [DOI] [PubMed] [Google Scholar]
- 4.Aggour M, White P, Kulcsar Z, et al. European society of minimally invasive neurological therapy (ESMINT) recommendations for optimal interventional neurovascular management in the COVID-19 era. J Neurointervent Surg. 2020;12:542–544. doi: 10.1136/neurintsurg-2020-016137. [DOI] [PubMed] [Google Scholar]
- 5.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hajdu SD, Pittet V, Puccinelli F, et al. Acute stroke management during the COVID-19 pandemic. Stroke. 2020;51:2593–2596. doi: 10.1161/STROKEAHA.120.030794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mission Thrombectomy, https://missionthrombectomy2020.org/about-mt2020/ 2020.
- 8.The global impact of COVID-19 on stroke - survey report from Prof. marc Fischer, WSO President-Elect, https://www.world-stroke.org/news-and-blog/news/the-global-impact-of-covid-19-on-stroke-survey (accessed 12th July 2020).
- 9.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. 2020/04/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Filippo O, D'Ascenzo F, Angelini F, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. 2020/04/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teo K-C, Leung WCY, Wong Y-K, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51:2228–2231. doi: 10.1161/STROKEAHA.120.030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 Pandemic. Jama. 2020 doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Diegoli H, Magalhães PSC, Martins SCO, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 Era. Stroke. 2020;51:2315–2321. doi: 10.1161/strokeaha.120.030481. 2020/06/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tejada Meza H, Lambea Gil Á, Saldaña AS, et al. Impact of COVID-19 outbreak on ischemic stroke admissions and in-hospital mortality in North-West Spain. Int J Stroke Offic J Int Stroke Soc. 2020;15:755–762. doi: 10.1177/1747493020938301. 2020/06/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao J, Li H, Kung D, et al. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51:1996–2001. doi: 10.1161/strokeaha.120.030225. 2020/05/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ortega-Gutierrez S, Farooqui M, Zha A, et al. Decline in mild stroke presentations and intravenous thrombolysis during the COVID-19 pandemic: the society of vascular and interventional neurology multicenter collaboration. Clin Neurol Neurosurg. 2021;201 doi: 10.1016/j.clineuro.2020.106436. 2021/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marijon E, Karam N, Jost D, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Publ Health. 2020 doi: 10.1016/s2468-2667(20)30117-1. 2020/05/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al Kasab S, Almallouhi E, Alawieh A, et al. International experience of mechanical thrombectomy during the COVID-19 pandemic: insights from STAR and ENRG. J Neurointervent Surgery. 2020;12:1039–1044. doi: 10.1136/neurintsurg-2020-016671. 2020/08/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PloS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. 2012/05/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schönenberger S, Möhlenbruch M, Pfaff J, et al. Sedation vs. Intubation for Endovascular Stroke TreAtment (SIESTA) - a randomized monocentric trial. Int J Stroke Offic J Int Stroke Soc. 2015;10:969–978. doi: 10.1111/ijs.12488. 2015/04/14. [DOI] [PubMed] [Google Scholar]
- 21.Alawieh A, Al Kasab S, Almallouhi E, et al. Letter: an international investigation into the COVID-19 pandemic and workforce depletion in highly specialized neurointerventional units - insights from stroke thrombectomy and aneurysm registry and endovascular neurosurgery research group. Neurosurgery. 2020 doi: 10.1093/neuros/nyaa415. 2020/09/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cho YI, TP Johnson, Vangeest JB. Enhancing surveys of health care professionals: a meta-analysis of techniques to improve response. Eval Health Prof. 2013;36:382–407. doi: 10.1177/0163278713496425. 2013/08/27. [DOI] [PubMed] [Google Scholar]
- 23.Phillips AW, Reddy S, Durning SJ. Improving response rates and evaluating nonresponse bias in surveys: AMEE Guide No. 102. Med Teach. 2016;38:217–228. doi: 10.3109/0142159x.2015.1105945. 2015/12/10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.