Summary
Background and objectives
High-angle Class II malocclusion is considered challenging to treat to a stable result and, although studies report treatment outcome in terms of morphology, patient satisfaction has not been addressed. The objectives of the present study were to examine patients’ motives for treatment and satisfaction with the results.
Material and methods
A structured questionnaire was distributed 3 years post-operatively to 93 consecutively treated patients with an initial diagnosis of mandibular-plane angle (ML/NSL) ≥34.0 degrees and ANB angle ≥4.0 degrees. Three surgical subsamples were defined: one-piece Le Fort I, bilateral sagittal split osteotomy, or a combination of the two (Bimax). Lateral cephalometric radiographs were used to assess morphological characteristics and post-treatment changes.
Results
Questionnaire participation was 69.8 per cent. The most frequently reported motives for seeking treatment were to improve oral function (85.0 per cent) and dental appearance (71.7 per cent). Thirty per cent were very satisfied, 53.3 per cent were satisfied, and 16.7 per cent were dissatisfied with the overall treatment result. Dissatisfaction was associated with a persisting post-treatment anterior open bite (AOB), horizontal relapse at B point, and with sensory impairment.
Conclusions and implications
A higher rate of dissatisfaction was found than what has usually been reported for othognathic surgical patients, and this was associated with a persisting AOB. In addition, mandibular relapse and impaired sensory function were related to dissatisfaction and are associated with mandibular surgery. Prospective high-angle Class II patients should be comprehensively informed about the unpredictability of treatment outcomes in terms of occlusion and facial appearance.
Introduction
An appraisal of patients’ opinions of treatment outcome is an important supplement to the clinical results when examining whether treatment meets the public’s expectations. Treatment, involving both orthodontic therapy and surgery, is comprehensive and demanding to the patient, uses considerable resources, and carries a risk of unwanted side effects. As treatment is elective, it is necessary to ensure that treatment results are according to patients’ needs.
A hierarchy of stability for surgical procedures has been established (1, 2) and mandibular advancement is known to have different relapse patterns depending on the vertical facial pattern (2–5). Despite these different patterns, many studies comprise of non-specific or mixed malocclusion samples (Class I, II, and III) or various surgical procedures, thus reporting a satisfaction rate for orthognathic surgical treatment in general. High rates of patients reporting satisfaction after mandibular advancement in Class II have been observed (6–9). However, a study of 516 orthognathic patients found that Class II patients were often dissatisfied with treatment and that mandibular advancement increased the risk for dissatisfaction (10). We have been unable to identify studies addressing patient satisfaction after surgical correction of high-angle Class II malocclusion.
The most common reasons reported for seeking orthognathic treatment are to improve biting or chewing (oral function), dental appearance, facial appearance, and to prevent future dental problems (9, 11–17). Motives have mainly been studied in unspecified or mixed malocclusion samples, but it is possible that patient motives also differ according to the type of malocclusion present (18). A feature often seen in skeletal high-angle Class II patients is an anterior open bite (AOB), which may cause functional problems.
Treatment that meets patients’ motives and expectations is associated with patient satisfaction, whereas factors such as prolonged treatment duration, post-treatment neurosensory impairment, and persisting temporomandibular pain (TMD) are likely to have a negative impact on overall satisfaction (16, 19). Self-completed patient questionnaires are tools that are available to try to understand patients’ subjective experiences (20, 21).
The purpose of the present study was to examine motivations for treatment and the rate of satisfaction/dissatisfaction among high-angle Class II patients 3 years after orthognathic surgery. Further objectives were to analyse the association between patient satisfaction and post-surgical skeletal relapse, different surgical approaches, and success or failure to correct an AOB.
Materials and methods
A 3 year follow-up questionnaire was distributed to consecutively treated high-angle Class II patients who had undergone a combination of orthodontic treatment and orthognathic surgery. The self-administered structured questionnaire was completed independently by patients at their final follow-up appointment in a separate room. At each question, patients could leave a comment if the answer alternatives did not apply or if they wished to elaborate on an answer. The questions addressed motivation for seeking treatment, perception of the treatment outcome, and sensory disturbances (Table 1).
Table 1.
Questionnaire with fixed alternative answers to patients at the 3 year follow-up visit, response alternatives in italics
| Q1. What was the reason for your decision to start treatment? |
| Not important at all/Not important/Somewhat important/Very important |
| a. Improve dental appearance |
| b. Improve facial appearance |
| c. Improve chewing ability |
| d. Improve speech |
| e. Other reasons (comments) |
| Q2. How would you describe the result of treatment? |
| Great improvement/Some improvement/No improvement/Worse |
| a. Dental appearance |
| b. Facial appearance |
| c. Chewing ability |
| d. Speech |
| e. Other (comments) |
| Q3. Are you satisfied with the result of treatment? |
| a. Very satisfied/Satisfied/Somewhat dissatisfied/Very dissatisfied |
| b. If you are dissatisfied, what is the reason? (comment) |
| Q4. With your current experience, would you have chosen this treatment again? |
| Yes, definitely/Yes, probably/No, probably not/No, definitely not |
| Q5. Have you experienced a change in sensation in your face/ lip/ gums? |
| a. Yes/No/Unsure |
| b. Comments |
Surgery took place at the Department of Maxillofacial Surgery at the Oslo University Hospital, Ullevål, between 1990 and 2014. All patients were seen by members of the Orthognathic team before, during, and after treatment. Orthodontic treatment was carried out by referring orthodontists in private practice or by post-graduate students at the Department of Orthodontics, University of Oslo.
To be included in the study there had to be an initial diagnosis of high-angle Class II malocclusion as defined by the mandibular-plane angle (ML/NSL) ≥34.0 degrees and the ANB angle ≥4.0 degrees (values equal to or higher than 1 standard deviation from the mean values obtained from the Oslo Growth Material) (22). A subsample was established of patients with AOB ≥0 mm.
