Abstract
Background:
Spinal cord injury (SCI) is a debilitating disorder with dysfunction in daily activities and psychological consequences like anxiety as well as depression impacting the quality of life substantially. Existing treatments focus mainly on rehabilitation, symptom reduction, and secondary complications. However, psychological, social, and existential issues are least addressed in the prevailing models.
Aims:
To study the role of meditation in addressing psychological impairment and any resultant improvement in functional outcomes in SCI patients.
Methods:
Nonrandomized controlled study was conducted in a tertiary care center for SCI patients. Hospital inpatients were recruited into either experimental intervention group (add on easy rāja yoga with conventional rehabilitation-ER n = 50) or control intervention group (conventional rehabilitation alone-CR n = 50). Patients in the ER group received easy rāja yoga for 1 month, along with conventional rehabilitation and the CR group patients received only conventional rehabilitation. All the subjects were assessed for psychological (perceived stress scale [PSS], Hospital Anxiety and Depression Scale [HADS]) and functional impairment (spinal cord independence measure (SCIM), numeric pain rating (NPR) and WHO quality of life-BRIEF (WHOQOLBREF)] at baseline and after 1 month.
Results:
After 1 month of add-on easy rāja yoga, there was significant decrease in the scores of HADS (F[1,88] = 272.92, P < 0.001), PSS (F[1,88] = 274.41, P < 0.001) and NPR (F[1,88] = 60.60, P < 0.001) and significant increase in the scores of WHOQOLBREF (F[1,88] = 349.94, P < 0.001) and SCIM (F[1,88] = 29.09, P < 0.001) in the ER group compared to CR group in analysis of covariance.
Conclusion:
One-month add-on easy rāja yoga improves psychological and functional outcomes (HADS, PSS, NPR, WHOQOLBREF and SCIM) in patients with SCI. Future studies with robust designs are needed to validate the results.
Keywords: Psychological and functional impairment, rāja yoga, spinal cord injury
Introduction
Spinal cord injury (SCI) is a debilitating disorder with impairment in motor, sensory, and autonomic functions and it is very commonly caused by trauma. Every year millions of people sustain SCI globally.[1] People with SCI are predominantly in the age group of 20–40 years-relatively the most productive time of life. People with SCI are two to five times more likely to die prematurely than people without SCI.[1] Adding to the acute impairments, secondary health problems such as pressure sore, sepsis, respiratory muscle impairment, etc., increases the cost of management enormously. Due to direct and indirect cost of management, including long-term rehabilitation, psychological and social problems are also very common and make the condition more complex.
Difficulty in carrying out activities of daily living independently due to the neuromuscular compromise and the ensuing psychological and social distress affects the quality of life considerably. A recent study has shown that 17%–25% of the people with SCI are prone to develop psychological disorders[2] and >36% of them were prescribed psychotropic medications,[2] A metanalysis of 19 studies had shown a depression prevalence of 22.2% following SCI.[3] Chronic pain, fatigue, depressed mood, anxiety, and reduced self-efficacy following SCI are also reported in the literature.[4]
After acute management of SCI, rehabilitative and preventive management is the mainstay of care for people with SCI for successful reintegration of psychological and social life. Optimal management of physical and psychological impairment following SCI should go parallelly, as physical and psychological factors influence each other. For example, inadequate management of chronic pain could lead to depression, which in turn could worsen chronic pain.[5] Hence the need for a multidisciplinary management team including surgeons, physicians, physiotherapist, nurses, occupational therapist, dietician, psychologists, etc., is of paramount importance. In fact, the long-term outcome of quality of life is inversely proportional to the quality of care.[2]
Prevailing rehabilitation models focus on symptom reduction, optimizing functional outcomes, and prevention of secondary health problems like pressure sore, spasticity of muscles, etc., and their functional consequences. But as the problems related to SCI are complex involving psychological, social, and existential factors, it is imperative to explore applications of complementary therapies along with conventional treatment to strengthen the patient as an individual in a holistic way.
In recent times, besides conventional care, mind-body practices like yogasana, pranayama and meditation are found to be helpful in managing the physical, psychological, and social distress in people with SCI.[6,7] Among people with SCI, complementary and integrative health interventions usage is reported to be 14% to 73%, and 3% of SCI patients use them in the first few weeks of inpatient rehabilitation.[8] Patients receiving complementary therapies had shown greater reductions in pain severity and improvement in the quality of life and measures related to activities of daily living.[8]
Mind-body practices used in therapeutic setup range widely from physical movement-based therapies like yogasana, tai chi, Qi Gong to mental focusing or observation related practices like mindfulness, sahaj yoga, rāja yoga, etc.[9] For patients with SCI who are mostly paraplegic or tetraplegic, though movement-based practices like yogasana and pranayama would help due to improved body and breath awareness, meditation-based practices would play an apt role to improve the psychological functioning and related outcomes. Indeed, improvement in psychological functioning would reflexively improve physical functioning also, as physical and psychological factors influence each other.
In this study, we have evaluated the effect of Brahmakumaris Rāja yoga (also called as easy rāja yoga) on patients with SCI. Easy rāja yoga is meditation technique with a framework of four different limbs comprising of (i) wisdom (gyān), (ii) remembrance (yog), (iii) practice of virtues (dhārana) and (iv) service i.e., to have good wishes for self and others (seva). The terms yoga and dharana used here is meant differently from that used commonly in ashtnānga yoga. For complete details of the easy rāja yoga module, refer the appendix. Easy rāja yoga has been used in various conditions like coronary heart disease, tension headache, for depression and anxiety in patients undergoing coronary artery bypass surgery, substance abuse, and diabetes mellitus.[10,11,12]
In this study, we aimed at evaluating the effect of Easy rāja yoga on psychological and functional outcomes of patients with SCI. Our primary hypothesis was that 1-month practice of easy rāja yoga would reduce anxiety and depression in patients with SCI measured by Hospital Anxiety and Depression Scale (HADS) and stress measured by the perceived stress scale (PSS). Further, we also hypothesized that 1-month practice of easy rāja yoga would improve functional independence measure assessed by spinal cord independence measure (SCIM) and quality of life assessed by WHO quality of life-brief (WHOQoLBREF) and would reduce pain measured by numeric pain rating (NPR) Scale.
Methods
Non-randomized controlled trial was conducted at a tertiary care SCI centre in north India. The study was approved by the institutional ethics committee (REF ISIC/IIRS/RP/2015/111). Acute and Chronic SCI patients (n = 100, 50 in each arm) admitted in the hospital and undergoing treatment and rehabilitation were recruited based on eligibility and their willingness to participate in the trial with written informed consent. Based on patients' choice, subjects were recruited by the consultant in the treating team to either experimental intervention group (add on easy rāja yoga with conventional rehabilitation-ER) or control intervention group (conventional rehabilitation alone-CR). All the subjects continued with their conventional treatment as prescribed by the treating team. Patients' unwillingness to participate in the study had no impact on regular treatment.
SCI patients in the age group of 16–60 years of either sex, either tetraplegic or paraplegic, with ability to understand the instructions were recruited. Patients who cannot sit for at least 30–45 min; expected to discharge within 1 month; with polytrauma; critically ill requiring life support measures like ventilator were excluded.
Patients in the ER group were taught a structured, easy rāja yoga module by a qualified easy rāja yoga teacher for 1 month along with conventional rehabilitation, and the CR group patients were given only conventional rehabilitation delivered by a multidisciplinary team including physician/surgeon, nurse, psychologist, physiotherapist, occupational therapist, peer counselor and dietician. All subjects were assessed at the beginning and end of 1 month with the following measures. Baseline and post data were collected by a trained physiotherapist who was not involved in recruitment or statistical analysis of the data.
Hospital anxiety and depression scale
Zigmond and Snaith originally developed this scale in 1983 to determine the levels of anxiety and depression among hospitalized patients.[13] It is a fourteen-item scale with seven items for anxiety and other seven items for depression. The total HADS score may be regarded as a global measure of psychological distress. It's a self-rated scale. Higher score represents higher anxiety and depression.
Perceived stress scale
Sheldon Cohen developed the PSS in 1983.[14] It evaluates the intensity of stress perceived by the individual in real-life situations in the last 1 month. Scores are made on a Likert scale ranging from 0 to 4. Higher score represents higher perceived stress. It is a valid and reliable tool used across disorders and in healthy population.
Spinal cord independence measure
This is a disability scale which describes the ability of person with SCI to accomplish their daily routine activities and functional assessments of this population.[15] This tool is more sensitive to capture the change following any intervention and hence commonly used in clinical trials. It has four sub-scales measuring (i) self-care, (ii) respiration and sphincter management, (iii) mobility in room and toilet and (iv) mobility indoors and outdoors. SCIM-III is the latest version and comprises 19 items score ranges from 0 to 100. Change in score of SCIM III over a period of time reflects functional change overall in a person with SCI.
WHO quality of life-BREF
The WHOQOL-BREF is the short version of WHOQOL-100 developed by the WHOQOL group.[16] It has 26 items measuring four domains comprising of physical health, psychological health, social and environmental health. It is a self-administered scale with scores ranging from 4 to 20 (after transformation for comparability with WHOQOL-100 scores). This scale is used across disorders and in a healthy population to assess the quality of life.
Numeric pain rating
It is a uni-dimensional measure of pain intensity in adults. The NPRS is a visual analog scale in which a respondent selects a number from segmented numeric scale with scores from zero to ten that show the intensity of his/her pain.
Socio-demographic data and the data of different variables measured were coded and entered in an excel sheet. Continuous data such as PSS, HADS, QOL, SCIM, and NPR were tested for normality using the Shapiro–Wilk test. For baseline comparison between groups, t-test for two independent sample mean was used for continuous variables and Chi-square test was used for categorical variables. Analysis of covariance (ANCOVA) was performed with baseline assessment as covariate and intervention group as between factor for comparing the postassessment. The coded data were analyzed by a statistician blind to the intervention using the software? Jamovi 1.2, Amsterdam, Netherlands.[17]
Results
Out of 150 patients approached, 100 agreed to participate in the study, with 50 in ER group and 50 in the CR group allotted as per patients' choice. Among the ER group four patients dropped as they got discharged early and from the CR group five patients dropped (unable to trace contact). There were 46 patients in ER group and 45 patients in the CR group available for analysis. An overview of the study flow is given in Figure 1.
Figure 1.
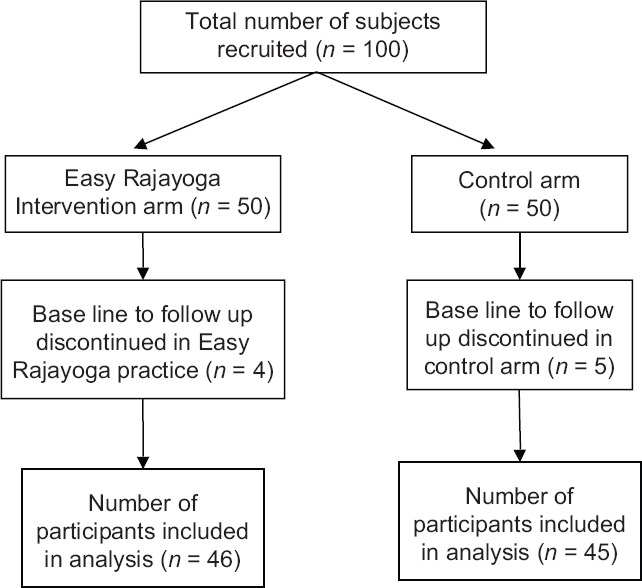
Outline of study flow
Baseline data were compared for both the groups and details are given in Table 1.
Table 1.
Group-wise baseline data
| Variables | Intervention (n=46) | Control (n=45) | t/χ2 |
|---|---|---|---|
| Age (years) | 31.19 (10.36) | 34.48 (12.48) | −1.37 |
| Sex ratio (male:female) | 36:10 | 41:4 | 2.88 |
| Married:single | 26:20 | 28:17 | 0.30 |
| Years of education | 13.20 (3.13) | 13.31 (3.66) | −0.16 |
| PSS | 29.98 (6.220) | 26.51 (6.622) | 2.57* |
| HADS | 28.41 (7.308) | 24.02 (8.341) | 2.67** |
| QOL | 48.91 (12.207) | 55.89 (13.074) | −2.63* |
| NPR | 4.78 (3.076) | 4.40 (3.165) | 0.58 |
| SCIM | 31.76 (15.571) | 38.84 (17.272) | −2.05* |
*P<0.05; **P<0.01; ***P<0.001. Values within bracket are standard deviation and outside bracket are mean. PSS=Perceived stress scale, HADS=Hospital anxiety and depression scale, SCIM=Spinal cord independence measure, NPR=Numeric pain rating, WHOQOLBREF=WHO quality of life
Data were tested for normality and found to be normally distributed. As there was significant difference at baseline for all the variables except NPR, data were analyzed with ANCOVA with baseline assessment as covariate and intervention group as between factor for comparing the post assessment [Table 2]. Following 1-month easy rāja yoga practice, there was significant decrease in the scores of HADS (F(1,88) = 272.92, P < 0.001), PSS (F[(,88) = 274.41, P < 0.001) and NPR (F(1,88) = 60.60, P < 0.001) and significant increase in the scores of WHOQOLBREF (F(1,88) = 349.94, P < 0.001) and SCIM (F(1,88) = 29.09, P < 0.001) in the ER group compared to CR group.
Table 2.
Pre-post comparison (analysis of covariance)
| Variable | Group | Mean (SD) |
F (df) | Partial η2 | |
|---|---|---|---|---|---|
| Pre | Post | ||||
| PSS | Intervention | 29.98 (6.220) | 12.22 (4.412) | 274.41*** (1,88) | 0.757 |
| Control | 26.51 (6.622) | 25.40 (6.580) | |||
| HADS | Intervention | 28.41 (7.308) | 8.72 (3.828) | 272.92*** (1,88) | 0.756 |
| Control | 24.02 (8.341) | 22.29 (7.754) | |||
| QOL | Intervention | 48.91 (12.207) | 87.87 (7.265) | 349.94*** (1,88) | 0.799 |
| Control | 55.89 (13.074) | 59.22 (12.954) | |||
| NPR | Intervention | 4.78 (3.076) | 1.20 (1.572) | 60.60*** (1.88) | 0.408 |
| Control | 4.40 (3.165) | 3.56 (2.590) | |||
| SCIM | Intervention | 31.76 (15.571) | 46.74 (17.085) | 29.09*** (1,88) | 0.248 |
| Control | 38.84 (17.272) | 44.20 (17.981) | |||
*P<0.05, **P<0.01, ***P<0.001. PSS=Perceived stress scale, HADS=Hospital anxiety and depression scale, SCIM=Spinal cord independence measure, NPR=Numeric pain rating, WHOQOLBREF=WHO quality of life
We also performed post hoc subgroup analysis for the level of injury (paraplegia and tetraplegia) and type of injury (acute SCI and chronic SCI). Subgroup analysis was performed with difference scores (pre minus post) to test for the group difference between ER group and CR group. As the data were found to be normal with Shapiro-Wilk test, independent t-test was performed. Both paraplegia and tetraplegia patients who were in the ER group improved significantly (P < 0.001) [Table 3] than the CR group subjects in PSS, HADS, SCIM, NPR and WHOQOLBREF, though the change in paraplegia patients was more than tetraplegia patients. Similarly, both acute and chronic SCI patients who were in the ER group improved significantly (P < 0.001) [Table 4] than the CR group in PSS, HADS, SCIM, NPR, and WHOQOLBREF, though acute SCI patients responded with greater change in scores than chronic SCI patients.
Table 3.
Comparison between intervention and control group for paraplegia and tetraplegia (t values are from independent t-test for difference (pre-post) scores
| Variables | Paraplegia |
Tetraplegia |
||||
|---|---|---|---|---|---|---|
| Intervention (n=22) | Control (n=29) | t | Intervention (n=24) | Control (n=16) | t | |
| PSS | ||||||
| Pre | 30.1 (6.0) | 25.8 (6.2) | −13.54*** | 29.8 (6.5) | 27.9 (7.3) | −9.43*** |
| Post | 12.4 (4.5) | 24.6 (7.0) | 12.1 (4.4) | 26.9 (5.7) | ||
| HADS | ||||||
| Pre | 27.9 (7.8) | 23.7 (8.2) | −12.71*** | 28.9 (7.2) | 24.6 (8.8) | −8.10*** |
| Post | 7.9 (3.8) | 21.6 (7.4) | 9.5 (3.8) | 23.5 (8.6) | ||
| SCIM | ||||||
| Pre | 43.7 (13.2) | 47.9(14.4) | 4.59*** | 20.8 (7.5) | 22.3 (5.9) | 4.82*** |
| Post | 62.1 (8.9) | 54.7 (13.1) | 32.6 (7.9) | 25.3 (5.8) | ||
| NPR | ||||||
| Pre | 4.9 (3.1) | 4.2 (3.0) | −4.80*** | 4.7 (3.1) | 4.8 (3.5) | −3.76** |
| Post | 0.95 (1.5) | 3.4 (2.3) | 1.4 (1.6) | 3.9 (3.1) | ||
| QOL | ||||||
| Pre | 50.4 (11.1) | 58.3 (13.8) | 15.81*** | 47.6 (13.2) | 51.4 (10.6) | 10.21*** |
| Post | 89.4 (7.8) | 62.1 (13.2) | 86.5 (6.6) | 54.1 (11.0) | ||
*P<0.05, **P<0.01, ***P<0.001. Values within bracket are standard deviation and outside bracket are mean. PSS=Perceived stress scale, HADS=Hospital anxiety and depression scale, SCIM=Spinal cord independence measure, NPR=Numeric pain rating, WHOQOLBREF=WHO quality of life
Table 4.
Comparison between intervention and control group for acute and chronic patients (t values are from independent t-test for difference (pre-post) scores
| Variables | Acutey |
Chronic |
||||
|---|---|---|---|---|---|---|
| Intervention (n=23) | Control (n=21) | t | Intervention (n=23) | Control (n=24) | t | |
| PSS | ||||||
| Pre | 30.6 (5.9) | 28.8 (5.9) | −11.56*** | 29.4 (6.5) | 24.50(6.6) | −10.67*** |
| Post | 12.4 (4.0) | 26.9 (5.5) | 12.0 (4.8) | 24.0 (7.2) | ||
| HADS | ||||||
| Pre | 29.4 (6.4) | 27.8 (6.5) | −12.99*** | 27.5 (8.1) | 20.7 (8.5) | −9.47*** |
| Post | 8.7 (3.6) | 24.6 (5.4) | 8.7 (4.1) | 20.3 (8.9) | ||
| SCIM | ||||||
| Pre | 33.6 (16.9) | 33.9(13.9) | 4.28*** | 29.9 (14.1) | 43.1(18.9) | 3.89** |
| Post | 50.3 (16.0) | 41.1(14.9) | 43.2 (17.7) | 46.9(20.2) | ||
| NPR | ||||||
| Pre | 4.7 (3.1) | 3.8 (2.9) | −4.44*** | 4.8 (3.1) | 4.9 (3.3) | −3.80*** |
| Post | 0.8 (1.3) | 2.9 (2.3) | 1.6 (1.7) | 4.1 (2.7) | ||
| QOL | ||||||
| Pre | 47.0 (10.6) | 51.9(10.3) | 15.94*** | 50.8 (13.6) | 59.4 (14.4) | 10.63*** |
| Post | 87.4 (6.5) | 57.6 (9.8) | 88.3 (8.1) | 60.3 (15.3) | ||
*P<0.05, **P<0.01, ***P<0.001. Values within bracket are standard deviation and outside bracket are mean. PSS=Perceived stress scale, HADS=Hospital anxiety and depression scale, SCIM=Spinal cord independence measure, NPR=Numeric pain rating, WHOQOLBREF=WHO quality of life
Discussion
Study results show that 1-month practice of easy rāja yoga helps patients with SCI in reducing depression, anxiety, stress, pain, and enhancing functional independence and quality of life. The results are concurrent with previous studies with mind-body interventions like yogasana, pranayama, and meditation.[7,8] The results also confirm our primary and secondary hypotheses.
