Abstract
Background and Objectives
Our aim was to create a “storyline” that provides empirical explanation of stakeholders’ perspectives underlying the use of patient- and family-reported outcome and experience measures to inform continuity across transitions in care for frail older adults and their family caregivers living at home.
Research Design and Methods
We conducted a meta-narrative synthesis to explore stakeholder perspectives pertaining to use of patient-reported outcome and experience measures (PROMs and PREMs) across micro (patients, family caregivers, and healthcare providers), meso (organizational managers/executives/programs), and macro (decision-/policy-makers) levels in healthcare. Systematic searches identified 9,942 citations of which 40 were included based on full-text screening.
Results
PROMs and PREMS (54 PROMs; 4 PREMs; 1 with PROM and PREM elements; 6 unspecified PROMs) were rarely used to inform continuity across transitions of care and were typically used independently, rarely together (n = 3). Two overarching traditions motivated stakeholders’ use. The first significant motivation by diverse stakeholders to use PROMs and PREMs was the desire to restore/support independence and care at home, predominantly at a micro-level. The second motivation to using PROMs and PREMs was to evaluate health services, including cost-effectiveness of programs and hospital discharge (planning); this focus was rarely at a macro-level and more often split between micro- and meso-levels of healthcare.
Discussion and Implications
The motivations underlying stakeholders’ use of these tools were distinct, yet synergistic between the goals of person/family-centered care and healthcare system-level goals aimed at efficient use of health services. There is a missed opportunity here for PROMs and PREMs to be used together to inform continuity across transitions of care.
Keywords: Continuity across transitions of Care, Family caregivers, Frailty, Frail older adults, Living at home, Quality of life
As society confronts unprecedented aging on a global scale (Bengtson, Lowenstein, Putney, & Gans, 2017), there is a pressing need to ensure continuity of care when frail older adults transition across sectors of care. Continuity across transitions of care is the experience of consistent, connected, coordinated care that includes meaningful relationships, management over time, place and providers, and information sharing (Cuthbertson, May 2014). Person/family-centered care necessitates that healthcare experiences and perceived outcomes be considered across all transitions of care. This can be facilitated through the use of patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs), which are increasingly and internationally promoted as an important basis for identifying, monitoring, and addressing the concerns and priorities that matters to patients and their family caregivers. PROMs are measurement instruments used to obtain appraisals from healthcare recipients (patients and family caregivers) about outcomes relevant to their quality of life (e.g., well-being, overall health, symptoms, functional status, and other aspects of psychological, social, and spiritual wellbeing) (Fayers & Machin, 2016). PREMs are measurement instruments used to obtain their appraisals from healthcare recipients about their satisfaction and experiences with the care provided (Kingsley & Patel, 2017). (See Table 1 for examples.) The objective of this study was to create a “storyline” that provides empirical explanation of different stakeholder perspectives underlying the selection, valuing, and use of PROMs and PREMs to inform continuity across transitions in care for frail older adults and their family caregivers living at home.
Table 1.
Examples of Quality of Life Assessment Instruments for Older Adults Living With Frailty and Their Family Caregivers
| Instrument | PROM/ PREM | Construct being measured | Target population | # of items and response scale(s) | Domains measured |
|---|---|---|---|---|---|
| McGill Quality of Life Questionnaire-Revised (MQOL-R) (Cohen, Mount, Strobel, & Bui, 1995; Cohen et al., 2017) | PROM | Quality of life over the past two days | People at all stages of a life-threatening illness (from diagnosis to cure or death) | 14 items (+ 1 global item) with a numerical response scale ranging from 0 to 10 | Physical, Psychological, Existential, and Social |
| Edmonton Symptom Assessment System-Revised (ESAS-r) (Watanabe et al., 2011) | PROM | Current symptoms | People with life-limiting illness | 11 items with a response scale ranging from 0 (no symptom) to 10 (worst possible) | 9 items measure individual symptoms, 1 measures wellbeing, and 1 measures a self-identified problem |
| PRISMA-7 (Raîche, Hébert, & Dubois, 2008) | PROM | Frailty | Older adults | 7 items with a response of either yes or no. Three or more “yes” answers indicates increased risk of frailty | 3 items related to activities of daily living, and 1 item measures support |
| Quality of Life in Life Threatening Illness-Family Carer (QOLLTI-F) (Cohen et al., 2006) | PROM | Quality of life over the past two days | Primary family caregiver of patients with life-threatening illness (but developed only with caregivers of cancer patients) | 16 items (+ 1 global item) with a numerical response scale ranging from 0 to 10 | Environment; Patient Condition; Caregiver’s Own State; Outlook; Quality of Care; Relationships; Financial Concerns |
| Canadian Health Care Evaluation Project Questionnaire (CANHELP-lite: patient version) (Heyland et al., 2010) | PREM | Satisfaction with end of life care during the past month | Patients with life-limiting illness | 20 items with a 5-point response scale ranging from 1 = not at all satisfied to 5 = completely satisfied | Relationship with Doctors, Illness Management, Communication, Decision-Making, Your Well-being, and Overall Satisfaction |
| Canadian Health Care Evaluation Project Questionnaire (CANHELP-lite: family caregiver version) (Heyland et al., 2010) | PREM | Satisfaction with end of life care during the past month | Family caregivers of patients with life-limiting illness | 21 items with a 5-point response scale ranging from 1 = not at all satisfied to 5 = completely satisfied | Relationship with Doctors, Characteristics of Doctors and Nurses, Illness Management, Communication and Decision-Making, Your Involvement, and Overall Satisfaction |
Traditionally, continuity of care has been idealized in the patient’s experience of a “continuous caring relationship” with an identified healthcare professional (Haggerty et al., 2003; Haggerty, Roberge, Freeman, & Beaulieu, 2013). For providers, the contrasting ideal is the delivery of “seamless service” through integration, coordination, and the sharing of information between different providers. As patients’ healthcare needs can rarely be met by a single healthcare professional, particularly frail older adults with multimorbidity, multidimensional models of continuity must be developed to accommodate the possibility of achieving both ideals simultaneously. Schang, Waibel, and Thomson (2013) concisely summarized these perspectives by differentiating that “care coordination concerns the health system or provider perspective. Continuity of care concerns the patient’s perspective” (p. 10).
Older adults and their families often prefer to receive care at home. However, when the older person’s health status changes, the individual may require care from multiple care providers across different care sectors, including community-based care, acute inpatient hospital care, and outpatient clinics. In our home country of Canada, older adults who are often in a state of frailty, increased vulnerability and risk, are likely to encounter changes between providers, institutions, and/or location of care (home vs. hospital, community or tertiary care) (Canadian Institutes of Health Research, 2019). Globally, healthcare systems are challenged to support the journey of frail older adults across the care continuum as they transition between multiple healthcare sectors.
Continuity and transitions is a key dimension of person/family-centered care (Picker Institute, 2019) and it is not surprising that the importance of this dimension increases with advancing age and frailty. Improving healthcare experiences and perceived outcomes of older adults and their family caregivers across multiple transitions of care is foundational to providing truly person/family-centered care. By person/family-centered care, we mean an approach to care that focuses on “getting to know the person,” including the patient and family caregivers, by considering their “history, values, beliefs, priorities, preferences, current situation future aspirations and how they make sense of what is happening to them” (Hewitt-Taylor, 2015). One emerging approach to integrate this concept into care is through the routine use of valid, person/family-centered measurement instruments across the sectors of care where most transitions for the older adult population occur (Cuthbertson, May 2014). The use of PROMs and PREMs to better understand and enhance person/family-centered care across transitions in care for frail older adults and their family caregivers has become mandated in several jurisdictions in Canada where our siloed healthcare systems have resulted in adverse and even sentinel events, as patients have “fallen through the cracks” (Bennett, 2019; Canadian Institute for Health Information, 2012).
Despite the availability of many PROMs and PREMs, their predominant use has been within sectors of care. Consequently, a knowledge gap exists regarding the selection and use of PROMs and PREMS to inform continuity across transitions of care for frail seniors who are living at home and for their families. A meta-narrative synthesis (MNS) was viewed as a novel means to understand different stakeholder perspectives (Gough, 2013) across micro (patients, family caregivers, and healthcare providers), meso (organizational managers/executives/programs), and macro (decision/policy-makers) levels in healthcare (Caldwell & Mays, 2012; Sutherland & Till, 1993). The research question guiding our meta-narrative review was: What are the motivations underlying stakeholders’ use of PROMs and PREMs in the context of continuity across transitions in care for frail older adults and their family caregivers living at home?
