Abstract
Background and Objectives
Greater everyday decision-making involvement by persons living with dementia (PLWD) and congruent appraisal between PLWDs and their caregivers have been associated with a better quality of life (QOL) for both members of the dyad. However, no study has examined the association between the appraisals of everyday decision-making involvement of PLWDs and their QOL among African Americans.
Research Design and Methods
A secondary analysis of cross-sectional data from 62 African American dementia dyads was conducted. Multilevel and latent class mixture modeling was used to characterize dyadic appraisal of the decision-making involvement of African American PLWDs and identify distinct patterns thereof.
Results
Three distinct patterns were observed. “Incongruent, PLWD Low Involvement” labeled 19.4% of the sample, 53.2% were labeled “Incongruent, PLWD Moderate Involvement,” and 27.4% were labeled “Congruent, PLWD High Involvement.” The Congruent, PLWD High Involvement pattern consisted of PLWDs who were significantly younger and had significantly less cognitive impairment than PLWDs in the other patterns. In the Incongruent, PLWD Moderate Involvement pattern, PLWDs had significantly better QOL than PLWDs in the Incongruent, PLWD Low Involvement pattern, but QOL did not significantly differ from PLWDs in the Congruent, PLWD High Involvement pattern.
Discussion and Implications
There is a need to tailor strategies to optimize QOL in African American dementia dyads. While increasing everyday decision-making involvement for PLWDs in the Incongruent, PLWD Low Involvement pattern is an important goal, other strategies may be needed to improve the QOL of PLWDs in the remaining patterns.
Keywords: Alzheimer’s disease, Informal caregiving, Quality of life
In the United States, African American older adults are twice as likely to develop Alzheimer’s disease and other dementias compared to non-Hispanic white older adults (Alzheimer’s Association, 2020; Ortman et al., 2014). African American older adults also are diagnosed at later stages of dementia, resulting in greater morbidity (Chin et al., 2011). Despite the disproportionately high risk of developing dementia in African American older adults, little is known about how African American dementia dyads (i.e., African American persons living with dementia [PLWD] and their African American caregivers) manage everyday decision making or the influence this decision making has on their quality of life (QOL). Many everyday decisions are made by PLWDs or on their behalf, such as what to eat and what clothes to wear (Fetherstonhaugh et al., 2013; Menne & Whitlatch, 2007; Menne et al., 2008). Understanding how involved PLWDs are in these everyday decisions and the level of (in)congruence regarding this involvement within the dyads can provide greater insight into dementia caregiving.
For more than a decade, dementia research has increasingly focused on the dementia dyad—moving away from sole reliance on proxy reports of caregivers alone (Lyons et al., 2002; Martire et al., 2010). Expanding research efforts to include the PLWD acknowledges the dual nature of both members of the dyad in the caregiving process (Kitwood, 1997). A family-centered approach is important as African American decision making is often family-based (Potter et al., 2017). While African Americans may be viewed as a single racial group, there is heterogeneity in their family structure and practices (Billingsley, 1988), which may influence everyday decision making. Dilworth-Anderson et al. (1999) identified caregiver types and structures within African American families. Primary caregivers were characterized as either providing care alone or with the help of other family members and were most involved with decision making (Dilworth-Anderson et al., 1999). Yet decision-making involvement (e.g., verbal and nonverbal communication) has been minimally studied within African American dementia dyads of primary caregivers and PLWDs (Bonds et al., 2020).
To date, we know that PLWDs desire greater involvement in everyday activities (Clark et al., 2008) and treatment decision making (Hirschman et al., 2005) but have been prematurely removed from involvement in both types of decisions often related to the concerns of their decision-making capacity (Miller et al., 2016). Moving beyond decision-making capacity to decision-making involvement may prove beneficial for both members of dementia dyads, particularly as it is a more strength-based approach and aligns strongly with person-centered care. Indeed, greater perceived decision-making involvement by PLWDs has been associated with better QOL for PLWDs (Menne et al., 2009) and their caregivers (Menne et al., 2008), although Menne et al. (2009) also found that PLWDs who self-identified as African American experienced worse QOL.
Research suggests when members of care dyads are “on the same page” or have congruent appraisals they are more likely to work together as a team to meet the needs of both members of the dyad and thereby improve the well-being of the dyad (Lyons & Lee, 2018; Merz et al., 2011; Moon et al., 2017). However, incongruent appraisal of phenomena within dyads—either dementia dyads or couples—has been negatively associated with the well-being and self-management of the members of dyads (Lyons & Lee, 2018). Moon et al. (2017) found when dementia dyad members had incongruent appraisal regarding the care values of PLWDs both PLWDs and their caregivers experienced significantly worse QOL. When spouses/partners of persons with prostate cancer had an incongruent appraisal of the characteristics of prostate cancer, this incongruence was significantly associated with worse health-related QOL for those couples (Merz et al., 2011).
The current study is informed by the Negro Family as a Social System conceptual framework (Billingsley, 1988) to optimize QOL for both members of African American dementia dyads. According to this conceptual framework, better outcomes and well-being are associated with interpersonal factors of the family (Billingsley, 1988) or a smaller unit of the family—the dyad (Bonds et al., 2020). These factors include family structure, instrumental role functions, and expressive role functions. Family structure consists of dyadic relationships of members of the family (e.g., mother–daughter, father–son), in this case, the type of relationship of members of the dementia dyads (i.e., spouse dyads or nonspouse dyads). Instrumental role functions are described by managing the family affairs through obtaining education, decision making, economic resources, and health management (i.e., caregiver’s educational status and PLWD cognitive status are proxies of instrumental role functions). Expressive role functions include a sense of belonging, emotional support, and feelings (i.e., dyadic relationship quality). The quality of the family structure and the extent to which needs are met based on the instrumental and expressive role functions can influence the outcomes (i.e., QOL) of African American dementia dyads differently (Billingsley, 1988; Bonds et al., 2020).
Pattern identification across dyads has been identified in PLWDs (Miller et al., 2018) and other chronic conditions such as persons diagnosed with heart failure (Lee et al., 2015, 2017) and lung cancer (Lee & Lyons, 2019). Identifying patterns of African American dementia dyads with different PLWD decision-making involvement can lead to the creation of tailored interventions to improve health outcomes and foster family-centered care. Given the importance of decision-making involvement of PLWDs and the interdependent nature of African American families, understanding patterns at greater risk for worse QOL can highlight strategies to improve decision making for care planning while caregiving.
The purpose of this study was to (a) identify and characterize patterns of dyadic appraisal regarding decision-making involvement by PLWDs within African American dementia dyads and (b) determine whether membership in the observed patterns was associated with the PLWD and caregiver QOL. Our hypotheses were as follows: (a) at least two distinct patterns of appraisal of African American PLWDs decision-making involvement would be identified, (b) dyads in a pattern with a higher dyadic appraisal of African American PLWD decision-making involvement would have better QOL for both members, and (c) dyads with more congruent appraisal would have better QOL for both members.
Design and Methods
A secondary data analysis of 62 African American dementia dyads was conducted using cross-sectional data from a prior study collected between 1998 and 2004 examining 202 caregiving dementia dyads—71 African American dyads and 131 non-Hispanic white dyads (Powers & Whitlatch, 2016). Dyads were recruited from Cleveland, OH and San Francisco Bay area, CA. Dyads in the original study were eligible for participation if (a) both members lived in the community, (b) caregivers were primary caregivers for the PLWDs, and (c) PLWDs had a formal diagnosis of dementia or scored 13–26 on the Mini-Mental State Examination. More in-depth recruitment details are presented elsewhere (Feinberg & Whitlatch, 2001). In the current study, PLWDs and their caregivers were required to self-identify as African American and have no missing data on the outcome measures and other study variables. Informed consent was obtained by each member of the dyad in the original study. The current study was approved by the Oregon Health & Science University’s institutional review board.
Outcome Measures
Decision-making involvement
Decision-making involvement of the PLWD was measured using the Decision-Making Involvement Scale developed for persons with mild to moderate dementia (Menne et al., 2008). The Decision-Making Involvement Scale is a 15-item scale, scored using a four-point Likert scale of 0 (Not Involved at All) to 3 (Very Involved). The caregiver version ascertains the caregiver’s appraisal of the PLWD’s involvement in decision making. A sample item is “How involved are you in decisions about what to spend your money on?” (PLWD version) or “How involved is your relative in decisions about what to spend his/her money on?” (Caregiver version). Responses are averaged resulting in a mean score between 0 and 3, with higher scores indicating greater decision-making involvement. The measure had strong interitem reliability using Cronbach’s alpha in the current sample (PLWD α = 0.86; Caregiver α = 0.94).
Quality of life
QOL of PLWDs and their caregivers was measured using the Quality of Life–Alzheimer’s Disease Scale developed for persons with mild to moderate dementia (Logsdon et al., 1999). The Quality of Life–Alzheimer’s Disease Scale is a 13-item, four-point Likert scale. Both PLWDs and caregivers rated the perception of their own QOL (Logsdon et al., 2002; Moon et al., 2017). A sample question is “How do you feel about your energy level?” Responses are from 1 (Poor) to 4 (Excellent). Responses are summed resulting in a total score between 13 and 52, with higher scores indicating better QOL. The measure demonstrated strong inter-item reliability in the current sample (PLWD α = 0.82; Caregiver α = 0.89).
Independent Variables
Demographic characteristics
The characteristics that were available in the original study and fit within the conceptual framework are age, gender, marital status, educational level, annual household income, and formal diagnosis of dementia (yes/no). These variables provided a way to characterize the patterns.
Cognitive impairment
Cognitive impairment of the PLWD was measured using the Mini-Mental State Examination. The Mini-Mental State Examination is an 11-item cognitive examination used to evaluate cognitive impairment spanning aspects of working memory, orientation, language, and delayed recall (Folstein et al., 1975). The total score ranges from 0 to 30, with a lower score signifying greater cognitive impairment. The scale demonstrated fair inter-item reliability in our sample (α = 0.54). With a cutoff score of 24, the Mini-Mental State Examination has a sensitivity of 70% and specificity of 93% in older adults (Baker et al., 1993).
Family structure
Family structure was examined based on the self-report of caregivers. The type of relationship of caregivers was identified as spouses or nonspouses.
Expressive role functions
Expressive role functions were examined using the Dyadic Relationship Scale (Sebern & Whitlatch, 2007), which was created to provide insight from both patient and caregiver (Sebern & Whitlatch, 2007). The Dyadic Relationship Scale has two subscales—Dyadic Strain and Positive Interaction. The Dyadic Strain subscale is a four-item measure for the PLWD and a five-item measure for the caregiver. An example item is “Because of my memory problems, I felt depressed when I had problems with my relationship with my caregiver” (PLWD version) or “Because of helping the PLWD, I felt depressed because of my relationship with her/him” (Caregiver version). The responses are rated from 0 (Strongly Disagree) to 3 (Strongly Agree). Responses are averaged resulting in a mean score between 0 and 3, with higher scores indicating greater strain within the dyad. The subscale demonstrated good interitem reliability in our sample (PLWD, α = 0.70; Caregiver, α = 0.78).
The six-item positive interaction subscale of the Dyadic Relationship Scale (Sebern & Whitlatch, 2007) was used to measure the positive interaction of the dyadic relationship quality by both PLWDs and caregivers. An example item is “Because of my memory problems, I felt closer to her/him than I have in a while” (PLWD version) or “Because of helping the PLWD, I felt closer to her/him than I have in a while” (Caregiver version). The responses are rated from 0 (Strongly Disagree) to 3 (Strongly Agree). Responses are averaged resulting in a mean score between 0 and 3, with higher scores indicating greater positive interaction. The subscale demonstrated good interitem reliability in our sample (PLWD, α = 0.68; Caregiver, α = 0.84).
Analytic Approach
Multilevel modeling
Dyadic data were analyzed using multilevel modeling resulting in empirical Bayes estimates of incongruence (i.e., gap between dyad members’ appraisal of PLWD decision-making involvement) and dyadic averages (i.e., average appraisal within the dyad) using the software program Hierarchical Linear Modeling, version 7 (Raudenbush et al., 2011). Multilevel modeling is a comprehensive approach used to examine incongruence and dyadic averages while controlling for measurement error and the interdependence within the dyads and has been used to examine incongruence between the PLWD and their caregiver in previous studies (Lyons et al., 2002; Miller et al., 2017; Moon et al., 2017; Reamy et al., 2011).
An unconditional Level 2 model, Yij = β 0j + β 1j (Dyadij) + rij, was used in the multilevel modeling analysis. Yij represents decision-making involvement of PLWDs i in dyad j. We coded the African American PLWD as −0.5 and the African American caregiver as 0.5 in the dyad (Dyadij). β 0j is the intercept and represents the dyadic average of PLWDs’ decision-making involvement plus measurement error (rij). β 1j is the slope and represents the incongruence between dyadic appraisals by PLWDs and caregivers regarding the decision-making involvement of PLWDs. The Hierarchical Linear Modeling program generated empirical Bayes estimates of the appraisal of decision-making involvement of PLWDs for each dyad that were used to identify potential patterns.
Latent class mixture modeling
Distinct and naturally occurring patterns were identified using latent class mixture modeling in Mplus, version 8 (Los Angeles, CA). Latent class mixture modeling uncovers unidentified heterogeneity among dyads, resulting in patterns. Empirical Bayes estimates of incongruence and dyadic average in the appraisal of PLWD decision-making involvement were included in our analysis (Lee et al., 2015). Model convergence (entropy near 1.0), size of observed classifications (5% or greater of the sample), average posterior probabilities (near 1.0), and significance of the parametric bootstrap likelihood ratio test and Lo–Mendell–Rubin adjusted likelihood ratio test (Lo et al., 2001) were used to examine the performance of other classifications (e.g., two classes vs. three; Ram & Grimm, 2009). Observed patterns were named based on the two results of multilevel modeling: incongruence (i.e., congruent or incongruent) and dyadic averages (i.e., low, moderate, or high).
Descriptive and comparative statistics were conducted using the software package StataIC, version 14 (StataCorp, 2015) to describe the overall participant characteristics. We compared observed patterns using analysis of variance and χ 2 and calculated effect size comparisons using Hedge’s g and Cramer’s V, respectively.
Results
African American PLWDs in the study were on average 77 ± 8 years old, with the majority widowed (48%), female (68%), having received a dementia diagnosis from a provider (76%), an Mini-Mental State Examination score of 21 ± 4 (reflecting mild dementia symptoms), and about one fourth had greater than a high school education (23%). African American caregivers were 15 years younger on average, were predominantly female (81%), married (60%), mostly nonspouse caregivers (69%), with greater than high school education (56%), and a half (50%) had annual household incomes of greater than or equal to $30,000. Table 1 displays additional sample characteristics.
Table 1.
African American Dementia Dyad Characteristics and Differences Among Patterns (ANOVA, χ 2)
| Characteristics (± SD or %) | Overall sample (N = 62) | Incongruent, PLWD Low Involvement (n = 12) | Incongruent, PLWD Moderate Involvement (n = 33) | Congruent, PLWD High Involvement (n = 17) | p Value | Effect size |
|---|---|---|---|---|---|---|
| PLWD age in years | 76.55 ± 7.84 | 78.75 ± 8.08a | 77.85 ± 6.81b | 71.93 ± 8.43a,b | .067a, .042b | 0.39 |
| CG age in years | 60.50 ± 13.35 | 56.83 ± 8.72a,c | 62.79 ± 12.82a,b | 58.64 ± 16.57b,c | .570a, .902b, 1.00c | 0.33 |
| PLWD female | 42 (68%) | 9 (75%) | 19 (58%) | 14 (82%) | .190 | 0.24 |
| CG female | 50 (81%) | 11 (92%) | 27 (82%) | 12 (71%) | .426 | 0.18 |
| PLWD married/ partnered | 21 (34%) | 1 (8%) | 17 (52%) | 3 (18%) | .029 | 0.29 |
| CG married/ partnered | 37 (60%) | 3 (25%) | 26 (79%) | 8 (47%) | .004 | 0.37 |
| PLWD living with CG | 40 (65%) | 8 (67%) | 25 (75%) | 7 (41%) | <.001 | 0.50 |
| Family structure | ||||||
| Type of CG, spouse/ partnerd | 19 (31%) | 1 (8%) | 14 (42%) | 4 (24%) | .078 | 0.30 |
| Instrumental role functions | ||||||
| PLWD greater than HS | 14 (23%) | 1 (8%) | 9 (27%) | 4 (24%) | .458 | 0.16 |
| CG greater than HS | 35 (56%) | 5 (42%) | 21 (64%) | 9 (53%) | .431 | 0.17 |
| PLWD MMSE score | 21.08 ± 3.94 | 18.33 ± 3.21a | 20.65 ± 3.74b | 23.86 ± 3.16a,b | <.001 a, .010b | 0.13 |
| Income,e ≥$30K/year | 31 (50%) | 4 (33%) | 21 (64%) | 6 (35%) | .029 | 0.36 |
| Expressive role functions | ||||||
| PLWD dyadic strain | 0.84 ± 0.57 | 0.92 ± 0.46 | 0.84 ± 0.65 | 0.79 ± 0.51 | 1.00 | 0.02 |
| CG dyadic strain | 1.01 ± 0.47 | 1.15 ± 0.39a,b | 1.04 ± 0.55a,c | 0.87 ± 0.33b,c | 1.00a, .366b, .733c | 0.06 |
| PLWD POS interaction | 2.14 ± 0.52 | 2.06 ± 0.62 | 2.17 ± 0.56 | 2.15 ± 0.40 | 1.00 | 0.13 |
| CG POS interaction | 1.88 ± 0.54 | 1.71 ± 0.38a,b | 1.95 ± 0.62a,c | 1.88 ± 0.49b,c | .608a, 1.00b,c | 0.30 |
| Outcome | ||||||
| PLWD QOL | 34.34 ± 5.80 | 31.25 ± 4.71a | 35.94 ± 6.33a | 33.41 ± 4.42 | .047 a | 0.60 |
| CG QOL | 37.41 ± 6.34 | 35.33 ± 6.88a,b | 38.73 ± 6.17ba,c | 36.25 ± 6.04b,c | .342a, 1.00b, .601c | 0.46 |
Note: ANOVA = analysis of variance; CG = caregiver; HS = high school; MMSE = Mini-Mental State Examination; PLWD = person living with dementia; POS = positive; QOL = quality of life; SD = standard deviation. p Value = ANOVA with Bonferroni correction and chi-square with Fischer’s exact test. Effect size = Hedge’s g (small = 0.2, medium = 0.5, and large = 0.8) and Cramer’s V (small = 0.1, medium = 0.3, and large = 0.5). Bold values indicate p values <.05.
a b,cWithin a row, difference between means without a common superscript.
dSpouse is the referent.
eHousehold income.
Dyadic Appraisal of Decision-Making Involvement
There was significant variability in the amount of incongruence (χ 2 = 489.48, p < .001) and the dyadic averages (χ 2 = 1152.98, p < .001) across African American dementia dyads regarding decision-making involvement of PLWDs. On average, PLWDs rated their decision-making involvement higher than their caregivers. The multilevel modeling analysis confirmed the heterogeneity within the data. The data could be better understood by examining whether subgroups of dyads belong to distinct patterns.
Patterns of Decision-Making Involvement of African American PLWDs
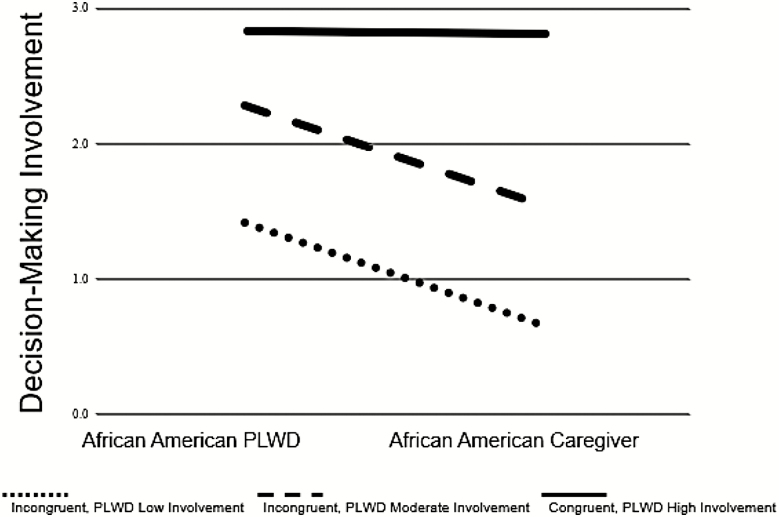
Three distinct patterns of dyadic appraisal of decision-making involvement of PLWDs were identified, supporting our first hypothesis. The model convergence (entropy = 0.954), size of observed patterns (greater than 5% of sample), posterior probabilities (>.980), parametric bootstrap likelihood ratio test (−135.683, p < .001), and Lo–Mendell–Rubin adjusted likelihood ratio test (16.95, p = .031) all represented good model fit. Table 2 provides the differences in dyadic appraisal by patterns; Figure 1 visually illustrates the differences.
Table 2.
Differences of Patterns Appraisal of Decision-Making Involvement by the African American PLWD
| Incongruent, PLWD Low Involvement (n = 12) ± SD | Incongruent, PLWD Moderate Involvement (n = 33) ± SD | Congruent, PLWD High Involvement (n = 17) ± SD | p Value (t test) | Effect size (Hedge’s g) | |
|---|---|---|---|---|---|
| Decision-making involvement | |||||
| Incongruence | −0.75 ± 0.31 | −0.77 ± 0.15 | −0.03 ± 0.10 | .008 | 0.51 |
| Dyadic average | 0.98 ± 0.07 | 1.87 ± 0.04 | 2.81 ± 0.05 | <.001 | 0.23 |
Notes: PLWD = person living with dementia; SD = standard deviation. Incongruence and average scores are empirical Bayes estimates from multilevel modeling which controls for the interdependent nature of the data and corrects measurement error. Negative incongruence scores signify PLWDs rated their decision-making involvement higher than their caregivers. Positive incongruence scores signify PLWDs rated their decision-making involvement lower than their caregivers. A score of 0 indicates congruence or no incongruence. Incongruent, PLWD Moderate Involvement pattern is a referent for Hedge’s g.