Reduction in anxiety, depression, and stress-related symptoms with mind-body intervention has been reported in SCI patients in few recent studies.[7,8] It is worth exploring further the possible mechanisms to guide clinicians for these techniques to be applied in bedside practice along with conventional treatment strategies. It would help in avoiding/reducing the prescription of psychotropics for anxiety and depression, which are obviously secondary to the mental trauma following SCI. It would also reduce the burden of psychological distress cascading into social burden in the form of caregivers' stress. Moreover, improving psychological functions would also reduce the mental stress and hence the pain and related consequences like muscle spasticity due to downregulation of hypothalamo-pituitary-adrenal axis stress pathway. One of the key components in easy rāja yoga is practicing soul consciousness with self-respect (swamān). This could have mediated increase in self-esteem and hence reduction of depressive symptoms. Many studies in the past had reported the predictive role of self-esteem in depression.[18,19]
Reduction of pain in chronic pain disorders is one of the robust evidence available for the effect of mind-body interventions, especially in low back pain.[20,21] Though the mechanisms behind this effect are not clear, this is one of the consistent findings. Previous studies too have documented reduced pain in patients with SCI.[6,22] In this study, reduction in pain score following easy rāja yoga could be due to the practice of sakshi bhav (equanimity), which is integral to easy rāja yoga. Sakshi bhav is a mental state where one consciously witnesses the pleasant and unpleasant happenings (either in the body, mind or social relations) as it unfolds.[23] Sakshi bhav though similar to mindfulness, is different in many aspects, especially the context with which it is practiced in rāja yoga. The understandings required for the practice of sakshi bhav in rāja yoga are as follows:
Peace and positivity are our original nature; pain, suffering, and all negative emotions are acquired due to ignorance of our original nature of positivity. Hence anchoring ourselves to our original nature enables to stop reacting to the pain and suffering in the body, mind, or social relations
Everything in this universe, both matter and nonmaterial beings (like soul), pass through the stages of sato, rajo and tamo. Pain and suffering are the indications of tamo stage prevailing all around. Understanding this Universal flow equips one to realize the need for creating the positive feeling in the self (i.e., recreating a sato stage) instead of getting struck with the question of why me? It empowers one to perform the subtle but powerful actions of right thinking and creating pleasant feelings instead of entangling in the vicious cycle of pain and suffering. It gives a sense of hope by consciously keeping away from the trauma created by the past
The supreme/Universal being (conceptualized as a Divine point of light) is a wonderful source of positive energy, as He is away from the effect of past, present, and future. Focusing on this Divine energy, which is actually called yoga in eastern scriptures, would encourage one to inculcate the virtue of equanimity or sakshi bhav with ease.
Improvement in quality of life and functional independence could be due to the profound psychological and spiritual impact of easy rāja yoga on thoughts, emotions, and behavior of the patients. Similar to other established psychosocial interventions such as cognitive behavioral therapy, coping effectiveness training, and pain management program,[24] easy rāja yoga could also be one of the psychosocial intervention programs for SCI patients, especially in the eastern population. As psychological stress could influence cognition, affect and behavior, including physical functioning of an individual,[25,26] so could positive and elevated spiritual thoughts impact the triad of cognition, affect, and conation. Recent studies have shown improvement of real-world functioning socially and occupationally with mind-body interventions possibly mediated by the experience of well-being due to positive thoughts and feelings.[27,28] Some studies have found improvement in musculoskeletal functions like improved posture and gait balance, reduced spasticity following mind-body practices in disorders like Parkinson, and multiple sclerosis supporting this notion.[29,30,31,32] Apart from the indirect effect of psychological factors affecting physical process in mind-body practices, studies have also shown meditation and lifestyle modification directly affect the body causing structural changes like increased cortical thickness and reduced telomere shortening.[33,34,35]
Though the study results are encouraging, there are several limitations of this study. Being a nonrandomized controlled trial, results need to be tested further in a planned randomized controlled trial to avoid bias in the selection and recruitments of the subjects, which impacts the results considerably. All rating scales used in this study were self-rated except SCIM.
Self-rated scales have the merit of capturing outcome responses as close to subjects' experience as possible but at the cost of social desirability bias leading to type 1 error very commonly. Though most of the SCI patients develop depression and anxiety, systematic evaluation of depression to qualify syndromal depression was not done. Only s?hort-term effect is demonstrated in this study. Whether the effects would persist for longer duration needs to be tested in future long term follow-up studies. Investigating inflammatory and cognitive biomarkers would add more validity to the results to support the psychological findings. Easy rāja yoga intervention was delivered at the hospital setup. Whether it could be translated in a community set up after the patients get discharged needs to be explored further. Future trials could focus more on the afore-mentioned limitations and explore the possible biological mechanisms for the available evidence of efficacy.
