ABSTRACT
Objective
This study compared the modification of musculoarticular stiffness (MAS) and clinical outcomes after mobilization with movement (MWM) on the inferior tibiofibular joint and a placebo MWM. Moreover, injured and non-injured ankle MAS were compared after MWM therapy.
Methods
A single-blinded randomized trial was conducted on 75 participants (mean age: 22.3 ± 2.17 years) with chronic self-reported asymmetric perception of ankle dorsiflexion stiffness. Participants were allocated to one of three groups: inferior tibiofibular MWM (ITFMWM), placebo and non-injured. Sinusoidal oscillation methods were used for experimental quantification of the MAS and clinical outcomes were assessed using the weight-bearing lunge test (WBLT), pain and stiffness perception. Three assessments were made: one pre-treatment (T0), one after the manual technique (T1) and one after taping (T2).
Results
Two-way ANOVA showed no significant differences between the groups and no interaction effect for the outcome measures. However, a significant difference for the time effect (T0-T1-T2) was found in the three groups for WBLT dorsiflexion range of motion (p < 0.001, Cohen’s d = 0.21) and stiffness perception (p < 0.001, Cohen’s d = 0.54) but the minimal clinically important differences were not reached for either value.
Discussion
The results could not support that a single session of ITFMWM modifies MAS or the clinical outcomes compared to placebo treatment. Furthermore, injured MAS does not differ from non-injured MAS in chronic ankle dorsiflexion stiffness. Further studies should assess subjects’ responsiveness concerning the Mulligan concept and focus on a medium- to long-term follow-up.
KEYWORDS: Mulligan, passive stiffness, MWM, weight-bearing lunge test, viscoelasticity
Introduction
Limitation of ankle dorsiflexion is a common musculoskeletal disorder among active people that affects daily life activities such as walking, running, stair climbing and squatting [1] and may predispose to further ankle injuries[2]. Stiffness describes the relationship between an applied load and the amount of elastic deformation that occurs in a structure. Increased stiffness may follow ankle injury such as ankle sprains, which is one of the most common injuries encountered in sport [3–5]. Conversely, in up to 32–74% of ankle sprains, patients complain of long-lasting functional instability [6] and demonstrate reduced dorsiflexion range of motion (ROM)[5].
Quantitative measurements of musculoarticular stiffness (MAS) in the ankle have been studied using several methodologies. The method of induced sinusoidal oscillations was introduced by Rack [7] and adapted by Detrembleur and Plaghki [8] to assess the viscoelasticity of a joint. It measures the stiffness of the muscle–tendon unit as well as passive stiffness provided by the skin, ligaments and articular capsule [8,9]. This method distinguishes between elastic stiffness (i.e. the spring mechanism of the joint) and viscous stiffness (i.e. the damper mechanism of the joint). Measuring ankle dorsiflexion MAS with an induced sinusoidal oscillatory device has been shown to be a valid and reliable method[10]. The MAS can be distinguished from the ROM, which is defined by the overall amplitude of the joint. Dorsiflexion ROM can be assessed clinically using the weight-bearing lunge test (WBLT) or goniometric measurements[1].
In a systematic review, Delahunt et al. [11] described the potential positive effects of manual therapy on ankle dorsiflexion ROM[12]. Mulligan’s mobilization with movement (MWM) technique is commonly used to treat musculoskeletal disorders and consists of passive joint gliding applied by the therapist’s hand or with rigid tape while the patient simultaneously performs the impaired active movement. The MWM treatment is thought to be pain free, provide instant results and long lasting effects, i.e. the PILL effect. [13,14] Several studies have reported a forward displacement of the inferior aspect of the fibula with respect to the tibia in subjects with ankle injury when compared to controls [15,16]. Evidence also suggests that patients with a chronic history of ankle or foot injury demonstrate greater MAS than non-injured people without a history of injury[17]. Hence, people with MAS may respond differently to manual therapy based on their injury history. It is also not clear if manual mobilization with repeated ankle dorsiflexion movement during MWM is more effective than simply repeating ankle dorsiflexion alone to improve dorsiflexion ROM or to modify MAS. To our knowledge, there has been no study assessing MAS modifications in people with different ankle dorsiflexion ROM disorders.
According to the Mulligan concept[18], rigid sports taping can be applied following MWM to mimic the MWM technique and to provide ongoing mobilization while the tape is worn during daily life activities. Inferior tibiofibular tape (ITFT) is thought to limit anterior displacement of the distal fibula [19] but the effect of this taping technique following ankle MWM on MAS has not been investigated.
The goals of this study were divided into two parts. Firstly, we wanted to compare the effect of a single session of real versus placebo MWM treatment of the ITF joint on ankle MAS, dorsiflexion ROM, pain and stiffness perception. Secondly, we compared the MAS modifications on injured and non-injured stiff ankles.
Methods
Ethics statement
This study was approved by local ethics committee ‘Comité d’Éthique Hospitalo-Facultaire’, Université catholique de Louvain, Belgium (Registration number: B 403,201,421,483). Participants received written information explaining the research and were guaranteed confidentiality at all times. All subjects provided signed informed consent.
