Abstract
The coronavirus disease 2019 (COVID-19) pandemic is currently recognized as a global health crisis. This viral infection is frequently associated with hypercoagulability, with a high incidence of thromboembolic complications that can be fatal. In many situations, the standard coagulation tests (SCT) fail to detect this state of hypercoagulability in patients with COVID-19 since clotting times are either not or only mildly affected. The role of viscoelastic tests such as rotational thromboelastometry (ROTEM®) during this pandemic is explored in this review. COVID-19-associated coagulopathy, as measured using the rotational thromboelastometry parameters, can vary from hypercoagulability due to increased fibrin polymerization and decreased fibrinolysis to bleeding from hypocoagulability. The use of a multimodal diagnostic and monitoring approach, including both rotational thromboelastometry and SCT, such as plasma fibrinogen and D-dimer concentrations, is recommended. Rotational thromboelastometry provides comprehensive information about the full coagulation status of each patient and detects individual variations. Since COVID-19-associated coagulopathy is a very dynamic process, the phenotype can change during the course of infection and in response to anticoagulation therapy. Data from published literature provide evidence that the combination of rotational thromboelastometry and SCT analysis is helpful in detecting hemostasis issues, guiding anticoagulant therapy, and improving outcomes in COVID-19 patients. However, more research is needed to develop evidence-based guidelines and protocols.
Keywords: Anticoagulants, Blood coagulation disorders, COVID-19, Fibrinolysis, SARSCoV-2, Thrombelastography, Thrombophilia, Thrombosis
Introduction
The first case of coronavirus disease 2019 (COVID-19) was reported in Wuhan City, China, in December 2019, before it became a global pandemic. The disease is highly contagious, and the clinical picture varies from an asymptomatic course to acute respiratory failure [1]. COVID-19-associated hypercoagulability and subsequent pulmonary thrombosis are among the leading causes of death from COVID-19. This hypercoagulability can be resistant to standard doses of low molecular weight heparin (LMWH), indicated by low anti-Xa levels (< 0.4 IU/ml), in patients with sub-therapeutic or therapeutic anticoagulation. Furthermore, hypercoagulability in COVID-19 is characterized by high plasma fibrinogen concentrations and elevated D-dimer levels (> 2,500 μg/L). Published data suggest that both hypercoagulability and a significant increase in proinflammatory cytokines (cytokine storm) are the leading causes of multiple organ failure in critically ill COVID-19 patients (immunothrombosis) [2–5]. Moreover, hypercoagulability is initiated by activating proinflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) [6]. The plasma fibrinogen concentration and D-dimer levels subsequently increase. These values exhibit a strong correlation with disease severity and can predict mortality at hospital and intensive care unit (ICU) admission [7]. The presence of other coexisting diseases, such as cardiovascular or cerebral diseases, can also increase the risk for morbidity and mortality [8]. Standard coagulation tests (SCT) of patients with COVID-19 such as platelet count, prothrombin time (PT), activated partial thromboplastin time (aPTT), and international normalized ratio (INR) may show normal results despite the presence of hypercoagulability on rotational thromboelastometry and microvascular thrombosis [9–11].
In contrast, viscoelastic tests (VETs) can evaluate the mechanical properties of clot formation and lysis. The most frequently used VETs are thromboelastography (TEG®) and rotational thromboelastometry (ROTEM®). Published literature regarding this pandemic explored the ability of TEG® and ROTEM® to detect COVID-19-associated coagulopathy [12,13]. Increased thrombin generation and clot formation plays an important role in the progression of COVID-19 and can be used to predict the severity and risk of complications [14,15].
Aim and method of the narrative review
This narrative review aimed to identify and discuss the peer-reviewed literature regarding the role of rotational thromboelastometry for COVID-19 patients who experienced coagulopathy. This review provides important information to clinicians and healthcare authorities regarding the possible role of rotational thromboelastometry as a diagnostic and monitoring tool during the current COVID-19 pandemic.
This literature review was approved by the local research and ethics committee on October 18, 2020 (approval no. 2020-10-50) of the College of Medicine, King Faisal University, Al-Ahsa, Hofuf, Kingdom of Saudi Arabia. This review explores and identifies several published studies focusing on the role of rotational thromboelastometry in critically ill patients with COVID-19. Medline, Scopus, PubMed, and Google Scholar were searched for related literature published between January and December 2020. Current peer-reviewed and accepted online ahead of print publications were also included. PubMed was searched using the following keywords, which obtained 24 results: (COVID-19 [Title/Abstract] OR SARS-CoV-2 [Title/Abstract]) AND (ROTEM [Title/Abstract] OR thromboelastometry [Title/Abstract]).
Rotational thromboelastometry
Rotational thromboelastometry (ROTEM®, Tem Innovations, Germany) is a point-of-care device that is capable of evaluating the viscoelastic properties and kinetics of the whole coagulation process, including clot formation and lysis, in vitro. Rotational thromboelastometry can assess both extrinsic and intrinsic coagulation pathways depending on the reagents used [16]. The four principal tests used with ROTEM include EXTEM, INTEM, FIBTEM, and HEPTEM, which assess the extrinsic coagulation pathway, intrinsic coagulation pathway, fibrin contribution to clot firmness, and heparin-like effects, respectively. Rotational thromboelastometry measures the following parameters: CT, CFT, A5, A10, and MCF. CT is the time needed to initiate clot development (until clot firmness = 2 mm). CFT characterizes clot kinetics based on the time needed to increase clot firmness from 2 to 20 mm. MCF is the maximum clot firmness measured in mm achieved during the thromboelastometric measurement. Finally, fibrinolysis is characterized by maximum lysis (ML in %), which is defined as the decrease in clot firmness, expressed in percentage, of MCF during run time. Lysis indexes at 30 (LI30), 45 (LI45), and 60 (LI60) min are defined as the residual clot firmness in percentage of MCF at 30 or 60 min after CT, respectively. To detect hypofibrinolysis/fibrinolysis shutdown, the run time should be at least 60 min in order to achieve LI60. The lysis onset time (LOT in seconds) is defined as the time from CT until the clot firmness amplitude decreases by 15% compared with MCF. LOT is not achieved during a 60-min run time in patients with hypofibrinolysis/fibrinolysis shutdown or prolonged in TPATEM/TPA-test with recombinant tissue plasminogen activator (r-tPA)-challenge in patients with COVID-19. TPATEM/TPA-test is a modified EXTEM test with the addition of r-tPA. Here, r-TPA-doses (Alteplase, Boehringer-Ingelheim, Germany) between 0.125 and 0.625 µg/ml were used for r-tPA-challenge by different investigators. Lysis time (LT in seconds), defined as the time from CT until the clot firmness decreases to 50% (in ClotPro®) or 10% (in ROTEM®) compared with MCF, can also be used to characterize fibrinolysis resistance. Fibrinolysis resistance is characterized by prolonged LOT, prolonged LT, and increased LI30 in the TPATEM/TPA-test. Fig. 1 illustrates the rotational thromboelastometry parameters and indices mentioned above [16].
Fig. 1.
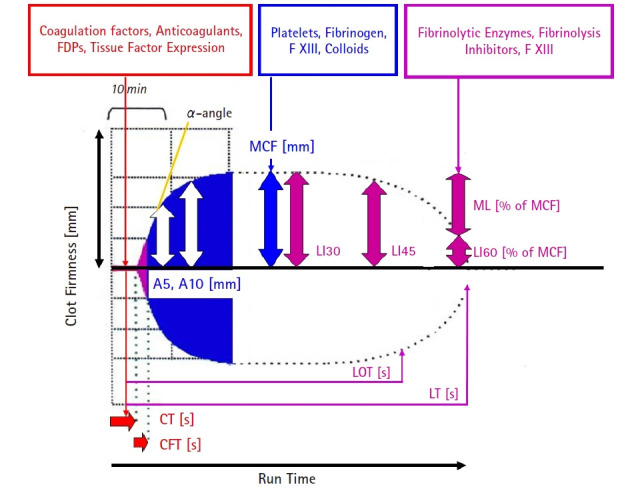
ROTEM® parameters and indices. A5: clot firmness amplitude 5 min after coagulation time (CT) in mm, A10: clot firmness amplitude 10 min after CT in mm, CFT: clot formation time in seconds (time from 2 to 20 mm clot firmness), CT: coagulation time in seconds (time from test start to 2 mm clot firmness), FDPs: fibrin(ogen) degrading products, F XIII: coagulation factor XIII, LI30: lysis index 30 min after CT in % (residual clot firmness in percentage of MCF), LI45: lysis index 45 min after CT in %, LI60: lysis index 60 min after CT in %, LOT: lysis onset time in seconds (time from CT to 15% fibrinolysis = 85% residual clot firmness compared to MCF), and LT: lysis time in seconds (time from CT to 90% fibrinolysis = 10% residual clot firmness compared to MCF). Courtesy of Klaus Görlinger, Munich, Germany.
Several studies prior to the COVID-19 pandemic demonstrated that an EXTEM or INTEM MCF of > 68 mm (A10 > 61.5 mm) is a strong indicator of hypercoagulability and predictor of thrombosis [17,18]. A FIBTEM MCF value of > 25 mm is associated with a five-fold increased risk of developing thrombosis in cirrhotic patients with hepatocellular carcinoma [19,20]. Hypercoagulability in COVID-19 patients was assessed by rotational thromboelastometry, which is used as a diagnostic tool [21,22]. Hypofibrinolysis/fibrinolysis shutdown in rotational thromboelastometry is diagnosed based on the following criterion: an EXTEM ML of < 3.5% following a 60-min run time, which corresponds to an EXTEM LI60 of > 96.5%. Accordingly, rotational thromboelastometry analysis should run for 65–70 min in COVID-19 patients in order to confirm or exclude hypofibrinolysis/fibrinolysis shutdown [22–24].
COVID-19-associated hypercoagulability in rotational thromboelastometry
Between April and August 2020, several independent research groups (Pavoni et al. [5], Spiezia et al. [25], Collett et al. [26], and Hoechter et al. [27]) reported and confirmed the presence of hypercoagulability after conducting a series of thromboelastometric analyses in COVID-19 patients, and it was associated with an increased risk of thrombosis. Kong et al. [21] described this hypercoagulability as an increase in EXTEM and FIBTEM MCF (Fig. 2). Moreover, Ibañez et al. [28] attributed this hypercoagulability to hypofibrinolysis/fibrinolysis shutdown. Chaudhary et al. [29] suggested that rotational thromboelastometry can monitor the hypercoagulability/hypofibrinolysis status and can be a predictor of thromboembolic complications. In October 2020, Almskog et al. [30] demonstrated that EXTEM and FIBTEM MCF, assessed at hospital admission, could help distinguish hospitalized COVID-19 patients who can be treated at a regular ward from those who will require treatment at specialized ICUs with the need for mechanical ventilation. They also suggested that this could be used in future triage protocols. Further studies conducted by Spiezia et al. [31], van Veenendaal et al. [32], and Blasi et al. [33] confirmed that these rotational thromboelastometry findings provide supportive evidence to indicate that hypercoagulability in EXTEM, INTEM, and FIBTEM were associated with a more severe COVID-19. Roh et al. [34] also suggested that the significant increase in fibrinogen plasma concentrations and FIBTEM MCF indicates the severity of COVID-19 and can be used for risk stratification for thrombosis, respiratory failure, and mortality. In fact, an ongoing multinational (11 countries), multicenter (16 hospitals) observational trial is aimed at assessing the value of rotational thromboelastometry and SCTs in predicting the need for hospital resources, patients’ course, and outcomes in 500 hospitalized patients with COVID-19 (ROHOCO study; DRKS00023934) [22].
Fig. 2.
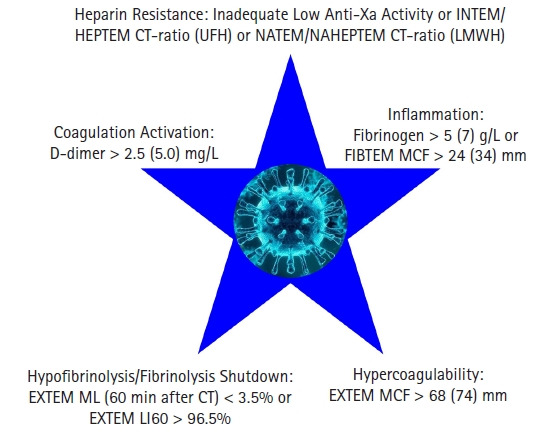
COVID-19-associated coagulopathy. Diagnostic value of D-dimer, fibrinogen, anti-Xa activity, and rotational thromboelastometry parameters. CT: coagulation time in seconds, EXTEM: ROTEM® test assessing the extrinsic coagulation pathway, FIBTEM: ROTEM® test assessing fibrin contribution to clot firmness, HEPTEM: ROTEM® test assessing the intrinsic coagulation pathway with elimination of heparin-like effects by heparinase, INTEM: ROTEM® test assessing the intrinsic coagulation pathway which is sensitive to heparin-like effects, LI60: lysis index 60 min after CT in % of MCF, LMWH: low molecular weight heparin, MCF: maximum clot firmness in mm, ML: maximum lysis in % of MCF, NAHEPTEM: native ROTEM® test with elimination of heparin-like effects by heparinase, NATEM: native ROTEM® test which is sensitive to LMWH, and UFH: unfractionated heparin. Courtesy of Klaus Görlinger, Munich, Germany.
COVID-19-associated hypofibrinolysis/fibrinolysis shutdown in rotational thromboelastometry
The failure of LMWH or unfractionated heparin (UFH) to reduce the incidence of thrombosis was reported by Creel-Bulos et al. [24] and was attributed to the presence of hypofibrinolysis/fibrinolysis shutdown, characterized by an EXTEM ML value of < 3.5%, which corresponds to an EXTEM LI60 value of > 96.5%. Here, either 8 of 9 (89%) patients with venous thrombosis met the diagnostic criteria for hypofibrinolysis/fibrinolysis shutdown, or 8 out of 11 (73%) patients with hypofibrinolysis/fibrinolysis shutdown developed thrombosis. Meanwhile, only 1 out of 14 (7%) patients without hypofibrinolysis/fibrinolysis shutdown developed thrombosis. The cut-off value for the hypofibrinolysis/fibrinolysis shutdown reported by Creel-Bulos et al. [24] is in line with those for hypofibrinolysis/fibrinolysis shutdown published by Adamzik et al. [35] and Schmitt et al. [36] for bacterial sepsis and Gomez-Builes et al. [23] and Stettler et al. [37] for trauma patients.
COVID-19-associated fibrinolysis resistance in rotational thromboelastometry
Weiss et al. [38] and Nougier et al. [39] demonstrated that clots from some critically ill COVID-19 patients were resistant to r-tPA challenge in rotational thromboelastometry (TPATEM = EXTEM with 0.125–0.625 µg/ml r-tPA (Alteplase, Boehringer-Ingelheim, Germany) despite the high D-dimer plasma concentrations. Fibrinolysis resistance was defined as a delay in the lysis onset time (LOT in seconds) or an increased LI30 in % of MCF after an in vitro r-tPA challenge (Fig. 3). Here, healthy controls showed a LI30 of 1.8 ± 3.2%; non-ICU COVID-19 patients, 18 ± 35%; ICU COVID-19 patients, 63 ± 39%; and ICU COVID-19 patients with thrombosis, 82 ± 26% (P = 0.003). A TPATEM assay with 0.125 µg/ml r-tPA has been validated on ROTEM® delta [40]; however, a CE-marked TPA-test can only be performed using the ClotPro® device, a modification of ROTEM® [41]. In COVID-19 patients with thrombosis, LT was significantly prolonged in the TPATEM/TPA-test. Whether detection of fibrinolysis resistance provides additional clinically relevant information compared with the detection of hypofibrinolysis/fibrinolysis shutdown remains unknown and requires further investigation.
Fig. 3.
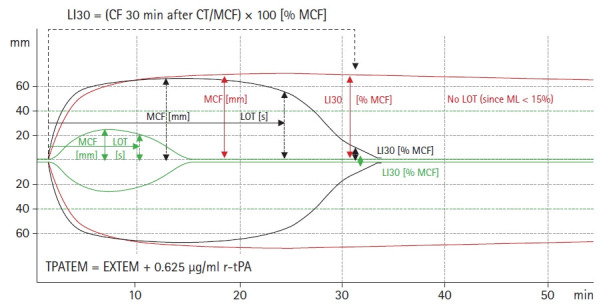
TPATEM/TPA-test findings in COVID-19 patients. Representative TPATEM curves from a healthy donor (green curve), a COVID-19 patient without thrombosis (black curve), and a COVID-19 patient with thrombosis (red curve). In COVID-19 patients, LOT and LT are prolonged, and MCF and LI30 are increased compared with those in healthy controls after r-tPA challenge (TPATEM = EXTEM + 0.625 µg/ml r-tPA). CF: clot firmness in mm, CT: coagulation time in seconds, EXTEM: ROTEM® test assessing the extrinsic coagulation pathway, LI30: lysis index 30 min after CT in % of MCF, LOT: lysis onset time in seconds, MCF: maximum clot firmness in mm, ML: maximum lysis in % of MCF, and r-tPA: recombinant tissue plasminogen activator. Courtesy of Klaus Görlinger, Munich, