Abstract
Background
The COVID-19 pandemic resulted in nationwide social distancing and shelter-in-place orders meant to curb transmission of the SARS-CoV-2 virus. The effect of the pandemic on injury patterns has not been well described in the USA. The study objective is to determine the effect of the COVID-19 pandemic on the distribution and determinants of traumatic injuries.
Methods
This retrospective multi-institutional cohort study included all hospital admissions for acute traumatic injury at six community level I trauma centers. Descriptive statistics were used to compare injury causes, diagnoses and procedures over two similar time periods: prepandemic (March 11–June 30, 2019) and pandemic (March 11–June 30, 2020).
Results
There were 7308 trauma patients included: 3862 (53%) prepandemic and 3446 (47%) during the pandemic. Cause of injury significantly differed by period (p<0.001). During the pandemic, there were decreases in motor vehicle crashes (from 17.0% to 14.0%, p<0.001), worksite injuries (from 5.2% to 4.1%, p=0.02), pedestrian injuries (from 3.0% to 2.2%, p=0.02) and recreational injuries (from 3.0% to 1.7%, p<0.001), while there were significant increases in assaults (6.9% to 8.5%, p=0.01), bicycle crashes (2.8% to 4.2%, p=0.001) and off-road vehicle injuries (1.8% to 3.0%, p<0.001). There was no change by study period in falls, motorcycle injuries, crush/strikes, firearm and self-inflicted injuries, and injuries associated with home-improvement projects. Injury diagnoses differed between time periods; during the pandemic, there were more injury diagnoses to the head (23.0% to 27.3%, p<0.001) and the knee/leg (11.7% to 14.9%, p<0.001). There were also increases in medical/surgical procedures (57.5% to 61.9%, p<0.001), administration of therapeutics/blood products (31.4% to 34.2%, p=0.01) and monitoring (11.0% to 12.9%, p=0.01).
Discussion
Causes of traumatic injury, diagnoses, and procedures were significantly changed by the pandemic. Trauma centers must adjust to meet the changing demands associated with altered injury patterns, as they were associated with increased use of hospital resources.
Level of evidence
III (epidemiological).
Keywords: COVID-19, multiple trauma, diagnosis, epidemiology
Background
On March 11, 2020, the WHO declared COVID-19 a pandemic. In the USA, nationwide social distancing and shelter-in-place orders meant to curb transmission of SARS-COV-2 immediately followed the WHO declaration, which resulted in instantaneous and widespread disruptions to daily routines and activities for Americans. Whether these changes have any significant impact on traumatic injury is not fully reported. There is preliminary evidence suggesting the pandemic resulted in reduced emergency medical service (EMS) activations,1 emergency department (ED) visits,2 trauma activations3 and acute care surgery admissions.4 Preliminary reports on trauma center admissions have been mixed, with one study in New Zealand showing a 43% reduction5 at their level I trauma center, while studies in the UK and Singapore reported no meaningful change in volume.4 6
There is an abundance of medical literature describing the effects of the pandemic on hospital planning and injury patterns, particularly in international settings that were affected early in the pandemic, including China7–9 and elsewhere in Asia,4 10 11 the UK6 12–16 and elsewhere in Europe,17–23 as well as Australia and New Zealand.5 24 There have also been numerous studies determining the effects of the pandemic on specific types of injuries, including burns,25 head injuries,19 26 facial injuries,12 14 domestic violence27 and especially orthopedic injuries,8 13 15 16 23 28 29 as they typically represent the most common injuries due to trauma.30
In the USA31 the effects of the COVID-19 pandemic on traumatic injury patterns are not as well described. Knowing how injury patterns changed due to the pandemic may allow hospitals to provide optimal care of trauma patients during unprecedented times, particularly during times of hospital surge capacity. This study sought to determine whether the COVID-19 pandemic and the resultant shelter-in-place and social distancing orders were associated with changes in the causes and types of injuries for trauma patients admitted to six level I trauma centers in the USA. We hypothesize that causes of injury will differ compared with the prepandemic time frame.
Methods
This retrospective multi-institutional cohort study was performed by the Injury Outcomes Network, a collaborative research network of six community-based, level I trauma centers: Swedish Medical Center, Englewood, CO; St. Anthony Hospital, Lakewood, CO; Penrose Hospital, Colorado Springs, CO; Medical City Plano, Plano, TX; Research Medical Center, Kansas City, MO; and Wesley Medical Center, Wichita, KS. We included all hospital admissions for acute traumatic injury based on ICD-10 diagnosis code S00-T88 over two similar time periods: prepandemic (March 11–June 30, 2019) and pandemic (March 11–June 30, 2020).
Study variables
The following demographic and clinical characteristics and outcomes were obtained from the trauma registries at each participating hospital: admission date, age, sex, race, cause of injury, injury severity score (ISS; <16 vs ≥16), trauma team activation (full/partial vs consult/not activated), ED disposition to operating room (OR), admission to the intensive care unit (ICU), Abbreviated Injury Scale (AIS) codes, ICD-10 diagnosis codes, ICD-10 procedure codes, hospital length of stay (LOS), ICU admission, in-hospital mortality, Glasgow coma score (3–8 vs 9–15) and abnormal ED hypotension (systolic blood pressure <90 mm Hg vs ≥90 mm Hg). Both the 10 most common ICD-10 injury diagnoses and the 10 most common ICD-10 medical/surgical procedures were identified and tabulated.