Population
The participants were recruited via convenience sampling from physiotherapy clinics or by word of mouth. All the participants enrolled on a voluntary basis without financial compensation. They were recruited if they were at least 18 years old and had a subjective perception of asymmetric ankle joint stiffness or pain during active dorsiflexion on the WBLT. The injured participants had to report an ankle injury that occurred more than six months prior to enrolling the study. Those participants who described asymmetric ankle stiffness during the WBLT without any history of injury were included in the non-injured group. Conversely, participants with a history of ankle injury were randomly allocated into two groups: the experimental group receiving ITFMWM and the placebo group (control) receiving sham treatment. Allocation to the ITFMWM and placebo groups was achieved through simple randomization, with the randomization sequence created using Excel 2007 (Microsoft, Redmond, WA, USA). The non-injured group was not randomly allocated (Figure 1). The ITFMWM and non-injured groups received real intervention. Three different physiotherapists provided treatment, allocation of subjects and assessment: one was in charge of allocating the participants to one of three groups; another was in charge of treatment and was blind concerning the subject’s status group (i.e. ITFMWM or non-injured) but, for pragmatic reasons, was not blind to the placebo group; and the third physiotherapist blindly assessed the different outcome measures during each follow-up for all the included subjects. (Appendix 1 – Consort Checklist)
Figure 1.
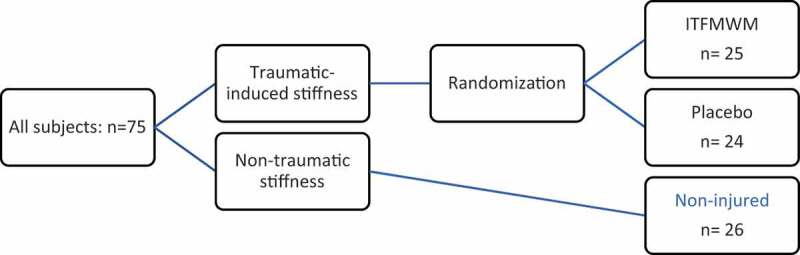
Flow chart of included subjects. ITFMWM: inferior tibiofibular mobilization with movement
Dependent variables: Primary and secondary outcome measures
Sociodemographic information on age, sex, weight, height, sports activities and history of injury was collected (Table 1).
Table 1.
Descriptive data of participants at baseline
| ITFMWM | Placebo | Non-Injured | |
|---|---|---|---|
| Gender Male (n) Female (n) |
19 6 |
17 7 |
11 15 |
| Age (years) | 23 (2.5) | 21.7 (1.74) | 22.3 (2.11) |
| Weight (kg) | 70.2 (10.48) | 71.5 (11.3) | 64.9 (11.38) |
| Height (cm) | 176.4 (9.24) | 177.9 (8.94) | 172.5 (8,61) |
| Sport activity (hour) | 5.4 (3.8) | 5,3 (4.43) | 3.5 (3.13) |
| Elasticity (N.m rad−1) | 36.5 (18.05) | 33.8 (15.69) | 37.2 (14.79) |
| Viscosity (N.m.s rad−1) | 6.9 (3.69) | 8.2 (3.99) | 5.8 (3.04) |
| Lpath (N.m rad−1) | 118.2 (37.59) | *135.3 (54.92) | *99.8 (31.77) |
| WBLT distance (cm) | 11.6 (3.33) | 12.5 (3.33) | 11.4 (3.24) |
| Pain (VAS,/10) | 1.7 (1.49) | 1.1 (1.18) | 0.8 (1.06) |
| Stiffness perception (/10) | 4.6 (1.68) | 3.9 (1.72) | 4.1 (1.87) |
Results are presented as means (SD). ITFMWM: inferior tibiofibular mobilization with movement; WBLT: weight-bearing lunge test (toe-to-wall distance); VAS: visual analogue scale; Lpath: path length or total stiffness representation. *One-way ANOVA demonstrates significant differences between marked groups (i.e. placebo and non-injured Lpath baseline values).
Several outcome measures were assessed objectively: three MAS experimental measures – elasticity, viscosity and total path length (Lpath); and three clinical outcome measures – dorsiflexion ROM with the WBLT, as well as subjective pain and stiffness recorded during each WBLT. All outcome measures were assessed blindly with no interaction between assessor and practitioner. Variables were recorded three times: before manual intervention (T0), after manual intervention (T1) and after application of the ITFT (T2).
The experimental measures of MAS were assessed with electromechanical devices (Figure 2) using a free oscillation technique that evaluated passive stiffness during ankle dorsiflexion. Lobet et al [20]. previously described excellent reliability for elasticity (ICC = 0.77–0.90) and viscosity (ICC = 0.83–0.90). Participants were supine with their knee in extension. The foot was strapped to a plate that produced passive ankle joint dorsiflexion with a 5° amplitude sinusoidal rotary displacement (2.5° in flexion and 2.5° in extension). The system assessed MAS from 3 Hz to 12 Hz, with three trials at each frequency (a total of 30 trials). An electrogoniometer placed on the rotatory axis recorded the angular displacement (Figure 2).
Figure 2.
