Abstract
Background
The aerosol box was rapidly developed and disseminated to minimize viral exposure during aerosolizing procedures during the COVID-19 pandemic, yet users may not understand how to use and clean the device. This could potentially lead to increased viral exposure to subsequent patients and practitioners. We evaluated intraoperative contamination and aerosol box decontamination and the impact of a preoperative educational visual aid.
Methods
Using a double-blinded randomized design, forty-four anesthesiology trainees and faculty completed a simulated anesthetic case using an aerosol box contaminated with a fluorescent marker; half of the subjects received a visual aid prior to the simulation. Intraoperative contamination was evaluated at 10 standardized locations using an ultraviolet (UV) light. Next, subjects were instructed to clean the aerosol box for use on the next patient. Following cleaning, the box was evaluated for decontamination using an UV light.
Results
Median total contamination score was significantly reduced in the experimental group (5.0 vs. 10.0, P < 0.001). The aerosol box was completely cleaned by 36.4% of subjects in the experimental group compared to 4.5% in the control group (P = 0.009).
Conclusions
The use of a visual aid significantly decreased intraoperative contamination and improved box cleaning. Despite these findings, a potentially clinically significant amount of viral exposure may exist. Thorough evaluation of the risks and benefits of the aerosol box should be completed prior to use. If an aerosol box is used, a visual aid should be considered to remind practitioners how to best use and clean the box.
Keywords: Airway management, Anesthesiology, Audiovisual aids, Equipment and supplies, High fidelity simulation training, Infection control
Introduction
The coronavirus disease (COVID-19) pandemic has led to numerous developments in personal protective equipment (PPE) as a means to protect healthcare workers from Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus responsible for COVID-19 [1,2]. Respiratory failure associated with COVID-19 often necessitates tracheal intubation, a high risk procedure exposing healthcare workers to droplet and aerosol particles carrying a significant viral load [3–5].
One potential exposure mitigation strategy is the use of a barrier device, such as a clear plastic aerosol box, over the patient’s head to contain any aerosols or droplets [6,7]. Early in the pandemic, news outlets and social media rapidly disseminated the construction and use of these aerosol boxes [8] and numerous variations on this basic design exist [9–11].
Simulation studies have demonstrated the effectiveness of aerosol boxes in preventing droplet spread [12–14], but concerns exist regarding clinical effectiveness in aerosol prevention and possible unintended complications with their use [8,15–18]. Due to the rapid development and dissemination of this medical device, no formal instructions or guidelines for use exist. Users may not know how to appropriately use and decontaminate the aerosol box that may lead to the box itself becoming a vector for viral transmission between patients or practitioners. Furthermore, the simple design may lead users to believe they know how to use the device even though they may not. Because medical devices should include instructions for proper use and this device lacks any such instructions, the authors postulate that an educational visual aid for proper aerosol box use may lead to safer utilization of the aerosol box.
In this study, we aim to evaluate the potential for viral particle spread using a fluorescent marker during a simulated anesthetic utilizing an aerosol box. Specifically, we have included an educational visual aid, containing a targeted list of recommendations describing best practices for the use and cleaning of this novel medical device [19–21]. Our primary endpoint was decreased intraoperative contamination of the anesthesia work area, while our secondary endpoint was improved decontamination of the aerosol box following use.
Materials and Methods
This study received an exemption from written consent by our Institutional Review Board. Anesthesiology trainees and faculty were voluntarily recruited to participate in this prospective, double-blinded, randomized-controlled study. Randomization was completed using a computer-generated randomization program (Research Randomizer, Urbaniak GC Plous S, www.randomizer.org). The study was completed in the Mount Sinai Department of Anesthesiology HELPS Simulation Center.