Surgery had to be either a one-piece Le Fort I, a bilateral sagittal split osteotomy (BSSO), or a combination of the two (Bimax), which constitute the three surgical subsamples. Rigid fixation was used in all cases and all participants underwent orthodontic treatment. Another requirement was the availability of complete patient files, including lateral cephalometric radiographs of acceptable quality. Craniofacial syndromes, cleft-lip-palate anomalies or dentofacial trauma cases were excluded.
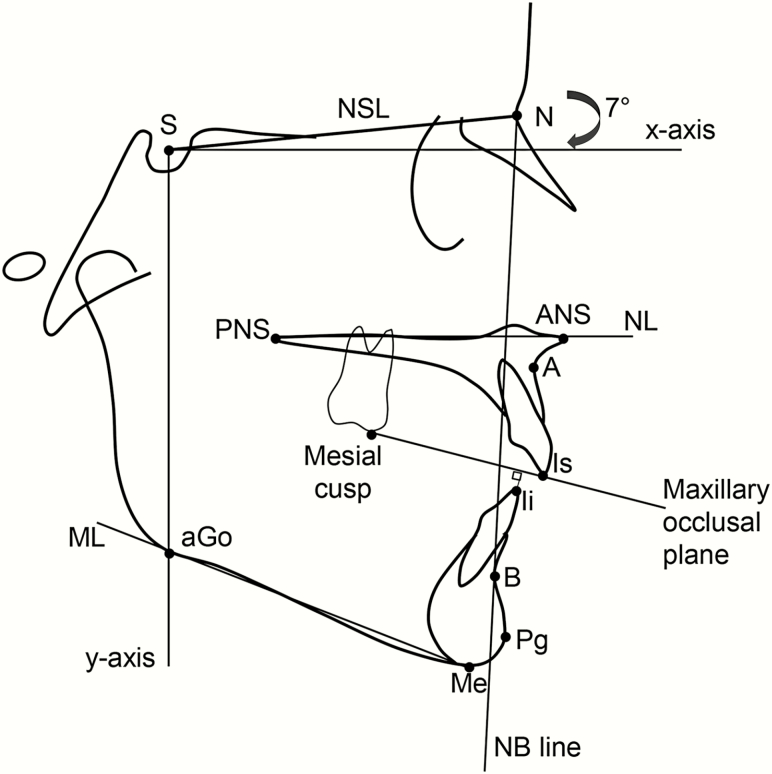
Lateral cephalometric radiographs were used for the assessment of morphological characteristics, treatment results, and changes. The Facad software (Ilexis AB, Linkõping, Sweden) was used for cephalometric analysis. Changes in dental and skeletal landmark positions were recorded using a coordinate system; the x-axis drawn 7.0 degrees below the nasion–sella line through sella and the y-axis, also passing through sella, was then drawn perpendicular to the x-axis. The x–y axes were transferred to each cephalogram by superimposition using the best fit of stable structures in the cranial base. Figure 1 shows the cephalometric landmarks and reference lines used. AOB was measured as the distance between the incisal edges perpendicular to the maxillary occlusal plane (23). The same examiner carried out all tracings and superimpositions (NT). Reproducibility of the cephalometric tracings was examined by duplicate tracings of 20 images, performed at least 2 weeks apart, with images chosen at random. For skeletal variables, clinically significant relapse was defined as changes greater or equal to 2 mm or 2 degrees.
Figure 1.
Landmarks, reference lines, and coordinate system used in the cephalometric analysis.
The study was reported to the Regional Ethical Committee (REC) but, as the aim of the study was to evaluate the quality of treatment patients had already received, the committee concluded that approval from REC was not necessary and had no objections to the study.
Descriptive statistical analysis was performed, results are presented in percentages or median with interquartile ranges (IQRs). Normality of continuous variables was analysed on histogram, -Q-Q plot, and by Shapiro–Wilk and Komologrov–Smirnov tests. Due to the low sample size and non-normal distribution of the continuous variables, Kruskal–Wallis analysis of variance was used to detect median differences of continuous variables and between the subsamples, and Fishers Exact test for the categorical variables. Eta squared (e2) was used to asses correlation between categorical and continuous data. Phi coefficient and Cramer’s V correlation were used to measure the strength of association between two categorical variables. Statistical analyses of the data were carried out in SPSS for Windows (SPSS, Chicago, Illinois, USA). The level of statistical significance was set to P value ≤0.05.
Results
Eighty-six patients fulfilled the inclusion criteria, and the questionnaire participation rate was 69.8 per cent (60 of 86). Thirteen participants were male (21.7 per cent) and 47 were female (78.3 per cent). The median age at surgery was 25.5 years. Twenty (33.3 per cent) individuals underwent a Le Fort I procedure only, 18 (30 per cent) underwent a BSSO procedure, and 22 (36.7 per cent) underwent bimaxillary surgery (Bimax). Fifty-one (85.0 per cent) of the patients had an AOB at T1 (pre-surgery) and constitute the AOB subsample.
Pre- and post-treatment cephalometric data of the total sample (n = 60) are shown in Table 2. The sample can generally be described as high-angle Class II with a retrognathic mandible, increased overjet, and often with an AOB. Pre- and post-treatment cephalometric data of the three surgical subsamples are shown in Table 3. Overall skeletal treatment changes were generally small from pre-surgery to 3 year follow-up in all subsamples (Tables 2 and 3). On average, there was an improvement in overbite and overjet.
Table 2.
