Editorial
2020 A.D.; although there was a solid base under the scientific method to suggest that the Planet Earth was a globe, thousands stoke something impossible to prove: The Flat Earth Theory. Based on this raw theory, self-styled influencers took advantage of media approval. This cognitive tendency to interpret, favor, and recall information in order to strengthen one’s personal beliefs, is known as ‘confirmation bias’ [1]. We aim to point out this continuously propagated bias in physiotherapy clinical practice.
Physiotherapy is one of the most growing professions worldwide, although relatively young compared to other medical and health-care professions [2–4]. We have plenty of examples of how this growth deeply impacts clinical research and therapeutic principles. Physiotherapy is continuously modified based mainly on contexts and trends accepting theoretical paradigms, too often unsupported by solid scientific evidence.
The Physiotherapy Science and Fashion
During the time of COVID-19 health emergency a new approach to patient care has emerged: telerehabilitation. Just before the pandemic, telerehabilitation was just a promising addition to traditional intervention offering a new perspective for selected patients. Comparing apples to oranges, telerehabilitation has rapidly become a new and widely discussed revolutionary discovery contributing to the ‘evolution’ of our profession, replacing office-based physiotherapy, often without proper consideration of risk and liability [5–8]. This is only the latest episode of a long story.
In managing patellofemoral pain, the physical therapy profession trends moved from the ‘selective’ strengthening of the Vastus Medialis Obliquus muscle [9,10] to taping the patella to correct its position or tracking, to ‘change’ the femoral bone position by reinforcing the gluteal muscles [11–14] or using motor control strategies [15]. In managing spine disorders we moved from abdominal strengthening, to releasing hypomobile segments, to reinforcing certain muscles ‘selected by good’ (i.e. transversus abdominis and deep neck flexors) to provide more stability to the spine [16–22]. We lost years in obsessively supporting clinical prediction rules that are so far from the clinical reasoning process–a core musculoskeletal physiotherapy competence [23–26]. We spent also decades demonstrating how mobilizations were at least as effective as high-velocity low-amplitude thrust manipulations and developing non-informative screening tools to support the anecdotical belief of manipulation risks [27–30]. Most recently, because of an ‘overdose’ of neuroscience, many pretend to only ‘talk’ to patients to cure them from persistent spinal pain, without possessing proper skills in that field, and forgetting that touch is an essential aspect of our professional identity [31].
We have lost our direction: physiotherapy knowledge suffers from ups and downs. We have forgotten that what makes our identity as a profession is tailored decisions on which and how much of each intervention must be multi-modally packaged based on the patient’s clinical findings, psychosocial profile, socio-cultural background, and evidence. Randomized controlled trials show us as much as they can if one technique is better than another [32]. We need more extensive research to understand what our interventions do–how they work–and how we might improve our patients’ outcomes. It is time to acknowledge that our interventions are skill and environment dependent [33,34].
The biopsychosocial model advent rises a new challenge at a patient’s management level. Even if not supported by strong evidence, the biopsychosocial model is the best available framework to our knowledge to embrace current literature for application into real clinical practice [35]. But we have not yet learned from previous experiences; we rapidly changed clinical practice without using our proverbial critical sense. The biopsychosocial approach focused our attention on more general aspects of the person’s well-being, lifestyle, fitness, and the psycho-social domains [36]; but it is hypostasized that the bio-psycho-social model is misunderstood and ineffectively applied [37] due to a rigid categorization of its domains [38]. In this scenario, for some the ‘bio’ domain sounds erroneously as the pathoanatomical construct and is trivialized with the ‘nonspecific’ tag leading to a sterile debate if our physiotherapy intervention has to be hands-on or hands-off [39,40]. However, the complex interactions of the innumerable causal factors that can play a role in musculoskeletal pain should be appreciated as correlations. Applying the biopsychosocial model means favoring the uniqueness of the person, where all these factors interact in a non-linear fashion. Such complex causal interactions require a different ontological view of causation–the dispositional theory of causation–where cause is interpreted as a cluster of powers, or dispositions, that lead to different effects depending on time and the causal context [41]. Are we minimizing the biological domain too early?
Lead researchers and social influencers pretend to change real clinical practice but they forget their responsibilities regarding the Figure 1physiotherapy profession’s identity. The new trend is changing our profession into personal trainer or psychologist; but performing hundreds of ‘squats’ per day, posting one systematic review per week or studying genes is not enough to make a physiotherapist a good clinician [42]. Let’s face it: Exercise is one of the most powerful medicines and protective factors [43]; but at the same time is a risk factor for death when its dosage is not appropriate [44–46]. It sounds quirky how most consider exercises immune from placebo, contextual and psychological factors compared to manual therapy [47]. Physiotherapists still don’t possess an appropriate expertise on exercise science–how to appropriately exclude who is at risk (e.g. cardiovascular or respiratory parameters evaluation inside the ‘bio’ domain) and how to translate exercise science knowledge to a symptomatic population [48–52] – and to psychological interventions [53].