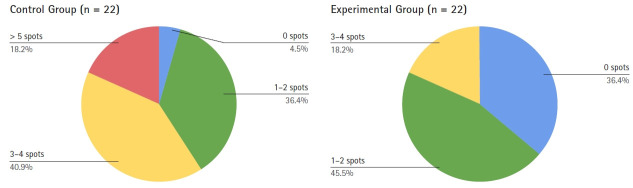
Each subject was randomized to an experimental group and received a visual aid describing how to use an aerosol box (Fig. 1), or to a control group without a visual aid. The visual aid content was developed using World Health Organization recommendations [19] as well as anesthesiology-specific guidelines [20,21] for infection control and intubation during the COVID-19 pandemic.
Fig. 1.
Educational visual aid for aerosol box use provided to the experimental group.
One study team member not involved in data collection provided the subject with a simulation prompt describing a patient under investigation for COVID-19 requiring a laparoscopic appendectomy. The study team member also provided the educational visual aid for subjects in the experimental group. The subject then had the opportunity to practice intubating a mannequin with an aerosol box in place, using a video laryngoscope (GlideScope™, Verathon Inc., USA); each subject was provided with sufficient time until they felt comfortable. The subjects were then brought into another room for the simulation. The visual aid was left in the previous room in order to keep the remaining study team members blinded to their group allocation.
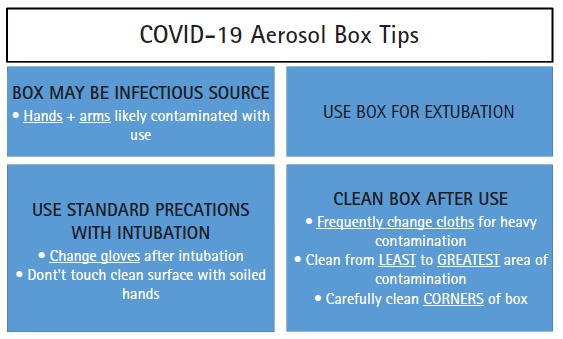
The aerosol box was created using the initial widely publicized design specifications [6] and constructed using clear acrylic plastic and rubber cement. The aerosol box was then placed over an airway management trainer (Laerdal, Norway). An ultraviolet (UV) fluorescent marker (Glo-germ™, Glo-Germ Company, USA) was used in a lotion and powder form. One ml of the lotion was placed on the high-fidelity simulator’s lips and inside the mouth to simulate oral secretions, while ⅛ teaspoon of the powder was distributed uniformly within the inside of the aerosol box using a powder brush, to simulate droplet contamination (Fig. 2). The fluorescent marker is not fluorescent under normal lighting conditions and was minimally visible during the simulation.
Fig. 2.
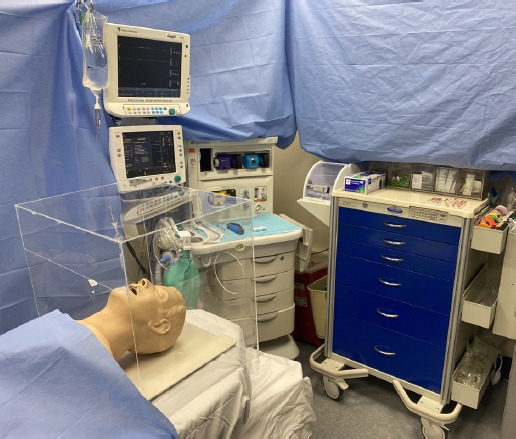
Image of simulated operating room with aerosol box in position.
A standardized simulation sequence was utilized (Supplementary Table 1). Vital signs were generated using a high-fidelity patient simulator (CAE human patient simulator, Canada). Subjects were instructed to wear standard PPE for patients under investigation for COVID-19, including a gown, gloves, and surgical mask according to our hospital protocols. In order to conserve PPE, N95 respirators, masks, eye protection, and head coverings were not used in the study. Each subject then induced anesthesia and intubated the high-fidelity patient simulator with a video laryngoscope with the aerosol box in place. Subjects were required to administer drugs using saline filled syringes through a stopcock on the intravenous line. Additional relaxation was requested by the simulated surgeon prior to incision, in order to prompt additional medications to be administered through the intravenous line. Upon completion of the simulated surgery, the subject then prepared for and performed extubation of the high-fidelity simulator.