Conclusion
One-month add on easy rāja yoga improves psychological and functional outcomes in patients with SCI along with improvement in the quality of life and subjective measure of pain. Further studies with the robust design are required to validate the efficacy of easy rāja yoga on psychological and functional outcomes. Possible biological mechanisms also need to be studied systematically for its applications in clinical set up.
Ethical clearance
The study was approved by the institutional ethics committee (REF ISIC/IIRS/RP/2015/111).
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Spinal Cord Injury. [Last accessed on 2020 Sep 04]. Available from: https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury .
- 2.Craig A, Nicholson Perry K, Guest R, Tran Y, Dezarnaulds A, Hales A, et al. Prospective study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabil. 2015;96:1426–34. doi: 10.1016/j.apmr.2015.02.027. [DOI] [PubMed] [Google Scholar]
- 3.Williams R, Murray A. Prevalence of depression after spinal cord injury: A meta-analysis. Arch Phys Med Rehabil. 2015;96:133–40. doi: 10.1016/j.apmr.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 4.Craig A, Tran Y, Wijesuriya N, Middleton J. Fatigue and tiredness in people with spinal cord injury. J Psychosom Res. 2012;73:205–10. doi: 10.1016/j.jpsychores.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy P, Hasson L. The relationship between pain and mood following spinal cord injury. J Spinal Cord Med. 2017;40:275–9. doi: 10.1080/10790268.2016.1147680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Curtis K, Hitzig SL, Leong N, Wicks C, Ditor DS, Katz J. Evaluation of a modified yoga program for persons with spinal cord injury. Ther Recreation J. 2015;49:97. [Google Scholar]
- 7.Madhusmita M, Ebnezar J, Srinivasan TM, Mohanty PP, Deepeshwar S, Pradhan B. Efficacy of yoga as an add-on to physiotherapy in the management of patients with paraplegia: Randomised controlled trial. J Clin Diagn Res. 2019;13:KC01–6. [Google Scholar]
- 8.Taylor SM, Cheung EO, Sun R, Grote V, Marchlewski A, Addington EL. Applications of complementary therapies during rehabilitation for individuals with traumatic Spinal Cord Injury: Findings from the SCIRehab Project. J Spinal Cord Med. 2019;42:571–8. doi: 10.1080/10790268.2018.1481693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wahbeh H, Elsas SM, Oken BS. Mind-body interventions: Applications in neurology. Neurology. 2008;70:2321–8. doi: 10.1212/01.wnl.0000314667.16386.5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta SK, Sawhney RC, Rai L, Chavan VD, Dani S, Arora RC, et al. Regression of coronary atherosclerosis through healthy lifestyle in coronary artery disease patients—Mount Abu Open Heart Trial. Indian Heart J. 2011;63:461–9. [PubMed] [Google Scholar]
- 11.Kiran U, Ladha S, Makhija N, Kapoor PM, Choudhury M, Das S, et al. The role of Rajyoga meditation for modulation of anxiety and serum cortisol in patients undergoing coronary artery bypass surgery: A prospective randomized control study. Ann Card Anaesth. 2017;20:158–62. doi: 10.4103/aca.ACA_32_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Does Raja Yoga meditation Bring out Physiological and Psychological General Well Being Among Practitioners of It? [Last accessed on 2020 Sep 04]. Available from: http://internalmedicine.imedpub.com/does-raja-yoga-meditation-bring-out-physiological-andpsychological-general-well-being-among-practitioners-of-itphp?aid=6409 .