Figure 1.
Distinct patterns of dyadic appraisal of decision-making involvement by African American PLWDs. The level illustrates the average decision-making involvement (range 0–3) of PLWDs by PLWDs and their caregivers. The incongruence or slope of each line illustrates the differences of the appraisals of decision-making involvement between both members of African American dementia dyads. PLWD = person living with dementia.
Patterns were labeled based on the dominant characteristics of incongruence and dyadic averages. Dyads were labeled as “Incongruent, PLWD Low Involvement” (19.4%) because PLWDs and their caregivers reported significant incongruence and lower dyadic averages of decision making by PLWDs. Dyads were labeled as “Incongruent, PLWD Moderate Involvement” (53.2%) because PLWDs and their caregivers reported significant incongruence and midlevel dyadic averages. Lastly, dyads were labeled as “Congruent, PLWD High Involvement” (27.4%) because of statistically nonsignificant incongruence and significantly higher dyadic averages. Unadjusted characteristics based on family structure, instrumental role functions, and expressive role functions are provided by each observed pattern and presented in Table 1.
Group membership was significantly associated (p < .05) with the age of PLWDs, whether the PLWD lived with their caregiver, the Mini-Mental State Examination score of PLWDs, the household income of caregivers, and the marital status of both PLWDs and their caregivers. Older PLWDs were significantly more likely to be in the Incongruent, PLWD Low Involvement or Incongruent, PLWD Moderate Involvement patterns. In the Congruent, PLWD High Involvement pattern, PLWDs were more likely to live alone and to have higher Mini-Mental State Examination scores. In the Incongruent, PLWD Moderate Involvement pattern, PLWDs and caregivers were significantly more likely to be married/partnered and caregivers were more likely to have higher household incomes. Additionally, there was a small effect size for the age of PLWDs, the Mini-Mental State Examination score of PLWDs, the household income of caregivers, and the marital status of both PLWDs and caregivers. There was a large effect size for the living arrangements of PLWDs.
There was a significant difference and a moderate effect size for the QOL experienced by PLWDs. In the Incongruent, PLWD Moderate Involvement pattern, PLWDs experienced significantly better QOL compared to the PLWDs in the Incongruent, PLWD Low Involvement pattern, which partially supported our second hypothesis. In the Congruent, PLWD High Involvement pattern, PLWDs did not significantly differ from PLWDs in either the Incongruent, PLWD Moderate Involvement pattern or the Incongruent, PLWD Low Involvement pattern, which did not support our third hypothesis. Although there was no significant difference experienced in QOL of caregivers by group membership, there was a moderate effect size.
Discussion
This study examined dyadic appraisal of decision-making involvement of PLWDs in 62 African American dementia dyads. To the best of our knowledge, this is the first study to identify patterns of dyadic appraisal of decision-making involvement among African American dementia dyads and examine the association between these distinct patterns of dyadic appraisal with other variables. Dementia research has acknowledged the importance of heterogeneity between cultures when examining health outcomes among different racial/ethnic groups (Chin et al., 2011). However, one area of heterogeneity that has been examined less is the variability of culture within African American families. The identification of three patterns based on PLWDs’ decision-making involvement begins to elucidate the heterogeneity within family culture. Billingsley (1988) describes African American families as groups of people with a shared history who are often characterized as one monolithic group despite variability in conditions, personalities, and behaviors. Thus, we view African American families as members of one racial group with multiple dyads and family-based preferences and customs. Understanding the heterogeneity within and across these dementia dyads may hold promise for developing tailored interventions in clinical and research settings. Nurses in inpatient and outpatient settings spend a considerable amount of time with patients and may benefit from understanding that heterogeneity exists within African American dementia dyads regarding the PLWD’s decision-making involvement. Our findings highlight both similarities and differences from previous research. African American caregivers in the three patterns did not experience significantly different QOL. Moon et al. (2017) found incongruence in decision-making involvement was not significantly associated with QOL in caregivers or PLWDs. In contrast, while our findings for African American caregivers are similar, the findings are divergent for African American PLWDs. Lindauer et al. (2016) found African American caregivers worked to keep African American PLWDs present in activities. This present focus by African American caregivers could be an attempt to encourage African American PLWDs to be involved in everyday decision making. As a result, when African American caregivers are unable to uphold the involvement in decision making of African American PLWDs, African American PLWDs’ QOL is negatively affected.
Over half of the sample was described as the Incongruent, PLWD Moderate Involvement pattern in which dyads tended to include PLWDs with midlevel Mini-Mental State Examination scores and significantly better QOL than PLWDs in the Incongruent, PLWD Low Involvement pattern. Yet within the two incongruent patterns, dyadic appraisal of decision-making involvement of PLWDs plays a greater role in predicting QOL. Because dyadic appraisal of the PLWD’s decision-making involvement was similar between these two groups, QOL did not differ between PLWDs in the Incongruent, PLWD Moderate Involvement pattern and the Congruent, PLWD High Involvement pattern. In contrast, QOL did not differ between PLWDs in the Congruent, PLWD High Involvement pattern and the Incongruent, PLWD Low Involvement pattern because their QOL may be similar given their respective stages of Alzheimer’s disease and related dementias. Based on the tenet of the Negro Family as a Social System that African American communities consist of a racial/ethnic subsociety with much variability, we speculate the reason for these findings are related to the family structure, instrumental and/or expressive role functions within the dyads in these three patterns.