Cephalometric characteristics of the total sample pre-surgery (T1) and at the 3 year follow-up (T5) [median (M) and interquartile range (IQR)]. ML/NSL, mandibular-plane angle
| Pre-surgery (T1) | 3 year follow-up (T5) | |||
|---|---|---|---|---|
| M | IQR | M | IQR | |
| Age (years) | 25.7 | (20.1, 29.2) | ||
| SNA | 78.6 | (76.4, 81.6) | 79.0 | (76.6, 81.9) |
| SNB | 70.9 | (69.4, 73.7) | 73.5 | (71.2, 75.5) |
| ANB | 7.0 | (5.9, 9.1) | 5.1 | (3.6, 7.3) |
| ML/NSL | 43.9 | (41.2, 46.5) | 42.5 | (40.4, 46.0) |
| Overjet (mm) | 6.6 | (4.4, 8.1) | 3.8 | (2.7, 4.9) |
| Overbite (mm) | −1.8 | (−2.9, −0.8) | 0.0 | (−0.6, 0.8) |
Table 3.
Cephalometric characteristics of the surgical subsamples at pre-surgery (T1) and at the 3 year follow-up (T5) [median (M) and interquartile range (IQR)]. BSSO, bilateral sagittal split osteotomy; ML/NSL, mandibular-plane angle
| Le Fort I | BSSO | Bimax | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 20 | n = 18 | n = 22 | ||||||||||||
| Pre-surgery (T1) | 3 year follow-up (T5) | Pre-surgery (T1) | 3 year follow-up (T5) | Pre-surgery (T1) | 3 year follow-up (T5) | P-value | ||||||||
| M | IQR | M | IQR | M | IQR | M | IQR | M | IQR | M | IQR | T1 | T5 | |
| Age (years) | 26.2 | (19.9, 29.5) | 26.8 | (21.0, 31.1) | 20.3 | (20.3, 27.3) | 0.5 | |||||||
| SNA | 78.6 | (76.7, 81.7) | 78.8 | (75.7, 81.0) | 81.0 | (77.5, 82.6) | 81.7 | (77.3, 82.6) | 77.3 | (75.2, 80.0) | 78.4 | (76.4, 81.3) | 0.09 | 0.2 |
| SNB | 73.3 | (70.2, 76.5) | 72.2 | (71.3, 77.5) | 72.3 | (69.4, 75.5) | 73.8 | (72.2, 79.0) | 69.6 | (67.7, 71.1) | 72.6 | (70.4, 74.4) | 0.002 | 0.3 |
| ANB | 5.5 | (4.4, 6.8) | 4.7 | (3.6, 6.5) | 8.0 | (6.8, 9.7) | 4.6 | (3.7, 7.4) | 8.5 | (6.5, 9.7) | 6.2 | (3.6, 7.5) | <0.001 | 0.4 |
| ML/NSL | 42.1 | (37.4, 46.3) | 41.8 | (36.4, 45.7) | 43.5 | (42.0, 46.9) | 43.7 | (41.4, 46.1) | 45.0 | (43.5, 47.5) | 42.0 | (40.5, 45.5) | 0.2 | 0.3 |
| Overjet (mm) | 4.6 | (4.3, 5.3) | 3.1 | (2.6, 3.8) | 8.6 | (6.4, 10.0) | 4.2 | (3.0, 5.7) | 6.8 | (4.6, 7.6) | 3.6 | (2.8, 4.5) | 0.001 | 0.3 |
| Overbite (mm) | −2.3 | (−3.4, −1.0) | 0.6 | (−0.1, 1.2) | −1.5 | (−1.9, −0.8) | −0.4 | (−1.0, 0.7) | −1.2 | (−2.8, 0.2) | −0.2 | (−0.7, 0.9) | 0.07 | 0.1 |
P-value <0.05 indicates statistically significant difference between the surgical subsamples.
Motives for treatment
Total sample
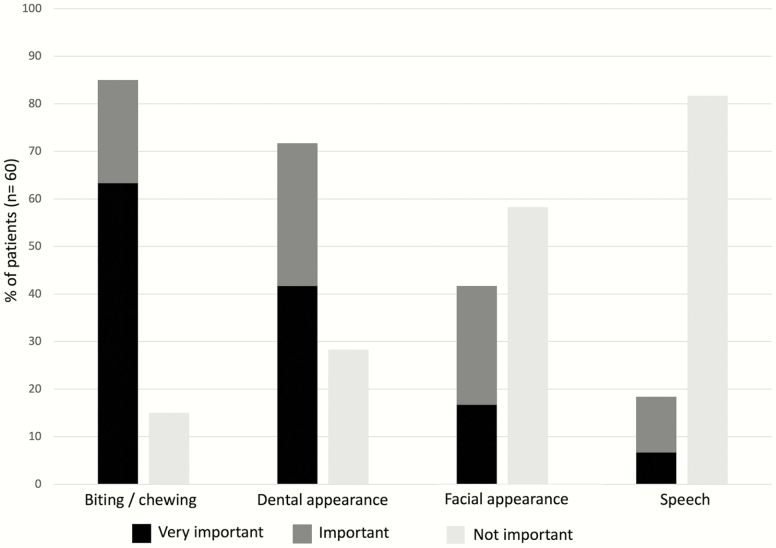
The most frequently reported motives for seeking treatment were to improve oral function (85.0 per cent) and dental appearance (71.7 per cent; Figure 2). Facial appearance was reported by 41.7 per cent, and the least reported motive was speech. Two individuals reported TMD as a motive for seeking treatment.
Figure 2.
Relative distribution of responses to questions about motives for treatment (Q1; Table 1) among the total sample of 60 patients. The responses ‘Not important’ and ‘Not important at all’ are combined.
Surgical subsamples
A statistically significant difference between the surgical subsamples was found for speech (P = 0.03), which was most frequently reported in the LeFort I subsample (35.0 per cent).
AOB subsample
Oral function (88.2 per cent) and dental appearance (70.5 per cent) were the two most frequently reported motives. Speech was again the least reported (19.6 per cent), and facial appearance was reported slightly less than in the total sample (35.0 per cent).