- 13.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 14.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 15.Catz A, Itzkovich M, Agranov E, Ring H, Tamir A. SCIM—spinal cord independence measure: A new disability scale for patients with spinal cord lesions. Spinal Cord. 1997;35:850–6. doi: 10.1038/sj.sc.3100504. [DOI] [PubMed] [Google Scholar]
- 16.Group W. Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 17.Love J, Dropmann D, Selker RJ. Jamovi. Amsterdam, Netherlands: Jamovi Project; 2018. [Google Scholar]
- 18.Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. 2013;139:213–40. doi: 10.1037/a0028931. [DOI] [PubMed] [Google Scholar]
- 19.Brown GW, Andrews B, Harris T, Adler Z, Bridge L. Social support, self-esteem and depression. Psychol Med. 1986;16:813–31. doi: 10.1017/s0033291700011831. [DOI] [PubMed] [Google Scholar]
- 20.Astin JA. Mind-body therapies for the management of pain. Clin J Pain. 2004;20:27–32. doi: 10.1097/00002508-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29:450–60. doi: 10.1097/AJP.0b013e31825e1492. [DOI] [PubMed] [Google Scholar]
- 22.Curtis K, Hitzig SL, Bechsgaard G, Stoliker C, Alton C, Saunders N, et al. Evaluation of a specialized yoga program for persons with a spinal cord injury: A pilot randomized controlled trial. J Pain Res. 2017;10:999–1017. doi: 10.2147/JPR.S130530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prajapita Brahmakumaris Ishwariya Vishwa Vidyalaya. Avyakt Murli 2009-2010. Mount Abu: Gyanamrit Bhavan; 2010. [Google Scholar]
- 24.Li Y, Bressington D, Chien WT. Systematic review of psychosocial interventions for people with spinal cord injury during inpatient rehabilitation: Implications for evidence-based practice. Worldviews Evid Based Nurs. 2017;14:499–506. doi: 10.1111/wvn.12238. [DOI] [PubMed] [Google Scholar]
- 25.Lin N, Ensel WM. Life stress and health: Stressors and resources. Am Sociol Rev. 1989;54:382–99. [Google Scholar]
- 26.DeLongis A, Folkman S, Lazarus RS. The impact of daily stress on health and mood: Psychological and social resources as mediators. J Pers Soc Psychol. 1988;54:486–95. doi: 10.1037//0022-3514.54.3.486. [DOI] [PubMed] [Google Scholar]
- 27.Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia A randomized controlled trial. Acta Psychiatr Scand. 2007;116:226–32. doi: 10.1111/j.1600-0447.2007.01032.x. [DOI] [PubMed] [Google Scholar]
- 28.Varambally S, Gangadhar BN, Thirthalli J, Jagannathan A, Kumar S, Venkatasubramanian G, et al. Therapeutic efficacy of add-on yogasana intervention in stabilized outpatient schizophrenia: Randomized controlled comparison with exercise and waitlist. Indian J Psychiatry. 2012;54:227–32. doi: 10.4103/0019-5545.102414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oken BS, Kishiyama S, Zajdel D, Bourdette D, Carlsen J, Haas M, et al. Randomized controlled trial of yoga and exercise in multiple sclerosis. Neurology. 2004;62:2058–64. doi: 10.1212/01.wnl.0000129534.88602.5c. [DOI] [PubMed] [Google Scholar]
- 30.Velikonja O, Curic K, Ozura A, Jazbec SS. Influence of sports climbing and yoga on spasticity, cognitive function, mood and fatigue in patients with multiple sclerosis. Clin Neurol Neurosurg. 2010;112:597–601. doi: 10.1016/j.clineuro.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 31.Ahmadi A, Nikbakh M, Arastoo A, Habibi AH. The effects of a yoga intervention on balance, speed and endurance of walking, fatigue and quality of life in people with multiple sclerosis. J Hum Kinet. 2010;23:71–8. [Google Scholar]
- 32.Roland KP. Applications of yoga in Parkinson's disease: A systematic literature review. Res Rev Parkinsonism. 2014;4:1–8. [Google Scholar]
- 33.Afonso RF, Balardin JB, Lazar S, Sato JR, Igarashi N, Santaella DF, et al. Greater cortical thickness in elderly female yoga practitioners A cross-sectional study. Front Aging Neurosci. 2017;9:201. doi: 10.3389/fnagi.2017.00201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lazar SW, Kerr CE, Wasserman RH, Gray JR, Greve DN, Treadway MT, et al. Meditation experience is associated with increased cortical thickness. Neuroreport. 2005;16:1893–7. doi: 10.1097/01.wnr.0000186598.66243.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schutte NS, Malouff JM, Keng SL. Meditation and telomere length: A meta-analysis. Psychol Health. 2020;35:901–15. doi: 10.1080/08870446.2019.1707827. [DOI] [PubMed] [Google Scholar]


