Abstract
Coronavirus disease 2019 (COVID-19) is a clinical syndrome caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Patients with severe disease show hyperactivation of the immune system, which can affect multiple organs besides the lungs. Here, we propose that SARS-CoV-2 infection induces a process known as immunothrombosis, in which activated neutrophils and monocytes interact with platelets and the coagulation cascade, leading to intravascular clot formation in small and larger vessels. Microthrombotic complications may contribute to acute respiratory distress syndrome (ARDS) and other organ dysfunctions. Therapeutic strategies aimed at reducing immunothrombosis may therefore be useful. Several antithrombotic and immunomodulating drugs have been proposed as candidates to treat patients with SARS-CoV-2 infection. The growing understanding of SARS-CoV-2 infection pathogenesis and how it contributes to critical illness and its complications may help to improve risk stratification and develop targeted therapies to reduce the acute and long-term consequences of this disease.
Subject terms: Coagulation system, Antimicrobial responses, Cytokines, Innate immunity, Viral infection
Here, the authors propose that SARS-CoV-2 induces a prothrombotic state, with dysregulated immunothrombosis in lung microvessels and endothelial injury, which drive the clinical manifestations of severe COVID-19. They discuss potential antithrombotic and immunomodulating drugs that are being considered in the treatment of patients with COVID-19.
Introduction
Coronavirus disease 2019 (COVID-19) is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and can present with a range of manifestations, including pneumonia and acute respiratory distress syndrome (ARDS)1. Although many individuals develop asymptomatic or paucisymptomatic SARS-CoV-2 infection, those with severe-to-critical disease show a dysregulated hyperactivation of the immune system that can cause an abnormal cytokine immune response and is likely to be responsible for most of the organ damage occurring in the late phase of the disease2.
It is now apparent that SARS-CoV-2 infection induces a prothrombotic state manifesting especially with microthrombosis3,4, as observed in patients with COVID-19 and in post-mortem samples from individuals who died after SARS-CoV-2 infection5–9. This thrombotic state is reminiscent of a process known as immunothrombosis (Box 1; Fig. 1), in which the immune and coagulation systems cooperate to block pathogens and limit their spread10. In this Perspective, we describe how SARS-CoV-2 might induce a prothrombotic state and discuss how currently available and developing therapies may address COVID-19-associated immunothrombosis.
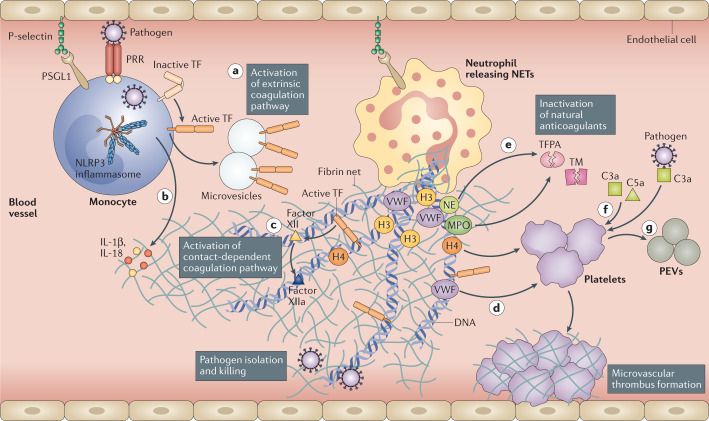
Fig. 1. Immunothrombosis is important in promoting immune defence.
Following recognition of a pathogen through pattern recognition receptors (PRRs), monocytes and monocyte-derived microvesicles present activated tissue factor (TF) on their surfaces and release it at sites of pathogen localization, thus activating the extrinsic pathway of coagulation (path a). Pathogens also stimulate the NLRP3 inflammasome in monocytes and/or macrophages, leading to the release of pro-inflammatory cytokines, such as interleukin-1β (IL-1β) and IL-18 (path b). Neutrophils are recruited and contribute to this process through the release of neutrophil extracellular traps (NETs), which directly activate factor XII and, thus, the contact-dependent pathway of coagulation (path c). NETs also bind von Willebrand factor (VWF) and help to recruit platelets (path d). Histones, in particular H3 and H4, trigger activation of platelets. In addition, neutrophil elastase (NE) and myeloperoxidase (MPO) in NETs cleave and inactivate natural anticoagulants (tissue factor pathway inhibitor (TFPA) and thrombomodulin (TM)) (path e). Finally, NETs can externalize and bind TF, promoting activation of the extrinsic pathway of coagulation. Platelets support the immunothrombotic process by activating the contact-dependent pathway of coagulation through the release of polyphosphates and, along with endothelial cells, may promote fibrin generation. Platelets can also be activated by C3a and C5a (path f). Activated platelets release large amounts of pro-inflammatory cytokines in platelet extracellular vesicles (PEVs) (path g). Through this mechanism, pathogens such as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) become trapped within the fibrin-based NETs and killed. The immunothrombotic process allows pathogen killing to be restricted to the intravascular compartment, thus limiting injury to organs. Although it is clear that immunothrombosis participates in SARS-CoV-2 pathogenesis, the exact mechanisms are still under investigation. These may include the following: direct injury of endothelial cells by the virus and consequent activation of the coagulation cascade; infiltration of neutrophils that lead to NET formation; induction of hypoxaemia causing upregulation of TF expression by hypoxia-inducible transcription factors and formation of clots; activation of complement that promotes coagulation and recruits and activates platelets, monocytes and neutrophils, thus triggering TF expression; and an abnormal increase in the levels of pro-inflammatory cytokines causing direct cell damage.
Box 1 Immunothrombosis: a conserved mechanism of host defence.
The term immunothrombosis was originally described by Engelmann and Massberg to refer to an intrinsic effector pathway of innate immunity triggered by pathogens and injured cells to reduce the spread and survival of the invading pathogens10,157. By contrast, the term ‘thromboinflammation’ refers to a process in which inflammation and thrombosis coexist within microvessels in response to harmful stimuli (pathogens, injured cells or other irritants)158. Immunothrombosis is mainly triggered by neutrophils and monocytes and is supported by the formation of microthrombi in small vessels, in which endothelial cells exposed to microorganisms adopt a pro-adhesive phenotype159.
During immunothrombosis, neutrophils and monocytes release tissue factor and extracellular nucleosomes and degrade endogenous anticoagulants, thereby facilitating activation of coagulation induced by inflammation160. Importantly, tissue factor decorates neutrophil extracellular traps (NETs), as found in sepsis161 and, more recently, in coronavirus disease 2019 (COVID-19)-related immunothrombosis86. NETosis by neutrophils also enhances the activity of the coagulation system by increasing fibrin deposition162,163. Histones present in NETs, especially histones H3 and H4, can dose-dependently enhance thrombin generation not only by reducing thrombomodulin-mediated protein C activation164 but also by directly activating platelets141. Finally, NETs can bind plasma proteins needed for platelet adhesion and thrombus development, such as fibronectin and von Willebrand factor (VWF)141. In turn, platelets participate in this process in several ways: they increase the accumulation of immune cells that express tissue factor10,165; they bind directly to neutrophils and NETs162,166,167; they release damage-associated molecular patterns that promote tissue factor expression within thrombi168; and they directly bind to microorganisms for presentation to innate immune cells169,170.
Microorganisms have evolved mechanisms to escape immunothrombosis, such as the expression of streptokinase to dissolve fibrin171 or nucleases to degrade NETs172,173. Some bacteria use immunothrombosis to avoid their killing, such as Staphylococcus aureus, whose staphylocoagulase and VWF-binding protein trigger fibrin generation to form a biofilm and an abscess pseudocapsule174,175.
In sum, immunothrombosis can be considered a beneficial mechanism of intravascular immunity. However, when immunothrombosis is uncontrolled, it causes dysregulated activation of the coagulation cascade, leading to microthrombus formation and inflammation, which in turn enhance each other and may, ultimately, develop into thrombosis (thromboinflammation) and disseminated intravascular coagulation.
Immunothrombosis in COVID-19
COVID-19-associated hyperinflammation
The clinical spectrum of COVID-19 ranges from asymptomatic or paucisymptomatic (in up to 45% of individuals) to severe disease requiring admission of patients to the intensive care unit (ICU)11. Generally, 3–10% of subjects requires hospitalization, with up to 20% of them experiencing severe disease and a high mortality rate12,13. The initial phase of COVID-19 is characterized by damage directly driven by the virus. After approximately 7–10 days of symptoms (including fever, cough, fatigue, anorexia and myalgias), a subgroup of patients progresses to severe disease and develops hypoxaemia (low oxygen levels in the blood) and dyspnoea (shortness of breath), potentially evolving towards ARDS14. This stage of the disease is characterized by high levels of pro-inflammatory cytokines, such as interleukin-6 (IL-6), IL-1β, IL-18 and granulocyte–macrophage colony-stimulating factor (GM–CSF)2,15–17. This event has been referred to as a cytokine storm18,19, although recent evidence suggests that cytokine levels in patients with COVID-19 are lower than those reported in patients with non-COVID-19 ARDS, sepsis, influenza virus infection and chimeric antigen receptor (CAR) T cell-induced cytokine release syndrome20,21. SARS-CoV-2 has been shown to trigger the IL-1/IL-6 pathway to a larger extent than other coronaviruses22. Through the analysis of lungs of patients who died from COVID-19-related ARDS, SARS-CoV-2 was found to activate the NLRP3 inflammasome23,24. In vitro studies also showed NLRP3 inflammasome activation by SARS-CoV-2 infection of primary human monocytes. In addition, NLRP3 inflammasome products, such as IL-1β and IL-18, are increased in patients with severe COVID-19 and positively correlated with adverse clinical outcomes24. These findings support a potential relationship between SARS-CoV-2 infection and inflammatory features, such as the dysregulated cytokine response.
Increased levels of ferritin have also been observed among patients with COVID-19, similar to what is observed in macrophage activation syndrome16,19,25. Even though ferritin levels observed in macrophage activation syndrome are markedly higher than those currently observed in COVID-19 (≥10,000–100,000 ng ml–1 versus 500–3,000 ng ml–1), ferritin levels remain predictive of poor outcomes in COVID-19 (refs26,27).