Methods
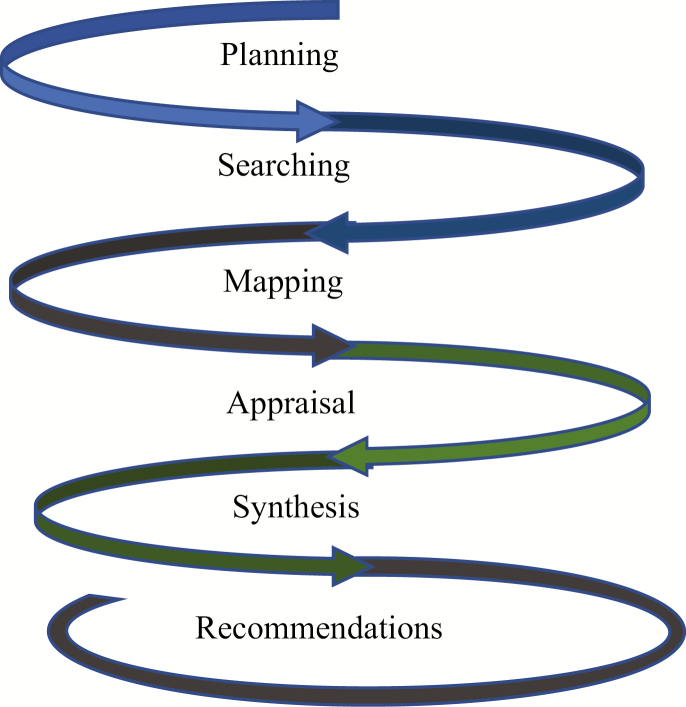
We used MNS to unravel the storylines of how and why PROMs and PREMs had been selected, valued, and used to inform continuity of healthcare for frail seniors and their family caregivers (family, friends, or informal caregivers) living at home. MNS was chosen as an established approach for synthesizing heterogeneous bodies of literature while providing knowledge users, policy-makers, and researchers with evidence that encompasses complex, and at times, competing priorities (Greenhalgh & Wong, 2013; Greenhalgh et al., 2005).. As shown in Figure 1, the MNS was undertaken within six overlapping phases, and MNS publications standards were followed (Greenhalgh, Long, & Flynn, 2005). The first five phases are presented in this paper under Methods section and the last under Implications section.
Figure 1.
Phases in meta-narrative synthesis.
Planning Phase
This project emerged from a prior collaboration between clinical and healthcare administration knowledge users (KUs) and researchers in Canada who conducted a knowledge synthesis of patient- and family-reported outcome and experience measures for older adults in acute care (Sawatzky et al., 2015). We worked in consultation throughout the six phases (Greenhalgh et al., 2005), thereby ensuring that the review was informed by and relevant to micro–meso–macro levels of healthcare. A series of weekly in-person/telephone meetings between the team leaders and research assistants provided oversight to the project. In addition, our methodology expert (Geoff Wong) provided training and consultation to enhance methodological rigor.
Searching Phase
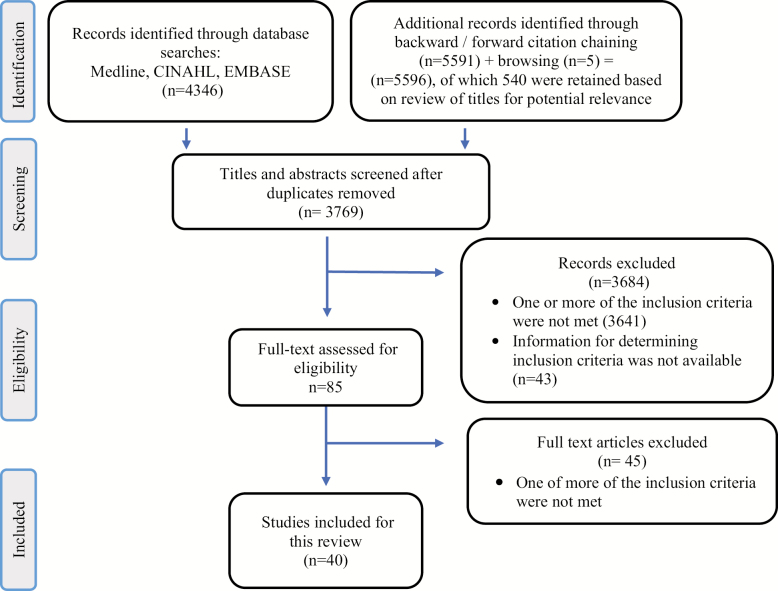
The searching phase was conducted between October 2016 and October 2018, and incorporated three strategies (see Figure 2).
Figure 2.
PRISMA flow diagram.
1. Browsing included the identification of seminal citations based on team members’ recommendations. This strategy yielded five articles.
2. An electronic database search was designed in consultation with a health science librarian. This strategy was not limited by date and employed two methods:
(a) a general database search of Medline, CINAHL, and EMBASE. The search included terms related to four concepts: PROM and PREM instruments, continuity of care, sectors of care, and older adult population (see Supplementary Table 1). This strategy yielded a total of 1,280 citations;
(b) specific searches of individual instruments whose focus was either generic or population specific. The instruments that were individually searched included those identified in our previous project (Sawatzky et al., 2015), as well as those recommended by the KUs.
In total, three rounds of specific searches were conducted and yielded 3,066 citations, for a total of 4,346 records.
3. Citations tracking included two steps:
(a) forward citation tracking;
(b) backward citations tracking.
If a paper was a protocol, we contacted study authors requesting follow-up publications. In total, 5,596 citations were identified via three rounds of citation tracking processes and screened for eligibility. Of the 5,596, 540 were retained based on review of titles for potential relevance.
Mapping Phase
Two research assistants screened titles and abstracts in EndNote X8 independently using two sets of inclusion criteria: (a) Generic criteria (older adult ≥65 years, living at home, application/use of PROM/PREM instruments); (b) Evidence-related criteria (use in at least one of the following: >1 sector of care, health administration use, use in clinical practice) (see Table 2). We excluded articles not written in English, but the primary reasons for exclusion were because the texts did not address our evidence-related criteria. Inconsistencies were resolved through consensus with other team members. Forty articles were included in the MNS review.
Table 2.
Inclusion Criteria
| I. Generic Criteria | II. Evidence-related Criteria |
|---|---|
| All of the following three Generic Criteria were met prior to screening for the three Evidence-related criteria | At least one of the following three Evidence-related Criteria had to be met prior to selecting a relevant citation |
| 1. Older Adult • The concept of older adult is defined as aged 65 years and older, or explicitly described in the abstract/title as “senior”, “older adult”, “elderly”, or “aged”, or the author(s)’ definition of aging/older adults/seniors, even if they use a different age criterion. 2. Living at Home • Explicit evidence showing the term of home or community setting of the older adults where they receive care. 3. Application or Use of PROM/PREM Instrument(s) • Explicit evidence indicating the actual use of the PROM/PREM instrument(s) ◦ PROM (Patient-Reported Outcome Measure) instruments refer to the self-report instruments used to obtain healthcare recipients’ appraisals of health outcomes relevant to their quality of life. ◦ PREM (Patient-Reported Experience Measure) instruments refer to the self-report instruments used to obtain patients’ appraisals of their experience and satisfaction with the quality of care and services. | 1. >1 Care Sector • Explicit evidence showing the applications of same PROM/PREM instrument(s) by same people in more than one of the following sectors: primary care, home care, acute care, and emergency services. 2. Health Administration Use • Explicit evidence showing the use of the PROM/PREM instrument(s) for healthcare administration or policymaking purposes. 3. Use in Clinical Practice • Explicit evidence showing the use of PROM/PREM instrument(s) at the point-of-care in clinical practice. |
The mapping phase entailed recording the key conceptual, theoretical, methodological, and instrumental underpinnings of the various stakeholder perspectives. We first identified the research traditions that historically unfolded over time (Wong et al., 2013). All papers were from the health disciplines. We identified eight traditions (see Table 3). References were grouped according to the tradition that each paper was grounded in: person/family-centered care (n = 7), health promotion (n = 3), comprehensive care for complex needs (n = 4), disability (n = 3), cost effectiveness of an intervention to stay at/return to home (n = 7), hospital discharge (planning) (n = 4), health service utilization (n = 10), and psychometric properties (n = 2). Mapping continued as we coded data to identify different theoretical approaches, controversies or contested findings, gaps, and underlying assumptions.
Table 3.
Characteristics of the 40 Studies Included in the Meta-narrative Review
| Overarching Traditions | Traditions | Authors (Year) | Scope | Country | Disciplines | Participants | PROMs / PREMs |
|---|---|---|---|---|---|---|---|
| Restoring / supporting independence and care at home | Person/family- centered care | Coleman et al. (2004) | Effectiveness of OAs and CGs engagement in care transitions | USA | Health Care Policy, Geriatric Medicine | OAs & CGs | PREM |
| Coleman et al. (2015) | Refinement of the Care Transitions Model focusing on FCGs needs | USA | Medicine, Policy, Nursing | FCGs & OAs | PREM | ||
| Hawkin (1996) | Identification of stressors experienced by daughters caregiving | USA | Nursing | FCGs | PROMs | ||
| Hoskins et al. (2005) | Evaluation of the effectiveness of interventions in reducing stress in carers | UK | Nursing, Health Science | FCGs | PROM | ||
| Marek et al. (2013) | Evaluate health outcomes of medication self-management with care coordination and technology | USA | Nursing, Health Economics | OAs & CGs | PROMs | ||
| Stolee et al. (2012) | Explore the responsiveness, feasibility, and utility of an individualized goal-setting and measurement approach (Goal Attainment Scaling) | Canada | Public Health, Sociology, Rehabilitation | OAs | PROMs | ||
| Stotter et al. (2015) | Comprehensive geriatric assessment and prediction of 3-year survival | UK | Medicine | OAs | PROMs | ||
| Health promotion | Markle-Reid et al. (2013) | To evaluate nurse-led health promotion and disease prevention interventions on HRQOL and autonomy of OAs | Canada | Nursing | OAs | PROMs | |
| Sarna et al. (2010) | Describe the physical and emotional QOL for older women with lung cancer | USA | Nursing, Medicine | OAs | PROMs | ||
| Sletvold et al. (2011) | Investigate a comprehensive geriatric assessment in OAs with hip fracture: A protocol | Norway | Medicine | OAs | PROMs | ||
| Comprehensive care for complex need | Berglund et al. (2013) | Analyze frail OA’s quality of care when receiving a comprehensive continuum of care intervention | Sweden | Public Health and Community Medicine, Social Medicine, Social Work, Medicine | OAs | *Unspecified PROM and PREM | |
| Berkman et al. (1999) | Examine viability of screening OAs with psychosocial needs with SF-36 to predict need for social work assessment | USA | Social Work | OAs | PROMs | ||
| Caplan et al. (2004) | Effectiveness of a comprehensive geriatric assessment and multidisciplinary intervention | Australia | Public Health and Community Medicine | OAs | PROMs | ||
| Hutchinson et al. (2013) | Describe the relationship between HRQOL of older adults with complex needs, readmission, and survival | Australia | Medicine | OAs | PROM | ||
| Disability | Fairhall et al. (2012) | To assess the impact of a multifactorial intervention on mobility | Australia & New Zealand | Physiotherapy, Neuroscience, Nursing, Medicine | OAs | PROMs | |
| Farriols et al. (2009) | Assess the predictive value of the truck control test on recovering ambulation in OAs who have developed walking-disability | Spain | Medicine, Rehabilitation | OAs | PROMs | ||
| Holt et al. (2013) | Identify impairment/s responsible for mobility decline and disability progression | USA | Rehabilitation, Medicine | OAs | PROMs | ||
| Evaluating / Decreasing utilization of health services (especially acute care) | Cost-effectiveness of an intervention to stay at/return to home setting | Anderson et al. (1999) | Effectiveness of a early hospital discharge | Australia | Medicine | OAs & FCGs | PROMs |
| Burch et al. (2000) | Comparing services after discharge | UK | General Medicine | OAs | PROMs and *Unspecified PROM | ||
| Cook et al. (2011) | Effectiveness of a post-fracture clinic: A protocol | Canada | Multidiscipline | OAs | PROMs | ||
| Hammar et al. (2009) | The cost-effectiveness of a home care program | Finland | Public Health | OAs | PROMs | ||
| Hughes et al. (2000) | Effectiveness of a home-based primary care intervention | USA | Public Health | OAs & FCGs | PROMs and PREM | ||
| Sandberg et al. (2015) | Effectiveness of a case management program | Sweden | Medicine | OAs | PROMs | ||
| Watson et al. (2015) | Comparison of transitional care programs | UK | Medicine, Health Sciences, Business | OAs | PROMs | ||
| Hospital discharge (planning) | Buurman et al. (2016) | Effectiveness of comprehensive geriatric assessment and transitional care program after discharge | Netherlands | Geriatric Medicine | OAs | PROMs | |
| Clark et al. (1997) | Impact of reduced hospital stay and discharge practices on OAs, and their FCGs | Australia | Occupational therapy, Physiotherapy & Nursing | OAs & FCGs | PROM and the OARS (which has both PROM and PREM questions) | ||
| Comans et al. (2013) | Impact of a transitional care program | Australia | Geriatric Medicine | OAs | PROMs | ||
| Joosten et al. (2003) | Agreement and disagreement between nurses and OAs about discharge needs | USA | Social Work | OAs | PROMs | ||
| Health service utilization | Asmus-Szepesi et al. (2014) | Formal and informal healthcare utilization costs until one year after hospitalization | Netherlands | Public Health, Policy & Management | OAs & CGs | PROMs | |
| Courtney et al. (2009) | Effectiveness of an exercise-based program | Australia | Nursing, Biomedical Sciences, Physiotherapy | OAs | PROM | ||
| Courtney et al. (2012) | Evaluate of a multifaceted transitional care intervention | Australia | Nursing, Biomedical Sciences, Physiotherapy | OAs | PROMs | ||
| De Almeida Mello et al. (2012) | Evaluation of innovative interventions to keep OAs at home and out of residential care: A protocol | Belgium | Public Health, Epidemiology, Sociology | OAs & FCGs | PROMs | ||
| Faucher et al. (2016) | The effectiveness of a transitional program | USA | Medicine, Health Sciences | OAs | *Unspecified PROM | ||
| Gladman et al. (1994) | Compare longitudinal effectiveness of home rehabilitation vs hospital-based rehabilitation | UK | Rehabilitation | OAs | PROMs | ||
| Hofhuis et al. (2011) | Assessment of impact of ICU stay on HRQOL in surviving octogenarians | Netherlands | Health Sciences, Medicine | OAs | PROM | ||
| Naylor et al. (2004) | Effectiveness of a transitional care intervention | USA | Nursing, Health Economics | OAs | PROMs | ||
| Rozario et al. (2006) | To measure intra-individual changes after discharge from an inpatient geropsychiatry unit | USA | Social Work | OAs | PROM | ||
| Rudd et al. (1997) | To evaluate early discharge policy with community based rehabilitation | UK | Medicine, Public Health | OAs & CGs | PROMs | ||
| Psychometric properties | Hokoishi et al. (2001) | Evaluate interrater reliability between multidisciplinary raters | Japan | Neuropsychiatry, Medicine, Health Science | OAs & FCGs | PROMs | |
| Hicks et al. (2009) | Evaluation of psychometric properties | USA | Physiotherapy | OAs | PROMs |
CGs: Caregivers (not explicitly identified as family caregivers); FCGs: Family caregivers; OAs: Older Adults; OARS: Older Americans Resources and Services Functional Assessment.
*Unspecified PROMs include those with limited information and/or no reference.
Appraising Phase
In addition to appraising the articles based on their relevance to the research question, the study quality of each article was assessed using the Mixed-Methods Appraisal Tool (MMAT) (Pace et al., 2012). All articles ranked as high- and medium-quality levels.
Synthesis Phase
The synthesis was iterative, entailed aggregation, contextualization, and interpretation of findings to create a storyline that thread through the different perspectives. To do so, all included studies were imported into NVivo11 to facilitate organizing the data. Two principal investigators and one research assistant independently read and re-read the data. The data from each study was interpreted within its own tradition. To unravel the overarching storylines of different research traditions, stakeholder perspectives were compared and contrasted across micro–meso–macro levels in healthcare.
Results
To answer our research question, we first address how PROMs and PREMs were used in transitions in care with frail older adults and their family caregivers, before addressing motivations for use.
Use in Transitions in Care
PROM and PREM instruments (54 PROMs; 4 PREMs; 1 with PROM and PREM elements; 6 unspecified PROMs) used in transitions of care were typically utilized independently, rarely used together (except in Berglund et al., 2013; Clark, Steinberg, & Bischoff, 1997; Hughes et al., 2000). (See Table 3 for study characteristics, and Supplementary Table 2 for instruments.) Following MNS, we assessed the research traditions that unfolded over time. Historically, PROMs were developed and used in contexts of research and clinical practice, whereas PREMs were developed and used for quality improvement and performance monitoring (Bryan et al., 2014; Miller, Gray, Kuluski, & Cott, 2015). Looking historically at the literature included in our MNS, the first article was published in 1994 (Gladman, Lincoln, & Group, 1994), and PROMs and PREMs were not used together in the context of supporting frail older adults, and their family caregivers, living at home for continuity across transition of care. Contextually, it is only more recent that PROMs and PREMs have begun to be used together (Black, Varaganum, & Hutchings, 2014; Hodson, Andrew, & Roberts, 2013; O’Connell et al., 2018), but this was not present in the literature included in our MNS.
Although continuity across transitions of care for older adults was widely recognized by scholars as a need due to “intricate, often disjoined care” systems (Naylor et al., 2004, p. 683) and “fragmented care and discontinuity” (Sandberg, Jakobsson, Midlov, & Kristensson, 2015, p. 1), this body of literature did not propose PROMs or PREMs as a resource to inform or guide continuity across transitions in care. Rather, their predominant use was to evaluate the effectiveness of an intervention or a program to support frail older adults and their families during care transitions. In addition, PROMs and PREMs have traditionally been used in isolation of one another, except in three instances (Berglund et al., 2013; Clark et al., 1997; Hughes et al., 2000), with PREMs being used much less frequently than PROMs.
In short, PROMs and PREMs were not used to guide care transitions. As Faucher, Rosedahl, Finnie, Glasgow, and Takahashi (2016) and Allen, Hutchinson, Brown, and Livingston (2014) identified, the efficacy of transitional care interventions were more commonly assessed with metrics such as 30-day hospital readmissions, whereas patients’ and family caregivers’ reports of experiences and satisfaction were less commonly utilized. This finding highlights that the impetus in the field has been to use these instruments as a means for intervention evaluation, not as means towards assessment of quality of life or experience for routine use and transitions of care.
The controversies raised in the literature were more general in nature, often pertaining to methods. These included:
instrument selection, particularly the inability to compare results when different instruments were used (Burch, Longbottom, McKay, Borland, & Prevost, 2000; Comans, Peel, Gray, & Scuffham, 2013; Markle-Reid, Browne, & Gafni, 2013; Sandberg et al., 2015);
frequency of instrument use (i.e., when and how often). As an example of siloing, they were primarily used within sectors, rarely across sectors, for use by healthcare professionals (Comans et al., 2013; Faucher, Rosedahl, Finnie, Glasgow, & Takahashi, 2016; Sarna et al., 2010);
who completed the instrument, recognizing the variability of sub-groups of frail older adults, and the inability to compare intervention results across groups (Courtney et al., 2009; Hicks & Manal, 2009; Markle-Reid et al., 2013; Naylor et al., 2004; Sandberg et al., 2015; Sarna et al., 2010);
how to treat missing data, at times modifying instruments for purposes of reporting (Comans et al., 2013; Fairhall et al., 2012; Stotter, Reed, Gray, Moore, & Robinson, 2015).
In summary, the routine use of PROMs or PREMs to assess outcomes or experience of care during transition was not a motivation found in the literature reviewed, nor was this identified as a gap or contested area in the body of literature.
Motivation for Use
Motivation underlying use of PROMs and PREMs can be grouped into two overarching “traditions”: (a) restoring/supporting independence and care at home, and (b) decreasing/evaluating utilization of health services, especially acute care (see Table 3).
Restoring/Supporting Independence and Care at Home
The first “tradition” underlying the motivation of diverse stakeholders to use PROMs and PREMs was their desire to restore/support independence and care at home, primarily at a micro-level of healthcare (Berglund et al., 2013; Berkman et al., 1999; Coleman, Roman, Hall, & Min, 2015; Fairhall et al., 2012; Farriols, Bajo, Muniesa, Escalada, & Miralles, 2009; Hawkins, 1996; Hoskins, Coleman, & McNeely, 2005; Hutchinson et al., 2013; Marek et al., 2013; Rozario, Morrow-Howell, & Proctor, 2006; Sarna et al., 2010; Sletvold et al., 2011; Stolee et al., 2012; Stotter et al., 2015), less often at the meso-level of healthcare programs/interventions (Caplan, Williams, Daly, & Abraham, 2004) (Coleman et al., 2004; Markle-Reid et al., 2013). A person/family-centered approach underpinned the use of PROMs and PREMs primarily at micro-levels of healthcare (Hawkins, 1996; Hoskins et al., 2005; Marek et al., 2013; Stolee et al., 2012; Stotter et al., 2015), with only one at the meso-level (Coleman et al., 2004). Of note, the stress and “burden” on family caregivers was highly acknowledged and interventions focused on providing a family-centered approach at a mico-level (Coleman et al., 2015; Hawkins, 1996; Hoskins et al., 2005).
A focus on health promotion influenced interventions to support frail older adults, specifically with the intention to improve their quality of life and support them in their independence to not only live at home, but also reduce hospital time. A holistic emphasis underpinned one macro-level use of PROMs to evaluate three nurse-led health promotion and disease prevention interventions targeting risk factors of frailty and functional decline with community-living frail older adults (Markle-Reid et al., 2013). On a micro-level, scholars investigated how health-promoting interventions affected the quality of life of frail older women with lung cancer (Sarna et al., 2010) or older adults with hip fractures (Sletvold et al., 2011). Interventions to support continuity across transitions (Markle-Reid et al., 2013) or transitions of care (Sarna et al., 2010; Sletvold et al., 2011) underscored the need for health-promoting provision of care.
In the context of restoring/supporting independence and care at home, the complexity of needs (Berkman et al., 1999; Hutchinson et al., 2013) and disability (Fairhall et al., 2012; Farriols et al., 2009; Holt et al., 2013) of frail older adults was paramount. Comprehensive, coordinated care that manages continuity of care across sectors (Berglund et al., 2013; Caplan et al., 2004) in often-fragmented healthcare systems (Berglund et al., 2013) was offered as a means to address the complex needs of frail older adults living at home. Stakeholders (researchers) addressing frail older adults experiencing disability did so from an overarching framework of rehabilitation (Holt et al., 2013) at a micro-level. PROM use was to aid identification of impairments longitudinally (Holt et al., 2013), or to evaluate interventions targeting mobility-related disability (Fairhall et al., 2012; Farriols et al., 2009). The use of PROMs and PREMs with family caregivers was notably absent in this subset of literature pertaining to comprehensive care for complex need or disability.
Evaluating/Decreasing Utilization of Health Services (Especially Acute Care)
The second “tradition” underlying the motivation to use PROMs and PREMs was to evaluate health service utilization, including cost-effectiveness of programs and hospital discharge (planning). Although this focus existed across all levels of healthcare, there were two examinations at a macro-level (Buurman et al., 2016; De Almeida Mello, Van Durme, Macq, & Declercq, 2012). The rest were closely split between micro-level impact on the older adult or caregiver (Clark et al., 1997; Comans et al., 2013; Faucher et al., 2016; Gladman et al., 1994; Hicks & Manal, 2009; Hofhuis, van Stel, Schrijvers, Rommes, & Spronk, 2011; Hokoishi et al., 2001; Joosten & Potts, 2003; Rozario et al., 2006) and meso-levels of healthcare programs/interventions (Anderson et al., 2000; Asmus-Szepesi et al., 2014; Burch et al., 2000; Buurman et al., 2016; Cook et al., 2011; Courtney et al., 2009; Courtney et al., 2012; Naylor et al., 2004; Rudd, Wolfe, Tilling, & Beech, 1997; Sandberg et al., 2015; Watson et al., 2015).
PROMs were used in the consideration of health services utilization when transitioning from hospital (including emergency and ICU) to home. At a micro-level, PROMs were used to identify the impact of transition of care on the quality of life for the older adult (Faucher et al., 2016; Gladman et al., 1994; Hofhuis et al., 2011; Rozario et al., 2006). These results were used for evaluation of health services provided, but PROM reports were not provided to healthcare professionals, nor were they used to inform care. At a meso-level, PROMs were used in the context of comparing formal and informal healthcare costs for hospitalized older adults (Asmus-Szepesi et al., 2014), utilization of an exercise-based model of hospital and home care follow-up (Courtney et al., 2009; Courtney et al., 2012), early hospital discharge policy (Rudd et al., 1997), and effectiveness of a transitional care intervention provided by advanced practice nurses to older adults hospitalized with heart failure (Naylor et al., 2004). At a macro-level, De Almeida Mello et al. (2012) proposed the use of PROMS to compare the effectiveness of innovations to delay institutionalization of frail older adults. Although this article was a study protocol, their purpose was to determine which interventions could be added to home-care services already funded in Belgium. This overarching motivation to PROM use was considered from the perspectives of stakeholders invested in all levels of healthcare decision-making.
Stakeholders were motivated to use PROMs and PREMs at the meso-level to evaluate the cost-effectiveness of hospitals and programs testing interventions on the effectiveness of supporting frail older adults to stay at/return to home. Although some studies used instruments in the context of cost-evaluation (Anderson et al., 2000; Burch et al., 2000; Hughes et al., 2000), four studies used these instruments directly as a part of the cost-evaluation (Cook et al., 2011; Hammar, Rissanen, & Perälä, 2009; Sandberg et al., 2015; Watson et al., 2015). The primary context of transition of care was from hospital to home, often explicitly to minimize hospital stay.
Discharge from hospital, and planning to this end, was acknowledged as an important element of continuity across transitions in care from the patient and caregiver perspective. At a micro-level, research addressed the impact on frail older adults and their family caregivers (Clark et al., 1997), the impact of adequate discharge planning (Comans et al., 2013), or areas of agreement and disagreement between older adult patients and nurses regarding perceived needs following hospital discharge (Joosten & Potts, 2003). Buurman et al. (2016) uniquely focused on macro-level effectiveness of a comprehensive geriatric assessment and transitional care program after discharge, with a focus on continuity of care. This was also a rare instance in which PROM results were provided to a nurse during the intervention (Buurman et al., 2016). Compared with the other studies in this section, those focused on hospital discharge had less emphasis on costs and resource allocation. Instead, the focus on was the impact of discharge to the frail older adult and their family caregivers.
Two articles focused on psychometric evaluations of PROMs for older adults living at home (not in hospital) (Hicks & Manal, 2009; Hokoishi et al., 2001). Their use was at a micro-level, included an evaluation of interrater reliability between multidisciplinary raters to ensure consistency when used by different professionals (Hokoishi et al., 2001), as well as a psychometric evaluation to support use in care and research with community-dwelling adults living with back pain (Hicks & Manal, 2009). Although they did not focus on utilization of health services, they were both motivated to develop robust methods for fulsome use both in healthcare practice and research settings.
Implications
Recommendations phase
The motivations underlying stakeholders’ use of PROMs and PREMs in the context of continuity across transitions in care for frail older adults and their family caregivers living at home were distinct, yet synergistic between:
the ideological desire to restore/support independence and care at home, and
system goals to evaluate/decrease utilization of health services, especially inpatient hospital care.
Working towards improving quality of life and care, these motivations are not in conflict, but rather in synch across micro–meso–macro levels of healthcare. These motivations are related in a dialectic manner (Öhlén et al., 2017) in that the goals of restoring/supporting independence and care at home are often of utmost importance to the older adult and caregiver, and evaluating/decreasing utilization of health services is paramount for the healthcare system. Policymakers, including the KUs on our team, work to balance and enact both goals. Through this synthesis, we have added to the body of literature by identifying that PROMs and PREMs are used not only with the intention to promote independence for frail older adults and their family caregivers, but to also as a metric for evaluation of health service utilization, particularly the emergency, ICU, and hospital.
We suggest that there is a missed opportunity here for PROMs and PREMs to be used together (Caneiras et al., 2019; Hodson et al., 2019; O’Connell et al., 2018; Walker et al., 2017) to support the journey by frail older adults, and their families, across the care continuum involving multiple healthcare sectors. We found minimal evidence of this in the literature, nor did we see it highlighted as an area of concern. At a micro-level, routine use of PROMs offers opportunities for individuals to see their own trajectories and actively discuss these with their healthcare providers (Greenhalgh, 2009; Greenhalgh et al., 2005; Greenhalgh et al., 2017; Greenhalgh et al., 2018; Krawczyk et al., 2019). Clinicians may use these reports to not only help them prioritize care (Donaldson, 2008; Greenhalgh, 2009; Greenhalgh et al., 2017), but in discussion with patients and family caregivers to make shared decisions about treatment and discharge plans, as well as with clinicians in other sectors during transitions of care. However, in this body of literature, micro-level use was rarely integrated at the point-of-care. Rather, the focus was on the impact of transition of care on the quality of life for older adults (Clark et al., 1997; Comans et al., 2013; Fairhall et al., 2012; Farriols et al., 2009; Faucher et al., 2016; Gladman et al., 1994; Hicks & Manal, 2009; Hofhuis et al., 2011; Hokoishi et al., 2001; Holt et al., 2013; Joosten & Potts, 2003; Rozario et al., 2006; Sarna et al., 2010; Sletvold et al., 2011) and family caregivers (Clark et al., 1997; Coleman et al., 2015; Hawkins, 1996; Hoskins et al., 2005). At a meso-level, these data could be used for quality improvement of processes, including workflow (Krawczyk et al., 2019) and resource allocation within programs intended to assist transitions. At a macro-level, the use of PROMs and PREMs across transitions of care offers potential insights for health organizations and government ministries that similarly desire to optimize the bridging of health services, while restoring and maintaining independence for frail older adults and their families living at home.
Although our KUs are particularly interested in meso- and macro-level use of PROMs and PREMs in this context, the literature providing guidance in these areas was lean. Nonetheless, it is an area that requires timely evidence. For example, accreditation bodies and international health institutes around the world are collectively focusing on “patient flow” (Emergency Health and Planning Services, 2017; Institute for Healthcare Improvement, 2003; Showell et al., 2012; The Health Foundation, 2013). Patient or client flow is a term that has been coined to prompt healthcare organization leaders and care providers to examine the impediments to timely and efficient flow of patients between hospital departments. For KUs on our team in Canada, “client flow” has been articulated as a part of the Worklife/Workforce Patient Safety Area highlighted by Accreditation Canada (2016; 2017) in “Required Organizational Practices.” Although patient flow efforts have primarily focused on reducing waits and bottlenecks within hospitals, we suggest that looking at patient flow through the lens of continuity across transitions in care across micro–meso–macro levels, rather than between isolated programs, presents an opportunity to improve the care of older adults and their family caregivers, as they move not only between hospital departments, but back to their home, home communities, and community-based providers.
Further research is needed to guide scientifically rigorous development and use of PROMs and PREMs for providing a person/family-centered perspective of the experiences and outcomes associated with continuity across transitions in care. Such research requires collaborations with community agencies, primary care providers, hospital-based clinicians, and frail older adults and their family caregivers.
Limitations
Although our MNS was developed following well-established guidelines (Gough, 2013; Greenhalgh & Wong, 2013), there are limitations. First, our review is limited to the English language. As a result, cultural differences in studies conducted in countries where English is not the predominant language may not be represented. Second, our searches primarily retrieved peer-reviewed sources and omitted gray literature; thus, results may be influenced by publication bias. Third, only two articles (Buurman et al., 2016; De Almeida Mello et al., 2012) addressed macro-level use of PROMs and PREMs. Thus, recommendations need to be critically appraised by readers in applying these to the unique context in which they work—a caveat which applies to the nature of any meta-analyses.
Conclusions
PROMs have a longer history of use than PREMs; thus, it is not surprising that PROMs were predominantly used, and rarely used with PREMs in transitions in care for frail older adults and their family caregivers. PROM and PREM use was frequently enacted for the purposes of evaluating the effectiveness of an intervention or a program to support frail older adults, and their families, during care transitions. The motivations underlying stakeholders’ use were distinct, yet synergistic between (1) the ideological desire to restore/support independence and care at home and (2) system goals to evaluate/decrease utilization of health services, especially inpatient hospital care. Future research and service delivery is needed to investigate how PROMs and PREMs may be used together across micro–meso–macro levels of healthcare to inform continuity across transitions of care.
Supplementary Material
Acknowledgments
We thank Stirling Bryan, Michelina Mancuso, Margaret McGregor, Ayumi Sasaki, Kelli Stajduhar, Carolyn Tayler, and Geoff Wong who were Research Team members involved in this research.
Funding
This work was supported by Canadian Institutes of Health Research for the project, “A meta-narrative review of patient- and family-reported experience and outcome measures across transitions of care for frail seniors living at home” (Grant number: 144042).
Authors’ Contributions
R. S., K. S-. M., and L.C. co-designed and co-led the study. K. S-. M. led the MNS analysis and the drafting and revisions of the manuscript. D. D., S. R. C., and N. H. substantially contributed to the design of the study. All authors helped write and revise the manuscript for intellectual content, and all read and approved the final manuscript.
Conflict of Interest
K. S.-M. is an assistant professor in the Faculty of Nursing, University of Alberta. She is also a New Investigator funded by Can-SOLVE CKD—KRESCENT (Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease; Kidney Research Scientist Core Education & National Training Program). R.S.: This analysis was undertaken, in part, thanks to funding from the Canada Research Chairs (CRC) program supporting Dr. Sawatzky’s CRC in Person-Centered Outcomes.
References
- Accreditation Canada. (2016). Priority Process: Patient Flow. Retrieved from https://www3.accreditation.ca/SurveyorPreSurvey/PDF/Tracers/Current/en-CA/Patient%20Flow.pdf. Accessed December 20, 2019.
- Accreditation Canada . (2017). Required Organizational Practices (ROPs). Retrieved from https://accreditation.ca/required-organizational-practices/. Accessed April 17, 2019.
- Allen, J., Hutchinson, A. M., Brown, R., & Livingston, P. M. (2014). Quality care outcomes following transitional care interventions for older people from hospital to home: A systematic review. BMC Health Services Research, 14, 346. doi:10.1186/1472-6963-14-346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, C., Rubenach, S., Mhurchu, C. N., Clark, M., Spencer, C., & Winsor, A. (2000). Home or hospital for stroke rehabilitation? Results of a randomized controlled trial. Stroke, 31, 1024–1031. doi: 10.1161/01.STR.31.5.1024 [DOI] [PubMed] [Google Scholar]
- Asmus-Szepesi, K. J., Koopmanschap, M. A., Flinterman, L. E., Bakker, T. J., Mackenbach, J. P., & Steyerberg, E. W. (2014). Formal and informal care costs of hospitalized older people at risk of poor functioning: A prospective cohort study. Archives of Gerontology and Geriatrics, 59, 382–392. doi:10.1016/j.archger.2014.04.014 [DOI] [PubMed] [Google Scholar]
- Benstson, V. L., & Lowenstein, A. eds. (. 2017). Global aging and challenges to families.New York: Routledge. [Google Scholar]
- Bennett, D.(Writer). (2019). Falling Through the Cracks: Greg’s Story In. Canada: Greg’s Wings Projects. Retrieved from http://gregswings.ca/fttc-gregsstory/. Accessed December 20, 2019.
- Berglund, H., Wilhelmson, K., Blomberg, S., Dunér, A., Kjellgren, K., & Hasson, H. (2013). Older people’s views of quality of care: A randomised controlled study of continuum of care. Journal of Clinical Nursing, 22, 2934–2944. doi:10.1111/jocn.12276 [DOI] [PubMed] [Google Scholar]
- Berkman, B., Chauncey, S., Holmes, W., Daniels, A., Bonander, E., Sampson, S., & Robinson, M. (1999). Standardized screening of elderly patients’ needs for social work assessment in primary care: Use of the SF-36. Health & Social Work, 24, 9–16. doi:10.1093/hsw/24.1.9 [DOI] [PubMed] [Google Scholar]
- Black, N., Varaganum, M., & Hutchings, A. (2014). Relationship between patient reported experience (PREMs) and patient reported outcomes (PROMs) in elective surgery. BMJ Quality & Safety, 23, 534–542. doi:10.1136/bmjqs-2013-002707 [DOI] [PubMed] [Google Scholar]
- Bryan, S., Davis, J., Broesch, J., Doyle-Waters, M. M., Lewis, S., McGrail, K., … Sawatzky, R. (2014). Choosing your partner for the PROM: a review of evidence on patient-reported outcome measures for use in primary and community care. Healthcare Policy, 10, 38–51. [PMC free article] [PubMed] [Google Scholar]
- Burch, S., Longbottom, J., McKay, M., Borland, C., & Prevost, T. (2000). The Huntingdon Day Hospital Trial: Secondary outcome measures. Clinical Rehabilitation, 14, 447–453. doi:10.1191/0269215500cr334oa [DOI] [PubMed] [Google Scholar]
- Buurman, B. M., Parlevliet, J. L., Allore, H. G., Blok, W., van Deelen, B. A., Moll van Charante, E. P.,…de Rooij, S. E. (2016). Comprehensive geriatric assessment and transitional care in acutely hospitalized patients: The transitional care bridge randomized clinical trial. JAMA Internal Medicine, 176, 302–309. doi:10.1001/jamainternmed.2015.8042 [DOI] [PubMed] [Google Scholar]
- Caldwell, S. E., & Mays, N. (2012). Studying policy implementation using a macro, meso and micro frame analysis: The case of the Collaboration for Leadership in Applied Health Research & Care (CLAHRC) programme nationally and in North West London. Health Research Policy and Systems, 10, 32. doi:10.1186/1478-4505-10-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Institute for Health Information . (2012). All-Cause Readmission to Acute Care and Return to the Emergency Department. Retrieved from https://secure.cihi.ca/free_products/Readmission_to_acutecare_en.pdf. Accessed December 20, 2019.
- Canadian Institutes of Health Research . (2019). Transitions in Care – Overview. Retrieved from http://www.cihr-irsc.gc.ca/e/50972.html. Accessed December 20, 2019.
- Caneiras, C., Jácome, C., Mayoralas-Alises, S., Ramon Calvo, J., Almeida Fonseca, J., Escarrabill, J., & Winck, J. C. (2019). Patient experience in home respiratory therapies: Where we are and where to go. Journal of Clinical Medicine, 8, 555. doi: 10.3390/jcm8040555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplan, G. A., Williams, A. J., Daly, B., & Abraham, K. (2004). A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department–the DEED II study. Journal of the American Geriatrics Society, 52, 1417–1423. doi:10.1111/j.1532-5415.2004.52401.x [DOI] [PubMed] [Google Scholar]
- Clark, M., Steinberg, M., & Bischoff, N. (1997). Patient readiness for return to home: Discord between expectations and reality. Australian Occupational Therapy Journal, 44, 132–141. doi: 10.1111/j.1440–1630.1997.tb00765.x [Google Scholar]
- Cohen, R., Leis, A. M., Kuhl, D., Charbonneau, C., Ritvo, P., & Ashbury, F. D. (2006). QOLLTI-F: Measuring family carer quality of life. Palliative Medicine, 20, 755–767. doi:10.1177/0269216306072764 [DOI] [PubMed] [Google Scholar]
- Cohen, S. R., Mount, B. M., Strobel, M. G., & Bui, F. (1995). The McGill Quality of Life Questionnaire: A measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliative Medicine, 9, 207–219. doi:10.1177/026921639500900306 [DOI] [PubMed] [Google Scholar]
- Cohen, S. R., Sawatzky, R., Russell, L. B., Shahidi, J., Heyland, D. K., & Gadermann, A. M. (2017). Measuring the quality of life of people at the end of life: The McGill Quality of Life Questionnaire-Revised. Palliative Medicine, 31, 120–129. doi:10.1177/0269216316659603 [DOI] [PubMed] [Google Scholar]
- Coleman, E. A., Roman, S. P., Hall, K. A., & Min, S. J. (2015). Enhancing the care transitions intervention protocol to better address the needs of family caregivers. Journal for Healthcare Quality, 37, 2–11. doi:10.1097/01.JHQ.0000460118.60567.fe [DOI] [PubMed] [Google Scholar]
- Coleman, E. A., Smith, J. D., Frank, J. C., Min, S. J., Parry, C., & Kramer, A. M. (2004). Preparing patients and caregivers to participate in care delivered across settings: The Care Transitions Intervention. Journal of the American Geriatrics Society, 52, 1817–1825. doi:10.1111/j.1532-5415.2004.52504.x [DOI] [PubMed] [Google Scholar]
- Comans, T. A., Peel, N. M., Gray, L. C., & Scuffham, P. A. (2013). Quality of life of older frail persons receiving a post-discharge program. Health and Quality of Life Outcomes, 11, 58. doi:10.1186/1477-7525-11-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook, W. L., Khan, K. M., Bech, M. H., Brasher, P. M., Brown, R. A., Bryan, S.,…Ashe, M. C. (2011). Post-discharge management following hip fracture–get you back to B4: A parallel group, randomized controlled trial study protocol. BMC Geriatrics, 11, 30. doi:10.1186/1471-2318-11-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney, M. D., Edwards, H. E., Chang, A. M., Parker, A. W., Finlayson, K., Bradbury, C., & Nielsen, Z. (2012). Improved functional ability and independence in activities of daily living for older adults at high risk of hospital readmission: A randomized controlled trial. Journal of Evaluation In Clinical Practice, 18, 128–134. doi:10.1111/j.1365-2753.2010.01547.x [DOI] [PubMed] [Google Scholar]
- Courtney, M., Edwards, H., Chang, A., Parker, A., Finlayson, K., & Hamilton, K. (2009). Fewer emergency readmissions and better quality of life for older adults at risk of hospital readmission: A randomized controlled trial to determine the effectiveness of a 24-week exercise and telephone follow-up program. Journal of the American Geriatrics Society, 57, 395–402. doi:10.1111/j.1532-5415.2009.02138.x [DOI] [PubMed] [Google Scholar]
- Cuthbertson, L.(May 2014). Continuity across transitions of care – Does it differ from integrated care and other terms?. Vancouver, BC. [Google Scholar]
- De Almeida Mello, J., Van Durme, T., Macq, J., & Declercq, A. (2012). Interventions to delay institutionalization of frail older persons: Design of a longitudinal study in the home care setting. BMC Public Health, 12, 615. doi:10.1186/1471-2458-12-615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson, M. S. (2008). Taking PROs and patient-centered care seriously: Incremental and disruptive ideas for incorporating PROs in oncology practice. Quality of Life Research, 17, 1323–1330. doi:10.1007/s11136-008-9414-6 [DOI] [PubMed] [Google Scholar]
- Emergency Health and Planning Services, Health Prince Edward Island . (2017). Patient flow and system utilization system, 2017-2020. Prince Edward Island. Retrieved from https://www.princeedwardisland.ca/sites/default/files/publications/patient_flow_and_system_utilization_strategy_2017-2020.pdf
- Fairhall, N., Sherrington, C., Kurrle, S. E., Lord, S. R., Lockwood, K., & Cameron, I. D. (2012). Effect of a multifactorial interdisciplinary intervention on mobility-related disability in frail older people: Randomised controlled trial. BMC Medicine, 10, 120. doi:10.1186/1741-7015-10-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farriols, C., Bajo, L., Muniesa, J. M., Escalada, F., & Miralles, R. (2009). Functional decline after prolonged bed rest following acute illness in elderly patients: Is trunk control test (TCT) a predictor of recovering ambulation? Archives of Gerontology and Geriatrics, 49, 409–412. doi:10.1016/j.archger.2008.12.008 [DOI] [PubMed] [Google Scholar]
- Faucher, J., Rosedahl, J., Finnie, D., Glasgow, A., & Takahashi, P. (2016). Patient quality of life in the Mayo Clinic Care Transitions program: A survey study. Patient Preference and Adherence, 10, 1679–1685. doi:10.2147/PPA.S109157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fayers, P., & Machin, D. (2016). Quality of life: The assessment, analysis and reporting of patient-reported outcomes. 3rd ed.Oxford: Wiley; 2016. [Google Scholar]
- Gladman, J., Lincoln, N., & Group, D. S. (1994). Follow-up of a controlled trial of domiciliary stroke rehabilitation (DOMINO Study). Age and Ageing, 23, 9–13. doi: 10.1093/ageing/23.1.9 [DOI] [PubMed] [Google Scholar]
- Gough, D. (2013). Meta-narrative and realist reviews: Guidance, rules, publication standards and quality appraisal. BMC Medicine, 11, 22. doi:10.1186/1741-7015-11-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh, J. (2009). The applications of PROs in clinical practice: What are they, do they work, and why? Quality of Life Research, 18, 115–123. doi:10.1007/s11136-008-9430-6 [DOI] [PubMed] [Google Scholar]
- Greenhalgh, T., & Wong, G. (2013). Training materials for meta-narrative reviews. [Google Scholar]
- Greenhalgh, J., Dalkin, S., Gibbons, E., Wright, J., Valderas, J. M., Meads, D., & Black, N. (2018). How do aggregated patient-reported outcome measures data stimulate health care improvement? A realist synthesis. Journal of Health Services Research & Policy, 23, 57–65. doi: 10.1177/1355819617740925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh, J., Dalkin, S., Gooding, K., Gibbons, E., Wright, J., Meads, D., … Pawson, R. (2017). Functionality and feedback: A realist synthesis of the collation, interpretation and utilisation of patient-reported outcome measures data to improve patient care. Health Services and Delivery Research, 5, 1–280. doi: 10.3310/hsdr05020 [PubMed] [Google Scholar]
- Greenhalgh, J., Long, A. F., & Flynn, R. (2005). The use of patient reported outcome measures in routine clinical practice: Lack of impact or lack of theory? Social Science & Medicine (1982), 60, 833–843. doi:10.1016/j.socscimed.2004.06.022 [DOI] [PubMed] [Google Scholar]
- Greenhalgh, T., Robert, G., Macfarlane, F., Bate, P., Kyriakidou, O., & Peacock, R. (2005). Storylines of research in diffusion of innovation: A meta-narrative approach to systematic review. Social Science & Medicine (1982), 61, 417–430. doi:10.1016/j.socscimed.2004.12.001 [DOI] [PubMed] [Google Scholar]
- Haggerty, J. L., Reid, R. J., Freeman, G. K., Starfield, B. H., Adair, C. E., & McKendry, R. (2003). Continuity of care: A multidisciplinary review. BMJ (Clinical Research ed.), 327, 1219–1221. doi:10.1136/bmj.327.7425.1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty, J. L., Roberge, D., Freeman, G. K., & Beaulieu, C. (2013). Experienced continuity of care when patients see multiple clinicians: A qualitative metasummary. Annals of Family Medicine, 11, 262–271. doi:10.1370/afm.1499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammar, T., Rissanen, P., & Perälä, M. L. (2009). The cost-effectiveness of integrated home care and discharge practice for home care patients. Health Policy (Amsterdam, Netherlands), 92, 10–20. doi:10.1016/j.healthpol.2009.02.002 [DOI] [PubMed] [Google Scholar]
- Hawkins, B. (1996). Daughters and caregiving: Taking care of our own. AAOHN Journal, 44, 433–437. doi: 10.1177/216507999604400904 [PubMed] [Google Scholar]
- Hewitt-Taylor, J. (2015). Developing person-centred practice: A practical approach to quality healthcare. London: Palgrave Macmillan. [Google Scholar]
- Heyland, D. K., Cook, D. J., Rocker, G. M., Dodek, P. M., Kutsogiannis, D. J., Skrobik, Y.,…Cohen, S. R.; Canadian Researchers at the End of Life Network . (2010). The development and validation of a novel questionnaire to measure patient and family satisfaction with end-of-life care: The Canadian Health Care Evaluation Project (CANHELP) Questionnaire. Palliative Medicine, 24, 682–695. doi:10.1177/0269216310373168 [DOI] [PubMed] [Google Scholar]
- Hicks, G. E., & Manal, T. J. (2009). Psychometric properties of commonly used low back disability questionnaires: Are they useful for older adults with low back pain? Pain Medicine (Malden, Mass.), 10, 85–94. doi:10.1111/j.1526-4637.2008.00548.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodson, M., Andrew, S., & Roberts, C. M. (2013). Towards an understanding of PREMS and PROMS in COPD. Breathe, 9, 358–364. doi: 10.1183/20734735.006813 [Google Scholar]
- Hodson, M., Roberts, C. M., Andrew, S., Graham, L., Jones, P. W., & Yorke, J. (2019). Development and first validation of a patient-reported experience measure in chronic obstructive pulmonary disease (PREM-C9). Thorax, 74, 600–603. doi:10.1136/thoraxjnl-2018-211732 [DOI] [PubMed] [Google Scholar]
- Hofhuis, J. G. M., van Stel, H. F., Schrijvers, A. J. P., Rommes, J. H., & Spronk, P. E. (2011). Changes of health-related quality of life in critically ill octogenarians: a follow-up study. CHEST, 140, 1473–1483. doi:10.1378/chest.10-0803 [DOI] [PubMed] [Google Scholar]
- Hokoishi, K., Ikeda, M., Maki, N., Nomura, M., Torikawa, S., Fujimoto, N.,…Tanabe, H. (2001). Interrater reliability of the Physical Self-Maintenance Scale and the Instrumental Activities of Daily Living Scale in a variety of health professional representatives. Aging & Mental Health, 5, 38–40. doi:10.1080/13607860020020627 [DOI] [PubMed] [Google Scholar]
- Holt, N. E., Percac-Lima, S., Kurlinski, L. A., Thomas, J. C., Landry, P. M., Campbell, B.,…Bean, J. F. (2013). The boston rehabilitative impairment study of the elderly: A description of methods. Archives of Physical Medicine and Rehabilitation, 94, 347–355. doi:10.1016/j.apmr.2012.08.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoskins, S., Coleman, M., & McNeely, D. (2005). Stress in carers of individuals with dementia and Community Mental Health Teams: An uncontrolled evaluation study. Journal of Advanced Nursing, 50, 325–333. doi:10.1111/j.1365-2648.2005.03396.x [DOI] [PubMed] [Google Scholar]
- Hughes, S. L., Weaver, F. M., Giobbie-Hurder, A., Manheim, L., Henderson, W., Kubal, J. D.,…Cummings, J.; Department of Veterans Affairs Cooperative Study Group on Home-Based Primary Care . (2000). Effectiveness of team-managed home-based primary care: A randomized multicenter trial. JAMA, 284, 2877–2885. doi:10.1001/jama.284.22.2877 [DOI] [PubMed] [Google Scholar]
- Hutchinson, A., Rasekaba, T. M., Graco, M., Berlowitz, D. J., Hawthorne, G., & Lim, W. K. (2013). Relationship between health-related quality of life, and acute care re-admissions and survival in older adults with chronic illness. Health and Quality of Life Outcomes, 11, 136. doi:10.1186/1477-7525-11-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Healthcare Improvement . (2003). Optimizing patient flow: Moving patients smoothly through acute care settings. IHI Innovation Series white paper. Boston: Institute for Healthcare Improvement, p. 12 Retrieved from www.ihi.org/knowledge/Pages/IHIWhitePapers/OptimizingPatientFlowMovingPatientsSmoothlyThroughAcuteCareSettings.aspx. Accessed December 20, 2019.