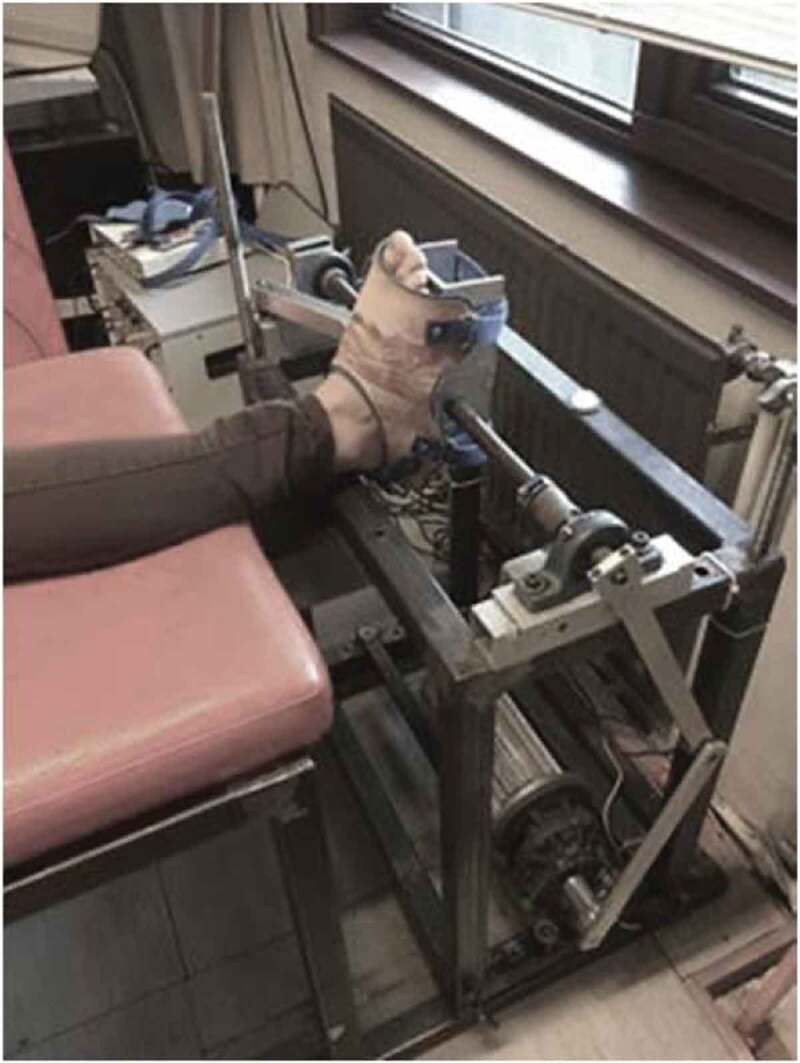
Electromechanical system adapted by Detrembleur (2000) [8] from the work of Rack (1960) [7] and Lehman (1989) [22] to measure passive ankle musculoarticular stiffness
Three variables were calculated by the electromechanical device[8]: Elasticity is independent of frequency and represented by the intercept values (N.m rad−1) of the regression line; Viscosity is represented by the slope of the regression line (N.m.s rad−1) and is frequency dependent; and Lpath is the reflex response to movement quantified by the phase diagram between elasticity and viscosity over 10 different ankle oscillation frequencies (N.m rad−1). Lpath is a vectoral representation of viscoelasticity: the higher the Lpath, the higher the viscoelasticity. These three variables represent MAS, which together evaluate the articular and muscle effects of ankle stiffness, although the triceps surae muscles have been shown to be the main contributors in ankle MAS[21].
The WBLT (Figure 3) was used to assess dorsiflexion ROM. This test [1,23] has been shown to have moderate to excellent intra- and inter-rater reliability (ICC = 0.80–0.99), with a minimal detectable change of 1.9 cm[24]. Standardized instructions were given to the participant. The distance between the foot and the wall was measured with a ruler during the WBLT[25]. Participants were asked to perform an active WBLT (Figure 3) and the pain was assessed simultaneously using a visual analogue scale (VAS) comprising a 10-cm horizontal line from 0 to 10: 0, ‘no pain at all’; 10, ‘the most intense pain’. The minimal detectable change for the VAS score is a change of at least 2 points[26]. The participant’s stiffness perception during the WBLT was evaluated subjectively using the same VAS scale: 0, ‘no rigidity’; 10, ‘the most rigid’. To the author’s knowledge, this last scale has not yet been previously reported.
Figure 3.