Upon completion of the simulation, 10 standardized sites (Table 1) were evaluated for viral contamination using an UV light by two study team members who were blinded to subject randomization. These sites were selected based on previous intraoperative contamination studies [22–24]. Sites were deemed clean if no fluorescence was observed (0) or contaminated if any amount of fluorescence was visualized (1). The primary outcome was determined to be a total contamination score with a maximum score of 10. Subjects waited in the adjacent room while contamination scoring took place. Additionally, a secondary outcome was individual sites of contamination.
Table 1.
Individual Sites Evaluated for Fluorescent Marker Contamination Following Simulated Anesthetic
| 1. Outside of the aerosol box |
| 2. Reservoir bag |
| 3. Adjustable Pressure Limiting (APL) valve |
| 4. Anesthesia machine workstation |
| 5. Vital signs monitor or ventilator screen |
| 6. Intravenous stopcock |
| 7. Medication syringes |
| 8. Anesthesia supply cart |
| 9. Subject gown |
| 10. Subject gloves |
Finally, subjects were then instructed to clean the aerosol box in order for it to be used for their next patient. Cleaning wipes capable of cleaning the fluorescent marker (PDI Sani-Cloth, USA) were provided and subjects were able to clean the box until they were satisfied with its cleanliness. Two study team members blinded to subject randomization then examined the box under a UV light for areas not cleaned by the cleaning wipe. A scoring system was developed using a numbering system as follows: 1 = completely clean, 2 = 1–2 areas missed, 3 = 3–4 areas missed and 4 = 5 or more areas missed. Box cleaning scores were evaluated as a secondary endpoint.
Between simulations, all surfaces in the simulation lab were fully cleaned, as confirmed by two members of the study team using a UV light. Any materials that could not be fully cleaned were discarded and replaced.
Statistical analysis
Prior to the beginning of the study, pilot simulations without the educational visual aid had a median contamination score of 8.0 (Q1, Q3; 7.0, 9.0). We predicted the educational visual aid would decrease the contamination score that would be decreased by 50% to a median contamination score of 4.0. Using an ⍺ of 0.05 and a ꞵ of 0.2 and the predicted 50% decrease in contamination score, it was determined that a sample size of 22 subjects in each group would be needed for sufficient power. In order to allow for potential dropout, we aimed to recruit 24 subjects per group in order to reach our targeted sample size, though no subjects dropped out and we were able to achieve a full sample of 22 subjects per group. All continuous variables were first assessed for normality via Shaprio-Wilk or Kolmogorov–Smirnov tests, where applicable as well as visual inspections of histograms. All continuous variables were found to be non-normal and are reported as median (Q1, Q3). Proportions are reported as n (%). For categorical variables, chi-square tests were utilized, unless one value in the 2 x 2 matrix was under 5, in which case Fischer’s exact test was utilized. For binary tests, odds ratios with 95% CIs are reported. For continuous non-normally distributed variables, Mann-Whitney U test was used, with differences between groups and 95% CIs estimated via Hodges-Lehman estimation. All calculations were performed via SPSS Statistics Version 24 (IBM Corp., USA).
Results
Forty-four subjects were enrolled in the study with 22 subjects in each group (Fig. 3). The control group consisted of 16 trainees and six faculty members, while the experimental group consisted of 14 trainees and eight faculty members. All subjects completed the study.
Fig. 3.
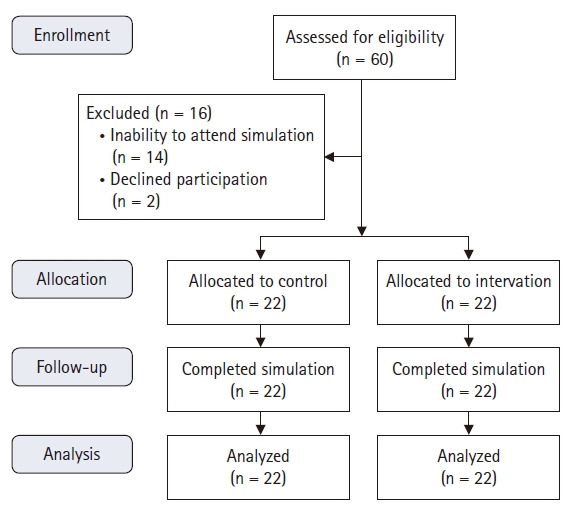
CONSORT diagram.
Our primary endpoint, median total contamination score, was 10.0 (8.0, 10.0) for the control group and 5.0 (4.0, 8.25) for the experimental group (Supplementary Fig. 1). Total contamination score was found to be significantly reduced in the experimental group (P < 0.001). When evaluating only trainees, the median total contamination scores were 10.0 (8.25, 10.0) and 6.0 (4.75, 9.0) for the experimental group (P = 0.002). For faculty members, the median total contamination scores were 8.5 (7.5, 10.0) for the control group and 5.0 (4.0, 5.0) for the experimental group (P = 0.001).
Individual site rates of contamination, a secondary exploratory endpoint, are in Table 2. Sites with statistically significant reductions in contamination for the experimental group include the reservoir bag (P = 0.002), adjustable pressure limiting (APL) valve (P = 0.003), vital signs monitor or ventilator screen (P < 0.001), I.V. stopcock (P = 0.026), medication syringes (P < 0.001), and anesthesia supply cart (P = 0.012). No statistically significant difference in contamination was noted for outside of the aerosol box, anesthesia machine workstation, gown, or gloves.
Table 2.
Presence of Fluorescent Marker Contamination Following Simulated Anesthetic at Individual Locations with Total Contamination Score
| Location | Control group (n = 22) | Experimental group (n = 22) | P value |
|---|---|---|---|
| Outside of the aerosol box | 22 (100) | 19 (86.3) | 0.073 |
| Reservoir bag | 17 (77.3) | 7 (31.8) | 0.002 |
| Adjustable Pressure Limiting (APL) valve | 20 (90.9) | 11 (50.0) | 0.003 |
| Anesthesia machine workstation | 20 (90.9) | 17 (77.3) | 0.216 |
| Vital signs monitor or ventilator screen | 18 (81.8) | 6 (27.3) | < 0.001 |
| Intravenous stopcock | 18 (81.8) | 11 (50.0) | 0.026 |
| Medication syringes | 18 (81.8) | 6 (27.3) | < 0.001 |
| Anesthesia supply cart | 18 (81.8) | 10 (45.5) | 0.012 |
| Subject gown | 22 (100.0) | 22 (100.0) | N/A |
| Subject gloves | 21 (95.5) | 21 (95.5) | 1.000 |
| Total score* | 10 | 5 | < 0.001 |
Values are presented as number (%). *Reported as total score number, not as a number or percent contaminated.
The distribution of aerosol box cleaning scores, a secondary endpoint, is shown in Fig. 4. A statistically significant difference in distribution between the control and experimental group was found (P = 0.009). In the experimental group, 36.4% of subjects completely cleaned the aerosol box compared to only 4.5% in the control group (P = 0.009, OR = 1.5 [1.08, 2.08]).
Fig. 4.
Aerosol box cleaning ratings. Data represents number of spots on the aerosol box that were not cleaned. Data with significant difference between control and experimental groups (P = 0.009).
Discussion
The aerosol box has been promoted throughout scientific journals, news, and social media as an effective method for limiting viral exposure during aerosolizing procedures, yet no high-quality evidence for its effectiveness exists. Despite its use, concerns exist regarding practitioner understanding of proper aerosol box use and potential unintended viral contamination associated with improper box use.
Our study is significant for several findings. First, we demonstrated that intraoperative contamination can be decreased with the use of a visual aid as measured as a decrease in the total contamination score. Individual sites with consistent contamination for all subjects included the outside of the aerosol box, the anesthesia workstation, and the subjects’ gown and gloves; therefore care must be taken to consistently avoid contamination of these sites. This contamination, particularly of the gown and gloves, could lead to increased intraoperative contamination and potential viral exposure to healthcare workers or subsequent patients. Furthermore, contamination of the anesthesia workstation may provide a reservoir for further contamination throughout an anesthetic or procedure despite proper hand hygiene [25].
Secondly, this study showed that cleaning of an aerosol box can be increased with the use of a visual aid. The effectiveness of this visual aid is likely associated with the lack of any pre-existing instructions accompanying this rapidly developed device as well as the visual aid serving as a reminder of the infectious potential associated with aerosol box use. In spite of the visual aid, nearly two thirds of aerosol boxes remained contaminated in the experimental group. Of particular note was the remaining contamination at the corners and edges of the box that suggests that these may be areas to focus on to fully decontaminate the box. The potential for incomplete terminal cleaning of operating rooms exists [26,27] and any amount of contamination may become clinically relevant if viral transfer to a ‘clean’ environment occurs. SARS-CoV-2 has been shown to be stable on plastic and steel surfaces for up to 72 hours [28] and could easily be transmitted between patients or practitioners if intraoperative surfaces or the aerosol box were improperly cleaned.
Finally, and most strikingly, we demonstrated potentially clinically significant contamination of the operating room and aerosol box independent of visual aid use. Several explanations for high rates of intraoperative contamination and contaminated aerosol boxes exist. The aerosol box could potentially be seen as a false sense of security to the subjects that could lead to less vigilance for infection control when compared to intubation without an aerosol box. Studies prior to the COVID-19 pandemic have found intraoperative contamination to be high [25] despite recommendations such as improved intraoperative hand hygiene [29], double gloving for intubation [23], protective devices during intubation [24], and more. Additionally, the aerosol box is an unfamiliar device to most practitioners and the novelty of it may cause changes in practice leading to increased intraoperative contamination or lack of thorough decontamination. The box’s geometry may also lend to a lack of thorough cleaning as the corners and edges were most often missed by subjects.
Our study adds to the growing number of criticisms associated with aerosol box use. Concerns associated with increased difficulty with airway management, restricted access to the patient for assistants, difficulties with portability in emergencies, the requirement for specialized supplies, potential to damage PPE, and potential redirection of aerosols towards the intubator have all been raised [8,15–18]. As a result of the current study, we would add potential for viral contamination to the list of concerns with aerosol boxes. Further investigation into intubation barrier devices’ effectiveness and safety are required.
The greatest limitation of this study is related to the simulation environment. Subjects were told they were in an operating room taking care of a person under investigation for COVID-19, but in reality, were in a simulation lab and may not have been as careful as a real-life situation. Similarly, the subjects knew they were being observed for the study and the Hawthorne effect must be considered. Although the fluorescent powder used in this study has commonly been used as a marker for viral and bacterial contamination, its use as a simulated SARS-CoV-2 virus has not been proven. One modification to this study could have been to evaluate if the fluorescent marker contamination was spread to the next simulated patient following cleaning, but this was not done due to time constraints. Subjects had no prior experience using the aerosol box during a simulation or in-patient care, but all were aware of the concept through scientific journals, news, and social media. Despite this lack of prior experience, we believe this data is generalizable because prior to COVID-19 the aerosol box was not used by any practitioners. However, these findings may be different in a practitioner with more experience using the aerosol box. Finally, numerous barrier devices exist and several modifications to the original design used in this study have been made; it is unclear how the current study’s findings would translate to other aerosol box designs.
We recommend a thorough evaluation of needs for those considering aerosol box use as it may have numerous unintended consequences. If an aerosol box is used, all users should receive at minimum a visual aid describing how to best use and clean the aerosol box. Given the uncertain benefits, our recommendation is to forgo aerosol box use and utilize appropriate PPE with all necessary precautions such as a rapid sequence induction and intubation with a video laryngoscope [1,30]. It is vital that all practitioners, regardless of aerosol box use, stay vigilant during use and cleaning of the operating room.
Footnotes
Funding
This research was supported internally by the Department of Anesthesiology, Perioperative & Pain Medicine at the Icahn School of Medicine at Mount Sinai. No external funding was received for this research.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Garrett W. Burnett (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Supervision; Writing – original draft; Writing – review & editing)
George Zhou (Conceptualization; Data curation; Investigation; Methodology; Writing – review & editing)
Eric A. Fried (Data curation; Investigation; Writing – review & editing)
Ronak S. Shah (Data curation; Writing – review & editing)
Chang Park (Conceptualization; Writing – review & editing)
Daniel Katz (Conceptualization; Formal analysis; Methodology; Supervision; Writing – review & editing)
Supplementary Materials
Standardized simulation sequence
Total contamination score for control and experimental groups.
References
- 1.World Health Organization . Geneva: WHO; 2020. Dec 23, Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages [Internet] [cited 2020 Jul 13]. Available from https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages. [Google Scholar]
- 2.Centers for Disease Control and Prevention . Atlanta: CDC; Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic [Internet] [updated Feb 23; cited 2020 Jul 13]. Available from https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. [Google Scholar]
- 3.El-Boghdadly K, Wong DJ, Owen R, Neuman MD, Pocock S, Carlisle JB, et al. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study. Anaesthesia. 2020;75:1437–47. doi: 10.1111/anae.15170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7:e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banik RK, Ulrich A. Evidence of short-range aerosol transmission of SARS-CoV-2 and call for universal airborne precautions for anesthesiologists during the COVID-19 pandemic. Anesth Analg. 2020;131:e102–4. doi: 10.1213/ANE.0000000000004933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai HY. Aerosol Box - Design [Internet] 2020 Jul 9; [2020 Jul 9]. Available from https://sites.google.com/view/aerosolbox/design.
- 7.Everington K. Taipei: Taiwan News; 2020. Mar 23, Taiwanese doctor invents device to protect US doctors against coronavirus [Internet] [cited 2020 Jul 9]. Available from https://www.taiwannews.com.tw/en/news/3902435. [Google Scholar]
- 8.Turner MC, Duggan LV, Glezerson BA, Marshall SD. Thinking outside the (acrylic) box: a framework for the local use of custom-made medical devices. Anaesthesia. 2020;75:1566–9. doi: 10.1111/anae.15152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Endersby RV, Ho EC, Spencer AO, Goldstein DH, Schubert E. Barrier devices for reducing aerosol and droplet transmission in COVID-19 patients: advantages, disadvantages, and alternative solutions. Anesth Analg. 2020;131:e121–3. doi: 10.1213/ANE.0000000000004953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gazoni FM, Amato PE, Malik ZM, Durieux ME. The impact of perioperative catastrophes on anesthesiologists: results of a national survey. Anesth Analg. 2012;114:596–603. doi: 10.1213/ANE.0b013e318227524e. [DOI] [PubMed] [Google Scholar]
- 11.Kinjo S, Dudley M, Sakai N. Modified wake forest type protective shield for an asymptomatic, COVID-19 nonconfirmed patient for intubation undergoing urgent surgery. Anesth Analg. 2020;131:e127–8. doi: 10.1213/ANE.0000000000004964. [DOI] [PubMed] [Google Scholar]
- 12.Canelli R, Connor CW, Gonzalez M, Nozari A, Ortega R. Barrier Enclosure during Endotracheal Intubation. N Engl J Med. 2020;382:1957–8. doi: 10.1056/NEJMc2007589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feldman O, Meir M, Shavit D, Idelman R, Shavit I. Exposure to a surrogate measure of contamination from simulated patients by emergency department personnel wearing personal protective equipment. JAMA. 2020;323:2091–3. doi: 10.1001/jama.2020.6633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laosuwan P, Earsakul A, Pannangpetch P, Sereeyotin J. Acrylic box versus plastic sheet covering on droplet dispersal during extubation in COVID-19 patients. Anesth Analg. 2020;131:e106–8. doi: 10.1213/ANE.0000000000004937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Begley JL, Lavery KE, Nickson CP, Brewster DJ. The aerosol box for intubation in coronavirus disease 2019 patients: an in-situ simulation crossover study. Anaesthesia. 2020;75:1014–21. doi: 10.1111/anae.15115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenblatt WH, Sherman JD. More on Barrier Enclosure during Endotracheal Intubation. N Engl J Med. 2020;382:e69. doi: 10.1056/NEJMc2012960. [DOI] [PubMed] [Google Scholar]
- 17.Simpson JP, Wong DN, Verco L, Carter R, Dzidowski M, Chan PY. Measurement of airborne particle exposure during simulated tracheal intubation using various proposed aerosol containment devices during the COVID-19 pandemic. Anaesthesia. 2020;75:1587–95. doi: 10.1111/anae.15188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brown H, Preston D, Bhoja R. Thinking outside the Box: A Low-cost and Pragmatic Alternative to Aerosol Boxes for Endotracheal Intubation of COVID-19 Patients. Anesthesiology. 2020;133:683–4. doi: 10.1097/ALN.0000000000003422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization . Geneva: WHO; 2020. May 16, Cleaning and disinfection of environmental surfaces in the context of COVID-19 [Internet] [cited 2020 Jul 13]. Available from https://www.who.int/publications/i/item/cleaning-and-disinfection-of-environmental-surfaces-inthe-context-of-covid-19. [Google Scholar]
- 20.Zucco L, Levy N, Ketchandji D, Aziz M, Ramachandran SK. Recommendations for Airway Management in a Patient with Suspected Coronavirus (2019-nCoV) Infection. Anesth Patient Saf Found. 2020 [Google Scholar]
- 21.Dexter F, Parra MC, Brown JR, Loftus RW. Perioperative COVID-19 Defense: An Evidence-Based Approach for Optimization of Infection Control and Operating Room Management. Anesth Analg. 2020;131:37–42. doi: 10.1213/ANE.0000000000004829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Birnbach DJ, Rosen LF, Fitzpatrick M, Carling P, Munoz-Price LS. The Use of a Novel Technology to Study Dynamics of Pathogen Transmission in the Operating Room. Anesth Analg. 2015;120:844–7. doi: 10.1213/ANE.0000000000000226. [DOI] [PubMed] [Google Scholar]
- 23.Birnbach DJ, Rosen LF, Fitzpatrick M, Carling P, Arheart KL, Munoz-Price LS. Double Gloves: A Randomized Trial to Evaluate a Simple Strategy to Reduce Contamination in the Operating Room. Anesth Analg. 2015;120:848–52. doi: 10.1213/ANE.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 24.Hunter S, Katz D, Goldberg A, Lin HM, Pasricha R, Benesh G, et al. Use of an anaesthesia workstation barrier device to decrease contamination in a simulated operating room. Br J Anaesth. 2017;118:870–5. doi: 10.1093/bja/aex097. [DOI] [PubMed] [Google Scholar]
- 25.Loftus RW, Brown JR, Koff MD, Reddy S, Heard SO, Patel HM, et al. Multiple reservoirs contribute to intraoperative bacterial transmission. Anesth Analg. 2012;114:1236–48. doi: 10.1213/ANE.0b013e31824970a2. [DOI] [PubMed] [Google Scholar]
- 26.Bommarito M, Morse DJ. A Multi-site Field Study Evaluating the Effectiveness of Terminal Cleaning in Patient and Operating Rooms. Am J Infect Control. 2013;41:S43–4. [Google Scholar]
- 27.Pedersen A, Getty Ritter E, Beaton M, Gibbons D. Remote Video Auditing in the Surgical Setting. AORN J. 2017;105:159–69. doi: 10.1016/j.aorn.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 28.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Loftus RW, Muffly MK, Brown JR, Beach ML, Koff MD, Corwin HL, et al. Hand contamination of anesthesia providers is an important risk factor for intraoperative bacterial transmission. Anesth Analg. 2011;112:98–105. doi: 10.1213/ANE.0b013e3181e7ce18. [DOI] [PubMed] [Google Scholar]
- 30.Orser BA. Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth Analg. 2020;130:1109–10. doi: 10.1213/ANE.0000000000004803. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Standardized simulation sequence
Total contamination score for control and experimental groups.