With regard to inflammatory cells, large numbers of CD68+ macrophages were observed in the alveoli of patients who died from COVID-19-associated pneumonia, and SARS-CoV-2 proteins were detected in CD68+ alveolar macrophages28,29. Analysis of the bronchoalveolar fluid of patients with severe or critical COVID-19 showed a higher percentage of macrophages and neutrophils and a lower proportion of myeloid dendritic cells, plasmacytoid dendritic cells and T cells than that of patients with moderate disease30. They also had higher levels of pro-inflammatory cytokines (such as IL-6, IL-8 and IL-1β) and chemokines (such as CCL2, CCL3, CCL4 and CCL7) in the bronchoalveolar fluid30. These data suggest that lung macrophages contribute to inflammatory responses in SARS-CoV-2 infection, favouring excessive inflammation in severe pneumonia. Similar to other respiratory infections, leukocyte recruitment to the lungs is finely tuned by specific molecules31, the uncontrolled activity of which may result in complications observed in patients with COVID-19 in both the lungs and other organs5,32.
COVID-19-associated coagulopathy
An important pathophysiological feature of COVID-19 is the development of a prothrombotic state. The occurrence of a COVID-19-specific coagulopathy is suggested by elevated levels of fibrinogen, von Willebrand factor (VWF) and the fibrin degradation product D-dimer in the blood, whereas patients generally show minor or no changes in prothrombin time (a measure of time to clot), activated partial thromboplastin time (coagulation time), antithrombin levels, activated protein C levels and platelet count33–36. These features are more consistent with a state of hypercoagulability coupled with a severe inflammatory state rather than with classical disseminated intravascular coagulation (DIC)36. Indeed, DIC has been reported in a few patients, usually in the advanced stages of the disease33,37,38. Recently, low antithrombin levels were linked to poor outcomes in COVID-19, especially among patients with obesity39. Hence, it is possible that antithrombin activity changes as SARS-CoV-2 infection worsens and a putative mechanism might be the cytokine-driven imbalance in endogenous anticoagulant levels40. In macrophage activation syndrome, liver function impairment is a typical feature and may contribute to coagulopathy, yet liver impairment in COVID-19 is usually mild and transient, without overt acute liver injury41,42.
Apart from a state of hypercoagulability in the lungs of patients with ARDS, a hypofibrinolytic state in the alveolar space was observed in COVID-19-related ARDS due to increased levels of fibrinolytic inhibitors43. Accordingly, high levels of plasminogen activator inhibitor 1 (PAI1) were described in patients with SARS-CoV44.
In order to properly identify COVID-19-associated coagulopathy, Iba et al. proposed the occurrence of two or more of the following four criteria in cases of proven COVID-19: a decrease in platelet count (<150 × 109 l–1); an increase in D-dimer levels (more than two times the upper limit of normal); prothrombin time >1 s or international normalized ratio >1.2; and the presence of thrombosis (macrothrombosis and/or microthrombosis)45. The risk of COVID-19-associated coagulopathy is defined by one of the aforementioned four criteria and one of the following ones: increased fibrinogen levels; increased VWF levels (more than two times the upper normal limit); or the presence of lupus anticoagulant and/or high-titre antiphospholipid antibodies45. Importantly, COVID-19-associated coagulopathy and risk of COVID-19-associated coagulopathy may further progress and/or predispose to DIC as COVID-19 severity increases.
COVID-19-associated endothelial dysfunction
Although COVID-19 should be regarded as a systemic disease, it acutely causes a lung-centred injury primarily affecting the vascular endothelium. COVID-19-associated pneumonia is characterized by infiltration of the lungs with macrophages and neutrophils that cause diffuse lung alveolar damage, the histological equivalent of ARDS46–48. Similar findings were previously reported in patients with SARS-CoV49. However, the striking finding in COVID-19 compared with SARS-CoV is the more extensive viral infection within the lungs, which results in more diffuse inflammation involving the pulmonary vessels50. This extensive infection reflects the particular tropism of SARS-CoV-2 for angiotensin-converting enzyme 2 (ACE2) — the cellular receptor for SARS-CoV-2 — expressed by type II pneumocytes51, which are anatomically close to the lung vascular network and are typically described to be hyperplasic in samples from patients with COVID-19 (refs52–54). This hyperplasia of endothelial cells is likely to be caused by lung tissue ischaemia due to congestion of small vessels by inflammatory cells (that is, immunothrombosis) and thrombosis in large vessels55.
Endothelial dysfunction was suggested to be an important pathophysiological event in infections by other coronaviruses, which can directly infect endothelial cells56–59. SARS-CoV-2 directly infects vascular endothelial cells and leads to cellular damage and apoptosis, thus decreasing the antithrombotic activity of the normal endothelium7,55. Alveolar damage, vessel wall oedema, hyaline thrombi, microhaemorrhage and diffuse thrombosis of peripheral small vessels have emerged as key features of COVID-19 contributing to respiratory failure6,8,46 (Fig. 2).
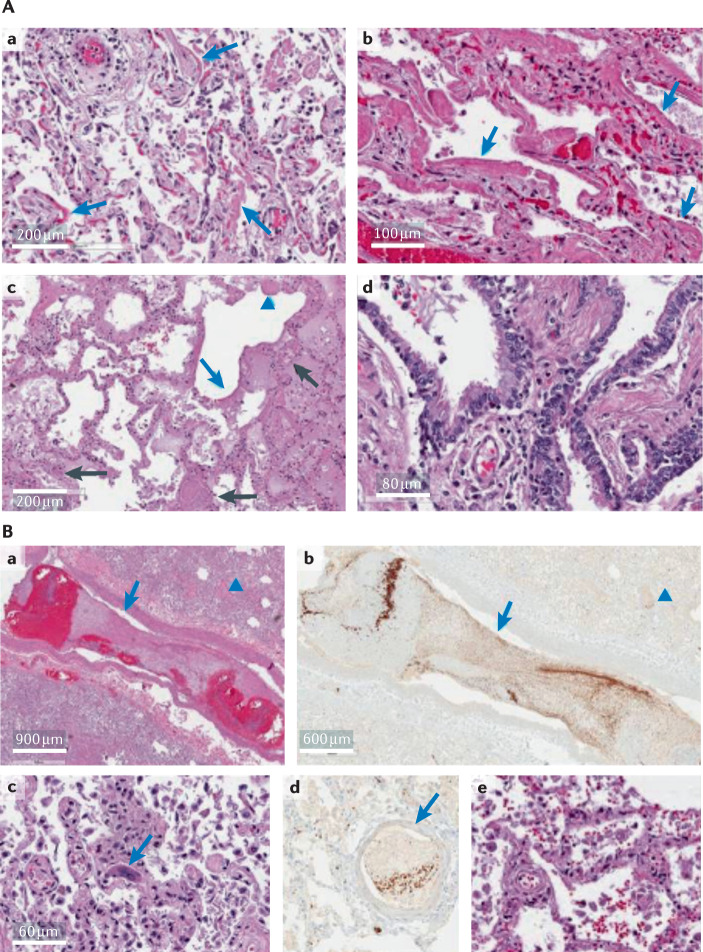
Fig. 2. Seminal pathology features of patients with COVID-19.
A | Hyaline membrane formation is a typical finding in patients with alveolar damage irrespective of being ventilated or not (blue arrows in panels a and b). Organizing fibrosis (blue arrowhead) and fibrin thrombi in small blood vessels (black arrows) with oedema, along with extensive haemorrhage (haematoxylin and eosin staining) and hyaline membranes (blue arrows) (panel c). The bronchial respiratory mucosa is almost entirely intact and no squamous metaplasia is evident (panel d), different to that observed in patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). B | Two thrombi, one in a small pulmonary artery (blue arrow) and one in a pulmonary venule (blue arrowhead), in the haematoxylin and eosin staining (panel a) and in the CD61 immunostaining for platelets within thrombi (panel b). Megakaryocytes within small vessels and alveolar capillaries (panel c, blue arrow). CD61 immunostaining of a fibrin- and platelet-rich thrombus in a small vessel (panel d), with a megakaryocyte stained below (blue arrow). Small, perivascular aggregates of lymphocytes (panel e). COVID-19, coronavirus disease 2019. Images reprinted from The Lancet, 8, Fox, S. E. et al., Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans, 681–686, Copyright (2020), with permission from Elsevier (ref.6).
Endothelial cells of lung blood vessels can be activated by the high levels of pro-inflammatory cytokines (IL-1, IL-6 and TNF) and ferritin in severe COVID-19 (ref.60). Moreover, increased levels of the endothelial adhesion protein VWF were reported both in patients admitted to the ICU and in non-critically ill patients34,35,61,62, and this increase seems to be associated with a mild reduction in the activity of a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS13), a metalloproteinase that regulates the size of VWF multimers63. Endothelial cell perturbation along with the release of large VWF multimers and relative insufficient VWF cleavage owing to ADAMTS13 consumption may account for increased platelet–vessel wall interactions causing thrombotic microangiopathy. Indeed, a relative deficiency in ADAMTS13 activity was previously described in inflammatory conditions with high levels of IL-6, as found in patients with SARS-CoV-2 infection64. Other markers of endothelial cell injury have been recently investigated. Higher levels of soluble P-selectin (a marker of endothelial and platelet activation) were observed in patients admitted to the ICU than in patients not in the ICU, whereas increased levels of thrombomodulin (a specific marker of endothelial activation generally released during endothelial cell injury) were associated with increased mortality risk35. Higher numbers of circulating endothelial cells were described in patients with COVID-19, especially among those admitted to the ICU, and the presence of circulating endothelial cells positively correlated with platelet and lymphocyte counts and with the classical endothelial marker soluble vascular cell adhesion molecule 1 (sVCAM1)65. This was recently confirmed by another report from Italy, showing that patients with COVID-19 had increased circulating endothelial cells and higher plasma levels of soluble intercellular adhesion molecule 1 (sICAM1) and sVCAM1, further supporting the concept of endothelial dysfunction in COVID-19 (ref.66).