Figure 1.
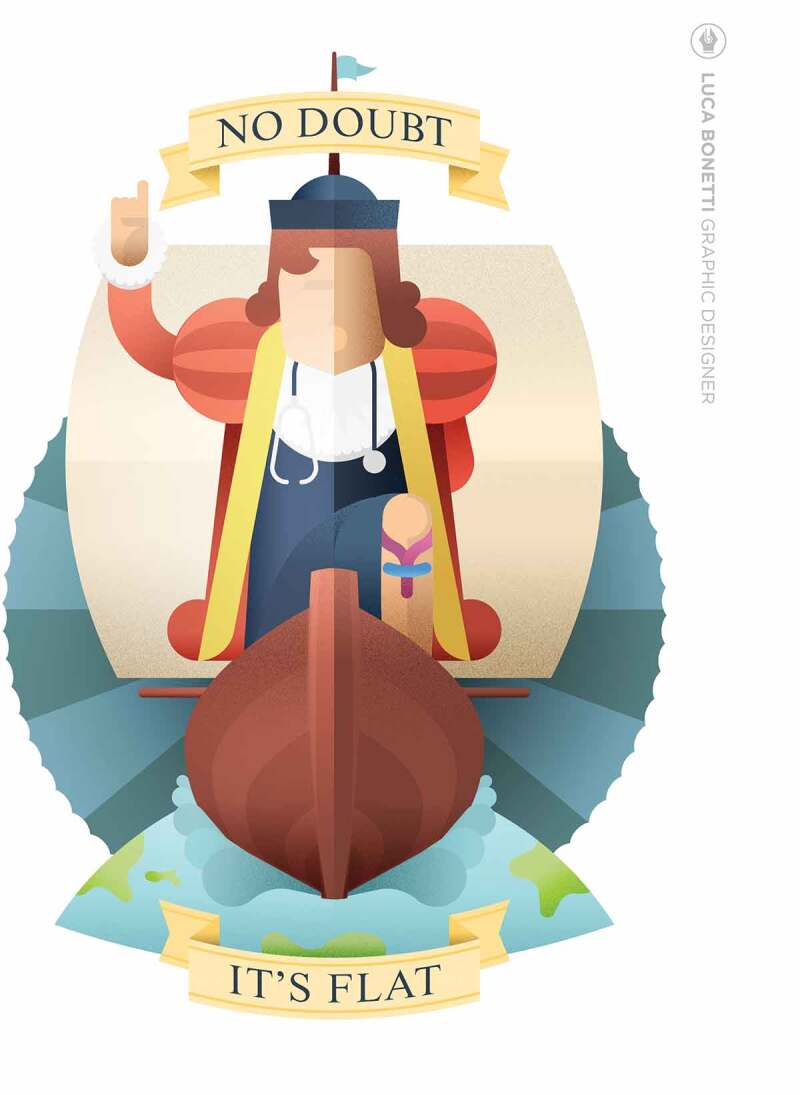
The figure was specifically created for this manuscript: no permission needed
We over-focused and froze the social and psychological constructs at a pathological level in persistent pain sufferers, forgetting that ontologically patients experience pain in their body [54]. Our knowledge in that field is based on old-fashioned psychology research findings and intervention (i.e. cognitive-behavior therapy) [55]. Over the past 20 years, psychology has moved to a paradigm shift with the ”positive psychology” [56] and the ‘psychological wellbeing constructs’ [57], which is more appropriate for our professional expertise [58].
The growth of the profession hides a more fragmented reality where clinicians and researchers live in parallel dimensions. However, clinical practice is intimately influenced by research trends that too often provide outdated targets for clinical practice.
This is a call to action for the profession. Based on the fallibility of many scientific constructs we need more solid evidence before substantially modifying clinical practice. We should be more cautious and respectful on changing our models of care.
Biographies
Dr. Maselli Filippo is a PhD, OMPT physiotherapist and educator experts on the management of low back pain and the differential diagnosis in physiotherapy. He has twenty years of clinical experience in Musculoskeletal Physiotherapy. He is the author of peer-reviewed articles and a keynote speaker at numerous courses and conferences in Italy. He lectures at the Universities of Genova; also, he provides masterclasses and CPD courses on the screening for referral and spinal manipulation. He is President of the Italian manual therapy and musculoskeletal physiotherapy group.