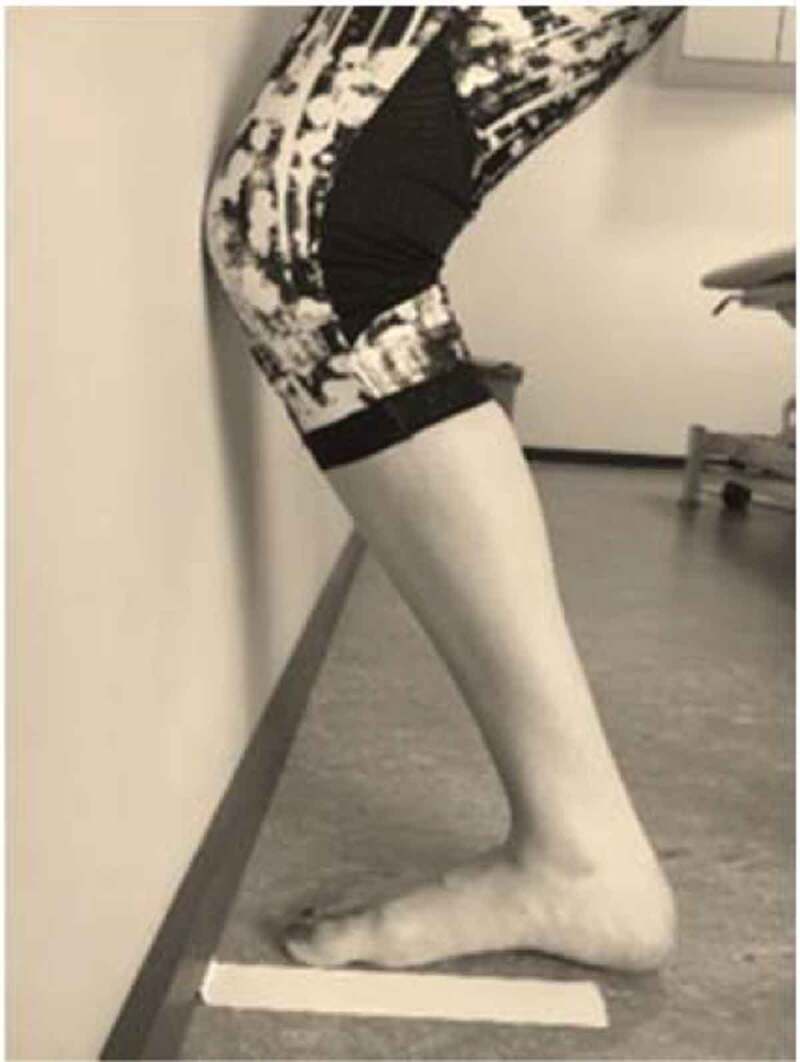
The weight-bearing lunge test (WBLT)
Interventions
The real intervention consisted of a weight-bearing ITFMWM on the restricted and painful ankle. Participants stood on a raised treatment table in a lunge position with their affected foot forward in front of the physiotherapist. The physiotherapist performed a combined posterior/superior/lateral glide of the distal head of the fibular bone with respect to the tibia while the participant lunged forward over the foot to produce active dorsiflexion (Figure 4). As for all MWM techniques, the movement was required to be pain-free. Treatment comprised three sets of 10 repetitions with a 1-min break between each set. A placebo intervention was applied to evaluate the effectiveness of MWM compared to repeated active dorsiflexion on outcome measures. The placebo treatment also consisted of three sets of 10 repetitions with a 1-min break between each set. The physiotherapist applied a similar technique as previously described but with just the hands placed on the fibula without the glide (light touch) to mimic real MWM.
Figure 4.
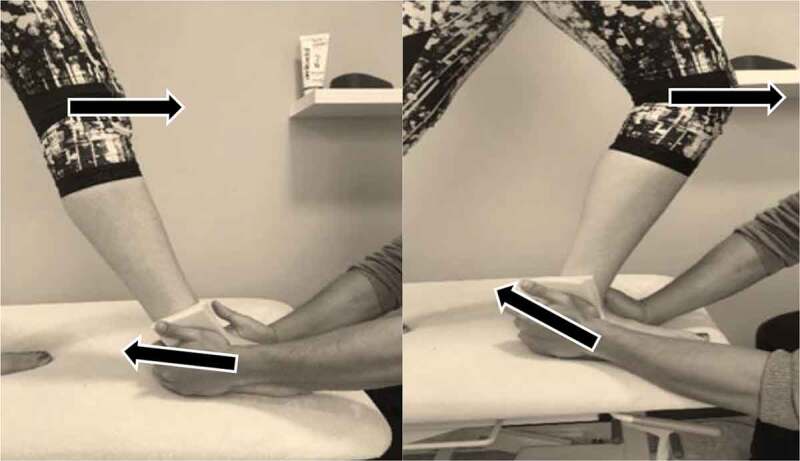
Weight-bearing mobilization with movement on the fibula for improvement of ankle dorsiflexion. Real treatment was applied to the ITFMWM and non-injured groups, whereas the placebo group received a sham treatment. The arrows at the top show the direction of movement of the participant and the arrows at the bottom show the direction of glide applied by the physiotherapist
Taping has been recommended to enhance the effect of the MWM during everyday life activities. Therefore, an ITFT was applied and participants were asked to walk in an empty corridor for 5 min. The ITFT is a 5-cm rigid sports tape (Strappal B.S.N. Medical) applied 2 cm anterior to the edge of the fibula and 1 cm proximal to the tip of the lateral malleolus directed proximally up the leg in a spiral (Figure 5). Tension was applied from the start in combination with a postero-superior-lateral glide of the distal fibula while the treated ankle stayed in a non-weight-bearing neutral position. For the ITFMWM and non-injured groups the tape was applied after the application of MWM, whereas the physiotherapist applied no tension and no glide for the placebo application in the placebo group. At the end, the outcome variables were all reassessed.
Figure 5.

Mulligan’s fibular repositioning tape. The arrow shows the direction of tension applied in the tape for real treatment
The participants were given no feedback regarding the type of procedure they had received during the entire session. (Appendix 2. TIDieR checklist)
Independent variables
Data were compared among three independent variables: group, which represents the effect between the three groups; time, which represents the effect of time by comparing values at baseline (T0), after MWM or placebo treatment (T1) and after tape or placebo tape application (T2); and the interaction between group and time (i.e. the efficacy of the intervention in one group compared to another).