Cause of injury was defined using ICD-10 injury classification, as follows: fall, motor vehicle crash (MVC), motorcycle crash, pedestrian, bicycle, off-road vehicle (all-terrain vehicle, snowmobile, dune buggy and dirt bike), recreation/sport (eg, skiing, football and horseback riding), assault, intentional self-harm, firearm (accidental discharge or malfunction, legal intervention and unspecified intent), home improvement (eg, contact with powered/non-powered tools or machinery), crush or strike (caught, crushed, jammed, pinched and struck by or against), worksite injury, and other causes (eg, burn or explosion, contact with sharp glass/object, animal bite/attack, unknown or not applicable and other (eg, tornado, overexertion and foreign body penetration)).
Statistical analyses
All statistical analyses were conducted using SAS V.9.4 (SAS Institute Inc, Cary, NC) with significance level of p value <0.05. Univariate statistics (Pearson χ2 tests, t-tests and Wilcoxon rank-sum tests) were performed to determine the association between study covariates and time period (prepandemic vs pandemic). The outcomes included causes of injury, the most common diagnoses and the most common procedures, analyzed by time period.
We also compared traumatic cause of injury in two additional populations: (1) patients admitted during the period coinciding with the White House’s extended COVID-19 guidelines on working from home and social distancing: March 11–April 30, 2020 compared with March 11–April 30, 2019; and (2) historic cohort of patients admitted March 11–June 30 in 2018 compared with 2019, to determine whether any differences seen in 2020 could be attributed to the pandemic.
Results
There were 7308 patients included in the study: 3862 (53%) prepandemic and 3446 (47%) during the pandemic. Overall demographics and injury severity characteristics were similar between time periods; however, clinical outcomes of in-hospital mortality and hospital and ICU LOS were significantly worse during the pandemic period (table 1). Overall, the most common causes of injury were falls (43%), MVCs (16%) and assaults (8%).
Table 1.
Demographics by study period
| Covariate, % (n) | Prepandemic March 11, 2019–June 30, 2019 n=3862 |
Pandemic March 11, 2020–June 30, 2020 n=3446 |
P value |
| Mean (SD) age, years | 54.4 (22) | 53.9 (21) | 0.32 |
| Female sex | 42.0 (1621) | 41.4 (1427) | 0.63 |
| White race | 75.8 (2926) | 74.7 (2575) | 0.43 |
| Full/partial trauma activation | 16.0 (619) | 16.3 (560) | 0.80 |
| ED disposition: operating room | 9.6 (371) | 10.0 (344) | 0.59 |
| ED SBP <90 mm Hg | 4.3 (164) | 4.7 (163) | 0.32 |
| Injury severity score ≥16 | 17.7 (685) | 18.1 (625) | 0.66 |
| Severe injury, AIS ≥3 | |||
| Head trauma | 14.9 (575) | 15.6 (539) | 0.37 |
| Thoracic trauma | 13.0 (503) | 13.7 (471) | 0.42 |
| Abdomen/pelvic trauma | 3.2 (125) | 3.3 (114) | 0.86 |
| Upper extremity trauma | 1.2 (45) | 1.6 (55) | 0.11 |
| Lower extremity trauma | 18.1 (698) | 18.8 (647) | 0.44 |
| In-hospital mortality | 3.2 (125) | 4.7 (163) | 0.001 |
| Hospital LOS, median (IQR) | 3 (1.2–6) | 3 (1–5) | 0.02 |
| ICU LOS, median (IQR) | 2 (0–3) | 1 (0–3) | 0.002 |
Bolding denotes statistical significance with p<0.05.
AIS, Abbreviated Injury Scale; ED, emergency department; ICU, intensive care unit; LOS, length of stay; SBP, systolic blood pressure.;
Cause of injury significantly differed by period (p<0.001) (table 2). During the pandemic, there were significant increases in assaults (6.9% to 8.5%, p=0.01), bicycle crashes (2.8% to 4.2%, p=0.001) and off-road vehicle injuries (1.8% to 3.0%, p<0.001), while there were significant decreases in MVCs (from 17.0% to 14.0%, p<0.001), worksite injuries (from 5.2% to 4.1%, p=0.02), pedestrian injuries (from 3.0% to 2.2%, p=0.02) and recreation/sport injuries (from 3.0% to 1.7%, p<0.001). There were no significant differences in the incidence of falls, motorcycle injuries, crush/strikes, firearm and self-inflicted injuries, and injuries associated with home improvement projects when comparing the prepandemic and pandemic periods.
Table 2.