- Joosten, D., & Potts, M. (2003). Areas of discharge agreement and disagreement between older adult patients and nurses. Care Management Journals, 4, 185–190. doi:10.1891/cmaj.4.4.185.63690 [DOI] [PubMed] [Google Scholar]
- Kingsley, C., & Patel, S. (2017). Patient-reported outcome measures and patient-reported experience measures. BJA Education, 17, 137–144. doi: 10.1093/bjaed/mkw060 [Google Scholar]
- Krawczyk, M., Sawatzky, R., Schick-Makaroff, K., Stajduhar, K., Öhlen, J., Reimer-Kirkham, S., … Cohen, R. (2019). Micro-Meso-macro practice tensions in using patient-reported outcome and experience measures in hospital palliative care. Qualitative Health Research, 29, 510–521. doi: 10.1177/1049732318761366 [DOI] [PubMed] [Google Scholar]
- Marek, K. D., Stetzer, F., Ryan, P. A., Bub, L. D., Adams, S. J., Schlidt, A.,…O’Brien, A. M. (2013). Nurse care coordination and technology effects on health status of frail older adults via enhanced self-management of medication: Randomized clinical trial to test efficacy. Nursing Research, 62, 269–278. doi:10.1097/NNR.0b013e318298aa55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markle-Reid, M., Browne, G., & Gafni, A. (2013). Nurse-led health promotion interventions improve quality of life in frail older home care clients: Lessons learned from three randomized trials in Ontario, Canada. Journal of Evaluation in Clinical Practice, 19, 118–131. doi:10.1111/j.1365-2753.2011.01782.x [DOI] [PubMed] [Google Scholar]
- Miller, D., Steele Gray, C., Kuluski, K., & Cott, C. (2015). Patient-Centered Care and Patient-Reported Measures: Let’s Look Before We Leap. The Patient, 8, 293–299. doi:10.1007/s40271-014-0095-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor, M. D., Brooten, D. A., Campbell, R. L., Maislin, G., McCauley, K. M., & Schwartz, J. S. (2004). Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. Journal of the American Geriatrics Society, 52, 675–684. doi:10.1111/j.1532-5415.2004.52202.x [DOI] [PubMed] [Google Scholar]
- O’Connell, S., Palmer, R., Withers, K., Saha, N., Puntoni, S., & Carolan-Rees, G.; PROMs, PREMs and Effectiveness Programme . (2018). Requirements for the collection of electronic PROMS either “in clinic” or “at home” as part of the PROMs, PREMs and Effectiveness Programme (PPEP) in Wales: A feasibility study using a generic PROM tool. Pilot and Feasibility Studies, 4, 90. doi:10.1186/s40814-018-0282-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öhlén, J., Reimer‐Kirkham, S., Astle, B., Håkanson, C., Lee, J., Eriksson, M., & Sawatzky, R. (2017). Person‐centred care dialectics—Inquired in the context of palliative care. Nursing Philosophy, 18, e12177. doi: 10.1111/nup.12177 [DOI] [PubMed] [Google Scholar]
- Pace, R., Pluye, P., Bartlett, G., Macaulay, A. C., Salsberg, J., Jagosh, J., & Seller, R. (2012). Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. International Journal of Nursing Studies, 49, 47–53. doi:10.1016/j.ijnurstu.2011.07.002 [DOI] [PubMed] [Google Scholar]
- Picker Institute . (2019). About us: Principles of person centered care. Retrieved from https://www.picker.org/about-us/picker-principles-of-person-centred-care/. Accessed December 20, 2019.
- Raîche, M., Hébert, R., & Dubois, M.-F. (2008). PRISMA-7: A case-finding tool to identify older adults with moderate to severe disabilities. Archives of Gerontology and Geriatrics, 47, 9–18. doi: 10.1016/j.archger.2007.06.004 [DOI] [PubMed] [Google Scholar]
- Rozario, P. A., Morrow-Howell, N. L., & Proctor, E. K. (2006). Changes in the SF-12 among depressed elders six months after discharge from an inpatient geropsychiatric unit. Quality of Life Research, 15, 755–759. doi:10.1007/s11136-005-3996-z [DOI] [PubMed] [Google Scholar]
- Rudd, A. G., Wolfe, C. D., Tilling, K., & Beech, R. (1997). Randomised controlled trial to evaluate early discharge scheme for patients with stroke. BMJ (Clinical Research ed.), 315, 1039–1044. doi:10.1136/bmj.315.7115.1039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg, M., Jakobsson, U., Midlöv, P., & Kristensson, J. (2015). Cost-utility analysis of case management for frail older people: Effects of a randomised controlled trial. Health Economics Review, 5, 51. doi:10.1186/s13561-015-0051-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarna, L., Cooley, M. E., Brown, J. K., Chernecky, C., Padilla, G., Danao, L.,…Elashoff, D. (2010). Women with lung cancer: Quality of life after thoracotomy: A 6-month prospective study. Cancer Nursing, 33, 85–92. doi:10.1097/NCC.0b013e3181be5e51 [DOI] [PubMed] [Google Scholar]
- Sawatzky, R., Chan, E. C. K., Bryan, S., Cohen, R., Cuthbertson, L., Dixon, D., … Tayler, C. (2015). Patient- and family-reported experience and outcome measures for use in acute care: A knowledge synthesis. Retrieved from 10.6084/m9.figshare.1412721. Accessed December 20, 2019. [DOI]
- Schang, L., Waibel, S., & Thomson, S. (2013). Measuring care coordination: Health system and patient perspectives: Report prepared for the Main Association of Austrian Social Security Institutions. London: LSE Health. [Google Scholar]
- Showell, C., Ellis, L., Keen, E., Cummings, E., Georgiou, A., & Turner, P. (2012). An evidence-based review and training resource on smooth patient flow. Retrieved from https://researchers.mq.edu.au/en/publications/an-evidence-based-review-and-training-resource-on-smooth-patient. Accessed December 20, 2019.
- Sletvold, O., Helbostad, J. L., Thingstad, P., Taraldsen, K., Prestmo, A., Lamb, S. E.,…Saltvedt, I. (2011). Effect of in-hospital comprehensive geriatric assessment (CGA) in older people with hip fracture. The protocol of the Trondheim Hip Fracture trial. BMC Geriatrics, 11, 18. doi:10.1186/1471-2318-11-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolee, P., Awad, M., Byrne, K., Deforge, R., Clements, S., & Glenny, C.; Day Hospital Goal Attainment Scaling Interest Group of the Regional Geriatric Programs of Ontario . (2012). A multi-site study of the feasibility and clinical utility of Goal Attainment Scaling in geriatric day hospitals. Disability and Rehabilitation, 34, 1716–1726. doi:10.3109/09638288.2012.660600 [DOI] [PubMed] [Google Scholar]
- Stotter, A., Reed, M. W., Gray, L. J., Moore, N., & Robinson, T. G. (2015). Comprehensive Geriatric Assessment and predicted 3-year survival in treatment planning for frail patients with early breast cancer. The British Journal of Surgery, 102, 525–33; discussion 533. doi:10.1002/bjs.9755 [DOI] [PubMed] [Google Scholar]
- Sutherland, H. J., & Till, J. E. (1993). Quality of life assessments and levels of decision making: Differentiating objectives. Quality of Life Research, 2, 297–303. doi:10.1007/bf00434801 [DOI] [PubMed] [Google Scholar]
- The Health Foundation . (2013). Improving patient flow: How two trusts focused on flow to improve the quality of care and use available capacity effectively. Retrieved from www.health.org.uk/publications/improving-patient-flow/. Accessed December 20, 2019.
- Walker, S., Andrew, S., Hodson, M., & Roberts, C. M. (2017). Stage 1 development of a patient-reported experience measure (PREM) for chronic obstructive pulmonary disease (COPD). NPJ Primary Care Respiratory Medicine, 27, 47. doi:10.1038/s41533-017-0047-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe, S. M., Nekolaichuk, C., Beaumont, C., Johnson, L., Myers, J., & Strasser, F. (2011). A multicenter study comparing two numerical versions of the Edmonton Symptom Assessment System in palliative care patients. Journal of Pain and Symptom Management, 41, 456–468. doi:10.1016/j.jpainsymman.2010.04.020 [DOI] [PubMed] [Google Scholar]
- Watson, A., Charlesworth, L., Jacob, R., Kendrick, D., Logan, P., Marshall, F.,…Sahota, O. (2015). The Community In-Reach and Care Transition (CIRACT) clinical and cost-effectiveness study: Study protocol for a randomised controlled trial. Trials, 16, 41. doi:10.1186/s13063-015-0551-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, G., Greenhalgh, T., Westhorp, G., Buckingham, J., & Pawson, R. (2013). RAMESES publication standards: Meta-narrative reviews. BMC Medicine, 11(1), 20. doi:10.1186/ 1741-7015-11-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.