Abstract
In the current paper, we describe an integrated online- and mobile-based application for the treatment of childhood anxiety disorders, Anxiety Coach. The technology is designed to increase the use of exposure therapy by therapists and patients. We begin by outlining the clinical content and design of the application, and then review the clinical administration and theoretical basis for the program. Next, using results from an implementation feasibility study, we illustrate how data collected during application use can inform therapists, supervisors, and researchers about process variables (i.e., use of exposure) and outcomes (i.e., symptom improvement). Implications of the potential for Anxiety Coach to increase access to evidence-based treatment and directions for further research are discussed.
Keywords: childhood anxiety disorders, obsessive-compulsive disorder, information and communication technology, fidelity, exposure
ANXIETY disorders are among the most common psychiatric disorders in childhood, with prevalence rates as high as 25% (Beesdo, Knappe, & Pine, 2009), and are associated with substantial impairment in functioning, are highly comorbid with other psychiatric disorders, and often persist into adulthood (Anderson, 1994; Chorpita & Southam-Gerow, 2006; Mendlowicz & Stein, 2000; Quilty, Van Ameringen, Mancini, Oakman, & Farvolden, 2003). Unfortunately, anxiety disorders are the least likely psychiatric disorder to be treated (approximately 30%; Merikangas et al., 2010), despite the strong literature supporting the efficacy of exposure-based cognitive behavioral therapy (CBT; AACAP, 2007; Higa-McMillan, Francis, Rith-Najarian, & Chorpita, 2016; James, James, Codrey, Soler, & Choke, 2013). Two of the leading reasons that childhood anxiety disorders are inadequately treated include the infrequency with which community therapists use exposure-based CBT (Whiteside, Deacon, Benito, & Stewart, 2016; Whiteside, Sattler, et al., 2016) and the insufficient number of therapists to meet the population’s need for mental health services (Kazdin & Blase, 2011). Information and communication technology (ICT; i.e., Internet, mobile devices) provides a platform to increase access to evidence-based treatment for childhood anxiety disorders. In the present paper, we describe an integrated online- and mobile-based application for the treatment of childhood anxiety disorders, Anxiety Coach, and use data from an implementation feasibility pilot to illustrate its potential capabilities.
Anxiety Coach: An Overview
To introduce Anxiety Coach, we first describe the clinical content and design of the application. We then review the clinical administration and theoretical basis. Anxiety Coach began as a mobile application for iOS. This paper describes the addition of a web-based application for therapists to access during therapy sessions via a computer. The current description focuses on changes to the original mobile-based application, which has been described in detail elsewhere (Carper, 2017; Whiteside, 2016; Whiteside, Ale, Vickers Douglas, Tiede, & Dammann, 2014).
Anxiety Coach: Clinical Content
The therapeutic content of the Anxiety Coach application consists of Parent-Coached Exposure Therapy (PC-Exp; Whiteside et al., 2015). The goal of PC-Exp is to emphasize exposure by introducing it early in treatment and training parents to facilitate exposures during and outside of sessions. Sessions are conducted with the parent and child together. Treatment begins with psychoeducation regarding the role of avoidance in the maintenance of anxiety disorders, use of exposure to break this cycle, and how this conceptualization applies to the child’s symptoms. The therapist then guides the patient and parent through creation of a fear hierarchy. Once these steps are completed, typically within one to three sessions, treatment consists of exposure therapy in-session and assigned between sessions. To facilitate completion of exposure in real-world settings, parents are trained during the sessions by the therapist to be exposure coaches. Cognitive change is encouraged to occur during exposures, rather than through independent exercises. Other anxiety-management strategies, such as relaxation, are not introduced.
Anxiety Coach: Technological Design
Web-Based Portal
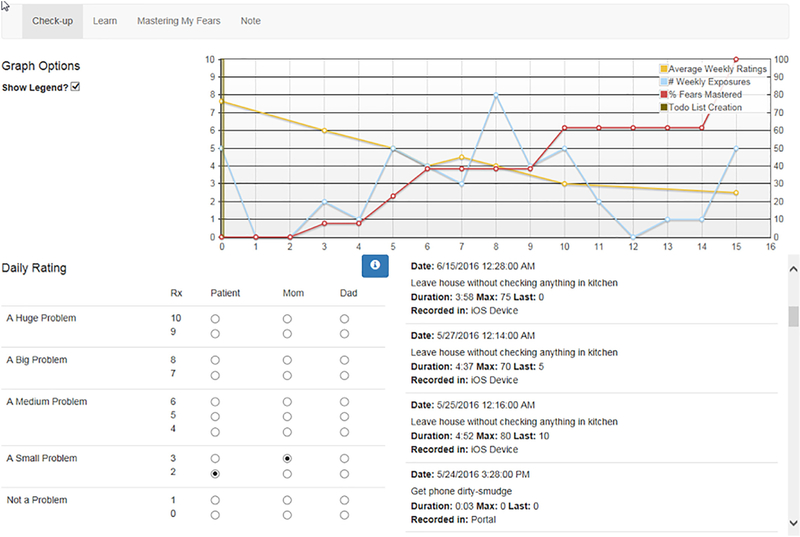
The web-based portal is designed to be used by the therapist during face-to-face sessions or to monitor progress outside of sessions. The web-based component of the application contains four treatment sections on three separate web pages. The initial page is the patient’s home page and is labeled “Check-up” (see Figure 1). This page includes: (a) a graph (not available through the original mobile application) tracking the date the fear ladder was constructed, weekly anxiety ratings, the number of exposures completed each week, and the percentage of items on the fear ladder that have been mastered; (b) a log of all the exposures that have been completed, including the date and time of completion, device (mobile or web-based) they were completed on, the item, highest and final anxiety rating, and duration; and (c) a section to enter 0-to-10 ratings from the child, mother, and father of the recent severity of anxiety symptoms (as opposed to a rating from a single respondent available in the mobile application).
Figure 1.
Check-up screen from therapist web-based portal.