Causes of injury by study period
| Covariate, % (n) | Prepandemic March 11, 2019–June 30, 2019 n=3862 |
Pandemic March 11, 2020–June 30, 2020 n=3446 |
P value |
| Fall | 42.2 (1630) | 43.8 (1508) | 0.18 |
| Motor vehicle crash | 17.0 (657) | 14.0 (481) | <0.001 |
| Assault | 6.9 (265) | 8.5 (294) | 0.01 |
| Motorcycle crash | 5.1 (198) | 5.6 (193) | 0.37 |
| Worksite injury | 5.2 (202) | 4.1 (141) | 0.02 |
| Crush/strike | 4.0 (156) | 3.2 (111) | 0.06 |
| Bicycle | 2.8 (107) | 4.2 (146) | <0.001 |
| Home improvement | 3.3 (127) | 3.3 (115) | 0.91 |
| Pedestrian | 3.0 (116) | 2.2 (74) | 0.02 |
| Recreational | 3.0 (116) | 1.7 (58) | <0.001 |
| Off-road vehicles | 1.8 (68) | 3.0 (103) | <0.001 |
| Firearm | 1.1 (44) | 1.5 (52) | 0.17 |
| Self-inflicted | 1.2 (46) | 1.3 (45) | 0.66 |
| Other* | 3.4 (130) | 3.6 (125) | 0.54 |
*Other: burn (n=98), animal bite (n=59), glass/sharp object (n=38), 'other' (n=35) or unknown (n=25).
We examined the change in injury patterns by admission week between the two study periods. Highlighted are the three most common causes of injury (figure 1). The incidence of falls remained relatively consistent in both time periods. The decrease in MVCs was most pronounced during the initial 8 weeks of the pandemic before reverting to the incidence seen prepandemic. The increase in assaults was typically greater at each study week during the pandemic than compared with the similar prepandemic week.
Figure 1.
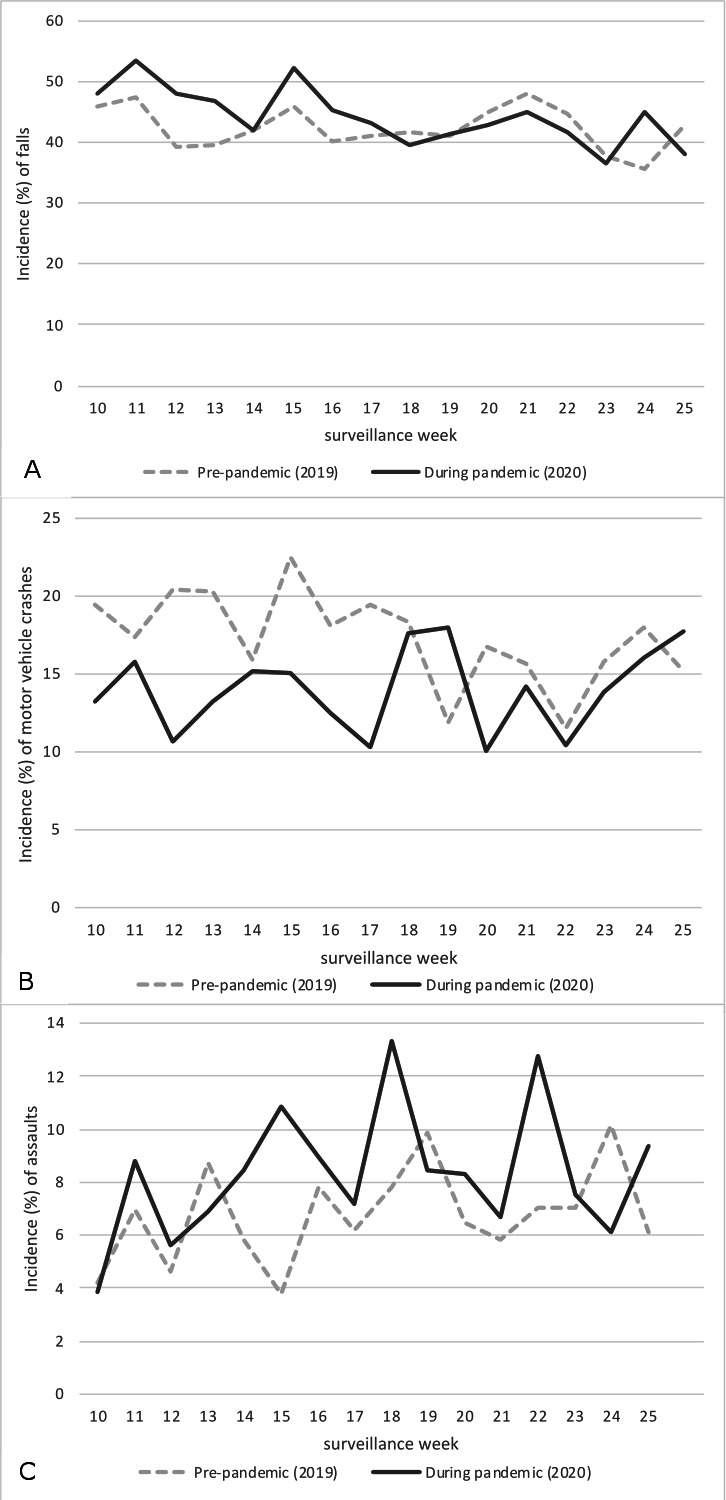
Incidence (%) of the three most common causes of injury, by surveillance week and pandemic period. (A) Incidence of falls; (B) incidence of motor vehicle crashes; and (C) incidence of assaults.