Better QOL has been associated with higher Mini-Mental State Examination scores (Miller et al., 2016, 2017) and greater decision-making involvement by PLWDs (Bonds et al., 2020; Menne et al., 2008). In addition, Bonds et al. (2020) found that in African American dementia dyads having a spouse caregiver was associated with better QOL for PLWDs. In the Congruent, PLWD High Involvement pattern, PLWDs had Mini-Mental State Examination scores reflecting on average mild dementia symptoms and congruent dyadic appraisal of the decision-making involvement of PLWDs. Compared to the other PLWDs, PLWDs in the Congruent, PLWD High Involvement pattern still lived alone. Persons with mild dementia symptoms can often still function at home alone where they are the primary decision maker. The majority of PLWDs in the other two patterns were already living with their caregivers.
In this study and in previous research (Menne et al., 2008), the incongruence within the dyads was a result of caregivers underestimating the level of decision-making involvement of PLWDs or PLWDs overestimating their decision-making involvement. We prefer to focus on how they disagree, how much they disagree, and the implications associated with the disagreement. This focus is less on valuing the perception of one member of the dyad over the other and more about focusing on the dyad as a unit.
Many of the decisions examined on the Decision-Making Involvement Scale are decisions that many African American older adults have been involved in for years with minimal or no input from other members of the household. Yet as the disease trajectory continues these dyads will have to determine ways to support decision-making involvement in PLWDs. Piiparinen and Whitlatch (2011) described existential loss in relation to how caregivers navigate caregiving for PLWDs. Given the role many African American older adults have in the family prior to a dementia diagnosis, there may be more existential loss experienced by African American PLWDs in the mild-to-moderate stages. This loss may be why their QOL and not the QOL of African American caregivers was significant in our findings. The authors recommend that caregivers view the PLWD in a humanistic way considering their personhood and not the losses experienced during the dementia trajectory (Piiparinen & Whitlatch, 2011). This approach is demonstrated in a qualitative study of African American caregivers, which found these caregivers described the African American PLWDs as “changed, but still here” (Lindauer et al., 2016). African American caregivers decided to focus on the characteristics that were still present instead of focusing on what was lost during the dementia trajectory (Lindauer et al., 2016). Because the change in family roles and decision making is inevitable as the dementia trajectory continues, strategies to support the dyad to a larger degree during the mild-to-moderate stages are necessary. One way to support African American dementia dyads and begin to tailor interventions to optimize their QOL is to support decision-making involvement of PLWDs. Fetherstonhaugh et al. (2013) found the “essence of decision making” through interviews of PLWDs, which may be helpful now for PLWDs in the Incongruent, PLWD Low Involvement pattern and for future care planning with PLWDs in the Congruent, PLWD High Involvement pattern. The essence of decision making is described by three conflicting characteristics between PLWDs and their caregivers—“subtle support versus taking over,” “hanging on versus letting go,” and “being central versus being marginalized or excluded” (Fetherstonhaugh et al., 2013). Subtle support was described by PLWDs as feeling comfortable and involved in decision making with their caregiver providing backup when needed (Fetherstonhaugh et al., 2013). PLWDs described hanging on as the awareness that they would have to relinquish some decision-making involvement in one area (e.g., driving) but could still make decisions in another area (e.g., cleaning; Fetherstonhaugh et al., 2013). Being central to decision making meant PLWDs were consulted and not insignificant (Fetherstonhaugh et al., 2013). For example, if an African American PLWD was the primary homemaker for her/his family, decisions around what to eat may be a way to incorporate the essence of decision making. The goal is to tailor decision-making involvement to the African American PLWDs’ specific needs to optimize their QOL.
Limitations
There are limitations to note in this study. First, the sample size is relatively small. Although our sample size is comparable to another study in which latent class mixture modeling was conducted (Lee et al., 2017), these results should be interpreted with caution. Although we detected several differences between the patterns, future work is needed to understand the mechanisms underlying these observed differences. Second, the study used a cross-sectional design limiting our ability to see if group memberships change over time and how group memberships will influence outcomes over time. Larger and more diverse longitudinal studies are warranted to improve our analysis. Third, we only examined one outcome associated with group membership. There are other variables beyond QOL that are critical to understanding dementia caregiving. Fourth, the Mini-Mental State Examination, which was used as a screening tool and not diagnostic, had relatively low reliability. Studies have identified concerns with the specificity and sensitivity of the Mini-Mental State Examination in screening African American older adults (Baker et al., 1993; Mast et al., 2001). Lastly, while the Decision-Making Involvement Scale and Dyadic Relationship Scale have been used in multiracial/ethnic samples, the measures have not been validated in entirely African American samples, which could influence internal consistency and content validity.
Strengths
There are several strengths noted in this study. This study is the first to examine the dyadic appraisal of decision-making involvement in African American dementia dyads. The analysis is novel in its emphasis on identifying patterns of dyadic appraisal of decision-making involvement of African American PLWDs and associating the patterns with QOL. Our results could be used to improve clinical interactions and support caregiving dyads. Caregiving is at least a dyadic process (Lyons et al., 2002), if not a family process within the African American population (Epps et al., 2019) in which including at least two perspectives is necessary.
Although decision making within African American families tends to be a shared experience (Potter et al., 2017), our study only highlights the significance of decision-making involvement by African American PLWDs. Future research should focus on the shared decision-making involvement, including African American PLWDs, their African American caregivers, and other family members when necessary. Decision-making involvement is modifiable and may provide a strategy for intervening to improve health outcomes for both members of African American dementia dyads. For example, the Support, Health, Activities, Resources, and Education is a counseling-based program that includes both PLWDs and their caregivers to help with care planning decision making, which focuses on the values and preferences of the PLWD (Whitlatch et al., 2006). Understanding different patterns that exist in African American dementia dyads could facilitate the tailoring of interventions based on the dyads’ appraisal of decision-making involvement of African American PLWDs.