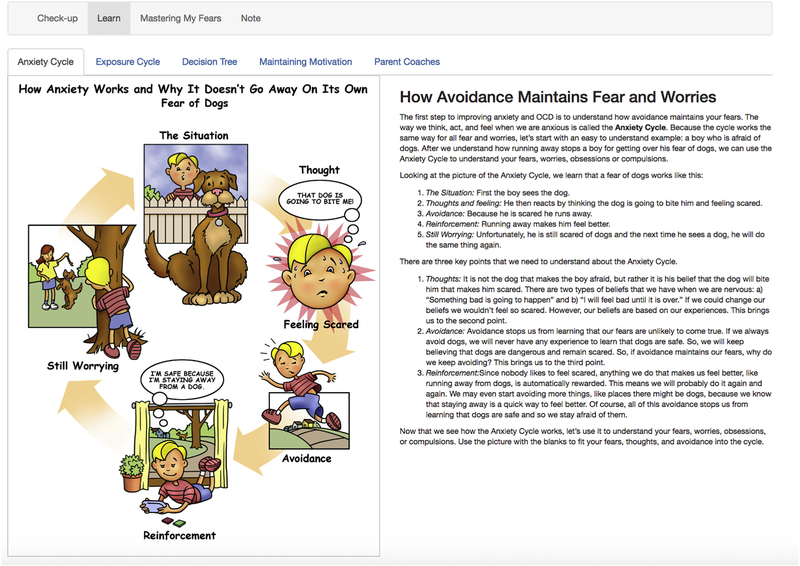
The next page includes psychoeducation and is labeled “Learn.” The Learn section consists of five tabs with static graphics and/or text covering the following content: (a) the role of avoidance in maintaining anxiety or OCD; (b) the role of exposure in breaking the cycle of avoidance; (c) explanation of how to rate the likelihood and severity of negative outcomes when conducting exposures; (d) instructions to guide parent coaching of exposures; and (e) overview of behavioral strategies to promote compliance with exposure. Changes from the original mobile application include the addition of content specific to child treatment (e.g., parent coaching and behavioral management) and child-oriented graphics (Figure 2).
Figure 2.
Child-oriented psychoeducation screen from therapist web-based portal.
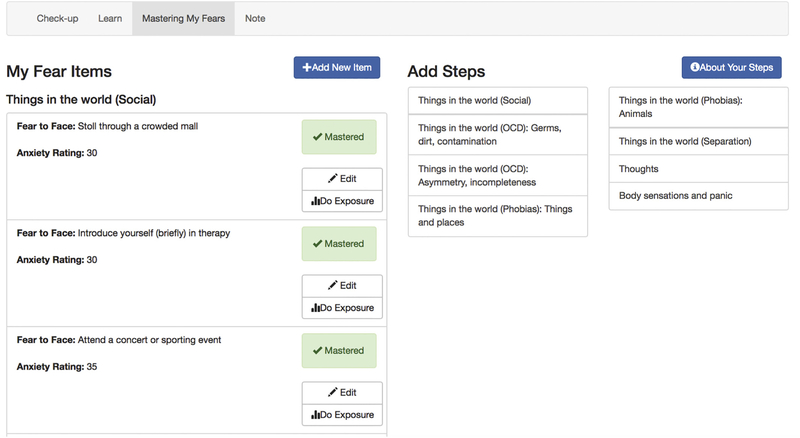
The third page contains the central components of the application, creation of fear ladders and completion of exposures. The left side of the screen displays the patient’s fear ladder and the right side displays a library of exposure exercises targeting symptoms of all anxiety disorders and OCD. Each item in the library can be selected individually and added to the patient’s fear ladder (Figure 3; a change from the original mobile application that required selection of full fear ladders). In addition, the therapist can create original items by entering free text. After items have been added to the fear ladder, they can be arranged into subgroups (e.g., social vs. contamination exposures) and organized by perceived difficulty.
Figure 3.
Fear ladder screen from therapist web-based portal.
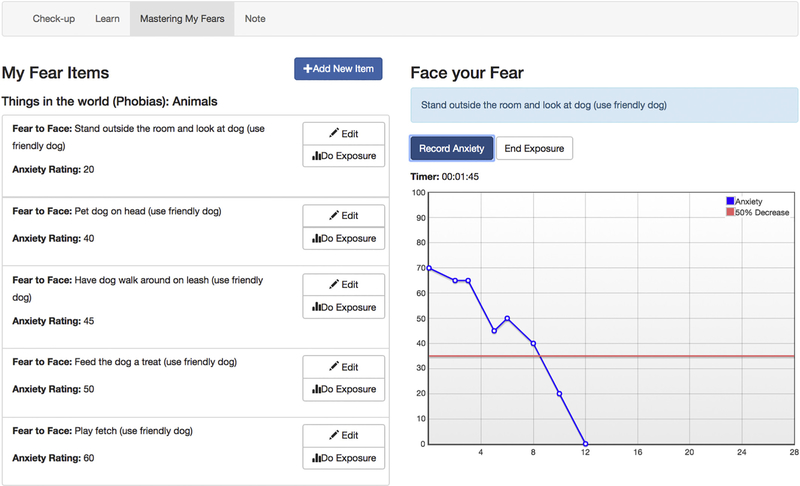
Once a hierarchy is established, items can be selected to complete exposures. When an item from the hierarchy is selected, the library on the right side of the screen is replaced with an exposure form. The form first asks the patient to rate the likelihood and severity of negative outcomes, as well as initial fear level. The exposure form then displays a graph with the initial rating, a line designating 50% decrease in anxiety, and a button to provide subsequent ratings (Figure 4). When the exposure is completed, the exposure form prompts the patient to summarize the outcome (e.g., fear did not come true and anxiety decreased). The item can also be designated as mastered, which will result in it being marked as such on the fear ladder.
Figure 4.
Exposure screen from therapist web-based portal.
Mobile Device App
The mobile device component of Anxiety Coach operates on iOS (i.e., iPhone, iPad, iPodTouch) and is designed to be used by the child and family outside of sessions. The content and functionality mirrors that of the web-based portal and has been described in previous publications (Carper, 2017; Whiteside, 2016; Whiteside et al., 2014). Changes from earlier versions include additional psychoeducational material regarding child-oriented treatment with parent-coached exposure and the ability to select individual items rather than entire fear ladders.
Data Capture and Synchronization
We designed Anxiety Coach to capture and display clinically relevant data generated through use of the mobile-device and web-based portal. Patients can send a request from their mobile device to have the therapist link that device to the patient’s record in the web-based portal. Once the mobile-device and web-based portal are linked, data regarding anxiety ratings, fear ladder items, and completed exposures are synced into a single record. Thus, tasks completed through one medium can be viewed and edited through the other. Data captured regarding exposures not only provides a count of the number of exposures completed and to which fear ladder item, but the time and duration of the exposure, as well as the peak and final anxiety rating.
Clinical Administration
We designed Anxiety Coach to be used by therapists with an appropriate background in child mental health, but not necessarily experience with exposure therapy. Training in the use of Anxiety Coach consists of a 60- to 90-minute phone training and an 18-page written manual that covers the clinical content of PC-Exp (Whiteside et al., 2015), how the integrated application can be used to deliver PC-Exp, a guide to the technical use of the technology, and a session-by-session suggested timeline. The training does not prescribe a session-by-session protocol, but rather a number of tasks that need to be completed to deliver exposure therapy.
Treatment begins with a general introduction to PC-Exp and the Anxiety Coach application. If interested in using the mobile-application, families can download it to their device and send a link request to therapist during the session. Families can decide whether they prefer to have the application on the child’s or parent’s device. The therapist then presents the psychoeducational material using the graphics and text in the web-based portal and by showing the family where the information can be found in the mobile application. In addition, the therapist helps the family apply the psychoeducational material to understand the child’s symptoms. The therapist then uses the web-based exposure-item library to work with the family to build a fear ladder and again, show the family where to find and edit the ladder in the mobile device. Once the preparatory steps are completed the therapist guides the family through conducting exposures. The therapist uses the web-based portal to set up and record exposures completed in the session. Exposures completed by the family between sessions or during a session, but out of the office, can be recorded through the mobile device. Initially during the session, the therapist leads the exposure, but over time the parent takes over coaching the child under the therapist’s direction.
Progress can be monitored by the therapist and family through the check-up module in the web-based portal and the mobile-device. As displayed in Figure 1, the check-up screen includes measures of symptom improvement (i.e., anxiety ratings), engagement in therapeutic activities designed to address symptoms (i.e., number of exposures completed per week), and progress toward therapeutic goals (i.e., percentage of fear ladder mastered). The therapist can begin each session by reviewing the check-up screen with the family and asking them to provide anxiety ratings. The therapist also has detailed information about the number and adequacy (i.e., duration, anxiety levels) of exposures conducted during the week. To support treatment with minimal or no direct contact, the therapist can monitor the check-up page periodically and provide direction to the family remotely. Finally, to facilitate therapist training or ongoing quality assurance, a supervisor can monitor the therapist’s use of exposure and the patient’s response through the web-based check-up screen as well.
Theoretical Basis
We designed Anxiety Coach to efficiently increase therapist fidelity to, and patient engagement in, evidence-based treatment (EBT) for anxiety disorders and OCD (i.e., exposure therapy). As such, the clinical content of Anxiety Coach is designed to focus exclusively on exposure without other anxiety management strategies. Second, by automatically collecting and displaying data on process variables (i.e., exposure completion) and outcome (i.e., anxiety ratings), Anxiety Coach provides information to implement supportive accountability (Mohr, Cuijpers, & Lehman, 2011), whether it be therapist self-monitoring, oversight from a supervision, or therapists monitoring patient engagement. Third, to address the shortage of therapists, Anxiety Coach is designed to maximize the amount of treatment delivered without a therapist by increasing patient engagement in skill use between sessions.
Feature Demonstration
To illustrate how Anxiety Coach could be used clinically to monitor fidelity and engagement, we present a case series from the initial implementation feasibility piloting. This pilot was designed to identify and address issues with the technology or its clinical administration that would interfere with implementation. Data collection included frequency of exposure as an indicator of engagement, symptom change to estimate therapeutic value, and feedback from therapists and families regarding acceptability. Although the trial was not designed to test the ability of the program to improve fidelity, engagement, or outcome, the data provide an informative illustration of the program’s potential to do so.
Participants
Four therapists (one doctoral-level psychologist, two master-level therapists, and one postdoctoral psychology fellow) with expertise in the delivery of exposure therapy for childhood anxiety disorders/OCD and familiarity with the Anxiety Coach application provided treatment to eight children. The children (six girls, 75%) ages 8 to 17 (mean = 12.63, SD = 2.8) had a primary diagnosis of an anxiety disorder, n = 5; 62.5%, (generalized anxiety disorder [GAD] = 2, social phobia = 1; specific phobia = 2) or OCD (n = 3; 37.5%). Half of the patients had a single diagnosis while one had two diagnoses, one had three, and two had four diagnoses. The children were all Caucasian with parents that typically had at least a college degree (n = 7, 87.5%) and were married (n = 7, 87.5%). The medical center’s Institutional Review Board approved the research protocol and materials. Parents and children provided informed written consent (or assent by children 12 or under) prior to participation.
Procedures
Participants were recruited following the completion of a family-initiated clinical assessment within an outpatient clinic specializing in childhood anxiety and OCD housed within a Department of Psychiatry and Psychology. Families that agreed to participate in the study were asked to complete the research questionnaires and a pretreatment assessment (time 1) with an independent evaluator (IE) via videophone. Following the research evaluation, six of the families participated in up to 12 weekly therapy appointments using Anxiety Coach. Two families participated in minimal contact treatment which consisted of one or two initial therapy sessions followed by remote monitoring through Anxiety Coach for up to 12 weeks after the initiation of treatment. The decision to participate in minimal contact treatment was based on family preference (e.g., geographical distance from the clinic). To protect confidentiality no identifiable information could be entered into Anxiety Coach. Posttreatment evaluations consisted of families completing the assessment measures and videophone interview with the IE. Qualitative interviews were then completed with the families and therapists.