Dr Firas Mourad is a PhD, OMPT physiotherapist and educator experts on the management and assessment of neck pain/whiplash and associated disorders, especially on the differential diagnosis of serious pathologies of the cervical region. He is the author of peer-reviewed articles and book chapters on this topic. He has been a keynote speaker at numerous courses and conferences in Italy and Worldwide. He lectures at the Universities of Tor Vergata Rome and Brescia; also, he gives masterclasses and CPD courses on the screening for referral of the cervical spine, spinal manipulation, the philosophy behind physiotherapy and patient-centered care. He is also the IFOMPT MO delegate for ITALY and the Vicepresident of the Italian manual therapy and musculoskeletal physiotherapy group.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Talluri BC, Urai AE, Tsetsos K, et al. Confirmation bias through selective overweighting of choice-consistent evidence. Curr Biol. 2018. October 8;28(19):3128–3135.e8. [DOI] [PubMed] [Google Scholar]
- [2].Vercelli S, Ravizzotti E, Paci M.. Are they publishing? A descriptive cross-sectional profile and bibliometric analysis of the journal publication productivity of Italian physiotherapists. Arch Physiother. 2018. January 2;8:1. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Downie F, McRitchie C, Monteith W, et al. Physiotherapist as an alternative to a GP for musculoskeletal conditions: a 2-year service evaluation of UK primary care data. Br J Gen Pract. 2019. May;69(682):e314–e320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Demont A, Bourmaud A, Kechichian A, et al. The impact of direct access physiotherapy compared to primary care physician led usual care for patients with musculoskeletal disorders: a systematic review of the literature. Disabil Rehabil. 2019. October 11:1–12. DOI: 10.1080/09638288.2019.1674388 [DOI] [PubMed] [Google Scholar]
- [5].Howard IM, Kaufman MS. Telehealth applications for outpatients with neuromuscular or musculoskeletal disorders. Muscle Nerve. 2018. October;58(4):475–485. [DOI] [PubMed] [Google Scholar]
- [6].Pastora-Bernal JM, Martín-Valero R, Barón-López FJ. Cost analysis of telerehabilitation after arthroscopic subacromial decompression. J Telemed Telecare. 2018. September;24(8):553–559. [DOI] [PubMed] [Google Scholar]
- [7].Azma K, RezaSoltani Z, Rezaeimoghaddam F, et al. Efficacy of tele-rehabilitation compared with office-based physical therapy in patients with knee osteoarthritis: A randomized clinical trial. J Telemed Telecare. 2018. September;24(8):560–565. [DOI] [PubMed] [Google Scholar]
- [8].Cottrell MA, Hill AJ, O’Leary SP, et al. Service provider perceptions of telerehabilitation as an additional service delivery option within an Australian neurosurgical and orthopaedic physiotherapy screening clinic: A qualitative study. Musculoskelet Sci Pract. 2017. December;32:7–16. [DOI] [PubMed] [Google Scholar]
- [9].Pattyn E, Verdonk P, Steyaert A, et al. Vastus medialis obliquus atrophy: does it exist in patellofemoral pain syndrome? Am J Sports Med. 2011. July;39(7):1450–1455. [DOI] [PubMed] [Google Scholar]
- [10].Smith TO, Nichols R, Harle D, et al. Do the vastus medialis obliquus and vastus medialis longus really exist? A systematic review. Clin Anat. 2009. March;22(2):183–199. [DOI] [PubMed] [Google Scholar]
- [11].Crossley K, Bennell K, Green S, et al. A systematic review of physical interventions for patellofemoral pain syndrome. Clin J Sport Med. 2001. April;11(2):103–110. [DOI] [PubMed] [Google Scholar]
- [12].Crossley K, Bennell K, Green S, et al. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002. Nov-Dec;30(6):857–865. [DOI] [PubMed] [Google Scholar]
- [13].Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003. November;33(11):639–646. [DOI] [PubMed] [Google Scholar]
- [14].Liao TC, Yang N, Ho KY, et al. Femur Rotation Increases Patella Cartilage Stress in Females with Patellofemoral Pain. Med Sci Sports Exerc. 2015. September;47(9):1775–1780. [DOI] [PubMed] [Google Scholar]
- [15].Earl JE, Hoch AZ. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011. January;39(1):154–163. [DOI] [PubMed] [Google Scholar]
- [16].Hodges P, Richardson C, Jull G. Evaluation of the relationship between laboratory and clinical tests of transversus abdominis function. Physiother Res Int. 1996;1(1):30–40. [DOI] [PubMed] [Google Scholar]