All study covariates (severity characteristics and demographics) differed by cause of injury, as shown in table 3. Patients suffering injuries due to intentional self-harm, assaults, motorcycle crashes and pedestrian injuries were among the most severe causes, with high mortality and ISS and proportionally more patients with ED hypotension, ED disposition to OR and severe head injuries (AIS ≥3).
Table 3.
Injury characteristics and outcomes by cause of injury
| Cause | Trauma activation, % (n) | ED to OR, % (n) | ISS ≥16, % (n) | Head AIS ≥3 (severe), % (n) | ED SBP <90 mm Hg, % (n) | Mortality, % (n) |
| Fall | 6.2 (195) | 5.1 (158) | 13.2 (413) | 18.0 (566) | 3.4 (108) | 3.5 (112) |
| Motor vehicle crash | 21.0 (239) | 8.5 (97) | 24.7 (281) | 10.6 (121) | 4.4 (50) | 4.6 (52) |
| Assault | 46.7 (261) | 22.4 (125) | 19.1 (107) | 11.3 (63) | 7.9 (44) | 3.6 (20) |
| Motorcycle crash | 26.6 (104) | 14.3 (56) | 28.9 (113) | 17.4 (68) | 7.7 (30) | 7.2 (28) |
| Worksite injury | 14.3 (49) | 18.9 (68) | 17.5 (60) | 14.3 (49) | 6.1 (21) | 1.2 (4) |
| Crush/strike | 5.6 (15) | 8.2 (22) | 13.1 (35) | 18.4 (49) | 1.5 (4) | 1.9 (5) |
| Bicycle | 7.5 (19) | 6.7 (17) | 17.4 (44) | 14.2 (36) | 3.2 (8) | 2.8 (7) |
| Home improvement | 9.1 (22) | 17.4 (42) | 19.8 (48) | 9.1 (22) | 2.5 (6) | 2.1 (5) |
| Pedestrian | 31.1 (59) | 8.4 (16) | 28.4 (54) | 22.6 (43) | 9.0 (17) | 6.3 (12) |
| Recreational | 14.4 (25) | 9.2 (16) | 26.4 (46) | 12.1 (21) | 1.2 (2) | 0.6 (1) |
| Off-road vehicles | 15.8 (27) | 5.9 (10) | 19.3 (33) | 11.7 (20) | 2.9 (5) | 0.6 (1) |
| Firearm | 60.4 (58) | 19.8 (19) | 20.8 (20) | 10.4 (10) | 7.3 (7) | 10.4 (10) |
| Self-inflicted | 71.4 (65) | 29.7 (27) | 31.9 (29) | 28.6 (26) | 16.5 (15) | 24.2 (22) |
| Other | 16.1 (41) | 16.5 (42) | 10.6 (27) | 7.8 (20) | 3.9 (10) | 2.5 (9) |
| P value* | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
*P value denotes significant differences in the injury characteristic/outcome by cause of injury.
AIS, abbreviated injury scale; ED, emergency department; ISS, injury severity score; OR, operating room; SBP, systolic blood pressure.
The 10 most common injury diagnoses in the population represented 83.0% of all diagnosis codes. Superficial head injuries and intracranial injuries were common in both study periods and were reported in 25% of all hospital admissions. The most common superficial head injuries included scalp contusions (37%), abrasions (31%) and eye injuries (17%). As shown in table 4, injury diagnoses differed between time periods with more superficial injuries to the head (23.0% to 27.3%, p<0.001) and more injury diagnoses to the knee/leg (11.7% to 14.9%, p<0.001) during the pandemic than prepandemic.
Table 4.
Specific injury diagnoses: 10 most common reported in the population
| ICD-10 code – description | Prepandemic March 11, 2019–June 30, 2019 N=3862, % (n) |
Pandemic March 11, 2020–June 30, 2020 N=3446, % (n) |
P value |
| Superficial injury* of head | 23.0 (863) | 27.3 (918) | <0.001 |
| Intracranial injury (TBI) | 25.1 (943) | 24.1 (812) | 0.37 |
| Fracture of rib(s), sternum and thoracic spine | 22.2 (832) | 21.1 (707) | 0.26 |
| Open wound of head | 15.8 (630) | 17.9 (599) | 0.23 |
| Femur fracture | 14.6 (549) | 16.0 (536) | 0.11 |
| Fracture of lumbar spine and pelvis | 14.6 (548) | 13.1 (440) | 0.07 |
| Fracture of skull and facial bones | 13.6 (511) | 12.9 (433) | 0.38 |
| Superficial injury of knee and lower leg | 11.7 (440) | 14.9 (499) | <0.001 |
| Intrathoracic organ injury – other/unspecified | 11.1 (417) | 11.5 (387) | 0.57 |
| Fracture of lower leg, including ankle | 9.5 (355) | 10.2 (342) | 0.30 |
Note: 83% of patients had one of the 10 most common injury diagnoses.
*For example, contusion, abrasion, blister and bite to head (scalp, eye, nose, ear, cheek and mouth).
TBI, Traumatic Brain Injury.
Imaging procedures were most common (91% of patients), followed by medical/surgical procedures (60%). The proportion of patients with a medical/surgical procedure increased significantly during the pandemic (57.5% to 61.9%, p<0.001) (table 5). There were also significant increases in administration procedures (eg, therapeutics and blood products, from 13.4% to 34.2%, p=0.01) and monitoring procedures (from 11.0% to 12.9%, p<0.001) during the pandemic than prepandemic. The 10 most common medical/surgical procedures represented 61.6% of all medical/surgical procedures. Compared with prepandemic, there were increases in the proportion of patients during the pandemic having a medical/surgical procedure of the general anatomy (eg, hemorrhage control, excision and drainage and tube change) from 6.9% to 8.3% (p=0.02) and procedures of the subcutaneous tissue or fascia (6.1% to 7.8%, p=0.01) and a borderline increase in procedures of the lower joints (8.1% to 9.4%, p=0.07).
Table 5.
Procedure types and 10 most common medical/surgical procedures reported in the population
| Procedure grouping by ICD-10 codes (with examples) |
Prepandemic March 11, 2019–June 30, 2019 n=3862, % (n) |
Pandemic March 11, 2020–June 30, 2020 n=3446, % (n) |
P value |
| Imaging (CT scan, X-ray) | 91.1 (3488) | 90.6 (3082) | 0.51 |
| Administration (blood products and therapeutics) | 31.4 (1201) | 34.2 (1165) | 0.01 |
| Placement (packing and immobilization) | 24.3 (931) | 24.3 (827) | 0.99 |
| Measure and monitor (ICP monitor) | 11.0 (421) | 12.9 (438) | 0.01 |
| Medical/surgical procedures (repair/replace) | 57.5 (2201) | 61.9 (2106) | <0.001 |
| Lower bone | 18.8 (718) | 19.8 (673) | 0.26 |
| Skin | 15.7 (602) | 17.0 (579) | 0.13 |
| Upper bone | 9.0 (344) | 9.9 (338) | 0.17 |
| General anatomic* | 6.9 (264) | 8.3 (282) | 0.02 |
| Respiratory | 7.5 (288) | 8.4 (284) | 0.19 |
| Subcutaneous/fascia | 6.1 (235) | 7.8 (265) | 0.01 |
| Lower joints | 8.1 (312) | 9.4 (318) | 0.07 |
| Gastrointestinal | 3.9 (149) | 4.2 (144) | 0.46 |
| Upper joints | 4.0 (153) | 4.5 (152) | 0.32 |
| Head and face | 3.1 (120) | 3.2 (110) | 0.81 |
Sixty percent of patients had one of the 10 most common medical/surgical procedures.
*For example, hemorrhage control, excision and drainage, tube change and biopsy.
ICP, Intracranial Pressure Monitor.
Additional population comparisons
When examining the abbreviated period to coincide with the White House guidelines, cause of injury significantly differed by period similarly to what was observed in the total study period (p<0.001) (online supplemental table 1). There were decreases in MVCs and recreation/sport injuries and increases in assaults and off-road vehicle injuries. Compared with prepandemic, the abbreviated time period also demonstrated significant increases in self-inflicted injuries during the pandemic (0.83% vs 1.73%, p=0.03, (online supplemental figure 1) and increases in falls (42.9% vs 47.5%, p=0.01). The significant increase in falls only during the abbreviated study period is presented in figure 1A.
tsaco-2020-000655supp001.pdf (191.1KB, pdf)
The comparison of cause of injury between 2018 and 2019 is presented in online supplemental table 2; overall, there was no statistically significant difference in injury cause. Individual causes of injury that differed between prepandemic years were MVCs (p=0.03) and pedestrian injuries (p=0.01). All remaining causes were not significant different between 2018 and 2019: fall, assault, motorcycle crash, worksite injury, crush/strike, bicycle injury, home improvement injury, recreational injury, off-road vehicle injury, firearms, self-inflicted injuries and ‘other injuries.
Discussion
This study adds to the literature examining the effect of the COVID-19 pandemic on traumatic injury patterns in the USA. The primary findings of this multicenter study of community level I trauma centers suggests that the pandemic had a significant effect on traumatic injury patterns and causes. These findings are to be expected because of the unprecedented scale to which the pandemic related restrictions affected our daily lives. The main findings demonstrate significant increases in the proportion of injuries due to assaults and injuries from biking and off-road vehicles within the context of an overall decrease in the volume of injuries. There were also significant decreases in MVCs, recreational injuries, pedestrian injuries and worksite injuries. The shift in injury patterns led to greater hospital resource utilization with more procedures required, longer ICU and hospital LOS and higher mortality.
The largest reductions were from MVCs and pedestrian injuries. There were fewer vehicles on the road due to shelter-in-place orders that closed schools and non-essential businesses. A California report of traffic identified a 20%–50% reduction in daily travel and an approximately 50% reduction in vehicular collisions.32 Interestingly, a study from London, UK, reported overall reductions in orthopedic trauma admissions but no change in the proportion of orthopedic injuries resulting from vehicular injuries, 15% in the same period in 2019 and 2020.16 MVCs also demonstrated a significant decrease from 2018 to 2019 and a decreased trend in incidence from 2018 to 2019 to 2020 (p<0.001), suggesting the decrease observed in this study in 2020 might not be entirely attributable to the pandemic and subsequent restrictions. MVCs and pedestrian injuries typically result in multisystem trauma, with 25%–28% of all patients in our study suffering severe (ISS ≥16) overall injuries. Fortunately, both of these causes of injury decreased with the pandemic.
Sports injuries decreased. The largest reduction was skisport injuries, from 44% to 10% of sports-related injuries, which reflects the location of three of our participating hospitals’ location in Colorado and early closure of ski resorts due to the pandemic. Conversely, there were increases in off-road vehicle injuries, which include ATVs and snowmobiles, likely because these activities are social distance ‘friendly’. The tradeoff between sports injuries and off-road vehicle injuries did not appear to have a large impact on resource allocation because these causes share similar injury severity patterns and low mortality of <1%.
Caputi and colleagues33 reported a substantial spike in Google searches for guns to an unprecedented level during the pandemic, and Google search is frequently used as a proxy for gun purchases. Prior research shows that events such as pandemics and civil unrest are linked to an increase in violence against women and children.34 We speculated that there would be an increase in assaults, firearm injuries and self-inflicted injuries related to social distancing and sheltering in place. Across the entire study period, only assaults significantly increased from 6.9% to 8.5% of all trauma hospital admissions. When the study period was abbreviated to March 11–April 30 to coincide with the White House restrictions, there were significant increases in self-inflicted injuries from 0.8% to 1.7%. Assaults and self-inflicted injuries required high hospital resource utilization, with 22% of assaults and 30% of self-inflicted injuries going directly to the OR from the ED. Self-inflicted injuries also resulted in significant mortality, 24%, more than all other causes of injury. There are also additional non-medical ancillary hospital resources required of victims of assault and self-harm such as social work consults. This study suggests there should be additional planning for and anticipation of increasing assault admissions and self-inflicted injuries during pandemics particularly when restrictions are put in place.
We also speculated that shelter-in-place sanctions would result in an increase in home improvement projects, which have the secondary effect of increasing traumatic injuries requiring hospitalization. In a study by Zhu et al,9 the authors noted an increase in elderly hip fractures due to injuries from chainsaws and falls from roofs/trees. Our study did not find an increase in injuries related to home improvement projects, which represented approximately 3% of injuries in both time periods. On the contrary, worksite injuries decreased during the pandemic period likely because shelter-in-place orders led to an increase in remote work. Worksite injuries represent a diverse group of injury causes that predominantly include falls and ‘other’ causes.
Similar to Nuñez and colleagues,22 we observed reductions in MVC injuries but no change in fall injuries and hip fracture volume. When we limited the analysis to the March 11–April 30 study period, the proportion of falls modestly increased, although the absolute number of admissions was still lower in the pandemic period than prepandemic. Injury prevention efforts could be targeted during the pandemic, as the lack of reduction in falls during the pandemic makes fall prevention efforts still timely and relevant.9
Regional COVID-19 cases and subsequent hospital surge will impact the ability of the trauma system to deliver optimal care, even if trauma patients do not have COVID-19. There is no shortage of publications describing hospital resource planning and risk stratification for surgical procedures,7 14 15 18 24 26 35 such as increased use of conservative orthopedic management,15 24 28 strategies for protecting clinicians and patients,4 20 23 25 35 including changing work shifts and surge capacity10 17 and use of teleconsult.19 These studies were published based on the assumption that trauma patient volume would decrease, but these resource and planning guidelines may need further revision based on injury patterns since observed during the pandemic.
There are limitations of the study. First, this was a retrospective registry study. Second, available data on the pandemic’s effects are limited to spring/summer seasons. Injury patterns seen during fall and winter seasons might vary greatly compared with those presented in this study. Third, the social distance orders broadly affected the USA between March 11 and April 30, before phased reopening was non-uniformly rolled out in May and June. For instance, stay-at-home orders in Texas expired May 1 but were reinstituted on June 25, while Colorado’s ‘safer at home’ order was in effect until May 27. Fourth, the findings may not be generalizable to future COVID-19 phases and ‘waves’ or other future pandemics unless directives and orders are similar, at least locally, to what occurred during the 2020 pandemic study period.
Conclusions
This study identified that traumatic injury causes and subsequent diagnoses and procedures were significantly changed by the pandemic. During times of pandemic related restrictions including shelter-in-place and social distancing orders, hospitals must prepare for more than the potential demand of an influx of infected patients. This study demonstrated increases in assaults, bicycle crashes and off-road vehicle injuries and decreases in motor vehicle/pedestrian injuries, worksite injuries and recreational injuries as people were ordered to stay at home. Trauma centers must adjust to meet the changing demands associated with altered traumatic injury patterns and causes. These shifts in injury patterns were associated with increased hospital resources. These findings may help with planning and decision making.