Funding
This work was supported by the Jonas Veterans Healthcare Scholarship; Oregon Health & Science University School of Nursing Dean’s Alumni Scholarship; Oregon Health & Science University School of Nursing Pierce Scholarship; and Substance Abuse and Mental Health Service Administration at American Nurses Association [1H79SM080386-01]. The views expressed in written training materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. government. Partially funded through the National Institutes of Health National Institute of Nursing Research [2T32NR012715; PI: S. Dunbar] for trainee K. Bonds. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was supported by grants from The Robert Wood Johnson Foundation; The AARP Andrus Foundation; The Retirement Research Foundation; The National Institute of Aging [P50AG08012]; and The National Institute of Mental Health [R01070629 to C. J. Whitlatch].
Conflict of Interest
None declared.
References
- Alzheimer’s Association. (2020). 2020 Alzheimer’s disease facts and figures. Alzheimer’s and Dementia, 16(3), 391–460. doi: 10.1002/alz.12068 [DOI] [PubMed] [Google Scholar]
- Baker, F M, Robinson, B H, & Stewart, B. (1993). Use of the Mini-Mental State Examination in African American elders. Clinical Gerontologist 14(1), 5–13. doi: 10.1300/J018v14n01_02 [DOI] [Google Scholar]
- Billingsley, A. (1988). Black families in White America. Touchstone Books; (original work published in 1968). [Google Scholar]
- Bonds, K, Whitlatch, C J, Song, M, & Lyons, K S. (2020). Factors influencing quality of life in African-American dementia dyads. Aging and Mental Health. Advance online publication. doi: 10.1080/13607863.2020.1711865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin, A L, Negash, S, & Hamilton, R. (2011). Diversity and disparity in dementia: The impact of ethnoracial differences in Alzheimer disease. Alzheimer Disease and Associated Disorders, 25(3), 187–195. doi: 10.1097/WAD.0b013e318211c6c9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, P A, Tucke, S S, & Whitlatch, C J. (2008). Consistency of information from persons with dementia: An analysis of differences by question type. Dementia, 7(3), 341–358. doi: 10.1177/1471301208093288 [DOI] [Google Scholar]
- Dilworth-Anderson, P, Williams, S W, & Cooper, T. (1999). Family caregiving to elderly African Americans: Caregiver types and structures. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54(4), 237–241. doi: 10.1093/geronb/54b.4.s237 [DOI] [PubMed] [Google Scholar]
- Epps, F, Rose, K M, & Lopez, R P. (2019). Who’s your family?: African American caregivers of older adults with dementia. Research in Gerontological Nursing, 12(1), 20–26. doi: 10.3928/19404921-20181212-04 [DOI] [PubMed] [Google Scholar]
- Feinberg, L F, & Whitlatch, C J. (2001). Are persons with cognitive impairment able to state consistent choices? The Gerontologist, 41(3), 374–382. doi: 10.1093/geront/41.3.374 [DOI] [PubMed] [Google Scholar]
- Fetherstonhaugh, D, Tarzia, L, & Nay, R. (2013). Being central to decision making means I am still here!: The essence of decision making for people with dementia. Journal of Aging Studies, 27(2), 143–150. doi: 10.1016/j.jaging.2012.12.007 [DOI] [PubMed] [Google Scholar]
- Folstein, M F, Folstein, S E, & McHugh, P R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198. doi: 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Hirschman, K B, Joyce, C M, James, B D, Xie, S X, & Karlawish, J H. (2005). Do Alzheimer’s disease patients want to participate in a treatment decision, and would their caregivers let them? The Gerontologist, 45(3), 381–388. doi: 10.1093/geront/45.3.381 [DOI] [PubMed] [Google Scholar]
- Kitwood, T. (1997). The experience of dementia. Aging and Mental Health, 1(1), 13–22. doi: 10.1080/13607869757344 [DOI] [Google Scholar]
- Lee, C S, & Lyons, K S. (2019). Patterns, relevance, and predictors of dyadic mental health over time in lung cancer. Psycho-Oncology, 28(8), 1721–1727. doi: 10.1002/pon.5153 [DOI] [PubMed] [Google Scholar]
- Lee, C S, Mudd, J O, Auld, J, Gelow, J M, Hiatt, S O, Chien, C V, Bidwell, J T, & Lyons, K S. (2017). Patterns, relevance and predictors of heart failure dyadic symptom appraisal. European Journal of Cardiovascular Nursing, 16(7), 595–604. doi: 10.1177/1474515117700760 [DOI] [PubMed] [Google Scholar]
- Lee, C S, Vellone, E, Lyons, K S, Cocchieri, A, Bidwell, J T, D’Agostino, F, Hiatt, S O, Alvaro, R, Buck, H G, & Riegel, B. (2015). Patterns and predictors of patient and caregiver engagement in heart failure care: A multi-level dyadic study. International Journal of Nursing Studies, 52(2), 588–597. doi: 10.1016/j.ijnurstu.2014.11.005 [DOI] [PubMed] [Google Scholar]
- Lindauer, A, Harvath, T A, Berry, P H, & Wros, P. (2016). The meanings African American caregivers ascribe to dementia-related changes: The paradox of hanging on to loss. The Gerontologist, 56(4), 733–742. doi: 10.1093/geront/gnv023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo, Y, Mendell, N R, & Rubin, D B. (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. doi: 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- Logsdon, R G, Gibbons, L E, McCurry, S M, & Teri, L. (1999). Quality of life in Alzheimer’s disease: Patient and caregiver reports. Journal of Mental Health and Aging, 5(1), 21–32. [Google Scholar]