- [17].Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976). 1996. November 15;21(22):2640–2650. [DOI] [PubMed] [Google Scholar]
- [18].Urquhart DM, Hodges PW, Allen TJ, et al. Abdominal muscle recruitment during a range of voluntary exercises. Man Ther. 2005. May;10(2):144–153. [DOI] [PubMed] [Google Scholar]
- [19].O’Leary S, Falla D, Elliott JM, et al. Muscle dysfunction in cervical spine pain: implications for assessment and management. J Orthop Sports Phys Ther. 2009. May;39(5):324–333. [DOI] [PubMed] [Google Scholar]
- [20].Jull GA, O’Leary SP, Falla DL. Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. J Manipulative Physiol Ther. 2008. September;31(7):525–533. [DOI] [PubMed] [Google Scholar]
- [21].Falla D, Hodges PW. Individualized exercise interventions for spinal pain. Exerc Sport Sci Rev. 2017. April;45(2):105–115. [DOI] [PubMed] [Google Scholar]
- [22].Schomacher J, Falla D. Function and structure of the deep cervical extensor muscles in patients with neck pain. Man Ther. 2013. October;18(5):360–366. [DOI] [PubMed] [Google Scholar]
- [23].Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine (Phila Pa 1976). 2002. December 15;27(24):2835–2843. [DOI] [PubMed] [Google Scholar]
- [24].Childs JD, Fritz JM, Flynn TW, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004. December 21;141(12):920–928. [DOI] [PubMed] [Google Scholar]
- [25].Haskins R, Rivett DA, Osmotherly PG. Clinical prediction rules in the physiotherapy management of low back pain: a systematic review. Man Ther. 2012. February;17(1):9–21. [DOI] [PubMed] [Google Scholar]
- [26].Haskins R, Osmotherly PG, Rivett DA. Validation and impact analysis of prognostic clinical prediction rules for low back pain is needed: a systematic review. J Clin Epidemiol. 2015. July;68(7):821–832. [DOI] [PubMed] [Google Scholar]
- [27].Rozmovits L, Mior S, Boon H. Exploring approaches to patient safety: the case of spinal manipulation therapy. BMC Complement Altern Med. 2016. June 2;16:164. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Carlesso LC, Gross AR, Santaguida PL, et al. Adverse events associated with the use of cervical manipulation and mobilization for the treatment of neck pain in adults: a systematic review. Man Ther. 2010. October;15(5):434–444. [DOI] [PubMed] [Google Scholar]
- [29].Nielsen SM, Tarp S, Christensen R, et al. The risk associated with spinal manipulation: an overview of reviews. Syst Rev. 2017. March 24;6(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kranenburg HAR, Tyer R, Schmitt M, et al. Effects of head and neck positions on blood flow in the vertebral, internal carotid, and intracranial arteries: a systematic review. J Orthop Sports Phys Ther. 2019. October;49(10):688–697. [DOI] [PubMed] [Google Scholar]
- [31].Geri T, Viceconti A, Minacci M, et al. Manual therapy: exploiting the role of human touch. Musculoskelet Sci Pract. 2019. December;44:102044. [DOI] [PubMed] [Google Scholar]
- [32].Anjum RL, Kerry R, Mumford SD. Evidence based on what? J Eval Clin Pract. 2015. December;21(6):E11–2. [DOI] [PubMed] [Google Scholar]
- [33].Testa M, Rossettini G. Enhance placebo, avoid nocebo: how contextual factors affect physiotherapy outcomes. Man Ther. 2016. August;24:65–74. [DOI] [PubMed] [Google Scholar]
- [34].Rossettini G, Carlino E, Testa M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Musculoskelet Disord. 2018. January 22;19(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Wade DT, Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil. 2017. August;31(8):995–1004. [DOI] [PubMed] [Google Scholar]
- [36].Holopainen R, Simpson P, Piirainen A, et al. Physiotherapists’ perceptions of learning and implementing a biopsychosocial intervention to treat musculoskeletal pain conditions: a systematic review and metasynthesis of qualitative studies. Pain. 2020. January 16;161:1150–1168. . [DOI] [PubMed] [Google Scholar]
- [37].Pincus T, Kent P, Bronfort G, et al. Twenty-five years with the biopsychosocial model of low back pain-is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine (Phila Pa 1976). 2013. November 15;38(24):2118–2123. [DOI] [PubMed] [Google Scholar]