Acknowledgments
We would like to acknowledge Oliwier Dziadkowiec, MD (Swedish Medical Center) for mentorship of resident Jalina Mueller.
Footnotes
Contributors: Conception: KS, RC and JM. IRB drafting: KS, RC, MMC, ML, GB and and DB-O. Study design: KS. Analysis of data: KS and AT. Interpretation of data: RC, JM, MMC, ML, GB and DB-O. Drafting: KS. Manuscript revisions: RC, JM, AT, MMC, ML, GB and DB-O. Administrative support: DB-O. All authors gave final approval of the submitted manuscript.
Funding: The study was investigator initiated. Internal funding provided by Swedish Medical Center, St. Anthony Hospital, Medical City Plano, Penrose-St. Francis Medical Center, Wesley Medical Center and Research Medical Center Kansas City.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request. Data are available on reasonable request from the corresponding author.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
All participating centers received approval through their respective Institutional Review Boards with a waiver of consent and HIPAA authorization: HealthONE IRB (Swedish Medical Center, Englewood, CO and Wesley Medical Center, Wichita, KS); Catholic Health Initiatives IRB (St. Anthony Hospital, Lakewood, CO; Penrose Hospital, Colorado Springs, CO); HCA IRB (Medical City Plano, Plano, TX) and Western IRB (Research Medical Center, Kansas City, MO).
References
- 1.Lerner EB, Newgard CD, Mann NC, Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV. Effect of the coronavirus disease 2019 (COVID-19) pandemic on the U.S. emergency medical services system: a preliminary report. Acad Emerg Med 2020;27:693–9. 10.1111/acem.14051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:699–704. 10.15585/mmwr.mm6923e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forrester JD, Liou R, Knowlton LM, Jou RM, Spain DA. Impact of shelter-in-place order for COVID-19 on trauma activations: SANTA Clara County, California, March 2020. Trauma Surg Acute Care Open 2020;5:e000505. 10.1136/tsaco-2020-000505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathur S, Jeremy Ng CF, Koh F, Cai M, Palaniappan G, Linn YL, Lim HL, Lakshman R, Ling XS, Chin ST, et al. Development of an enhanced acute care surgery service in response to the COVID-19 global pandemic. Injury 2020;51:2135–41. 10.1016/j.injury.2020.06.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J 2020;133:81–8. [PubMed] [Google Scholar]
- 6.Balogh ZJ, Way TL, Hoswell RL. The epidemiology of trauma during a pandemic. Injury 2020;51:1243–4. 10.1016/j.injury.2020.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, Zeng L, Li Z, Mao Q, Liu D, Zhang L, Zhang H, Xie Y, Liu G, Gan X, et al. Emergency trauma care during the outbreak of corona virus disease 2019 (COVID-19) in China. World J Emerg Surg 2020;15:33. 10.1186/s13017-020-00312-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lv H, Zhang Q, Yin Y, Zhu Y, Wang J, Hou Z, Zhang Y, Chen W. Epidemiologic characteristics of traumatic fractures during the outbreak of coronavirus disease 2019 (COVID-19) in China: A retrospective & comparative multi-center study. Injury 2020;51:1698–704. 10.1016/j.injury.2020.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhu Y, Chen W, Xin X, Yin Y, Hu J, Lv H, Li W, Deng X, Zhu C, Zhu J, et al. Epidemiologic characteristics of traumatic fractures in elderly patients during the outbreak of coronavirus disease 2019 in China. Int Orthop 2020;44:1565–70. 10.1007/s00264-020-04575-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ilenghoven D, Hisham A, Ibrahim S, Mohd Yussof SJ. Restructuring burns management during the COVID-19 pandemic: a Malaysian experience. Burns 2020;46:1236–9. 10.1016/j.burns.2020.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong JSH, Cheung KMC. Impact of COVID-19 on orthopaedic and trauma service: an epidemiological study. J Bone Joint Surg Am 2020;102:e80. 10.2106/JBJS.20.00775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blackhall KK, Downie IP, Ramchandani P, Kusanale A, Walsh S, Srinivasan B, Shields H, Brennan PA, Singh RP. Provision of Emergency Maxillofacial Service During the COVID-19 Pandemic : A Collaborative Five Centre UK Study. Br J Oral Maxillofac Surg 2020;58:698-703. 10.1016/j.bjoms.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hadfield JN, Gray AC. The evolving COVID-19 effect on hip fracture patients. Injury 2020;51:1411–2. 10.1016/j.injury.2020.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holmes S, Bhatti N, Bhandari R, Chatzopoulou D. Toward a consensus view in the management of acute facial injuries during the Covid-19 pandemic. Br J Oral Maxillofac Surg 2020;58:571–6. 10.1016/j.bjoms.2020.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iyengar K, Vaish A, Vaishya R. Revisiting conservative orthopaedic management of fractures during COVID-19 pandemic. J Clin Orthop Trauma 2020;11:718–20. 10.1016/j.jcot.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park C, Sugand K, Nathwani D, Bhattacharya R, Sarraf KM. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the "golden month". Acta Orthop 2020;91:556–61. 10.1080/17453674.2020.1783621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Casiraghi A, Domenicucci M, Cattaneo S, Maggini E, Albertini F, Avanzini S, Pansi Marini M, Galante C, Guizzi P, Milano G. Operational strategies of a trauma hub in early coronavirus disease 2019 pandemic. Int Orthop 2020;44:1511–8. 10.1007/s00264-020-04635-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haffer H, Schömig F, Rickert M, Randau T, Raschke M, Wirtz D, Pumberger M, Perka C. Impact of the COVID-19 pandemic on orthopaedic and trauma surgery in university hospitals in Germany: results of a nationwide survey. J Bone Joint Surg Am 2020;102:e78. 10.2106/JBJS.20.00756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joubert C, Desse N, Bernard C, Julien Cungi P, Bordes J, Dagain A. Indirect effects of the COVID19 pandemic in patients requiring neurosurgical care: will the second wave carry more severe neurosurgical patients? Br J Neurosurg 2020:1–3. 10.1080/02688697.2020.1782835 [DOI] [PubMed] [Google Scholar]
- 20.Kenanidis E, Tsiridis E. "Flattening the curve" of COVID-19 pandemic in orthopaedics and trauma: the Greek perspective. Injury 2020;51:1681–2. 10.1016/j.injury.2020.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lopez Martinez JJ, Rodríguez-Roiz JM, Salcedo Cánovas C. [Musculoskeletal injuries secondary to exercise during confinement by the pandemic COVID-19]. Med Clin 2020;155:221–2. 10.1016/j.medcle.2020.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nuñez JH, Sallent A, Lakhani K, Guerra-Farfan E, Vidal N, Ekhtiari S, Minguell J. Impact of the COVID-19 pandemic on an emergency Traumatology service: experience at a tertiary trauma centre in Spain. Injury 2020;51:1414–8. 10.1016/j.injury.2020.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rodrigues-Pinto R, Sousa R, Oliveira A. Preparing to perform trauma and orthopaedic surgery on patients with COVID-19. J Bone Joint Surg Am 2020;102:946–50. 10.2106/JBJS.20.00454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joseph T, Civil I. Trauma care in a low-COVID pandemic environment: a new normal. Injury 2020;51:1245–6. 10.1016/j.injury.2020.05.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barret JP, Chong SJ, Depetris N, Fisher MD, Luo G, Moiemen N, Pham T, Qiao L, Wibbenmeyer L, Matsumura H. Burn center function during the COVID-19 pandemic: an international multi-center report of strategy and experience. Burns 2020;46:1021–35. 10.1016/j.burns.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arnaout O, Patel A, Carter B, Chiocca EA. Letter: adaptation under fire: two Harvard neurosurgical services during the COVID-19 pandemic. Neurosurgery 2020;87:E173–7. 10.1093/neuros/nyaa146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Valera EM. When pandemics clash: gendered violence-related traumatic brain injuries in women since COVID-19. EClinicalMedicine 2020;24:100423. 10.1016/j.eclinm.2020.100423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phillips MR, Chang Y, Zura RD, Mehta S, Giannoudis PV, Nolte PA, Bhandari M. Impact of COVID-19 on orthopaedic care: a call for nonoperative management. Ther Adv Musculoskelet Dis 2020;12:1759720x20934276. 10.1177/1759720X20934276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stoker S, McDaniel D, Crean T, Maddox J, Jawanda G, Krentz N, Best J, Speicher M, Siwiec R. Effect of Shelter-in-Place orders and the COVID-19 pandemic on orthopaedic trauma at a community level II trauma center. J Orthop Trauma 2020;34:e336–42. 10.1097/BOT.0000000000001860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DiMaggio C, Ayoung-Chee P, Shinseki M, Wilson C, Marshall G, Lee DC, Wall S, Maulana S, Leon Pachter H, Frangos S. Traumatic injury in the United States: in-patient epidemiology 2000-2011. Injury 2016;47:1393–403. 10.1016/j.injury.2016.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention . Cases in the US USA: CDC. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html (29 Jul 2020).
- 32.Shilling F, Waetjen D. Special report: impact of COVID19 on California traffic accidents, 2020. [Google Scholar]
- 33.Caputi TL, Ayers JW, Dredze M, Suplina N, Burd-Sharps S. Collateral crises of gun preparation and the COVID-19 pandemic: Infodemiology study. JMIR Public Health Surveill 2020;6:e19369. 10.2196/19369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during covid-19 pandemic restrictions. BMJ 2020;28:m1712. 10.1136/bmj.m1712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Soltany A, Hamouda M, Ghzawi A, Sharaqi A, Negida A, Soliman S, Benmelouka AY. A scoping review of the impact of COVID-19 pandemic on surgical practice. Ann Med Surg 2020;57:24–36. 10.1016/j.amsu.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2020-000655supp001.pdf (191.1KB, pdf)
Data Availability Statement
Data are available on reasonable request. Data are available on reasonable request from the corresponding author.