- Logsdon, R G, Gibbons, L E, McCurry, S M, & Teri, L. (2002). Assessing quality of life in older adults with cognitive impairment. Psychosomatic Medicine, 64(3), 510–519. doi: 10.1097/00006842-200205000-00016 [DOI] [PubMed] [Google Scholar]
- Lyons, K S, & Lee, C S. (2018). The theory of dyadic illness management. Journal of Family Nursing, 24(1), 8–28. doi: 10.1177/1074840717745669 [DOI] [PubMed] [Google Scholar]
- Lyons, K S, Zarit, S H, Sayer, A G, & Whitlatch, C J. (2002). Caregiving as a dyadic process: Perspectives from caregiver and receiver. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57(3), 195–204. doi: 10.1093/geronb/57.3.p195 [DOI] [PubMed] [Google Scholar]
- Martire, L M, Schulz, R, Helgeson, V S, Small, B J, & Saghafi, E M. (2010). Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine, 40(3), 325–342. doi: 10.1007/s12160-010-9216-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mast, B T, Fitzgerald, J, Steinberg, J, MacNeill, S E, & Lichtenberg, P A. (2001). Effective screening for Alzheimer’s disease among older African Americans. The Clinical Neuropsychologist, 15(2), 196–202. doi: 10.1076/clin.15.2.196.1892 [DOI] [PubMed] [Google Scholar]
- Menne, H L, Judge, K S, & Whitlatch, C J. (2009). Predictors of quality of life for individuals with dementia: Implications for intervention. Dementia, 8(4), 543–560. doi: 10.1177/1471301209350288 [DOI] [Google Scholar]
- Menne, H L, Tucke, S S, Whitlatch, C J, & Feinberg, L F. (2008). Decision-making involvement scale for individuals with dementia and family caregivers. American Journal of Alzheimer’s Disease and Other Dementias, 23(1), 23–29. doi: 10.1177/1533317507308312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menne, H L, & Whitlatch, C J. (2007). Decision-making involvement of individuals with dementia. The Gerontologist, 47(6), 810–819. doi: 10.1093/geront/47.6.810 [DOI] [PubMed] [Google Scholar]
- Merz, E L, Malcarne, V L, Ko, C M, Sadler, M, Kwack, L, Varni, J W, & Sadler, G R. (2011). Dyadic concordance among prostate cancer patients and their partners and health-related quality of life: Does it matter? Psychology & Health, 26(6), 651–666. doi: 10.1080/08870441003721251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, L M, Lee, C S, Whitlatch, C J, & Lyons, K S. (2017). Involvement of hospitalized persons with dementia in everyday decisions: A dyadic study. The Gerontologist, 58(4), 644–653. doi: 10.1093/geront/gnw265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, L M, Whitlatch, C J, Lee, C S, & Caserta, M S. (2018). Care values in dementia: Patterns of perception and incongruence among family care dyads. The Gerontologist, 59(3), 509–518. doi: 10.1093/geront/gny008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, L M, Whitlatch, C J, & Lyons, K S. (2016). Shared decision-making in dementia: A review of patient and family carer involvement. Dementia (London, England), 15(5), 1141–1157. doi: 10.1177/1471301214555542 [DOI] [PubMed] [Google Scholar]
- Moon, H, Townsend, A L, Whitlatch, C J, & Dilworth-Anderson, P. (2017). Quality of life for dementia caregiving dyads: Effects of incongruent perceptions of everyday care and values. The Gerontologist, 57(4), 657–666. doi: 10.1093/geront/gnw055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortman, J M, Velkoff, V A, & Hogan, H. (2014). An aging nation: The older population in the United States (P25-1140). http://www.census.gov/library/publications/2014/demo/p25-1140.html [Google Scholar]
- Piiparinen, R, & Whitlatch, C J. (2011). Existential loss as a determinant to well-being in the dementia caregiving dyad: A conceptual model. Dementia, 10(2), 185–201. doi: 10.1177/1471301211398989 [DOI] [Google Scholar]
- Potter, E C, Roberto, K A, Brossoie, N, & Blieszner, R. (2017). Decisions, decisions: African American families’ responses to mild cognitive impairment. Research on Aging, 39(4), 476–500. doi: 10.1177/0164027516655581 [DOI] [PubMed] [Google Scholar]
- Powers, S M, & Whitlatch, C J. (2016). Measuring cultural justifications for caregiving in African American and White caregivers. Dementia (London, England), 15(4), 629–645. doi: 10.1177/1471301214532112 [DOI] [PubMed] [Google Scholar]
- Ram, N, & Grimm, K J. (2009). Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. International Journal of Behavioral Development, 33(6), 565–576. doi: 10.1177/0165025409343765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reamy, A M, Kim, K, Zarit, S H, & Whitlatch, C J. (2011). Understanding discrepancy in perceptions of values: Individuals with mild to moderate dementia and their family caregivers. The Gerontologist, 51(4), 473–483. doi: 10.1093/geront/gnr010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebern, M D, & Whitlatch, C J. (2007). Dyadic relationship scale: A measure of the impact of the provision and receipt of family care. The Gerontologist, 47(6), 741–751. doi: 10.1093/geront/47.6.741 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2015). Stata Statistical Software: Release 14. [Computer software]. StataCorp. [Google Scholar]
- Whitlatch, C J, Judge, K, Zarit, S H, & Femia, E. (2006). Dyadic intervention for family caregivers and care receivers in early-stage dementia. The Gerontologist, 46(5), 688–694. doi: 10.1093/geront/46.5.688 [DOI] [PubMed] [Google Scholar]
- Raudenbush, S. W., Bryk, A. S., & Congdon, R. (2017). HLM 7.03 for Windows. Scientific Software International. [Google Scholar]