- [38].Davidsen AS, Guassora AD, Reventlow S. Understanding the body-mind in primary care. Med Health Care Philos. 2016. December;19(4):581–594. [DOI] [PubMed] [Google Scholar]
- [39].Taylor AJ, Kerry R. When chronic pain is not “chronic pain”: lessons from 3 decades of pain. J Orthop Sports Phys Ther. 2017. August;47(8):515–517. [DOI] [PubMed] [Google Scholar]
- [40].Puentedura EJ, Flynn T. Combining manual therapy with pain neuroscience education in the treatment of chronic low back pain: A narrative review of the literature. Physiother Theory Pract. 2016. July;32(5):408–414. [DOI] [PubMed] [Google Scholar]
- [41].Low M. A novel clinical framework: the use of dispositions in clinical practice. A person centred approach. J Eval Clin Pract. 2017. October;23(5):1062–1070. [DOI] [PubMed] [Google Scholar]
- [42].Pershad Y, Hangge PT, Albadawi H, et al. Social Medicine: twitter in Healthcare. J Clin Med. 2018. May 28;7(6):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Ekelund U, Steene-Johannessen J, Brown WJ, et al.; Lancet Physical Activity Series 2 Executive Committe; Lancet Sedentary Behaviour Working Group . Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016. September 24;388(10051):1302–1310. [DOI] [PubMed] [Google Scholar]
- [44].Schwabe K, Schwellnus M, Derman W, et al. Medical complications and deaths in 21 and 56 km road race runners: a 4-year prospective study in 65 865 runners–SAFER study I. Br J Sports Med. 2014. June;48(11):912–918. [DOI] [PubMed] [Google Scholar]
- [45].Gordon L, Schwellnus M, Swanevelder S, et al. Recent acute prerace systemic illness in runners increases the risk of not finishing the race: SAFER study V. Br J Sports Med. 2017. September;51(17):1295–1300. [DOI] [PubMed] [Google Scholar]
- [46].Sewry N, Schwellnus M, Borjesson M, et al. Pre-race screening and stratification predicts adverse events-A 4-year study in 29585 ultra-marathon entrants, SAFER X. Scand J Med Sci Sports. 2020. March;30:18. [DOI] [PubMed] [Google Scholar]
- [47].Coenen P, Huysmans MA, Holtermann A, et al. Towards a better understanding of the ‘physical activity paradox’: the need for a research agenda. Br J Sports Med. 2020 Sep;54(17):1055–1057. [DOI] [PubMed] [Google Scholar]
- [48].Severin R, Wang E, Wielechowski A, et al. Outpatient Physical Therapist Attitudes Toward and Behaviors in Cardiovascular Disease Screening: A National Survey. Phys Ther. 2019. July 1;99(7):833–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Albarrati AM. Outpatient physical therapy cardiovascular assessment: physical therapist perspective and experience. Physiother Theory Pract. 2019. September;35(9):843–850. [DOI] [PubMed] [Google Scholar]
- [50].Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015. December;25(Suppl 3):1–72. [DOI] [PubMed] [Google Scholar]
- [51].Garber CE, Blissmer B, Deschenes MR, et al.; American College of Sports Medicine. American College of Sports Medicine position stand . Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011. July;43(7):1334–1359. [DOI] [PubMed] [Google Scholar]
- [52].Severin R, Sabbahi A, Albarrati A, et al. Blood Pressure Screening by Outpatient Physical Therapists: A Call to Action and Clinical Recommendations. Phys Ther. 2020 Jun 23;100(6):1008–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Alexanders J, Anderson A, Henderson S. Musculoskeletal physiotherapists’ use of psychological interventions: a systematic review of therapists’ perceptions and practice. Physiotherapy. 2015. June;101(2):95–102. [DOI] [PubMed] [Google Scholar]
- [54].Davidsen AS. How does the general practitioner understand the patient? A qualitative study about psychological interventions in general practice. Psychol Psychother. 2009. June;82(Pt 2):199–217. [DOI] [PubMed] [Google Scholar]
- [55].Thoma N, Pilecki B, McKay D. Contemporary cognitive behavior therapy: a review of theory, history, and evidence. Psychodyn Psychiatry. 2015. September;43(3):423–461. [DOI] [PubMed] [Google Scholar]
- [56].Seligman ME, Csikszentmihalyi M. Positive psychology. An introduction. Am Psychol. 2000. January;55(1):5–14. [DOI] [PubMed] [Google Scholar]
- [57].Ryff CD. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom. 2014;83(1):10–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Keyes CL. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol. 2007. Feb-Mar;62(2):95–108. [DOI] [PubMed] [Google Scholar]