Assessment Measures
Before and after treatment, an IE administered the interviewer-based measures via videophone. Diagnoses were determined based on the Anxiety Disorders Interview Schedule for DSM-IV: Child Version (ADIS:C; Albano & Silverman, 1996), a semistructured diagnostic interview of childhood anxiety disorders as well as mood and externalizing disorders with good interviewer-observer reliability, test-retest reliability, and construct validity (Wood, Piacentini, Bergman, McCracken, & Barrios, 2002). Measures of severity included the clinician’s severity rating (CSR) from the ADIS, as well as the Pediatric Anxiety Rating Scale (PARS; RUPP, 2002), a scale consisting of five items assessing anxiety severity, frequency, distress, avoidance, and interference that has good psychometric properties. In addition, the IE administered the Clinical Global Impression Scale (Guy, 1976) rating of (a) severity (CGI-S) ranging from 1 (not at all ill) to 7 (extremely ill), with a score of 1 or 2 reflecting no to minimal symptoms; and b) a rating of clinical improvement (CGI-I) ranging from 1 (very much improved) and 7 (very much worse) with a score of 1 (very much improved) or 2 (much improved) considered treatment responders. The first author trained the IE in the use of these measures and independently coded audio recordings to assess reliability. This led to a kappa of .74 for categorical diagnoses from four of the initial diagnostic interviews and .89 for continuous ratings (i.e., PARS, CGI-S, CGI-I) from 10 pre- and posttreatment assessments.
Parents and children completed symptoms measures before and after treatment. These included the Spence Children’s Anxiety Scale-Child and Parent Versions (SCAS-C/P), which is a Likert-type questionnaire with robust reliability and validity measuring six facets of anxiety in children and adolescents, although only the total subscale was included in the current study (Muris, Merckelbach, Ollendick, King, & Bogie, 2002; Muris, Schmidt, & Merckelbach, 2000; Spence, 1998).
Following the completion of treatment, two qualitative researchers not involved in the development or delivery of Anxiety Coach conducted semistructured interviews. We planned to use a purposive sampling approach, critical case sampling, which involves identification and selection of information-rich cases related to the research questions (Palinkas et al., 2015), considering variables such as gender, familiarity with technology, and level of application use. However, given the small sample size, we were able to invite all families and the five families that agreed were interviewed. The interviewer began with open-ended questions to the child and then parent to describe how they used the application (including with the therapist and at home), as well as their opinions (positive and negative) about the application. In addition, three of the therapists (the first author was not interviewed) were also interviewed. Therapists were asked to describe how they used the application with their patients (including each of the features), how they thought it impacted their patients, and their overall impression of the application.
Interviews were recorded and transcribed verbatim. The interview guides and initial coding structure were based on prior studies of patient experience with technology (Hsieh & Shannon, 2005; Patton, 2002; Weber, 1990). Text data was organized first by general topic area using NVivo qualitative analysis software. Two qualitative researchers then independently coded text using methods of content analysis, compared results, refined themes and organized them by predominant themes as well as nonrepresentative opinions that were considered relevant because of specific mention of patient interaction with technology.
Operational Issues Affecting Data Collection
A number of the recorded exposures were of very short duration (including zero seconds), very long duration (multiple hours), or had initial ratings of zero anxiety, suggesting that they did not accurately reflect the nature of the exposure. To address these data issues that would likely obscure an accurate summary of exposure use: (a) those with zero seconds duration were removed (e.g., assuming recording of an exposure only to mark the item as mastered); (b) those with an anxiety rating of zero at the beginning, all of which were 5 seconds in duration or less, were removed; (c) exposures of less than a minute in duration that included an initial anxiety rating greater than zero were counted as exposures, but the duration was not entered in the average duration (e.g., assuming recording of a previously completed exposures); (d) exposures with durations of multiple hours were included in the exposure count, but not entered in the average duration (e.g., assuming that the program was left running unattended during an exposure).
Results
Therapist Exposure Use
The six patients treated with face-to-face sessions attended from 6 to 11 appointments (mean = 8.50, SD = 1.9) over a period of 3.5 to 4 months (mean = 15.19 weeks; SD = 2.3; range 12.14 to 17.71). Table 1 presents data regarding therapist exposure use. Each of the four therapists treated one or two patients. There was significant variability in timing of beginning exposure (first to fifth session), the percentage of sessions in which exposures were recorded (25% to 84%) and in the maximum recorded anxiety rating (25 to 77). However, the length of exposures (7 to 15 minutes) and proportion of decrease in anxiety ratings (two-thirds or greater) were fairly consistent across therapists.
Table 1.
Therapist Use of Exposure
| Therapist | N | Appts | 1st Exp | #Exp | %Exp | Dur | Max | End | Dcr |
|---|---|---|---|---|---|---|---|---|---|
| A | 2 | 9.5 | 1 | 12.5 | 84% | 7.97 | 69.52 | 17.68 | 76% |
| B | 2 | 8.5 | 2.5 | 6 | 43% | 7.33 | 56.43 | 14.29 | 77% |
| C | 1 | 6 | 5 | 3 | 33% | 9.56 | 25 | 8.33 | 67% |
| D | 1 | 8 | 1 | 2 | 25% | 15.24 | 77.50 | 9.50 | 88% |
| Overall | 6 | 8.33 (2.1) | 2.17 (1.6) | 7 (4.7) | 52% | 8.54 (4.7) | 63.86 (21.4) | 15.84 (16.5) | 76% |
N = Number of patients; Appts = mean number of appointments per patient; 1st Exp = session during which exposures was first recorded; #Exp = number of in-session exposures recorded; %Exp = percentage of sessions during which an exposure was recorded; Dur = average duration (minutes) of recorded in-session exposures; Max = Average maximum anxiety rating recorded during in-session exposures; End = Average ending anxiety rating recorded during in-session exposures; Dcr = Average decrease in anxiety rating recorded during in-session exposures.