Data analysis
The MAS and clinical outcome measures were analyzed using Sigmaplot 14.0 (Windows) by Systat Software Inc. Descriptive analysis was performed for the sociodemographic data. First, a one-way ANOVA or Kruskal-Wallis test, depending on whether normality was respected, was performed to establish baseline differences between groups (Table 1). Then, a two-way repeated-measures ANOVA was used for each dependent variable (elasticity, viscosity, Lpath, WBLT, pain, stiffness perception). Three factors were assessed: group (between-group effect), time (within-group effect) and interaction (group x time effect). Post-hoc analysis was used with the Bonferroni t-test. Effect size was measured with a standardized mean of difference using Cohen’s d method with MedCalc for Windows, version 19.2.1 (MedCalc Software, Ostend, Belgium). We used a p value of < 0.05 as the critical value for significance.
Results
Seventy-five participants were included in the study. There were no dropouts. Ankle injuries included ankle sprains (68%), malleolar (2%) or navicular (2%) fracture, Achilles tendinopathy (20%) and calf strain (8%). All of the participants were included in the analysis of both clinical and MAS outcomes (25 in ITFMWM, 24 in placebo, 26 in non-injured). Descriptive analysis of baseline characteristics can be seen in Table 1. One-way ANOVA found no significant differences for any of the variables between the three groups, with the exception of Lpath between the placebo and non-Injured groups. The results of each time of assessment are shown in Table 2.
Table 2.
Report of the outcome measures for the different follow-ups
| ITFMWM |
Placebo |
Non-injured |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 Mean (SD) |
T1 Mean (SD) |
T2 Mean (SD) |
T0 Mean (SD) |
T1 Mean (SD) |
T2 Mean (SD) |
T0 Mean (SD) |
T1 Mean (SD) |
T2 Mean (SD) |
|||
| Elasticity (N.m rad−1) |
36.5 (18.1) |
41.7 (21.0) |
42.1 (20.7) |
33.8 (15.7) |
40.8 (21.7) |
39.8 (15.3) |
37.2 (14.8) |
31.6 (17.3) |
34.1 (16.1) |
||
| Viscosity (N.m.s rad−1) |
6.96 (3.69) |
6.7 (3.83) |
6.5 (3.7) |
8.2 (3.99) |
7.3 (4.48) |
7.3 (3.99) |
5.8 (3.04) |
6.97 (3.56) |
6.1 (3.01) |
||
| Lpath (N.m rad−1) |
118.2 (37.6) |
116.4 (39.9) |
111 (38.4) |
135.3 (54.9) |
126.9 (52.4) |
123.1 (38.8) |
99.8 (31.8) |
106.6 (35.0) |
100.1 (28.4) |
||
| WBLT (cm) |
11.6 (3.33) |
12.4 (3.35) |
12.4 (3.47) |
12.5 (3.33) |
13.2 (3.34) |
12.9 (3.53) |
11.4 (3.24) |
11.8 (2.99) |
12.2 (3.01) |
||
| Pain (/10 cm) |
1.7 (1,49) |
1.6 (1.78) |
1.4 (1.86) |
1.1 (1.18) |
1.7 (1.57) |
1.8 (1.74) |
0.8 (1.06) |
1.1 (1.57) |
1.3 (1.69) |
||
| Stiffness perception (/10) | 4.6 (1.68) |
3.7 (2.34) |
3.2 (2.15) |
3.9 (1.72) |
3.9 (1.75) |
3.4 (2.10) |
4.1 (1.86) |
3.4 (2.05) |
2.9 (1.90) |
||
Data are presented as means (SD). ITFMWM: inferior tibiofibular mobilization with movement; T0: data at baseline; T1: data after MWM or placebo MWM treatment; T2: data after taping; WBLT: weight-bearing lunge test; Lpath: path length or total stiffness representation.
Musculoarticular stiffness outcomes
No significant differences in the elasticity values between groups (p = 0.38), time (p = 0.29, Cohen’s d = 0.29) and interaction (p = 0.054) were found. Mean viscosity values between groups (p = 0.35), time (p = 0.465, Cohen’s d = 0.14) or interaction (p = 0.19) were not statistically relevant. A significant difference was found in Lpath values between the placebo and non-injured (p = 0.03, Cohen’s d = 0.68) groups and persisted through the trial for time (p = 0.14, Cohen’s d = 0.14) or interaction effects (p = 0.44). Between-group effect sizes (Cohen’s d) are shown in Table 3.
Table 3.
Two-way repeated-measures ANOVA results for group, time and interaction effects
| Group (between-group effect) |
Time (within-group effect) |
Interaction (Group x Time effect) |
||||
|---|---|---|---|---|---|---|
| p | Cohen’s d between ITFMWM and placebo |
Cohen’s d between ITFMWM and non-injured |
p | Cohen’s d T0-T2 |
p | |
| Elasticity (N.m rad−1) |
0.387 | 0.13 | 0.43 | 0.294 | 0.29 | 0.054 |
| Viscosity (N.m.s rad−1) |
0.357 | 0.20 | 0.14 | 0.465 | 0.14 | 0.198 |
| Lpath (N.m rad−1) |
0.032 | 0.31 | 0.32 | 0.145 | 0.15 | 0.448 |
| WBLT (cm) |
0.502 | 0.16 | 0.06 | <0.001 | 0.21 | 0.214 |
| Pain (/10 cm) |
0.325 | 0.23 | 0.05 | 0.097 | 0.34 | 0.106 |
| Stiffness perception (/10) | 0.725 | 0.08 | 0.18 | <0.001 | 0.54 | 0.18 |
Bold indicates significant p value. ITFMWM: inferior tibiofibular mobilization with movement; Lpath: total stiffness representation; WBLT: weight-bearing lunge test. Pain and stiffness perception are expressed using the visual analogue scale. T0 represent the baseline measurement and T2 the final measurement.