Perceived improvement
Total sample
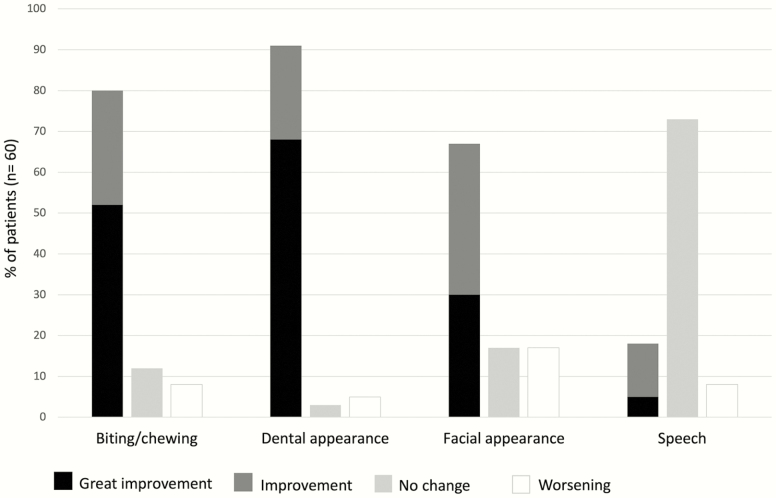
The majority reported an improvement in oral function, dental appearance, and facial appearance (Figure 3). Speech was unaffected for most patients.
Figure 3.
Relative distribution of responses to questions about the effects of treatment (Q2; Table 1) among the total sample of 60 patients.
Surgical subsamples
A statistically significant difference between the subsamples was only found for facial appearance (P = 0.02). Forty-five per cent of the Le Fort I subsample, 66.7 per cent of the BSSO, and 86.3 per cent of the Bimax subsample reported an improvement in facial appearance (Figure 4), with 20.0, 16.7, and 13.6 per cent, respectively, reporting a worsening.
Figure 4.
Relative distribution of responses to the question about the effect of treatment in terms of facial appearance (Q2; Table 1) among the three surgical subsamples.
AOB subsample
The AOB subsample reported results similar to the total sample. Dental appearance improved for 90.2 per cent and oral function for 80.4 per cent. Facial appearance improved for 60.8 per cent, 19.6 per cent reported no change, and 19.6 per cent reported a worsening. Speech was unchanged for 70.6 per cent and improved for 15.7 per cent.
Sensory impairment
Thirty-eight patients reported unchanged or fully recovered sensory function at 3 years post-surgery. Twenty-two reported permanent sensory impairment, and an association between patient dissatisfaction and sensory impairment was found (Cramer’s V = 0.3, P = 0.02).
Patient satisfaction with the treatment result
Total sample
Thirty per cent were very satisfied, 53.3 per cent were satisfied, and 16.7 per cent were dissatisfied with the treatment. Of the 10 dissatisfied patients, 8 gave their reasons in the comments section. Six were dissatisfied with the resulting occlusion, and two of these specifically mentioned relapse. Three patients were dissatisfied with their facial appearance, and one experienced loss of sensation in the lower lip. Eleven of the satisfied patients gave negative comments about the effects of changed sensation, facial appearance, TMD, and that the treatment process was extensive.
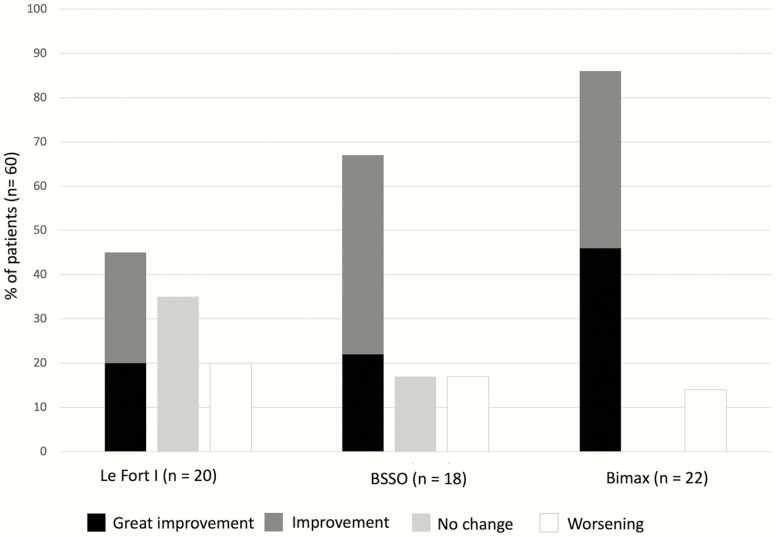
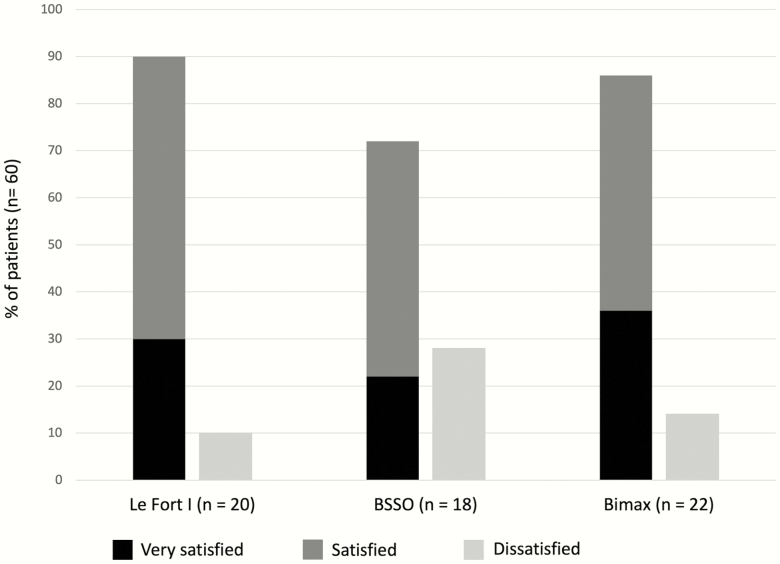
Surgical subsamples
Most patients in the Le Fort I subsample (90.0 per cent) was satisfied or very satisfied with the overall treatment result, the corresponding rates were 72.2 and 86.4 per cent for the BSSO and Bimax subsamples (Figure 5).