Patient Exposure Use
Table 2 summarizes data on patient exposure use. The patients treated with face-to-face therapy sessions recorded on average 25.33 exposures (SD = 17.0; range 7 to 54) over a period of 2.5 months from the first recorded exposure to the last (mean = 10.33 weeks, SD = 3.4, range = 6.71 to 14.86). The exposures were more often completed through the mobile application (mean = 21.83, SD = 15.0) than the web-based portal (mean = 3.5, SD = 3.3), although exposures in-session were often recorded through the mobile application. The two patients treated with minimal contact attended one and two sessions and had seven and four therapeutic messaging contacts during treatment over a period of 12 and 14 weeks. These patients completed 14 and 86 exposures each over 6 and 20 weeks (both patients continued to use the application after the posttreatment assessment). For the entire sample, exposures lasted an average of 7.03 minutes (SD = 2.2; range = 3.79 to 10.77) with an average maximum anxiety rating of 58.89 (SD = 14.5; range 36.33 to 80.48) that decreased by an average of two-thirds (mean = .69; SD = .16; range .37 to .84).
Table 2.
Patient Use of Exposure
| Contacts | Number of Exposure | During Exposure | ||||||
|---|---|---|---|---|---|---|---|---|
| PT# | Sessions | Messages | Total | Session | Session | Duration | Max Anx | % Decrease |
| FTF Tx A |
7 | 0 | 15 | 3 | 12 | 10.77 | 36.33 | 62.31 |
| B | 11 | 0 | 7 | 6 | 1 | 7.48 | 54.86 | 79.25 |
| C | 6 | 0 | 25 | 6 | 19 | 8.53 | 72.64 | 75.71 |
| D | 9 | 0 | 35 | 14 | 21 | 4.68 | 70.63 | 84.16 |
| E | 10 | 0 | 54 | 11 | 43 | 7.02 | 80.48 | 54.74 |
| F | 8 | 0 | 16 | 2 | 14 | 7.20 | 51.56 | 81.35 |
| FTF Total | 8.50 (1.9) | 0.00 (0.00) | 25.33 (17.0) | 7.00 (4.7) | 18.33 (14.0) | 7.61 (2.0) | 61.08 (16.39) | 72.92 (11.8) |
| MC Tx G |
1 | 7 | 86 | 1 | 85 | 6.78 | 53.13 | 78.05 |
| H | 2 | 4 | 14 | 1 | 13 | 3.79 | 51.42 | 36.60 |
| MC Total | 1.50 (0.7) | 5.50 (2.1) | 50.00 (50.9) | 1.00 (0.0) | 49.00 (50.9) | 5.29 (2.1) | 52.28 (1.2) | 57.32 (29.3) |
| Grand Total | 6.75 (3.6) | 1.38 (2.7) | 31.50 (26.6) | 5.50 (4.8) | 26.00 (26.7) | 7.03 (2.2) | 58.88 (14.5) | 69.02 (16.5) |
Number of Exposures: Total = Total recorded exposures, Session = Exposures recorded during a therapy session (through mobile- or web-application), Home = Exposures recorded outside of session times; Max Anx= Average maximum anxiety rating recorded during exposures; % Decrease = Average decrease in anxiety rating recorded during exposures. Individual scores reported for each patient. Means (standard deviations) presented for each condition and the total sample. FTF Tx = Face-to-face therapy. MC Tx = Minimal contact treatment.
Symptom Response
Table 3 presents the symptom measures before and after treatment. All patients that participated in face-to-face therapy sessions were classified as responders (CGI-I of 1 or 2) and showed improvement on the SCAS-C/P. Five out of six were rated as symptom free from the primary diagnosis on the CRS and four out of six received substantially improved PARS scores. Effect sizes comparing pre- to posttreatment scores were large (PARS = 2.98, CGI-S = 2.24, CRS = 4.87, SCAS-C = 2.00, SCAS-P = 3.15). Although both patients with minimal contact reported improvement on the SCAS-C/P, symptom improvement was not apparent on interview measures.
Table 3.
Symptom Response
| PARS | CGI-S | CGI-I | 1°CRS | SCAS-C | SCAS-P | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pt# | Pt | Pre | Post | Pre | Post | Post | Pre | Post | Pre | Post | Pre | Post |
| FTF Tx | ||||||||||||
| A | 13 | 0 | 4 | 1 | 1 | 6 | 0 | 52 | – | 24 | – | |
| B | 14 | 10 | 4 | 4 | 2 | 7 | 0 | 31 | 14 | 33 | 8 | |
| C | 16 | 0 | 4 | 3 | 2 | 8 | 0 | 31 | 21 | 32 | 6 | |
| D | 15 | 0 | 4 | 1 | 1 | 7 | 0 | 23 | 13 | 36 | 21 | |
| E | 15 | 10 | 4 | 2 | 2 | 6 | 4 | 46 | 28 | 24 | 11 | |
| F | 14 | 1 | 5 | 2 | 2 | 7 | 0 | 48 | 15 | 30 | 19 | |
| FTF Total | 14.50 (1.1) | 3.50 (5.1) | 4.17 (0.4) | 2.17 (1.2) | 1.67 (0.5) | 6.83 (0.8) | 0.67 (1.6) | 35.80 (10.7) | 18.20 (6.3) | 31.00 (4.5) | 13.00 (6.7) | |
| G | 14 | 14 | 5 | 3 | 3 | 6 | 4 | 30 | 15 | 37 | 16 | |
| H | 13 | 15 | 4 | 4 | 4 | 4 | 0 | 52 | 38 | 47 | 27 | |
| MC Total | 13.50 (0.7) | 14.50 (0.7) | 4.50 (0.7) | 3.50 (0.7) | 3.50 (0.7) | 5.00 (1.4) | 2.00 (2.8) | 41.00 (15.6) | 26.50 (16.3) | 42.00 (7.1) | 21.50 (7.8) | |
| Grand Total | 14.25 (1.0) | 6.25 (6.7) | 4.25 (0.5) | 2.50 (1.2) | 2.13 (1.0) | 6.38 (1.2) | 1.00 (1.9) | 37.29 (11.1) | 20.57 (9.3) | 34.14 (7.1) | 15.43 (7.6) | |
Individual scores reported for each patient. Means (standard deviations) presented for each condition and the total sample. FTF Tx = Face-to-face therapy. MC Tx = Minimal contact treatment.
Acceptability
All children and parents interviewed recommended use of Anxiety Coach for other families with an anxious child. Table 4 presents predominant themes and selected quotes. The strongest theme was that application helped plan, engage in, and track exposure exercises. This was viewed as a key aspect of anxiety improvement and that the application helped encourage exposure work outside of the therapy sessions. The ease of use of the application was appreciated by patients and parents, though there were some suggestions for technological improvements, including moving it to different mobile device. Use of the application was viewed as helpful in extending treatment beyond and between the therapy appointments. It was viewed as more convenient than therapy appointments, and having important data to enrich therapy appointments, but participants still stated they wanted to meet with their therapist in person along with the application. The study therapists also viewed Anxiety Coach favorably and stated that they were able to incorporate it into their treatment (Table 5). Therapists also saw the application as a useful tool for patients, although they experienced technological problems. Taken together, patient, parent, and therapist data indicates an overall positive experience with Anxiety Coach and a view that it helps encourage and deliver exposure-based anxiety treatment.
Table 4.
Patient and Parent Opinion of Anxiety Coach Application Presented as Predominant Themes and Representative Quotes
| Theme: Application emphasizes and facilitates planning, engaging in, and recording exposures (subthemes of engagement/accountability; exposure reduces anxiety) |
| The app definitely supported the whole idea of the exposure. |
| I thought the [app] was very helpful because it allowed [my child] a way to cope with things and kind of take that responsibility on herself as to “What can I do to help manage this?” And it did help her reduce a lot of those fears that she had overall. |
| Theme: Ease of use (subtheme of privacy, better than writing on paper) |
| I liked that [the app] was simple. There weren’t a lot of buttons and pages and options. It was just straight forward: Here’s all your stuff. |
| Here’s how to go there. It is a great way to organize your thoughts and just try to deal with it…it’s so easy. |
| It was easier to record stuff than if I were to write it on a piece of paper…. using computers is probably easier than writing it all down on paper. |
| Theme: Viewed as helpful adjunct to therapy (convenient, keeps up momentum between appointments, communication to therapist) |
| You definitely don’t want to see [the therapist] every week…. the app was good to say to therapist, “OK, here’s the things I’ve been doing.” |
| It helped for her to go and see [the therapist] every week….the app created new exposures and the majority of the time she did [the exposures] from the app, set goals each week, but I don’t think she would have been doing them or be as accountable if she wasn’t meeting with him every week… |
| Theme: Some technology upgrades and alternate mobile device are recommended |
| Have the app notify you, like, “Oh, this is when you should be doing exposures,” if you set it to a certain time. |
| Say you did an exposure and you forgot to record it, if you wanted to record it later, you have to wait a time to record the next one. Or else it will say that you did this in one minute. Even though you didn’t. |
| Theme: For some, the general education content was viewed as less useful (subthemes more exposure-specific education and motivation/engaging content would be more useful) |
| I guess we didn’t really use (the education part you read through) a lot. |
Table 5.
Therapists’ opinion of Anxiety Coach Application presented as predominant themes and representative quotes
| Theme: Therapists incorporated use of the app into their treatment and viewed it favorably. |
| So I think it’s a nice way of “in the moment” keeping track of things…. It was really helpful that he had a device that could be on-the-go with him…. |
| I would [go in and see if they had done it and entered things] before the child came in for their appointments. Periodically, I would look at it between appointments….It was fairly convenient. |
| Patients appeared to accept and use the technology without excessive effort |
| I think that the app was very user friendly for the patients. They were able to use it, particularly if they took the time to do it. |
| He [the patient] was really excited about the technology part of it. He seemed really happy to have the extra tool. He took to it quickly and it energized him to get started. |
| Recording exposure exercise data in the app is as useful and convenient as paper-and-pencil recording (yet some opportunities to improve tech) |
| I don’t think that there was a notable difference. When you have a paper copy, you get to put your own examples in….you don’t have that option to do it on the portal, or on the app. Overall, I felt that they did as well or even better with the app. |
| The kids probably enjoyed the app and the online a little bit more than paper. At one point, it seemed that if you added things into the fear ladder, that it didn’t necessarily do them in that chronological order from the most difficult to the easiest. |
| Recommendations to optimize flow of data to therapist |
| Set some kind of reminder so the device would pop up every couple days to make sure patients are putting in their log for the day. Or if they haven’t put anything in for a couple days, have it ask about it and maybe there could be a place for patient to respond with a reason. |
| Initially there were some quirks to work through in getting the outside data in… |
Discussion
The current study describes a promising new integrated mobile device and web-based application to improve the effectiveness and efficiency of therapy for childhood anxiety disorders and OCD in community mental health settings. Anxiety Coach is designed to facilitate exposure therapy by clearly communicating the importance of this technique, providing tools to easily administer exposure, and tracking the use of exposure. The potential for Anxiety Coach to provide useful data and be acceptably integrated into therapy was illustrated by the implementation feasibility case series. This preliminary work elicits a few topics for consideration.
To begin with, the symptom improvement with the Anxiety Coach application was large and consistent with previous studies supporting the success of exposure therapy without additional components (Whiteside et al., 2015). As designed, exposure began early in treatment, typically before the third session. Moreover, the interviews with patients and parents suggested that treatment was acceptable. This exposure-focused approach is considerably different from treatment in both research and clinical settings (Ale et al., 2015; Whiteside, Deacon, et al., 2016). As such, therapists are encouraged to incorporate exposure more fully into their practice. For those looking for additional support administering exposure therapy, the usage data suggests that therapists and families were able to use Anxiety Coach to plan and implement exposures within and between sessions. Moreover, youth, parents, and therapists tended to have positive responses to the application. In fact, families tended to prefer the use of technology over paper-and-pencil record keeping and felt that it facilitated engagement between sessions.
Second, the preliminary data from the technical feasibility study demonstrate the potential of automatically collecting data generated from therapist and patient use of treatment tools. The availability of process data (i.e., the quantity and quality of exposures) opens up new possibilities for clinical practice, quality assurance, and research. This process-oriented information (completion of exposure) can be viewed alongside outcome data (anxiety ratings and percent of fear items mastered), to associate lack of improvement with indicators of insufficient engagement. For example, a clinician working with Patient B might theorize that the limited improvement (as noted in Table 3) is attributable to completing an insufficient number of at-home exposures (Table 2), whereas Patient H might need to increase the number and duration of exposures (Table 2). By monitoring process and outcome (as graphed in Figure 1), the therapist becomes aware not only of when symptoms are not improving as expected, but also why.