Clinical outcomes
There were no significant group differences or interaction effects for WBLT, pain or stiffness perception (Table 3). Concerning the time effect on WBLT values, post-hoc analysis (Bonferroni t-test) demonstrated that T0 data were significantly different from T1 (p < 0.001, Cohen’s d = 0.11) and T2 (p < 0.001, Cohen’s d = 0.21) data. Concerning stiffness perception, the Bonferroni t-test showed significant differences between the three time periods: T0-T1 (p = 0.013, Cohen’s d = 0.019), T1-T2 (p = 0.005, Cohen’s d = 0.24) and T0-T2 (p < 0.001, Cohen’s d = 0.54).
Discussion
This study evaluated change in MAS for people with perceived ankle dorsiflexion stiffness, either with a history of ankle injury or not, following MWM therapy during a single session on the ITF joint. Also, we compared the usefulness of a real compared to placebo MWM on all outcome measures. Our results demonstrated no differences in MAS between an injured and non-injured ankle in elastic or viscous stiffness. Furthermore, we did not demonstrate a significant impact of real MWM compared to placebo MWM (i.e. an active dorsiflexion movement on all outcome measures). All group combined (i.e. ITFMWM, placebo and non-injured) demonstrated a greater dorsiflexion ROM and decreased stiffness perception.
Based on our results, we demonstrated no significant modifications of elastic or viscous properties between groups or throughout the time of measurement. The viscoelastic properties can be mostly explained by Hill’s model describing a contractile component (the active part of the actin-myosin protein), with an elastic component behaving like a spring mechanism (mostly due to myofibril structures, sarcomeres and connectin protein) and a viscous component behaving like a damper mechanism into the myofibril[27]. There was a tendency for elastic stiffness to increase in people with a history of ankle trauma. Although this stiffness decreased in people without a history of ankle injury, the differences were not significant (p = 0.54). This could be due to the repetitive dorsiflexion movement through the protocol rather than to the intervention. McNair [28] demonstrated that jogging was more effective than stretching for decreasing elastic muscle stiffness whereas stretching was more efficient for increasing dorsiflexion ROM. The significant Lpath differences between the placebo and non-injured groups could be explained by baseline values. Furthermore, as Lpath represents a vectoral representation of stiffness, it might be more useful in conditions with greater stiffness impairment, such as spasticity. We could hypothesize that a more rigorous physical involvement of the triceps surae could demonstrate modifications in the viscoelastic properties of the ankle. However, a single session of MWM and taping during walking activities did not demonstrate any change.
We recruited mainly people with over six months ankle sprains injuries (68%). Following injury such as an ankle sprain, displacement of the fibula has been shown to occur [15,16,29]. This displacement may explain the positive effects of MWM compared to conventional treatments in the acute state [14,30]. However, the current results revealed no significant improvement for MWM compared to a placebo. Similar results were found when comparing the immediate effects of talocrural MWM or Kaltenborn mobilization on MAS and dorsiflexion ROM. In that study there was no significant difference in outcome measures for the two forms of mobilization, with small to moderate effect sizes[17]. Marrón-Gómez et al. (2015) investigated a single application of talocrural MWM, which significantly improved ankle dorsiflexion ROM (but just below the minimal detectable change of +1.7 cm) immediately after the intervention of people with chronic ankle instability[2]. Several studies with a similar protocol and population but with talocrural MWM found that ankle dorsiflexion increased by 1.6 cm on the WBLT in a single session. Those results are consistent with the current study’s change around 0.8 cm but are under the minimal detectable change of 1.9 cm[31]. Following the intervention, our data showed mean changes in the WBLT of 0.76 cm (ITFMWM), 0.4 cm (placebo) and 0.8 cm (non-injured), with SD values of 0.66, 0.64 and 0.65 cm, respectively, very similar to the previous study of Hidalgo et al [17]. In the current study, improvement in ROM may be due to the repeated dorsiflexion rather than the MWM applied to the chronic subjective perception of dorsiflexion restriction. While the MWM technique is thought to improve function and ROM by altering the position of the fibula[32], it may not be applicable in chronic stiffness conditions but rather in the acute phase. Indeed, acute and chronic ankle impairment do not appear to respond in the same way, in particularly with a single session of treatment, therefore different treatments might be useful depending on injury timing. The use of MWM, if recommended either for pain or ROM, improves with the application of the technique[32]. In the current study, randomization and treatment were given without consideration of such symptom modification. This design is often used in randomized controlled trials but is not in phase with clinical practice within the Mulligan concept and might explain the non-improvement. There may be a subgroup of patients who could probably respond better but this cannot be determined by the current research.