Figure 5.
Relative distribution of responses to the question about satisfaction with the overall treatment result (Q3; Table 1) among the three surgical subsamples.
AOB subsample
Eighty-two point 4 per cent were satisfied or very satisfied with treatment result and 17.6 per cent were dissatisfied. The majority (81.7 per cent) of the patients reported they would re-elect treatment when they were asked ‘knowing what you know today, would you make the same decision to undergo treatment?’ (Table 4).
Table 4.
Distribution of responses to the question of whether the patient would re-elect surgery based on their experience with treatment and the result (Q4; Table 1)
| Surgery | No (%) | Unsure (%) | Yes (%) |
|---|---|---|---|
| Le Fort I | 10.0 | 5.0 | 85.0 |
| BSSO | 11.0 | 16.7 | 72.3 |
| Bimax | 0.0 | 13.6 | 86.4 |
| Total sample | 6.6 | 11.7 | 81.7 |
Association between patient satisfaction and skeletal relapse
More than 30 per cent of the total sample showed horizontal relapse of the mandible ≥2 mm, measured at B point (Table 5). Almost half of the BSSO and the Bimax subsamples had relapse ≥2 mm compared with 20 per cent in the LeFort I subsample. A moderate association was found between patient dissatisfaction and relapse at B point (e2 = 0.18).
Table 5.
Proportion of patients with relapse at B point ≥2 mm at the 3 year follow-up (T5)
| Surgical subsample | 3 year follow-up (T5) |
|---|---|
| Total sample | 36.2% |
| Le Fort I | 20.0% |
| BSSO | 43.8% |
| Bimax | 45.5% |
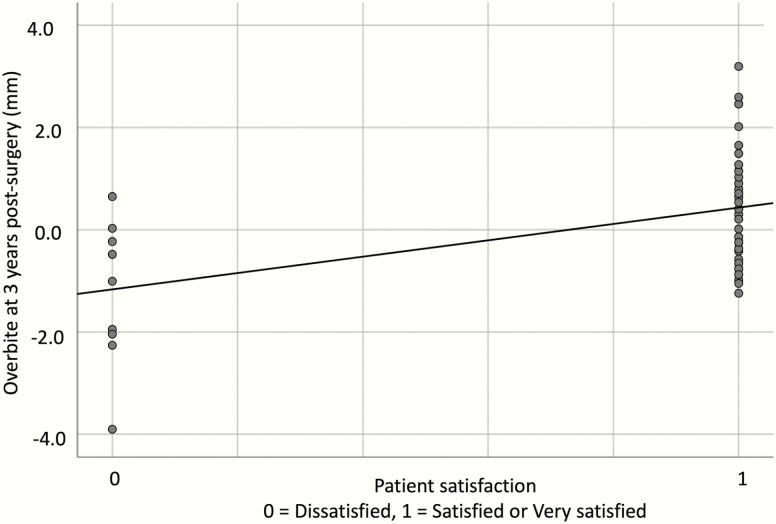
Association between patient satisfaction and correction of AOB
Almost half of the total sample (48.3 per cent) had an AOB at the 3 year follow-up (Table 6). The highest open bite rate was 62.5 per cent in the BSSO subsample. More than half (55.1 per cent) of the AOB subsample had an anterior bite at 3 years. The LeFort I subsample had the lowest rate of open bite at the 3 year follow-up (30.0 per cent).
Table 6.
Proportion of patients with an anterior open bite (AOB) at pre-surgery (T1) and at 3 year follow-up (T5) by subsample. BSSO, bilateral sagittal split osteotomy
| Subsample | Pre-surgery (T1) | 3 year follow-up (T5) |
|---|---|---|
| AOB | 100 % | 55.1% |
| Total sample | 85.0% | 48.3% |
| Le Fort I | 95.0% | 30.0% |
| BSSO | 94.4% | 62.5% |
| Bimax | 68.2% | 54.5% |
An association was found between patient dissatisfaction and an AOB at 3 years post-surgery (e2 = 0.23) (Figure 6). No association between patient satisfaction and gender or age was found. No association was found between the initial severity of the malocclusion and patient satisfaction.
Figure 6.
Association between patient satisfaction (satisfied or dissatisfied) and degree of open bite or positive overbite at 3 years post-surgery [a negative value indicates an open bite, a positive value indicates an overbite (millimetres)]
Discussion
In this study of 60 high-angle Class II patients, the most frequently reported reasons for seeking treatment were to improve oral function and dental appearance. Although the majority reported an improvement in these areas, 16.7 per cent reported a worsening in facial appearance from treatment. Only 30.0 per cent were ‘very’ satisfied with overall treatment and 22.0 per cent of the satisfied patients reported at least one negative consequence; 16.7 per cent were dissatisfied.
The Le Fort I subsample had the highest rate of patient satisfaction and likelihood to re-elect treatment. The Le Fort I had the lowest rate of AOB 3 years after surgery but also had the highest rate of self-reported worsening in facial appearance. This suggests that oral function was more important than facial appearance for this subsample. The BSSO and Bimax subsamples reported lower rates of overall satisfaction. Worryingly, almost one-third of BSSO patients were dissatisfied, although the differences between the surgical subsamples were not statistically significant, possibly due to small sample sizes.