The clinical use of Anxiety Coach can be further illustrated through a clinical vignette. Patient E1 in the demonstration study was a 12-year-old boy who presented with his parents for treatment of a specific phobia of vomiting, with features of GAD and OCD. During the initial treatment session, the therapist used the computer-based application to provide psychoeducation on the anxiety cycle. The family benefitted most notably from the conceptualization of thoughts and bodily sensations as triggers for anxiety. The therapist and family also built a fear ladder that included items for thought, in vivo, and interoceptive exposures. The family indicated their understanding of how parent-coached exposures reduces anxiety and left the appointment eager to begin exposures. This enthusiasm, particularly by parents, was apparent in the 13 exposures recorded by the family during the 2 weeks leading up to the second session. However, the family was disappointed that the exposures did not appear to be helpful, reflected in the ratings of symptom severity which remained unchanged. Upon review, the therapist noted that although the exposures averaged 50% decrease in anxiety ratings, they were generally short (approximately 4 minutes) and to a wide variety of items from the fear ladder. Based on this information and discussion with the family, the therapist encouraged patience in the pace of symptom change and completion of exposures, as well as a focus on completing longer exposures to a smaller number of items. The therapist then led an exposure to dirty surfaces that the child feared would lead to vomiting, demonstrating that remaining with an exposure for a longer duration (15 minutes) can lead to greater decrease in anxiety (76%).
The family attended 8 additional treatment sessions, each of which began with a review of home exposures, completion of an in-session exposure, and planning for the next week. Following Session 2, the family responded to the therapist’s direction by completing two exposures of greater than 10 minutes duration with an average decrease in anxiety of 70%. Beginning in the 3rd session the therapist had the patient’s father participate in coaching the in-session exposure. By the 5th session, the family was frequently conducting exposures of 10 to 20 minutes in duration, but were frustrated because some of the exposures did not lead to decrease in anxiety and the symptom severity ratings had remained relatively unchanged. A review of the recent symptoms and exposures suggested that the patient’s progress was likely hindered by frequent reassurance seeking from parents. The therapist and family created a structured behavior plan to encourage independence with exposures and to decrease reassurance seeking. By Session 7 the family reported a significant decrease in reassurance seeking and the first substantial decrease in symptom severity. Beginning in Session 8, the therapist began planning for termination by helping the family transition from structured planned exposure to handling anxiety-provoking situations as they arose during daily life. By the 10th session, the family’s severity ratings were in the low range, 80% of the items on the fear ladder were mastered, the patient was not asking for reassurance, and the family felt confident they could manage anxiety as it arose (consistent with the fact that exposures routinely resulted in greater than 80% decrease in anxiety). The family was encouraged to return as needed and therapy was ended.
In addition to informing therapeutic decision, by aggregating process and outcome data over multiple patients and therapists (as in Table 1), the information can be used to monitor quality over time. For example, while Therapist A appears to have used exposures early in treatment and in the vast majority of sessions, Therapist C introduced exposure later and used it in only a third of sessions. This objective data could guide a clinical supervisor’s discussion of the evidence-based treatment of childhood anxiety disorders, setting of specific behavioral goals, and monitoring progress. Because these goals are process-focused (i.e., use of exposures) as opposed to goal-focused (i.e., symptom improvement), they are within the therapist’s control. Moreover, because use of digital tools (regarding exposure or other techniques) automatically collects an unprecedented amount of information, such instruments could help researchers study therapist fidelity, patient engagement, and treatment dismantling.
The pilot study demonstrates the potential for Anxiety Coach to facilitate the implementation of exposure during therapy. Specifically, child engagement in exposures is supported by parents, while the family’s engagement in exposure with the application is supported by the therapist, and therapist engagement is supported by a supervisor. However, the current paper does not test the effectiveness of the application to achieve these goals and future research needs to examine whether Anxiety Coach is acceptable, increases the use of exposure, and improves outcomes when used by nonexpert therapists in community settings, as well as by more culturally and economically diverse patient populations with limited access to mental health care. Moreover, in contrast to patients who received face-to-face treatment, those with minimal contact and remote monitoring had limited success and patients commented on a preference for direct contact. Thus, further work needs to be done to determine whether the structure and data provided by Anxiety Coach can enhance engagement with limited direct therapist contact and whether this model is feasible for practicing therapists (i.e., billing for remote monitoring).
Finally, technical enhancements are needed to address issues that interfered with data collection or were identified by patients or therapists. For example, adding the ability to record exposures after their completion and to mark fear ladder items as mastered without doing an exposure could reduce the recording of exposures of very short durations and improve usability. Similarly, reminders viewable when the application is closed, automatically stopping the exposure timer after a period of inactivity, and requiring completion of exposures that are started could eliminate the recording of inaccurately long exposures. Because therapists can view the details of exposures (e.g., durations), they likely can identify recorded exposures that are affected by these issues; however, user experience and data aggregation need to be improved through such enhancements. Other modifications suggested by therapists include reminders for patients to engage with the application, more flexibility to customize the target of an exposure during administration, and more interactive psychoeducation.
In sum, this initial work suggests promise for the Anxiety Coach application to engage children and their parents in completion of in-session and between-session exposures, and to collect meaningful data on therapist and patient use of exposures. Use of the application and associated treatment approach was viewed positively by patients and parents. Future studies are indicated to test the potential of the technology to increase access to evidence-based treatment.
Acknowledgments
This project was supported by a grant from the National Institute for Mental Health, 1R34MH100468–0. The first author, Dr. Whiteside, and Mayo Clinic receive royalties from the sale of the Mayo Clinic Anxiety Coach mobile application.
Footnotes
Case vignette is based upon study participant with changes and additions to protect confidentiality and enhance illustrative value.
References
- AACAP. (2007). Practice parameter for the assessment and treatment of children and adolescents with anxiety disorders. Journal of American Academy of Child and Adolescent Psychiatry, 46, 267–283. [DOI] [PubMed] [Google Scholar]
- Albano AM, & Silverman WK (1996). Anxiety Disorders Interview Schedule for DSM-IV Child Version: Clinical Manual. Boulder, CO: Graywind Publications. [Google Scholar]
- Ale CM, McCarthy DM, Rothschild L, & Whiteside S (2015). Components of cognitive behavioral therapy related to outcomein childhood anxiety disorders. Clinical Child and Family Psychology Review, 18, 240–251. 10.1007/s10567-015-0184-8 [DOI] [PubMed] [Google Scholar]
- Anderson JC (1994). Epidemiological issues. In Ollendick TH, King NJ, & Yule W (Eds.), International handbook or phobic and anxiety disorders in children and adolescents (pp. 43–65). New York: Plenum Press. [Google Scholar]
- Beesdo K, Knappe S, & Pine DS (2009). Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America, 32, 483–524. 10.1016/j.psc.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carper MM (2017). Thinking about exposures? There’s an app for that! Cognitive and Behavioral Practice, 24(1), 121–127. 10.1016/j.cbpra.2016.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita BF, & Southam-Gerow MA (2006). Fears and anxieties. In Mash EJ & Barkley RA (Eds.), Treatment of child disorders (3rd ed., pp. 271–335). New York: Guilford. [Google Scholar]
- Guy W (1976). Clinical global impressions ECDEU assessment manual for psychopharmacology (Revised). (pp. 217–221). Rockville: MD: National Institute of Mental Health. [Google Scholar]
- Higa-McMillan CK, Francis SE, Rith-Najarian L, & Chorpita BF (2016). Evidence base update: 50 years of research on treatment for child and adolescent anxiety. Journal of Clinical Child and Adolescent Psychology, 45(2), 91–113. 10.1080/15374416.2015.1046177 [DOI] [PubMed] [Google Scholar]
- Hsieh H-F, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. [DOI] [PubMed] [Google Scholar]
- James A, James G, Codrey F, Soler A, & Choke A (2013). Cognitive behavioural therapy for anxiety disorders in children and adolescents (Review). Cochrane Database of Systematic Reviews, Issue 6. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, & Blase SL (2011). Rebooting Psychotherapy Research and Practice to Reduce the Burden of Mental Illness. Perspectives on Psychological Science, 6, 21–37. [DOI] [PubMed] [Google Scholar]
- Mendlowicz MV, & Stein MB (2000). Quality of life in individuals with anxiety disorders. American Journal of Psychiatry, 157(5), 669–682. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Brody D, Fisher PW, Bourdon K, & Koretz DS (2010). Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics, 125(1), 75–81. 10.1542/peds.2008-2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Cuijpers P, & Lehman K (2011). Supportive accountability: A model for providing human support to enhance adherence to eHealth interventions. Journal of Medical Internet Research, 13(1), e30. 10.2196/jmir.1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, & Bogie N (2002). Three traditional and three new childhood anxiety questionnaires: Their reliability and validity in a normal adolescent sample. Behaviour Research & Therapy, 40, 753–772. [DOI] [PubMed] [Google Scholar]
- Muris P, Schmidt H, & Merckelbach H (2000). Correlations among two self-report questionnaires for measuring DSM-defined anxiety disorder symptoms in children: The Screen for Child Anxiety Related Emotional Disorders and the Spence Children’s Anxiety Scale. Personality & Individual Differences, 28, 333–346. [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health, 42(5), 533–544. 10.1007/s10488-013-0528-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton MQ (2002). Qualitative research and evaluation methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Quilty LC, Van Ameringen M, Mancini C, Oakman J, & Farvolden P (2003). Quality of life and the anxiety disorders. Journal of Anxiety Disorders, 17(4), 405–426. [DOI] [PubMed] [Google Scholar]
- RUPP (2002). Fluvoxamine for the treatment of anxiety disorders in children and adolescents. The Research Unit on Pediatric Psychopharmacology Anxiety Study Group. The New England Journal of Medicine, 344(17), 1279–1285. 10.1056/NEJM200104263441703. [DOI] [PubMed] [Google Scholar]
- Spence SH (1998). A measure of anxiety symptoms among children. Behaviour Research & Therapy, 36, 545–566. [DOI] [PubMed] [Google Scholar]
- Weber RP (1990). Basic content analysis. Newbury Park, CA: Sage Publications. [Google Scholar]
- Whiteside SP (2016). Mobile device-based applications for childhood anxiety disorders. Journal of Child and Adolescent Psychopharmacology, 26(3), 246–251. 10.1089/cap.2015.0010 [DOI] [PubMed] [Google Scholar]
- Whiteside SPH, Ale CM, Vickers Douglas K, Tiede MS, & Dammann JE (2014). Case examples of enhancing pediatric OCD treatment with a smartphone application. Clinical Case Studies, 13, 80–94. [Google Scholar]
- Whiteside SPH, Ale CM, Young B, Dammann J, Tiede MS, & Biggs BK (2015). The feasibility of improving CBT for childhood anxiety disorders through a dismantling study. Behaviour Research and Therapy, 73, 83–89. 10.1016/j.brat.2015.07.011 [DOI] [PubMed] [Google Scholar]
- Whiteside SPH, Deacon BJ, Benito K, & Stewart E (2016). Factors associated with practitioners’ use of exposure therapy for childhood anxiety disorders. Journal of Anxiety Disorders, 40, 29–36. 10.1016/j.janxdis.2016.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteside SPH, Sattler A, Ale CM, Young B, Hillson Jensen A, Gregg MS, & Geske JR (2016). The use of exposure therapy for child anxiety disorders in a medical center. Professional Psychology: Research and Practice, 47, 206–214. 10.1037/pro0000077 [DOI] [Google Scholar]
- Wood JJ, Piacentini JC, Bergman RL, McCracken J, & Barrios V (2002). Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. Journal of Clinical Child and Adolescent Psychology, 31(3), 335–342. [DOI] [PubMed] [Google Scholar]