It was suggested that this type of taping, when applied immediately prior to activity and sport events, might help to increase the proprioceptive awareness of the ankle [19,33] or disinhibit soleus muscle activities in patients suffering from chronic ankle instability. In this protocol, our hypothesis was that the ITFT could enhance the effect of ITFMWM. However, this could not be supported based on our results. In the current study, it is not clear whether the taping or the repeated movement was useful.
The current study presents several limitations. Firstly, the inclusion criteria covered all subjects with a perception of asymmetric ankle mobility, without any regard for the type of injury. Secondly, no objective assessment or functional evaluation was made prior to the enrollment, therefore the results of this study should be considered with caution. In all groups, the participants exhibited low irritability and could differ from typical patients that present themselves in the clinical environment. Thirdly, we performed the same MWM on all patients during a single session without respecting the concept that MWM should only be applied when there is a positive outcome. Further study should assess medium- and long-term effects of such treatment with a larger sample and a more specific population (e.g. people with a history of ankle sprains). The sample size was shown retrospectively to be adequate for MAS values but insufficient for dorsiflexion ROM. In order to achieve a power of 80% with an alpha level of 0.05, we should have recruited 156 participants. Taping was not evaluated as a treatment in the present study and so no clear conclusions can be made. However, following the Mulligan concept, we could not conclude that taping would give any beneficial output. Finally, questionnaires and clinically relevant tests (e.g. the star excursion balance test, lateral or forward step-down test, hop tests) should be used to assess ankle stiffness and functional capacity
Conclusion
The present study showed no significant differences between groups following a single session of MWM therapy on MAS, Dorsiflexion ROM, pain or stiffness perception. All groups showed improved dorsiflexion ROM and stiffness perception. This study suggests that a single session of MWM on the ITF joint should not be used systematically in clinical conditions for people with a perception of chronic ankle stiffness. Further studies should assess whether there are responders with immediate effects and non-responders to ITFMWM and/or other MWM, on ankle joints regarding other more specific clinical outcome measures in a pragmatic clinical trial design.
Biographies
Anh Phong Nguyen is a physiotherapist and Ph.D. student at the Université Catholique de Louvain (UCLouvain) in Belgium. His time is divided in clinical work, teaching and research activities.
Prof. Philippe Mahaudens is a professor at the Université Catholique de Louvain (UCLouvain) in Belgium. His research is mainly focused on the biomechanics and stiffness of the scoliosis.
Prof. Christine Detrembleur is a professor at the Université Catholique de Louvain (UCLouvain) in Belgium and is the Head of laboratory of the NeuroMusculoSkeletal Lab (IREC/UCLouvain). She is an expert in biomechanics and walking analysis. She write and co-write more than 200 scientific articles.
Dr Toby Hall is an internationally respected teacher of manual therapy. He is an Adjunct Associate Professor at Curtin University, Perth Western Australia, and is also Senior Teaching Fellow at The University of Western Australia.
Dr. Benjamin Hidalgo is a physiotherapist, osteopath and Ph.D. He is a national academic associate professor in Belgium and international teacher in continuing education for physiotherapist in the musculoskeletal field. His research work is focused on the spine and lower limb.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Bennell K, Talbot R, Wajswelner H, Techovanich W, Kelly D.. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother. 1998;44(3):175–180. [DOI] [PubMed] [Google Scholar]
- [2].Marrón-Gómez D, Rodríguez-Fernández ÁL, Martín-Urrialde JA.. The effect of two mobilization techniques on dorsiflexion in people with chronic ankle instability. Phys Ther Sport. 2015;16(1):10–15. [DOI] [PubMed] [Google Scholar]
- [3].Collins N, Teys P, Vicenzino B.. The initial effects of a Mulligan’s mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther. 2004;9(2):77–82. [DOI] [PubMed] [Google Scholar]
- [4].Fong DT, Hong Y, Chan L, Yung PS, Chan K.. A systematic review on ankle injury and ankle sprain in sports. Sport Med. 2007;37(1):73–94. [DOI] [PubMed] [Google Scholar]
- [5].Hoch MC, Staton GS, Medina McKeon JM, Mattacola CG, McKeon PO.. Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J Sci Med Sport. 2012;15(6):574–579. [DOI] [PubMed] [Google Scholar]
- [6].Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. Br J Sport Med. 2014;48:1014–1018. 13 [DOI] [PubMed] [Google Scholar]
- [7].Rack PMH. The behaviour of a mammalian muscle during sinusoidal stretching. J Physiol. 1966;183(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Detrembleur C, Plaghki L.. Quantitative assessment of intrathecally administered baclofen in spasticity. Arch Phys Med Rehabil. 2000;81(3):279–284. [DOI] [PubMed] [Google Scholar]
- [9].Ditroilo M, Cully L, Boreham CA, De Vito G.. Assessment of musculo-articular and muscle stiffness in young and older men. Muscle and Nerve. 2012;46(4):559–565. [DOI] [PubMed] [Google Scholar]
- [10].Lobet S, Detrembleur C, Massaad F, Hermans C.. Three-dimensional gait analysis can shed new light on walking in patients with haemophilia. Sci World J. 2013;2013:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Delahunt E, Bleakley CM, Bossard DS, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br J Sports Med. 2018;52(20):1304–1310. [DOI] [PubMed] [Google Scholar]
- [12].van der Wees PJ, Lenssen AF, Hendriks EJM, Stomp DJ, Dekker J, de Bie RA.. Effectiveness of exercise therapy and manual mobilisation in acute ankle sprain and functional instability: A systematic review. Aust J Physiother. 2006;52(1):27–37. [DOI] [PubMed] [Google Scholar]
- [13].Vicenzino B, Paungmali A, Teys P.. Mulligan’s mobilization-with-movement, positional faults and pain relief: current concepts from a critical review of literature. Man Ther. 2007;12(2):98–108. [DOI] [PubMed] [Google Scholar]
- [14].Hudson R, Baker RT, May J, Reordan D.. Novel treatment of lateral ankle sprains using the Mulligan concept : an exploratory case series analysis. J Man Manip Ther. 2017;25(5):251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Hubbard TJ, Hertel J.. Anterior positional fault of the fibula after sub-acute lateral ankle sprains. Man Ther. 2008;13(1):63–67. [DOI] [PubMed] [Google Scholar]
- [16].Kavanagh J. Is there a positional fault at the inferior tibiofibular joint in patients with acute or chronic ankle sprains compared to normals? Man Ther. 1999;4(1):19–24. [DOI] [PubMed] [Google Scholar]
- [17].Hidalgo B, Hall T, Berwart M, Biernaux E, Detrembleur C.. The immediate effects of two manual therapy techniques on ankle musculoarticular stiffness and dorsiflexion range of motion in people with chronic ankle rigidity: A randomized clinical trial. J Back Musculoskelet Rehabil. 2018;31(3):515–524. [DOI] [PubMed] [Google Scholar]
- [18].Vallandingham RA, Gaven SL, Powden CJ.. Changes in dorsiflexion and dynamic postural control after mobilizations in individuals with chronic ankle instability: A systematic review and meta-analysis. J Athl Train. 2019;54(4):403–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Someeh M, Norasteh AA, Daneshmandi H, Asadi A.. Immediate effects of Mulligan’s fibular repositioning taping on postural control in athletes with and without chronic ankle instability. Phys Ther Sport. 2015;16(2):135–139. [DOI] [PubMed] [Google Scholar]
- [20].Lobet S, Henrard OCKPS, Hermans C.. Assessment of passive musculoarticular ankle stiffness in children, adolescents and young adults with haemophilic ankle arthropathy. Haemophilia. 2018;48:(February):1–10. [DOI] [PubMed] [Google Scholar]
- [21].Salsich GB, Mueller MJ, Sahrmann SA.. Passive ankle stiffness in subjects with diabetes and peripheral neuropathy versus an age-matched comparison group. Phys Ther. 2000;80(4):352–362. [DOI] [PubMed] [Google Scholar]
- [22].Lehmann J.F.. Spaticity: quantitative measurements as a bases for assessing effectiveness of therapeutic intervention. Arch Phys Med Rehabil. 1989;70:6–15. 1 [PubMed] [Google Scholar]
- [23].Cejudo A, Sainz de Baranda P, Ayala F, Santonja F.. A simplified version of the weight-bearing ankle lunge test: description and test-retest reliability. Man Ther. 2014;19(4):355–359. [DOI] [PubMed] [Google Scholar]
- [24].Powden CJ, Hoch JM, Hoch MC.. Reliability and minimal detectable change of the weight-bearing lunge test : A systematic review. Man Ther. 2015;20(4):524–532. [DOI] [PubMed] [Google Scholar]
- [25].Williams CM, Caserta AJ, Haines TP.. The TiltMeter app is a novel and accurate measurement tool for the weight bearing lunge test. J Sci Med Sport. 2013;16(5):392–395. [DOI] [PubMed] [Google Scholar]
- [26].Lee JS, Hobden E, Stiell IG, Wells GA.. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med. 2003;10(10):1128–1130. [DOI] [PubMed] [Google Scholar]
- [27].Gajdosik RL. Passive extensibility of skeletal muscle: review of the literature with clinical implications. Clin Biomech. 2001;16(2):87–101. [DOI] [PubMed] [Google Scholar]
- [28].McNair PJ. Effect of passive stretching and jogging on the series elastic muscle stiffness and range of motion of the ankle joint. Br J Sports Med. 1996;30(4):313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Hubbard TJ, Cordova M.. Effect of ankle taping on mechanical laxity in chronic ankle instability. Foot Ankle Int. 2010;31(6):499–504. [DOI] [PubMed] [Google Scholar]
- [30].Nisha K, Megha NA, Paresh P. Efficacy of weight bearing distal tibiofibular joint mobilization with movement (MWM) in improving pain, dorsiflexion range and function in patients with postacute lateral ankle sprain. Int J Physiother Res. 2014;2(3):542–548. www.ijmhr.org/ijpr.html [Google Scholar]
- [31].Vicenzino B, Branjerdporn M, Teys P, Jordan K.. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36(7):464–471. [DOI] [PubMed] [Google Scholar]
- [32].Loudon JK, Reiman MP, Sylvain J.. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: A systematic review. Br J Sports Med. 2014;48(5):365–370. [DOI] [PubMed] [Google Scholar]
- [33].Sesma AR, Mattacola CG, Uhl TL, Nitz AJ, McKeon PO.. Effect of foot orthotics on single- and double-limb dynamic balance tasks in patients with chronic ankle instability. Foot Ankle Spec. 2008;1(6):330–337. [DOI] [PubMed] [Google Scholar]