Dissatisfaction was associated with horizontal mandibular relapse and with an AOB at 3 years post-surgery. It was also associated with a loss of sensory function. The higher rate of dissatisfaction in the Bimax and BSSO subsamples may be due to the increased rates of AOB, mandibular relapse, and sensory impairment. Sensory impairment is frequently associated with the BSSO and Bimax procedure (10, 24, 25). The average long-term surgical skeletal changes were smaller than expected considering that the aim of surgery is to reduce the underlying skeletal discrepancy; nevertheless, the overjet and AOB improved in all subsamples.
The findings in the present study are in agreement with previous studies on motives for seeking orthognathic treatment, although a higher proportion reported facial appearance to be important in other studies (9, 11, 12, 15, 18, 26–28). There are a few studies on Class II malocclusion for comparison (7, 10, 25, 29), but none on high-angle Class II patients or Class II open bite. As studies tend to combine ‘very satisfied’ and ‘satisfied’, subtle distinctions between satisfaction rates in subsamples may be overlooked. The combined (satisfied and very satisfied) satisfaction rate (83.3 per cent) in the present study are amongst the lowest reported for orthognathic surgery so far, with most finding satisfaction rates of more than 90 per cent or at least a higher proportion of highly satisfied patients (6, 8, 9, 15, 16, 18, 30–35). The dissatisfaction rate found (16.7 per cent) is, thus, high relative to previous studies (9, 36), but there are few rates of dissatisfaction to compare with. When studies only report satisfaction rates, it is difficult to establish whether participants that were not among the satisfied were really dissatisfied. Two studies have reported that mandibular advancement patients were less satisfied than mandibular setback patients (10, 25), and treatment for a retrognathic mandible was associated with a lower score in overall satisfaction in another study (29). On the other hand, studies have also found no difference between surgical subsamples (16) or between malocclusion subsamples (18, 37). Patients with more severe deformities have reportedly been more satisfied after treatment (38), but such an association was not confirmed by this present study.
Limitations of the study
This study is based on retrospective data and accordingly there is a risk of bias. To reduce this risk, only consecutive treatments were included. The reasons for the 30.2 per cent non-participation rate are unknown, but highly satisfied or dissatisfied patients may have refrained from completing the questionnaire.
The present study has used a questionnaire with fixed alternative answers and, as this was a retrospective study, there was no opportunity to change to another method, such as a visual analogue scale or oral health-related quality of life index (15). The number of questions used to assess patient satisfaction could have been more comprehensive and included factors such as treatment duration, treatment costs, and quality of pre-treatment information that may also influence patient satisfaction (26). Nevertheless, the questionnaire uses two questions that have been consistently used in previous studies (6, 18, 30, 32, 34, 38–43), and a comments section was available for the patient to use after every question.
Although participants could give more than one reason for seeking treatment, it might have been more useful to ask them to rate their order of importance. A qualitative approach may be better suited than quantitative methods to reach a deeper understanding of patients’ expectations from treatment and on how to better support the small but important proportion of patients that report dissatisfaction with the treatment (13, 44). However, taking in to account the long-term interval needed to collect this sample of high-angle Class II patients, a qualitative study or the development of a new questionnaire to supplement the findings would probably have resulted in a low response rate.
The long follow-up time was considered important because relapse of high-angle Class II tends to appear over a period of time. However, 3 years is a considerable time span, which may affect patients’ memories about the treatment. (38)
The inclusion criteria restrict this sample to high-angle Class II malocclusion. The prevalence of high-angle Class II malocclusion treated by orthognathic surgery is relatively low compared to other types of malocclusions, and it was, therefore, not possible to increase the sample size whilst maintaining the inclusion criteria. The sample has a higher proportion of females than males, which is typical of surgical samples (45).
Conclusions
An improvement in oral function and dental and facial appearance was reported by the majority of these high-angle Class II surgical participants. However, a higher rate of dissatisfaction was found than what is usually reported for othognathic surgical patients in general, which is of concern. Dissatisfaction was primarily associated with a persisting AOB. In addition, mandibular relapse and impaired sensory function were related to dissatisfaction and these are associated with mandibular surgery.
Prospective patients may benefit from a comprehensive consultation about surgical approaches and possible treatment outcomes, including relapse tendencies. Future studies are needed to examine how to support the significant proportion of patients who report dissatisfaction, particularly as the negative effects of this elective procedure may have a large impact on a healthy individual’s life.
Acknowledgements
The authors would like to thank Beata Petrovski for valuable assistance with the statistical analyses.
Conflict of interest
None declared.