Considering the important role of the endothelium in regulating haemostasis, fibrinolysis and vessel wall permeability, endothelial dysfunction in pulmonary microvessels acts as a trigger for immunothrombosis, resulting in the coagulopathy observed in patients with COVID-19 (refs27,47,67,68). In addition, endothelial dysfunction is recognized as a risk factor of microvascular dysfunction through a shift towards vasoconstriction, by promoting ischaemia, inflammation and a procoagulant state69. In addition, the inflammatory environment triggers the expression of activated tissue factor on endothelial cells, macrophages and neutrophils, which amplifies activation of the coagulation cascade within the lungs60. These events fuel a positive immunothrombotic feedback loop in which hyperinflammation triggers the hypercoagulant state, with thrombosis occurring within pulmonary microvessels. Lastly, platelet activation within the microvasculature is increased in patients with severe COVID-19 and is associated with poor outcomes70,71. Platelet–vessel wall interactions, mediated by surface receptors (integrins and selectins) and adhesive proteins (VWF and fibrinogen), impair vessel wall integrity or increase endothelial injury, ultimately leading to microvascular obstruction72. Moreover, platelets were found to be hyperactivated in patients with COVID-19 and to be a source of procoagulant extracellular vesicles73 and polyphosphates, which can exacerbate the thromboinflammatory cascade via neutrophils74. Of importance, activated platelets are critically involved in neutrophil extracellular trap (NET) formation71, which is an essential element of immunothrombosis. All of these elements support the hypothesis that endothelial dysfunction, or endotheliopathy35,75, and platelet activation are key features of COVID-19-associated coagulopathy and may mediate the damage leading to severe disease.
COVID-19-associated ARDS
COVID-19-related ARDS is considered atypical, with its main characteristic being a dissociation between hypoxaemia severity and relatively good respiratory mechanics76,77. From a clinical standpoint, two phenotypes are described67,78. Patients with ‘type L’ have high lung compliance, lower lung weight as estimated by computed tomography scan and poor response to positive end-expiratory pressure. Patients with ‘type H’ are those with a deteriorating disease or suboptimally treated disease that present with areas of accumulation of inflammatory exudate in the alveoli as observed through computed tomography scan, low lung compliance, greater lung weight and good response to positive end-expiratory pressure. This clinical picture couples with endothelial damage, breaking down pulmonary vasoregulation, stimulating ventilation–perfusion mismatch — which is mainly responsible for hypoxaemia — and supporting immunothrombosis. In this respect, the events leading to atypical ARDS can be summarized by the term ‘microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome’ (MicroCLOTS)79. According to this proposed definition, ARDS is the result of a hyperimmune reaction of the host to SARS-CoV-2 that is both directly mediated by the virus through cellular injury and release of pro-inflammatory signals and indirectly mediated by complement activation (Box 2), leading to leukocyte recruitment and increased release of pro-inflammatory cytokines. This results in a severe tissue injury with vascular endothelial dysfunction and alveolar cell damage, which may explain the progressive worsening of ventilation–perfusion mismatch and pulmonary microthrombosis79.
Box 2 The role of complement in sepsis.
The complement system is an important component of the innate immune system and activates following infections. After complement activation (through the classic, alternative or lectin pathways), the common pathway is responsible for the production of C3a and C5a, then stimulating formation of the C5b–9 membrane attack complex, which causes the lysis of pathogen cells176. In a mouse model of intranasal infection with severe acute respiratory syndrome coronavirus (SARS-CoV), early activation of the complement system, especially complement component C3, caused acute respiratory distress syndrome (ARDS)177. However, C3-deficient mice experienced reduced respiratory dysfunction, limited neutrophil and monocyte lung infiltration, and showed lower levels of cytokines both in the lungs and the blood177. Excessive activation of complement in the advanced phases of sepsis may therefore cause tissue injury contributing to organ failure.
The complement and coagulation pathways are closely linked178,179. In particular, complement end products can trigger the release of procoagulant products and reduce the production of natural anticoagulants178. Additionally, the binding of C1q to its receptor on platelets triggers the expression of integrins and P-selectin180, whereas C3 stimulates platelet activation and aggregation. The activation of C5 during the inflammatory response is responsible for the expression of tissue factor on leukocytes and endothelial cells181,182. Complement may indirectly induce procoagulant changes; for example, activated C3 and C5 contribute to cytokine release soon after the innate immune response starts, particularly increasing the concentrations of tumour necrosis factor (TNF) and interleukin-6 (IL-6).
NETs in COVID-19-associated immunothrombosis
NETs are likely to be important players in deregulated immunothrombosis in COVID-19 (ref.80). Indeed, ARDS can be considered as a NETopathy81; higher levels of NETs were described in the plasma and bronchoalveolar fluid of patients with transfusion-associated and pneumonia-related ARDS compared with those without ARDS82–84. NETs are markers of disease severity in patients with SARS-CoV-2 infection80,85. Compared with controls, patients with COVID-19 have higher levels of serum85 or plasma80 myeloperoxidase (MPO)–DNA complexes, which are biomarkers of circulating NET fragments, and further increases were found in those patients requiring invasive mechanical ventilation. MPO–DNA complexes and thrombin–antithrombin complexes were positively correlated in patients with COVID-19, and the anticoagulant dabigatran or complement targeting inhibited NETosis86, further suggesting a central role for NETs in the immunothrombotic milieu. MPO–DNA levels return to normal in convalescent plasma, indicating that this is a transient increase80. High-dimensional flow cytometric analysis of circulating neutrophils revealed a highly activated phenotype in patients with most severe COVID-19 (ref.71). Neutrophils can be found embedded in fibrin clots and in close association with platelets within microthrombi in the lungs80, heart and kidneys of patients with COVID-19 (ref.71). In severe disease, neutrophils adopted the so-called low-density phenotype that is more prone to spontaneously form NETs; this greater NETosis was linked to increased intravascular aggregation, leading to microthrombosis and organ damage87. NETs have also been identified in the lung parenchyma and alveolar space in autopsy case reports9,88. Interestingly, neutrophils from healthy donors showed increased adhesion to activated platelets in plasma from patients with COVID-19 compared with that from control patients, causing enhanced NET generation71. Indeed, both serum and plasma from patients with COVID-19 strongly stimulate the production of NETs from healthy neutrophils71,80,85. In addition, neutrophils isolated from patients with COVID-19 showed elevated NET release at baseline similar to phorbol myristate acetate (PMA)-stimulated neutrophils from healthy donors, indicating that the COVID-19 plasma environment promotes NET formation80. The virus itself is also reported to directly activate neutrophils towards NETosis, promoting epithelial cell death89. NETs may provide a scaffold for the deposition of C3, properdin and factor B, thus directly participating in complement activation90. This mechanism may fuel an amplifying feedback loop promoting further NET formation and platelet and endothelial cell activation91. The observation of antiphospholipid antibodies, which can directly stimulate NETosis92, in patients with COVID-19, as well as in other infections93, suggests that SARS-CoV-2 infection might synergize with antiphospholipid antibodies to promote the immunothrombotic process. Indeed, higher titres of antiphospholipid antibodies were associated with increased activity of neutrophils and platelets and more severe respiratory disease94.
Whether NETs are direct contributors to the dysregulated cytokine response is still unclear. Indeed, NETs participate in acute lung injury by inducing macrophage release of IL-1β, which in turn can increase NET formation95,96. In addition, most inflammatory mediators that are increased in patients with COVID-19 are known to regulate neutrophil activity through the expression of chemotactic products16,97. These data suggest that dysregulated cytokine release might be sustained by crosstalk between neutrophils and macrophages mediated by NETs, resulting in a deranged or exaggerated immunothrombotic status.
COVID-19: a syndrome of deregulated immunothrombosis?
On the basis of the aforementioned evidence, we propose that exaggerated immunothrombosis, occurring for the most part within lung microvessels, drives the clinical manifestations of COVID-19 (ref.3), although systemic viraemia early in the disease course may also be important98 (Fig. 1). The occurrence of severe events, such as acute respiratory failure and ARDS, may be explained by a deregulated process of immunothrombosis involving the pulmonary microcirculation. In support of this, there is increasing evidence that COVID-19 is a disease of the endothelium35 that results in elevated levels of PAI1 and VWF, increased platelet activation and a state of hypercoagulability, with consequent venous, arterial and microvascular thrombosis. The exact factors triggering this endotheliopathy have not yet been recognized, but potentially include the virus itself (causing endothelial cell injury that triggers the coagulation cascade involving fibrin and platelets47,99), immune cell (neutrophil and/or macrophage and platelet73,100,101) infiltration, hypoxaemia (that can induce hypoxia-inducible transcription factors that upregulate tissue factor expression102 and lead to fibrin-based clot formation, thus supporting a thromboinflammatory feedback loop), complement-mediated damage or a surge in pro-inflammatory cytokine (such as IL-1β and IL-6) release with direct cell damage.
Thrombosis management in COVID-19
If we consider COVID-19 as a vascular disease primarily involving the endothelium, an ideal therapeutic approach would be both antithrombotic and anti-inflammatory. Here, we describe some of the main approaches that are being explored to address these features of COVID-19 (Table 1).
Table 1.
Putative therapeutic approaches for COVID-19
| Therapeutic agent | Target | Outcome | Clinical trial | Refs |
|---|---|---|---|---|
| Antithrombotic drugs | ||||
| Heparin | Inactivation of thrombin and activated factor X through an antithrombin-dependent mechanism | Controversial evidence on mortality and need for mechanical ventilation from observational studies | – | 105,152–154 |
| Garadacimab | Factor II blockade | One study is ongoing | NCT04409509 | – |
| Nafamostat mesylate | Serine protease inhibitor of thrombin, plasmin and trypsin | Ongoing trials based on in vitro blockade of MERS-CoV infection | NCT04352400, NCT04418128 | – |
| Tissue-type plasminogen activator | Conversion of plasminogen into plasmin, leading to breakdown of cross-linked fibrin |
Benefit in a small study of patients with severe COVID-19 A phase IIa trial in patients with COVID-19-related ARDS is ongoing |
NCT04357730 | 119 |
| Dipyridamole |
Phosphodiesterase inhibitor reversibly inhibiting platelet aggregation; in addition, it potentiates vascular-protective effects of endothelium-derived nitric oxide Possible activity against positive-stranded RNA viruses and prevention of NET formation |
In vitro suppression of SARS-CoV-2 replication and improvement of lung pathology in a model of viral pneumonia In 14 patients, reported improvement in clinical status compared with controls A trial is ongoing |
NCT04391179 | 121,124,125 |
| Ticagrelor | P2Y12-receptor antagonist and attenuation of NET formation | Ongoing trials | NCT02735707, NCT04518735 | – |
| Anti-inflammatory drugs | ||||
| NE inhibitors | NE inhibition blocks NET formation and reduces SARS-CoV-2 spike protein proteolytic activation |
Sivelestat has been approved to treat ARDS in Japan and South Korea, but findings are inconsistent No current indication is available for SARS-CoV-2-related ARDS |
– | 131–133 |
| DNase I | Dissolution of NETs |
Dornase alpha has been tested in two case studies in patients with COVID-19-associated ARDS Several trials are ongoing |
NCT04402944, NCT04355364, NCT04432987, NCT04359654, NCT04445285, NCT04402970 | 138,139 |
| Ruxolitinib | JAK1/2 inhibitor |
In a small pilot study, clinical improvement was observed after 1 week of treatment In a small RCT, ruxolitinib plus SOC did not significantly accelerate clinical improvement in patients with severe COVID-19 A trial is ongoing in Germany |
NCT04338958 | 142,155,156 |
| Eculizumab and ravulizumab | C5 inhibitors blocking MAC formation |
Eculizumab showed good efficacy in reducing inflammatory biomarkers In ICU patients, eculizumab improved 15-day survival and hypoxia compared with SOC Trials with eculizumab and ravulizumab are ongoing |
NCT04288713, NCT04369469, NCT04390464 | 147,148 |
| AMY-101 | Inhibition of C3 cleavage by direct binding |
Limited experience is now available, with encouraging results Three phase II clinical trials in patients with COVID-19-associated ARDS are ongoing |
EudraCT number 2020-001550-22, EudraCT number 2020-004408-32, NCT04395456 | 149 |
ARDS, acute respiratory distress syndrome; COVID-19, coronavirus disease 2019; ICU, intensive care unit, JAK, Janus kinase; MAC, membrane attack complex; MERS-CoV, Middle East respiratory syndrome coronavirus; NE, neutrophil elastase; NET, neutrophil extracellular trap; RCT, randomized controlled trial; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SOC, standard of care.
Antithrombotic therapies
As the coagulation cascade is dysregulated in COVID-19, anticoagulation approaches have been explored for the treatment, particularly of patients with incident venous thromboembolism (VTE) or acute coronary syndrome due to plaque rupture103. Indeed, a study reported that 40% of patients hospitalized with COVID-19 are at high risk of VTE104 and data from a large retrospective cohort of patients in the United States suggested that anticoagulation may reduce mortality, especially among those with severe disease requiring invasive mechanical ventilation105. Pharmacological VTE prophylaxis, including daily low molecular weight heparin or twice-daily subcutaneous unfractionated heparin, may also be of benefit to patients hospitalized with COVID-19 who are bedridden or need intensive care, or patients discharged from hospital but with relevant risk of VTE — that is, individuals with reduced mobility, pro-thrombotic comorbidities (active cancer or obesity), older age, a history of VTE and persistently elevated levels of D-dimer103,106,107.
Studies of heparin treatment of COVID-19 have shown positive results103,106 (Supplementary Table 1), and this is now one of a growing number of agents available to manage COVID-19 either as a prophylactic or therapeutic regimen108 (Table 1). The use of fondaparinux (a selective indirect antithrombin-dependent factor Xa inhibitor) in patients with COVID-19 was reported in two papers, with contrasting results about its safety109,110. The same applies to direct oral anticoagulants, the use of which in patients with COVID-19 has been little studied to date111,112. Several trials of heparin and other anticoagulant agents are in progress: the Randomized, Embedded, Multi-factorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP) (NCT02735707); the Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 (ACTIV-4) trial (NCT04505774); and the Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC) trial (NCT04372589). These trials are testing whether the use of full-dose versus low-dose unfractionated heparin or low molecular weight heparin benefits patients with COVID-19 requiring ICU admission. However, enrolment of critically ill patients has been temporarily stopped owing to futility and safety concerns for this subgroup of patients. Response to this anticoagulant therapy may depend on the time of administration; if given too late, thrombi in the microcirculation and large vessels may already be too extensive.
An alternative approach to pharmacologically disrupt the coagulation cascade involves blockade of factor XII (FXII), which is responsible for activation of the contact pathway (Table 1). FXII blockade has been shown to protect from occlusive thrombosis in animal models without impairing haemostasis113,114. Thus, a FXII-blocking antibody (garadacimab) is currently being explored in a multicentre, double-blind, placebo-controlled phase II trial in patients with respiratory distress and COVID-19 (NCT04409509). Similarly, a serine protease inhibitor of thrombin, plasmin and trypsin known as nafamostat mesylate (used in Japan for the treatment of pancreatitis and DIC and the prevention of clots during dialysis115) is being investigated in clinical trials for COVID-19 (NCT04352400, NCT04418128). This drug showed potential to block Middle East respiratory syndrome coronavirus infection in vitro116 (Table 1).
The hypofibrinolytic state observed in ARDS has been targeted by the use of tissue-type plasminogen activator, which is responsible for the conversion of plasminogen into plasmin, leading to the breakdown of cross-linked fibrin117,118. Indeed, tissue-type plasminogen activator infusion showed benefit in three patients with severe COVID-19 (ref.119), and a phase IIa trial in patients with COVID-19-related ARDS is currently ongoing (NCT04357730).
The antiplatelet agent dipyridamole may have therapeutic potential120 (Table 1). This agent, apart from its antiplatelet function, was shown to provide broad-spectrum antiviral activity (especially against positive-stranded RNA viruses), suppress inflammation and favour mucosal healing, and prevent acute injury and fibrosis in the lungs, heart and kidney121–123. Dipyridamole treatment in patients with COVID-19 may also have the added benefit of preventing NETosis by promoting 3′,5′-cyclic adenosine monophosphate (cAMP) generation in neutrophils, as was shown in the context of antiphospholipid syndrome124. Liu et al. demonstrated that dipyridamole can suppress SARS-CoV-2 replication in vitro and improve lung pathology in an animal model of viral pneumonia through a type I interferon response125. This drug was tested in 14 patients and led to an improvement in clinical status compared with controls125. A trial of dipyridamole is currently ongoing (NCT04391179). Another antiplatelet agent, ticagrelor, showed the ability to attenuate NET formation126. Accordingly, two trials of ticagrelor are ongoing or recently completed (NCT02735707, NCT04518735).
Anti-inflammatory therapies
Immunomodulatory therapies, such as inhibitors of IL-6, IL-1, GM-CSF and Janus kinases (JAKs), aim to blunt the cytokine dysregulation associated with severe COVID-19 (refs15,127,128) (Table 1), but little is known about their impact on the thrombotic complications of the disease.
Given that NETs have a direct role in the immunothrombotic process in COVID-19, blocking NETs may help to improve prognosis (Table 1). Some drugs targeting NETs already exist or are under development, such as inhibitors of neutrophil elastase (NE), PAD4 and gasdermin D129. For example, NE inhibitors can block NET formation, limit the toxic activities of NE itself on lung connective tissue and reduce spike protein proteolytic activation that is responsible for SARS-CoV-2 binding to host cells130. Sivelestat, an NE inhibitor, has been approved to treat ARDS in Japan and South Korea, but findings are inconsistent as the severity of lung injury is likely to represent the most important predictor for patient outcome131–133. However, no evidence is currently available in favour of using NE inhibitors for COVID-19-induced ARDS.
NETs can be degraded by recombinant DNase I (dornase alpha), which is currently given by inhalation to patients with cystic fibrosis to target NETs in the airways134. Dornase alpha may help to dissolve respiratory secretions in patients with COVID-19 (ref.135), reducing the risk for secondary infections and improving ventilation, and may also reduce the risk of progression towards ARDS, as shown in animal models136,137. Two case studies have shown that administration of dornase alpha is well tolerated in patients with COVID-19-associated ARDS138,139, and several trials are underway to determine the efficacy of this approach (NCT04402944, NCT04355364, NCT04432987, NCT04359654, NCT04445285, NCT04402970). Nebulizer administration of DNase provides direct access to NETs within the alveolar space, but there may be a barrier to reaching systemic efficacy owing to the high reported levels of platelet factor 4 (PF4) in severe COVID-19 (ref.80). PF4 binding to NETs leads to their compaction and decreased susceptibility to DNase degradation140. Therefore, DNase administration is unlikely to ameliorate NET-mediated thrombosis, although the combination with heparin (which also digests NETs141) may be able to overcome this DNase resistance.
Other promising approaches to prevent NET formation rather than target already released NETs include JAK1/2 inhibition with ruxolitinib142, dipyridamole124, ticagrelor126 and neonatal NET-inhibitory factor, an endogenous peptide produced in newborns that restricts the ability of neutrophils to produce NETs143. Neonatal NET-inhibitory factor was shown to prevent COVID-19 plasma-induced NET formation by healthy donor neutrophils in vitro, but the mechanism of action remains to be elucidated80.
Finally, evidence is accumulating on the role of complement activation in the pathogenesis and severity of SARS-CoV-2 (ref.144) as well as on complement-mediated thrombotic microangiopathy in patients with COVID-19 (ref.145). Thus, therapies for thrombotic microangiopathy — complement inhibitors — may be used in this setting. C3 blockade can inhibit the production of both C3a and C5a, but also of intrapulmonary C3a and the release of IL-6 from alveolar macrophages146. Currently, two FDA-approved complement inhibitors are available, eculizumab and ravulizumab, both of which bind to C5 and sterically block the cleavage of C5 to C5a, and thus membrane attack complex formation. Four patients with COVID-19 receiving eculizumab intravenously showed a prompt reduction in C-reactive protein levels and an improvement of the lesions observed through chest computed tomography scan147. Among 35 patients admitted to the ICU with COVID-19, eculizumab treatment improved 15-day survival and hypoxia compared with patients treated with standard care alone148. Trials with eculizumab (NCT04288713) and ravulizumab (NCT04369469, NCT04390464) are currently ongoing. In a report from Italy, a patient with severe COVID-19-related ARDS was safely and successfully treated with the compstatin-based complement C3 inhibitor AMY-101 (ref.149). A recent study comparing two different strategies targeting C3 and C5 has shown a general beneficial impact in patients with COVID-19, although C3 inhibition led to a broader therapeutic effect blocking cytokine dysregulation and NET generation, thereby having a positive impact on immunothrombosis-driven disease pathways150. The C3 inhibitor AMY-101 is currently being evaluated in three phase II clinical trials in patients with COVID-19-associated ARDS (EudraCT number 2020-001550-22, EudraCT number 2020-004408-32, NCT04395456). Another C3 inhibitor, the pegylated compound APL-9, is being tested in a phase I/II randomized controlled trial for severe COVID-19 (NCT04402060). The C1 esterase inhibitor ruconest (NCT04414631, NCT04530136) and the C5a inhibitor IFX-1 (NCT04333420) are being tested as well.
Conclusions
Progressive advancements in our understanding of the pathophysiology of COVID-19 have been crucial for better management of COVID-19. Severe COVID-19 is not limited to the respiratory tract but is a multisystem syndrome in which the vascular endothelium is the most damaged organ, characterized by a state of immunothrombosis within microvessels (MicroCLOTS) and a predisposition to macrothrombosis. McGonagle et al. recently pointed out the potential role of thrombosis in pulmonary veins distal to the alveolar capillary bed, which should act as a clot filter, suggesting this could be a SARS-CoV-2-related vasculitis responsible for ischaemic manifestations in different organs151. Based on all of these features, anticoagulant therapy and immunomodulatory agents are likely necessary to blunt the hyperinflammatory and prothrombotic conditions. Evidence from clinical trials is still limited and consensus-based guidelines recommend anticoagulation therapy based on an individual risk profile. With regard to immunomodulatory therapies, evidence is accumulating about a beneficial role in COVID-19. Timing of administration, however, is a challenging point that needs to be carefully considered, and data about a consistent effect on immunothrombosis are still lacking.
Supplementary information
Acknowledgements
F.M. is supported by a grant from the Italian Ministry of Health to the Italian Cardiovascular Network (#2754291).
Glossary
- Antithrombin
A glycoprotein produced by the liver that inactivates different enzymes of the coagulation cascade. Antithrombin activity is strongly increased by the anticoagulant medication heparin, which enhances the binding of antithrombin to factor IIa (thrombin) and factor Xa.
- Cytokine storm
A sudden surge in circulating levels of pro-inflammatory cytokines, such as interleukin-1 (IL-1), IL-6, tumour necrosis factor (TNF) and interferon-γ (IFNγ). Clinically, this can result in hypotension, acute renal failure, impaired pulmonary function and even death.
- D-dimer
A small protein derived from fibrin degradation that is found in the blood once a blood clot is degraded. The name comes from the presence of two D fragments of the fibrin protein united by a cross-link.
- Disseminated intravascular coagulation
(DIC). An acquired syndrome characterized by the intravascular activation of coagulation without a precise localization in response to microvascular injury, leading to organ dysfunction when sufficiently severe. DIC involves large production of thrombin accompanied by platelet activation and consumption, altered fibrinolysis and microvascular thrombosis. It can occur in critically ill patients with overwhelming infection, fulminant sepsis, extensive tissue damage or malignancy.
- Haemostasis
The combination of events that result in cessation of bleeding. Haemostatic processes include constriction of blood vessels, platelet aggregation and coagulation (clotting) of the blood.
- Hyaline thrombi
Clots occurring in small vessels due to the formation of hyaline membranes and surfactant dysfunction after an inflammatory injury. These formations are the pathological equivalent of acute respiratory distress syndrome (ARDS) occurring in patients with severe-to-critical coronavirus disease 2019 (COVID-19).
- Lung compliance
A measure of the ability of the lungs to stretch and expand. A low compliance refers to that of a stiff lung, as occurs in fibrosis. A high compliance means a flexible lung, as seen in emphysema.
- Macrophage activation syndrome
A syndrome in which a dysregulated activation and proliferation of macrophages and T cells leads to increased release of pro-inflammatory cytokines.
- Microthrombosis
The formation of thrombi (clots) within small vessels, which is typical of the immunothrombotic process. Microthrombosis is often encountered in patients with coronavirus disease 2019 (COVID-19).
- NLRP3 inflammasome
Macromolecular structure that is responsible for sensing danger and triggering a local or systemic inflammatory response. Following NLRP3 inflammasome activation, large quantities of pro-inflammatory cytokines (in particular IL‑1β) are released for extracellular secretion. These cytokines are important in the inflammatory response and responsible for symptoms such as fever.
- Neutrophil extracellular trap
(NET). Fibrillary structure consisting of DNA complexed with histones (H3 and H4) and proteins from neutrophil granules, especially neutrophil elastase (NE), myeloperoxidase (MPO) and cathepsin G. NETs act as a mesh that traps microorganisms and exposes them to neutrophil-derived effector molecules. NETs also provide a scaffold for thrombus formation and activation of coagulation.
- Positive end-expiratory pressure
Pressure within the lung alveoli above atmospheric pressure that is recorded at the end of expiration. Besides intrinsic positive end-expiratory pressure (caused by an incomplete exhalation), extrinsic positive end-expiratory pressure is provided by a ventilator during mechanical ventilation and is meant to reduce end-expiratory alveolar collapse, thus improving hypoxaemia or reducing ventilator-associated lung injury in patients with acute respiratory distress syndrome (ARDS).
- Thrombosis
The formation of a thrombus (clot) inside blood vessels, resulting in partial or complete vessel occlusion.
- Thrombotic microangiopathy
Pathology characterized by formation of thrombi in capillaries owing to endothelial damage. In particular, decreased levels of the protease a disintegrin and metalloproteinase with a thrombospondin type 1 motif, member 13 (ADAMTS13) lead to an accumulation of ultra-large von Willebrand factor (VWF) multimers, which promote platelet–vessel wall interactions, causing thrombus formation. The clinical presentation comprises multiple organ dysfunctions, especially in the brain and kidneys.
- Ventilation–perfusion mismatch
Impairment of the ventilation to perfusion ratio, meaning that a part of the lung is adequately oxygenated but not perfused, or vice versa, caused by diseases such as pneumonia and pulmonary embolism.
- Von Willebrand factor
(VWF). The main adhesive protein mediating interactions between platelets and the vessel wall, leading to platelet aggregation. Preformed multimers are released from Weibel–Palade bodies of activated endothelial cells.
Author contributions
A.B., A.V., K.M., S.M., M.L. and A.A. contributed to all aspects of the article. L.D., D.L.D., B.W.V.T., F.D. and F.M. contributed to discussion of the content and reviewed and/or edited the manuscript before submission. All authors approved the final version of the manuscript.
Competing interests
A.B. and A.V. received a travel grant from Kiniksa Pharmaceuticals Ltd and honoraria from Effetti s.r.l. (Milan, Italy). L.D. has received consultation honoraria from Abbvie, Amgen, Biogen, Bristol-Myers Squibb, Celltrion, GlaxoSmithKline, Novartis, Pfizer, Roche, Sanofi-Genzyme and SOBI. K.M. is an inventor on patent US9642822 and patent applications WO20180271953A1 and US2019167680A1, and is a consultant for PEEL Therapeutics, Inc. B.W.V.T. has served as a consultant for Novartis and Serpin Pharma, and has received research support from Novartis, Kiniksa Pharmaceuticals Ltd, Serpin Pharma and SOBI. A.A. has served as a consultant for Applied Clinical Intel, AstraZeneca, Cromos Pharma, Janssen, Kiniksa Pharmaceuticals Ltd, Merck, Olatec and Serpin Pharma, and has received research support from Janssen, Olatec and Serpin Pharma. All other authors declare no competing interests.
Footnotes
Peer review information
Nature Reviews Immunology thanks the anonymous reviewers for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41577-021-00536-9.
References
- 1.Pascarella G, et al. COVID-19 diagnosis and management: a comprehensive review. J. Intern. Med. 2020;288:192–206. doi: 10.1111/joim.13091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonaventura A, et al. Targeting GM-CSF in COVID-19 pneumonia: rationale and strategies. Front. Immunol. 2020;11:1625. doi: 10.3389/fimmu.2020.01625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McFadyen JD, Stevens H, Peter K. The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ. Res. 2020;127:571–587. doi: 10.1161/CIRCRESAHA.120.317447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ranucci M, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J. Thromb. Haemost. 2020;18:1747–1751. doi: 10.1111/jth.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta A, et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020;26:1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fox SE, et al. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir. Med. 2020;8:681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wichmann D, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann. Intern. Med. 2020;173:268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carsana L, et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect. Dis. 2020;20:1135–1140. doi: 10.1016/S1473-3099(20)30434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schurink B, et al. Viral presence and immunopathology in patients with lethal COVID-19: a prospective autopsy cohort study. Lancet Microbe. 2020;1:e290–e299. doi: 10.1016/S2666-5247(20)30144-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat. Rev. Immunol. 2013;13:34–45. doi: 10.1038/nri3345. [DOI] [PubMed] [Google Scholar]
- 11.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;324:782–793. doi: 10.1001/jama.2020.12839. [DOI] [PubMed] [Google Scholar]
- 12.Berlin DA, Gulick RM, Martinez FJ. Severe COVID-19. N. Engl. J. Med. 2020;383:2451–2460. doi: 10.1056/NEJMcp2009575. [DOI] [PubMed] [Google Scholar]
- 13.Lavezzo E, et al. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo′. Nature. 2020;584:425–429. doi: 10.1038/s41586-020-2488-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J. Heart Lung Transpl. 2020;39:405–407. doi: 10.1016/j.healun.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buckley LF, et al. Role for anti-cytokine therapies in severe coronavirus disease 2019. Crit. Care Explor. 2020;2:e0178. doi: 10.1097/CCE.0000000000000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vecchie A, et al. IL-18 and infections: is there a role for targeted therapies? J. Cell Physiol. 2021;236:1638–1657. doi: 10.1002/jcp.30008. [DOI] [PubMed] [Google Scholar]
- 18.Fajgenbaum DC, June CH. Cytokine storm. N. Engl. J. Med. 2020;383:2255–2273. doi: 10.1056/NEJMra2026131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehta P, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kox M, Waalders NJB, Kooistra EJ, Gerretsen J, Pickkers P. Cytokine levels in critically ill patients with COVID-19 and other conditions. JAMA. 2020;324:1565–1567. doi: 10.1001/jama.2020.17052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leisman DE, et al. Cytokine elevation in severe and critical COVID-19: a rapid systematic review, meta-analysis, and comparison with other inflammatory syndromes. Lancet Respir. Med. 2020;8:1233–1244. doi: 10.1016/S2213-2600(20)30404-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blanco-Melo D, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181:1036–1045.e9. doi: 10.1016/j.cell.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toldo S, et al. Inflammasome formation in the lungs of patients with fatal COVID-19. Inflamm. Res. 2021;70:7–10. doi: 10.1007/s00011-020-01413-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodrigues TS, et al. Inflammasomes are activated in response to SARS-CoV-2 infection and are associated with COVID-19 severity in patients. J. Exp. Med. 2021;218:e20201707. doi: 10.1084/jem.20201707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Quartuccio L, et al. Profiling COVID-19 pneumonia progressing into the cytokine storm syndrome: results from a single Italian centre study on tocilizumab versus standard of care. J. Clin. Virol. 2020;129:104444. doi: 10.1016/j.jcv.2020.104444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin. Chem. Lab. Med. 2020;58:1021–1028. doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 27.McGonagle D, O'Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020;2:e437–e445. doi: 10.1016/S2665-9913(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang C, et al. Alveolar macrophage dysfunction and cytokine storm in the pathogenesis of two severe COVID-19 patients. EBioMedicine. 2020;57:102833. doi: 10.1016/j.ebiom.2020.102833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adachi T, et al. Clinicopathologic and immunohistochemical findings from autopsy of patient with COVID-19, Japan. Emerg. Infect. Dis. 2020;26:2157–2161. doi: 10.3201/eid2609.201353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liao M, et al. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat. Med. 2020;26:842–844. doi: 10.1038/s41591-020-0901-9. [DOI] [PubMed] [Google Scholar]
- 31.Alon R, et al. Leukocyte trafficking to the lungs and beyond: lessons from influenza for COVID-19. Nat. Rev. Immunol. 2021;21:49–64. doi: 10.1038/s41577-020-00470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tay MZ, Poh CM, Renia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat. Rev. Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Panigada M, et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J. Thromb. Haemost. 2020;18:1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goshua G, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575–e582. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iba T, Levy JH, Levi M, Connors JM, Thachil J. Coagulopathy of coronavirus disease 2019. Crit. Care Med. 2020;48:1358–1364. doi: 10.1097/CCM.0000000000004458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lodigiani C, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iba T, Connors JM, Levy JH. The coagulopathy, endotheliopathy, and vasculitis of COVID-19. Inflamm. Res. 2020;69:1181–1189. doi: 10.1007/s00011-020-01401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gazzaruso C, et al. Association between antithrombin and mortality in patients with COVID-19. A possible link with obesity. Nutr. Metab. Cardiovasc. Dis. 2020;30:1914–1919. doi: 10.1016/j.numecd.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mir N, D'Amico A, Dasher J, Tolwani A, Valentine V. Understanding the andromeda strain — the role of cytokine release, coagulopathy and antithrombin III in SARS-CoV2 critical illness. Blood Rev. 2021;45:100731. doi: 10.1016/j.blre.2020.100731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J. Hepatol. 2020;73:807–816. doi: 10.1016/j.jhep.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Portincasa P, Krawczyk M, Machill A, Lammert F, Di Ciaula A. Hepatic consequences of COVID-19 infection. Lapping or biting? Eur. J. Intern. Med. 2020;77:18–24. doi: 10.1016/j.ejim.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Whyte CS, Morrow GB, Mitchell JL, Chowdary P, Mutch NJ. Fibrinolytic abnormalities in acute respiratory distress syndrome (ARDS) and versatility of thrombolytic drugs to treat COVID-19. J. Thromb. Haemost. 2020;18:1548–1555. doi: 10.1111/jth.14872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gralinski LE, et al. Mechanisms of severe acute respiratory syndrome coronavirus-induced acute lung injury. mBio. 2013;4:e00271–13. doi: 10.1128/mBio.00271-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iba T, Warkentin TE, Thachil J, Levi M, Levy JH. Proposal of the definition for COVID-19-associated coagulopathy. J. Clin. Med. 2021;10:191. doi: 10.3390/jcm10020191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tian S, et al. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J. Thorac. Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Varga Z, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schaller T, et al. Postmortem examination of patients with COVID-19. JAMA. 2020;323:2518–2520. doi: 10.1001/jama.2020.8907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nicholls JM, et al. Lung pathology of fatal severe acute respiratory syndrome. Lancet. 2003;361:1773–1778. doi: 10.1016/S0140-6736(03)13413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McGonagle D, Sharif K, O'Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun. Rev. 2020;19:102537. doi: 10.1016/j.autrev.2020.102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen L, Hao G. The role of angiotensin-converting enzyme 2 in coronaviruses/influenza viruses and cardiovascular disease. Cardiovasc. Res. 2020;116:1932–1936. doi: 10.1093/cvr/cvaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Magro C, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang H, et al. Histopathologic changes and SARS-CoV-2 immunostaining in the lung of a patient with COVID-19. Ann. Intern. Med. 2020;172:629–632. doi: 10.7326/M20-0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xu Z, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat. Rev. Immunol. 2020;20:389–391. doi: 10.1038/s41577-020-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goeijenbier M, et al. Review: Viral infections and mechanisms of thrombosis and bleeding. J. Med. Virol. 2012;84:1680–1696. doi: 10.1002/jmv.23354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guo Y, Korteweg C, McNutt MA, Gu J. Pathogenetic mechanisms of severe acute respiratory syndrome. Virus Res. 2008;133:4–12. doi: 10.1016/j.virusres.2007.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ding Y, et al. The clinical pathology of severe acute respiratory syndrome (SARS): a report from China. J. Pathol. 2003;200:282–289. doi: 10.1002/path.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hamming I, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004;203:631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Levi M, van der Poll T. Coagulation and sepsis. Thromb. Res. 2017;149:38–44. doi: 10.1016/j.thromres.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 61.Helms J, et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Escher R, Breakey N, Lammle B. Severe COVID-19 infection associated with endothelial activation. Thromb. Res. 2020;190:62. doi: 10.1016/j.thromres.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Martinelli N, et al. A relative ADAMTS13 deficiency supports the presence of a secondary microangiopathy in COVID 19. Thromb. Res. 2020;193:170–172. doi: 10.1016/j.thromres.2020.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Schwameis M, Schorgenhofer C, Assinger A, Steiner MM, Jilma B. VWF excess and ADAMTS13 deficiency: a unifying pathomechanism linking inflammation to thrombosis in DIC, malaria, and TTP. Thromb. Haemost. 2015;113:708–718. doi: 10.1160/TH14-09-0731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guervilly C, et al. Circulating endothelial cells as a marker of endothelial injury in severe COVID-19. J. Infect. Dis. 2020;222:1789–1793. doi: 10.1093/infdis/jiaa528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Falcinelli E, et al. Role of endothelial dysfunction in the thrombotic complications of COVID-19 patients. J. Infect. 2020 doi: 10.1016/j.jinf.2020.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA. 2020;323:2329–2330. doi: 10.1001/jama.2020.6825. [DOI] [PubMed] [Google Scholar]
- 68.Perico L, et al. Immunity, endothelial injury and complement-induced coagulopathy in COVID-19. Nat. Rev. Nephrol. 2021;17:46–64. doi: 10.1038/s41581-020-00357-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bonetti PO, Lerman LO, Lerman A. Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler. Thromb. Vasc. Biol. 2003;23:168–175. doi: 10.1161/01.atv.0000051384.43104.fc. [DOI] [PubMed] [Google Scholar]
- 70.Hottz ED, et al. Platelet activation and platelet–monocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020;136:1330–1341. doi: 10.1182/blood.2020007252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nicolai L, et al. Immunothrombotic dysregulation in COVID-19 pneumonia is associated with respiratory failure and coagulopathy. Circulation. 2020;142:1176–1189. doi: 10.1161/CIRCULATIONAHA.120.048488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Levi M. Platelets in critical illness. Semin. Thromb. Hemost. 2016;42:252–257. doi: 10.1055/s-0035-1570080. [DOI] [PubMed] [Google Scholar]
- 73.Zaid Y, et al. Platelets can associate with SARS-Cov-2 RNA and are hyperactivated in COVID-19. Circ. Res. 2020;127:1404–1418. doi: 10.1161/CIRCRESAHA.120.317703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chrysanthopoulou A, et al. Interferon λ1/IL-29 and inorganic polyphosphate are novel regulators of neutrophil-driven thromboinflammation. J. Pathol. 2017;243:111–122. doi: 10.1002/path.4935. [DOI] [PubMed] [Google Scholar]
- 75.Gu SX, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat. Rev. Cardiol. 2021;18:194–209. doi: 10.1038/s41569-020-00469-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not? Crit. Care. 2020;24:154. doi: 10.1186/s13054-020-02880-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gattinoni L, et al. COVID-19 does not lead to a ‘typical’ acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2020;201:1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gattinoni L, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46:1099–1102. doi: 10.1007/s00134-020-06033-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ciceri F, et al. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit. Care Resusc. 2020;22:95–97. doi: 10.51893/2020.2.pov2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Middleton EA, et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood. 2020;136:1169–1179. doi: 10.1182/blood.2020007008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mitsios A, Arampatzioglou A, Arelaki S, Mitroulis I, Ritis K. NETopathies? Unraveling the dark side of old diseases through neutrophils. Front. Immunol. 2016;7:678. doi: 10.3389/fimmu.2016.00678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rebetz J, Semple JW, Kapur R. The pathogenic involvement of neutrophils in acute respiratory distress syndrome and transfusion-related acute lung injury. Transfus. Med. Hemother. 2018;45:290–298. doi: 10.1159/000492950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bendib I, et al. Neutrophil extracellular traps are elevated in patients with pneumonia-related acute respiratory distress syndrome. Anesthesiology. 2019;130:581–591. doi: 10.1097/ALN.0000000000002619. [DOI] [PubMed] [Google Scholar]
- 84.Lv X, et al. Extracellular histones are clinically relevant mediators in the pathogenesis of acute respiratory distress syndrome. Respir. Res. 2017;18:165. doi: 10.1186/s12931-017-0651-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zuo Y, et al. Neutrophil extracellular traps in COVID-19. JCI Insight. 2020;5:e138999. doi: 10.1172/jci.insight.138999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Skendros P, et al. Complement and tissue factor-enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Invest. 2020;130:6151–6157. doi: 10.1172/JCI141374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Leppkes M, et al. Vascular occlusion by neutrophil extracellular traps in COVID-19. EBioMedicine. 2020;58:102925. doi: 10.1016/j.ebiom.2020.102925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Radermecker C, et al. Neutrophil extracellular traps infiltrate the lung airway, interstitial, and vascular compartments in severe COVID-19. J. Exp. Med. 2020;217:e20201012. doi: 10.1084/jem.20201012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Veras FP, et al. SARS-CoV-2-triggered neutrophil extracellular traps mediate COVID-19 pathology. J. Exp. Med. 2020;217:e20201129. doi: 10.1084/jem.20201129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.O'Flynn J, Dixon KO, Faber Krol MC, Daha MR, van Kooten C. Myeloperoxidase directs properdin-mediated complement activation. J. Innate Immun. 2014;6:417–425. doi: 10.1159/000356980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.de Bont CM, Boelens WC, Pruijn GJM. NETosis, complement, and coagulation: a triangular relationship. Cell Mol. Immunol. 2019;16:19–27. doi: 10.1038/s41423-018-0024-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yalavarthi S, et al. Release of neutrophil extracellular traps by neutrophils stimulated with antiphospholipid antibodies: a newly identified mechanism of thrombosis in the antiphospholipid syndrome. Arthritis Rheumatol. 2015;67:2990–3003. doi: 10.1002/art.39247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mendoza-Pinto C, Garcia-Carrasco M, Cervera R. Role of infectious diseases in the antiphospholipid syndrome (including its catastrophic variant) Curr. Rheumatol. Rep. 2018;20:62. doi: 10.1007/s11926-018-0773-x. [DOI] [PubMed] [Google Scholar]
- 94.Zuo Y, et al. Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Sci. Transl Med. 2020;12:eabd3876. doi: 10.1126/scitranslmed.abd3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin. Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chousterman BG, Swirski FK, Weber GF. Cytokine storm and sepsis disease pathogenesis. Semin. Immunopathol. 2017;39:517–528. doi: 10.1007/s00281-017-0639-8. [DOI] [PubMed] [Google Scholar]
- 97.Bosmuller H, et al. The evolution of pulmonary pathology in fatal COVID-19 disease: an autopsy study with clinical correlation. Virchows Arch. 2020;477:349–357. doi: 10.1007/s00428-020-02881-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wolfel R, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 99.Bradley BT, et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet. 2020;396:320–332. doi: 10.1016/S0140-6736(20)31305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Manne BK, et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020;136:1317–1329. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhang S, et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J. Hematol. Oncol. 2020;13:120. doi: 10.1186/s13045-020-00954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yan SF, Mackman N, Kisiel W, Stern DM, Pinsky DJ. Hypoxia/hypoxemia-induced activation of the procoagulant pathways and the pathogenesis of ischemia-associated thrombosis. Arterioscler. Thromb. Vasc. Biol. 1999;19:2029–2035. doi: 10.1161/01.atv.19.9.2029. [DOI] [PubMed] [Google Scholar]
- 103.Bikdeli B, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wang T, et al. Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol. 2020;7:e362–e363. doi: 10.1016/S2352-3026(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Paranjpe I, et al. Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J. Am. Coll. Cardiol. 2020;76:122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Barnes GD, et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J. Thromb. Thrombolysis. 2020;50:72–81. doi: 10.1007/s11239-020-02138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Levi M, Hunt BJ. Thrombosis and coagulopathy in COVID-19: an illustrated review. Res. Pract. Thromb. Haemost. 2020;4:744–751. doi: 10.1002/rth2.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Paar V, et al. Anti-coagulation for COVID-19 treatment: both anti-thrombotic and anti-inflammatory? J. Thromb. Thrombolysis. 2021;51:226–231. doi: 10.1007/s11239-020-02212-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Prandoni P, et al. The hazard of fondaparinux in non-critically ill patients with COVID-19: retrospective controlled study versus enoxaparin. Thromb. Res. 2020;196:395–397. doi: 10.1016/j.thromres.2020.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Russo V, et al. Fondaparinux use in patients with COVID-19: a preliminary multicenter real-world experience. J. Cardiovasc. Pharmacol. 2020;76:369–371. doi: 10.1097/FJC.0000000000000893. [DOI] [PubMed] [Google Scholar]
- 111.Rossi R, Coppi F, Talarico M, Boriani G. Protective role of chronic treatment with direct oral anticoagulants in elderly patients affected by interstitial pneumonia in COVID-19 era. Eur. J. Intern. Med. 2020;77:158–160. doi: 10.1016/j.ejim.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Flam B, Wintzell V, Ludvigsson JF, Martensson J, Pasternak B. Direct oral anticoagulant use and risk of severe COVID-19. J. Intern. Med. 2021;289:411–419. doi: 10.1111/joim.13205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Larsson M, et al. A factor XIIa inhibitory antibody provides thromboprotection in extracorporeal circulation without increasing bleeding risk. Sci. Transl Med. 2014;6:222ra217. doi: 10.1126/scitranslmed.3006804. [DOI] [PubMed] [Google Scholar]
- 114.Jansen PM, et al. Inhibition of factor XII in septic baboons attenuates the activation of complement and fibrinolytic systems and reduces the release of interleukin-6 and neutrophil elastase. Blood. 1996;87:2337–2344. [PubMed] [Google Scholar]
- 115.Asakura H, Ogawa H. Potential of heparin and nafamostat combination therapy for COVID-19. J. Thromb. Haemost. 2020;18:1521–1522. doi: 10.1111/jth.14858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yamamoto M, et al. Identification of nafamostat as a potent inhibitor of Middle East respiratory syndrome coronavirus S protein-mediated membrane fusion using the split-protein-based cell–cell fusion assay. Antimicrob. Agents Chemother. 2016;60:6532–6539. doi: 10.1128/AAC.01043-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bonaventura A, Montecucco F, Dallegri F. Update on the effects of treatment with recombinant tissue-type plasminogen activator (rt-PA) in acute ischemic stroke. Expert. Opin. Biol. Ther. 2016;16:1323–1340. doi: 10.1080/14712598.2016.1227779. [DOI] [PubMed] [Google Scholar]
- 118.Liu C, et al. Meta-analysis of preclinical studies of fibrinolytic therapy for acute lung injury. Front. Immunol. 2018;9:1898. doi: 10.3389/fimmu.2018.01898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang J, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J. Thromb. Haemost. 2020;18:1752–1755. doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kanthi Y, Knight JS, Zuo Y, Pinsky DJ. New (re)purpose for an old drug: purinergic modulation may extinguish the COVID-19 thromboinflammatory firestorm. JCI Insight. 2020;5:e140971. doi: 10.1172/jci.insight.140971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fata-Hartley CL, Palmenberg AC. Dipyridamole reversibly inhibits mengovirus RNA replication. J. Virol. 2005;79:11062–11070. doi: 10.1128/JVI.79.17.11062-11070.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Huang B, et al. Mucosal profiling of pediatric-onset colitis and IBD reveals common pathogenics and therapeutic pathways. Cell. 2019;179:1160–1176.e24. doi: 10.1016/j.cell.2019.10.027. [DOI] [PubMed] [Google Scholar]
- 123.Insel PA, et al. cAMP and Epac in the regulation of tissue fibrosis. Br. J. Pharmacol. 2012;166:447–456. doi: 10.1111/j.1476-5381.2012.01847.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ali RA, et al. Adenosine receptor agonism protects against NETosis and thrombosis in antiphospholipid syndrome. Nat. Commun. 2019;10:1916. doi: 10.1038/s41467-019-09801-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Liu X, et al. Potential therapeutic effects of dipyridamole in the severely ill patients with COVID-19. Acta Pharm. Sin. B. 2020;10:1205–1215. doi: 10.1016/j.apsb.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mitsios A, et al. Ticagrelor exerts immune-modulatory effect by attenuating neutrophil extracellular traps. Int. J. Mol. Sci. 2020;21:3625. doi: 10.3390/ijms21103625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Stebbing J, et al. JAK inhibition reduces SARS-CoV-2 liver infectivity and modulates inflammatory responses to reduce morbidity and mortality. Sci. Adv. 2020;7:eabe4724. doi: 10.1126/sciadv.abe4724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Cavalli G, et al. Repurposing of biologic and targeted synthetic anti-rheumatic drugs in COVID-19 and hyper-inflammation: a comprehensive review of available and emerging evidence at the peak of the pandemic. Front. Pharmacol. 2020;11:598308. doi: 10.3389/fphar.2020.598308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Barnes BJ, et al. Targeting potential drivers of COVID-19: neutrophil extracellular traps. J. Exp. Med. 2020;217:e20200652. doi: 10.1084/jem.20200652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Mohamed MMA, El-Shimy IA, Hadi MA. Neutrophil elastase inhibitors: a potential prophylactic treatment option for SARS-CoV-2-induced respiratory complications? Crit. Care. 2020;24:311. doi: 10.1186/s13054-020-03023-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zeiher BG, et al. Neutrophil elastase inhibition in acute lung injury: results of the STRIVE study. Crit. Care Med. 2004;32:1695–1702. doi: 10.1097/01.ccm.0000133332.48386.85. [DOI] [PubMed] [Google Scholar]
- 132.Aikawa N, Kawasaki Y. Clinical utility of the neutrophil elastase inhibitor sivelestat for the treatment of acute respiratory distress syndrome. Ther. Clin. Risk Manag. 2014;10:621–629. doi: 10.2147/TCRM.S65066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tagami T, et al. Effect of a selective neutrophil elastase inhibitor on mortality and ventilator-free days in patients with increased extravascular lung water: a post hoc analysis of the PiCCO Pulmonary Edema Study. J. Intensive Care. 2014;2:67. doi: 10.1186/s40560-014-0067-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Papayannopoulos V, Staab D, Zychlinsky A. Neutrophil elastase enhances sputum solubilization in cystic fibrosis patients receiving DNase therapy. PLoS ONE. 2011;6:e28526. doi: 10.1371/journal.pone.0028526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zou Y, et al. Neutrophil extracellular traps promote lipopolysaccharide-induced airway inflammation and mucus hypersecretion in mice. Oncotarget. 2018;9:13276–13286. doi: 10.18632/oncotarget.24022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lefrancais E, Mallavia B, Zhuo H, Calfee CS, Looney MR. Maladaptive role of neutrophil extracellular traps in pathogen-induced lung injury. JCI Insight. 2018;3:e98178. doi: 10.1172/jci.insight.98178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Thomas GM, et al. Extracellular DNA traps are associated with the pathogenesis of TRALI in humans and mice. Blood. 2012;119:6335–6343. doi: 10.1182/blood-2012-01-405183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Okur HK, et al. Preliminary report of in vitro and in vivo effectiveness of dornase alfa on SARS-CoV-2 infection. N. Microbes N. Infect. 2020;37:100756. doi: 10.1016/j.nmni.2020.100756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Weber AG, Chau AS, Egeblad M, Barnes BJ, Janowitz T. Nebulized in-line endotracheal dornase alfa and albuterol administered to mechanically ventilated COVID-19 patients: a case series. Mol. Med. 2020;26:91. doi: 10.1186/s10020-020-00215-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gollomp K, et al. Neutrophil accumulation and NET release contribute to thrombosis in HIT. JCI Insight. 2018;3:e99445. doi: 10.1172/jci.insight.99445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Fuchs TA, et al. Extracellular DNA traps promote thrombosis. Proc. Natl Acad. Sci. USA. 2010;107:15880–15885. doi: 10.1073/pnas.1005743107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wolach O, et al. Increased neutrophil extracellular trap formation promotes thrombosis in myeloproliferative neoplasms. Sci. Transl Med. 2018;10:eaan8292. doi: 10.1126/scitranslmed.aan8292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yost CC, et al. Neonatal NET-inhibitory factor and related peptides inhibit neutrophil extracellular trap formation. J. Clin. Invest. 2016;126:3783–3798. doi: 10.1172/JCI83873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Java A, et al. The complement system in COVID-19: friend and foe? JCI Insight. 2020;5:e140711. doi: 10.1172/jci.insight.140711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Zhang Y, et al. Coagulopathy and antiphospholipid antibodies in patients with COVID-19. N. Engl. J. Med. 2020;382:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Risitano AM, et al. Complement as a target in COVID-19? Nat. Rev. Immunol. 2020;20:343–344. doi: 10.1038/s41577-020-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Diurno F, et al. Eculizumab treatment in patients with COVID-19: preliminary results from real life ASL Napoli 2 Nord experience. Eur. Rev. Med. Pharmacol. Sci. 2020;24:4040–4047. doi: 10.26355/eurrev_202004_20875. [DOI] [PubMed] [Google Scholar]
- 148.Annane D, et al. Eculizumab as an emergency treatment for adult patients with severe COVID-19 in the intensive care unit: a proof-of-concept study. EClinicalMedicine. 2020;28:100590. doi: 10.1016/j.eclinm.2020.100590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Mastaglio S, et al. The first case of COVID-19 treated with the complement C3 inhibitor AMY-101. Clin. Immunol. 2020;215:108450. doi: 10.1016/j.clim.2020.108450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mastellos DC, et al. Complement C3 vs C5 inhibition in severe COVID-19: early clinical findings reveal differential biological efficacy. Clin. Immunol. 2020;220:108598. doi: 10.1016/j.clim.2020.108598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.McGonagle D, Bridgewood C, Ramanan AV, Meaney JFM, Watad A. COVID-19 vasculitis and novel vasculitis mimics. Lancet Rheumatol. 2021;3:e224–e233. doi: 10.1016/S2665-9913(20)30420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Tang N, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ayerbe L, Risco C, Ayis S. The association between treatment with heparin and survival in patients with COVID-19. J. Thromb. Thrombolysis. 2020;50:298–301. doi: 10.1007/s11239-020-02162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Nadkarni GN, et al. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J. Am. Coll. Cardiol. 2020;76:1815–1826. doi: 10.1016/j.jacc.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.La Rosee F, et al. The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19 with severe systemic hyperinflammation. Leukemia. 2020;34:1805–1815. doi: 10.1038/s41375-020-0891-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cao Y, et al. Ruxolitinib in treatment of severe coronavirus disease 2019 (COVID-19): a multicenter, single-blind, randomized controlled trial. J. Allergy Clin. Immunol. 2020;146:137–146.e3. doi: 10.1016/j.jaci.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Hickey MJ, Kubes P. Intravascular immunity: the host–pathogen encounter in blood vessels. Nat. Rev. Immunol. 2009;9:364–375. doi: 10.1038/nri2532. [DOI] [PubMed] [Google Scholar]
- 158.Jackson SP, Darbousset R, Schoenwaelder SM. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133:906–918. doi: 10.1182/blood-2018-11-882993. [DOI] [PubMed] [Google Scholar]
- 159.Massberg S, et al. Reciprocal coupling of coagulation and innate immunity via neutrophil serine proteases. Nat. Med. 2010;16:887–896. doi: 10.1038/nm.2184. [DOI] [PubMed] [Google Scholar]
- 160.von Bruhl ML, et al. Monocytes, neutrophils, and platelets cooperate to initiate and propagate venous thrombosis in mice in vivo. J. Exp. Med. 2012;209:819–835. doi: 10.1084/jem.20112322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kambas K, et al. Autophagy mediates the delivery of thrombogenic tissue factor to neutrophil extracellular traps in human sepsis. PLoS ONE. 2012;7:e45427. doi: 10.1371/journal.pone.0045427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Bonaventura A, et al. The pathophysiological role of neutrophil extracellular traps in inflammatory diseases. Thromb. Haemost. 2018;118:6–27. doi: 10.1160/TH17-09-0630. [DOI] [PubMed] [Google Scholar]
- 163.Martinod K, Wagner DD. Thrombosis: tangled up in NETs. Blood. 2014;123:2768–2776. doi: 10.1182/blood-2013-10-463646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ammollo CT, Semeraro F, Xu J, Esmon NL, Esmon CT. Extracellular histones increase plasma thrombin generation by impairing thrombomodulin-dependent protein C activation. J. Thromb. Haemost. 2011;9:1795–1803. doi: 10.1111/j.1538-7836.2011.04422.x. [DOI] [PubMed] [Google Scholar]
- 165.Nicolai L, Gaertner F, Massberg S. Platelets in host defense: experimental and clinical insights. Trends Immunol. 2019;40:922–938. doi: 10.1016/j.it.2019.08.004. [DOI] [PubMed] [Google Scholar]
- 166.Ma AC, Kubes P. Platelets, neutrophils, and neutrophil extracellular traps (NETs) in sepsis. J. Thromb. Haemost. 2008;6:415–420. doi: 10.1111/j.1538-7836.2007.02865.x. [DOI] [PubMed] [Google Scholar]
- 167.Guo L, Rondina MT. The era of thromboinflammation: platelets are dynamic sensors and effector cells during infectious diseases. Front. Immunol. 2019;10:2204. doi: 10.3389/fimmu.2019.02204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Reinhardt C, et al. Protein disulfide isomerase acts as an injury response signal that enhances fibrin generation via tissue factor activation. J. Clin. Invest. 2008;118:1110–1122. doi: 10.1172/JCI32376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Semple JW, Aslam R, Kim M, Speck ER, Freedman J. Platelet-bound lipopolysaccharide enhances Fc receptor-mediated phagocytosis of IgG-opsonized platelets. Blood. 2007;109:4803–4805. doi: 10.1182/blood-2006-12-062695. [DOI] [PubMed] [Google Scholar]
- 170.Zhang G, et al. Lipopolysaccharide stimulates platelet secretion and potentiates platelet aggregation via TLR4/MyD88 and the cGMP-dependent protein kinase pathway. J. Immunol. 2009;182:7997–8004. doi: 10.4049/jimmunol.0802884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Bergmann S, Hammerschmidt S. Fibrinolysis and host response in bacterial infections. Thromb. Haemost. 2007;98:512–520. [PubMed] [Google Scholar]
- 172.Buchanan JT, et al. DNase expression allows the pathogen group A Streptococcus to escape killing in neutrophil extracellular traps. Curr. Biol. 2006;16:396–400. doi: 10.1016/j.cub.2005.12.039. [DOI] [PubMed] [Google Scholar]
- 173.Beiter K, et al. An endonuclease allows Streptococcus pneumoniae to escape from neutrophil extracellular traps. Curr. Biol. 2006;16:401–407. doi: 10.1016/j.cub.2006.01.056. [DOI] [PubMed] [Google Scholar]
- 174.Cheng AG, et al. Contribution of coagulases towards Staphylococcus aureus disease and protective immunity. PLoS Pathog. 2010;6:e1001036. doi: 10.1371/journal.ppat.1001036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Guggenberger C, Wolz C, Morrissey JA, Heesemann J. Two distinct coagulase-dependent barriers protect Staphylococcus aureus from neutrophils in a three dimensional in vitro infection model. PLoS Pathog. 2012;8:e1002434. doi: 10.1371/journal.ppat.1002434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Gavriilaki E, Brodsky RA. Complementopathies and precision medicine. J. Clin. Invest. 2020;130:2152–2163. doi: 10.1172/JCI136094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Gralinski LE, et al. Complement activation contributes to severe acute respiratory syndrome coronavirus pathogenesis. mBio. 2018;9:e01753-18. doi: 10.1128/mBio.01753-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Markiewski MM, Nilsson B, Ekdahl KN, Mollnes TE, Lambris JD. Complement and coagulation: strangers or partners in crime? Trends Immunol. 2007;28:184–192. doi: 10.1016/j.it.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 179.Ramlall V, et al. Immune complement and coagulation dysfunction in adverse outcomes of SARS-CoV-2 infection. Nat. Med. 2020;26:1609–1615. doi: 10.1038/s41591-020-1021-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Peerschke EI, Reid KB, Ghebrehiwet B. Platelet activation by C1q results in the induction of αIIb/β3 integrins (GPIIb-IIIa) and the expression of P-selectin and procoagulant activity. J. Exp. Med. 1993;178:579–587. doi: 10.1084/jem.178.2.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ikeda K, et al. C5a induces tissue factor activity on endothelial cells. Thromb. Haemost. 1997;77:394–398. [PubMed] [Google Scholar]
- 182.Ritis K, et al. A novel C5a receptor-tissue factor cross-talk in neutrophils links innate immunity to coagulation pathways. J. Immunol. 2006;177:4794–4802. doi: 10.4049/jimmunol.177.7.4794. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.