References
- 1. Proffit, W.R., Turvey, T.A. and Phillips, C. (1996) Orthognathic surgery: a hierarchy of stability. The International Journal of Adult Orthodontics and Orthognathic Surgery, 11, 191–204. [PubMed] [Google Scholar]
- 2. Proffit, W.R., Turvey, T.A. and Phillips, C. (2007) The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head and Face Medicine, 3, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mobarak, K.A., Espeland, L., Krogstad, O. and Lyberg, T. (2001) Mandibular advancement surgery in high-angle and low-angle class II patients: different long-term skeletal responses. American Journal of Orthodontics and Dentofacial Orthopedics, 119, 368–381. [DOI] [PubMed] [Google Scholar]
- 4. Borstlap, W.A., Stoelinga, P.J., Hoppenreijs, T.J. and van’t Hof, M.A. (2004) Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part II. Radiographic parameters. International Journal of Oral and Maxillofacial Surgery, 33, 535–542. [DOI] [PubMed] [Google Scholar]
- 5. Douma, E., Kuftinec, M.M. and Moshiri, F. (1991) A comparative study of stability after mandibular advancement surgery. American Journal of Orthodontics and Dentofacial Orthopedics, 100, 141–155. [DOI] [PubMed] [Google Scholar]
- 6. Forssell, H., Finne, K., Forssell, K., Panula, K. and Blinnikka, L.M. (1998) Expectations and perceptions regarding treatment: a prospective study of patients undergoing orthognathic surgery. The International Journal of Adult Orthodontics and Orthognathic surgery, 13, 107–113. [PubMed] [Google Scholar]
- 7. Motegi, E., Hatch, J.P., Rugh, J.D. and Yamaguchi, H. (2003) Health-related quality of life and psychosocial function 5 years after orthognathic surgery. American Journal of Orthodontics and Dentofacial Orthopedics, 124, 138–143. [DOI] [PubMed] [Google Scholar]
- 8. Borstlap, W.A., Stoelinga, P.J., Hoppenreijs, T.J. and van’t Hof, M.A. (2004) Stabilisation of sagittal split advancement osteotomies with miniplates: a prospective, multicentre study with two-year follow-up. Part I. Clinical parameters. International Journal of Oral and Maxillofacial Surgery, 33, 433–441. [DOI] [PubMed] [Google Scholar]
- 9. Trovik, T.A., Wisth, P.J., Tornes, K., Bøe, O.E. and Moen, K. (2012) Patients’ perceptions of improvements after bilateral sagittal split osteotomy advancement surgery: 10 to 14 years of follow-up. American Journal of Orthodontics and Dentofacial Orthopedics, 141, 204–212. [DOI] [PubMed] [Google Scholar]
- 10. Espeland, L., Høgevold, H.E. and Stenvik, A. (2008) A 3-year patient-centred follow-up of 516 consecutively treated orthognathic surgery patients. European Journal of Orthodontics, 30, 24–30. [DOI] [PubMed] [Google Scholar]
- 11. Stirling, J., Latchford, G., Morris, D.O., Kindelan, J., Spencer, R.J. and Bekker, H.L. (2007) Elective orthognathic treatment decision making: a survey of patient reasons and experiences. Journal of Orthodontics, 34, 113–127; discussion 111. [DOI] [PubMed] [Google Scholar]
- 12. Proothi, M., Drew, S.J. and Sachs, S.A. (2010) Motivating factors for patients undergoing orthognathic surgery evaluation. Journal of Oral and Maxillofacial Surgery, 68, 1555–1559. [DOI] [PubMed] [Google Scholar]
- 13. Ryan, F.S., Barnard, M. and Cunningham, S.J. (2012) Impact of dentofacial deformity and motivation for treatment: a qualitative study. American Journal of Orthodontics and Dentofacial Orthopedics, 141, 734–742. [DOI] [PubMed] [Google Scholar]
- 14. Larsen, M.K. and Thygesen, T.H. (2016) Orthognathic Surgery: outcome in a Facebook group. The Journal of Craniofacial Surgery, 27, 350–355. [DOI] [PubMed] [Google Scholar]
- 15. Schilbred Eriksen, E., Moen, K., Wisth, P.J., Løes, S. and Klock, K.S. (2018) Patient satisfaction and oral health-related quality of life 10–15 years after orthodontic-surgical treatment of mandibular prognathism. International Journal of Oral and Maxillofacial Surgery, 47, 1015–1021. [DOI] [PubMed] [Google Scholar]
- 16. Finlay, P.M., Atkinson, J.M. and Moos, K.F. (1995) Orthognathic surgery: patient expectations; psychological profile and satisfaction with outcome. The British Journal of Oral and Maxillofacial Surgery, 33, 9–14. [DOI] [PubMed] [Google Scholar]
- 17. Williams, A.C., Shah, H., Sandy, J.R. and Travess, H.C. (2005) Patients’ motivations for treatment and their experiences of orthodontic preparation for orthognathic surgery. Journal of Orthodontics, 32, 191–202. [DOI] [PubMed] [Google Scholar]
- 18. Pereira, R.M.A., Souza, G.M.M., Rocha, V.A.C., Morimoto, S., Tedesco, T.K. and Mello-Moura, A.C.V. (2017) Evaluation of the post orthognathic surgery satisfaction: a comparative cross-sectional study of patients Class II and III. The Journal of Craniofacial Surgery, 28, 1833–1836. [DOI] [PubMed] [Google Scholar]
- 19. Pachêco-Pereira, C., Abreu, L.G., Dick, B.D., De Luca Canto, G., Paiva, S.M. and Flores-Mir, C. (2016) Patient satisfaction after orthodontic treatment combined with orthognathic surgery: a systematic review. The Angle Orthodontist, 86, 495–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kanatas, A.N. and Rogers, S.N. (2010) A systematic review of patient self-completed questionnaires suitable for oral and maxillofacial surgery. The British Journal of Oral and Maxillofacial Surgery, 48, 579–590. [DOI] [PubMed] [Google Scholar]
- 21. Lee, S., McGrath, C. and Samman, N. (2007) Quality of life in patients with dentofacial deformity: a comparison of measurement approaches. International Journal of Oral and Maxillofacial Surgery, 36, 488–492. [DOI] [PubMed] [Google Scholar]
- 22. Axelsson S. (2005) Variability of the Cranial and Dental Phenotype in Williams Syndrome. Oslo, Norway: Institute of Clinical Odontology, Faculty of Dentistry, University of Oslo. [PubMed] [Google Scholar]
- 23. Fontes, A.M., Joondeph, D.R., Bloomquist, D.S., Greenlee, G.M., Wallen, T.R. and Huang, G.J. (2012) Long-term stability of anterior open-bite closure with bilateral sagittal split osteotomy. American Journal of Orthodontics and Dentofacial Orthopedics, 142, 792–800. [DOI] [PubMed] [Google Scholar]
- 24. Ahmad, Z., Breeze, J. and Williams, R. (2018) Numbness of the lower lip does not adversely affect quality of life or patients’ satisfaction after mandibular orthognathic surgery. The British Journal of Oral and Maxillofacial Surgery, 56, 421–424. [DOI] [PubMed] [Google Scholar]
- 25. Pahkala, R.H. and Kellokoski, J.K. (2007) Surgical-orthodontic treatment and patients’ functional and psychosocial well-being. American Journal of Orthodontics and Dentofacial Orthopedics, 132, 158–164. [DOI] [PubMed] [Google Scholar]
- 26. Flanary, C.M., Barnwell, G.M., Jr and Alexander, J.M. (1985) Patient perceptions of orthognathic surgery. American Journal of Orthodontics, 88, 137–145. [DOI] [PubMed] [Google Scholar]
- 27. Modig, M., Andersson, L. and Wårdh, I. (2006) Patients’ perception of improvement after orthognathic surgery: pilot study. The British Journal of Oral and Maxillofacial Surgery, 44, 24–27. [DOI] [PubMed] [Google Scholar]
- 28. Yu, D., Wang, F., Wang, X., Fang, B. and Shen, S.G. (2013) Presurgical motivations, self-esteem, and oral health of orthognathic surgery patients. The Journal of Craniofacial Surgery, 24, 743–747. [DOI] [PubMed] [Google Scholar]
- 29. Rustemeyer, J., Eke, Z. and Bremerich, A. (2010) Perception of improvement after orthognathic surgery: the important variables affecting patient satisfaction. Oral and Maxillofacial Surgery, 14, 155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cunningham, S.J., Hunt, N.P. and Feinmann, C. (1996) Perceptions of outcome following orthognathic surgery. The British Journal of Oral and Maxillofacial Surgery, 34, 210–213. [DOI] [PubMed] [Google Scholar]
- 31. Bertolini, F., Russo, V. and Sansebastiano, G. (2000) Pre- and postsurgical psycho-emotional aspects of the orthognathic surgery patient. The International Journal of Adult Orthodontics and Orthognathic Surgery, 15, 16–23. [PubMed] [Google Scholar]
- 32. Busby, B.R., Bailey, L.J., Proffit, W.R., Phillips, C. and White, R.P., Jr. (2002) Long-term stability of surgical class III treatment: a study of 5-year postsurgical results. The International Journal of Adult Orthodontics and Orthognathic Surgery, 17, 159–170. [PubMed] [Google Scholar]
- 33. Al-Asfour, A., Waheedi, M. and Koshy, S. (2018) Survey of patient experiences of orthognathic surgery: health-related quality of life and satisfaction. International Journal of Oral and Maxillofacial Surgery, 47, 726–731. [DOI] [PubMed] [Google Scholar]
- 34. Nurminen, L., Pietilä, T. and Vinkka-Puhakka, H. (1999) Motivation for and satisfaction with orthodontic-surgical treatment: a retrospective study of 28 patients. European Journal of Orthodontics, 21, 79–87. [DOI] [PubMed] [Google Scholar]
- 35. Oland, J., Jensen, J., Elklit, A. and Melsen, B. (2011) Motives for surgical-orthodontic treatment and effect of treatment on psychosocial well-being and satisfaction: a prospective study of 118 patients. Journal of Oral and Maxillofacial Surgery, 69, 104–113. [DOI] [PubMed] [Google Scholar]
- 36. Liddle, M.J., Baker, S.R., Smith, K.G. and Thompson, A.R. (2015) Psychosocial outcomes in orthognathic surgery: a review of the literature. The Cleft Palate-Craniofacial Journal, 52, 458–470. [DOI] [PubMed] [Google Scholar]
- 37. Baherimoghaddam, T., Tabrizi, R., Naseri, N., Pouzesh, A., Oshagh, M. and Torkan, S. (2016) Assessment of the changes in quality of life of patients with class II and III deformities during and after orthodontic-surgical treatment. International Journal of Oral and Maxillofacial Surgery, 45, 476–485. [DOI] [PubMed] [Google Scholar]
- 38. Chen, B., Zhang, Z.K. and Wang, X. (2002) Factors influencing postoperative satisfaction of orthognathic surgery patients. The International Journal of Adult Orthodontics and Orthognathic Surgery, 17, 217–222. [PubMed] [Google Scholar]
- 39. Kiyak, H.A., Hohl, T., West, R.A. and McNeill, R.W. (1984) Psychologic changes in orthognathic surgery patients: a 24-month follow up. Journal of Oral and Maxillofacial Surgery, 42, 506–512. [DOI] [PubMed] [Google Scholar]
- 40. Ostler, S. and Kiyak, H.A. (1991) Treatment expectations versus outcomes among orthognathic surgery patients. The International Journal of Adult Orthodontics and Orthognathic Surgery, 6, 247–255. [PubMed] [Google Scholar]
- 41. Mihalik, C.A., Proffit, W.R. and Phillips, C. (2003) Long-term follow-up of Class II adults treated with orthodontic camouflage: a comparison with orthognathic surgery outcomes. American Journal of Orthodontics and Dentofacial Orthopedics, 123, 266–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Posnick, J.C. and Wallace, J. (2008) Complex orthognathic surgery: assessment of patient satisfaction. Journal of Oral and Maxillofacial Surgery, 66, 934–942. [DOI] [PubMed] [Google Scholar]
- 43. Kim, S., Shin, S.W., Han, I., Joe, S.H., Kim, M.R. and Kwon, J.J. (2009) Clinical review of factors leading to perioperative dissatisfaction related to orthognathic surgery. Journal of Oral and Maxillofacial Surgery, 67, 2217–2221. [DOI] [PubMed] [Google Scholar]
- 44. AlQuraini, N., Shah, R. and Cunningham, S.J. (2019) Perceptions of outcomes of orthodontic treatment in adolescent patients: a qualitative study. European Journal of Orthodontics, 41, 294–300. [DOI] [PubMed] [Google Scholar]
- 45. Bailey, L.J., Haltiwanger, L.H., Blakey, G.H. and Proffit, W.R. (2001) Who seeks surgical-orthodontic treatment: a current review. The International Journal of Adult Orthodontics and Orthognathic Surgery, 16, 280–292. [PubMed] [Google Scholar]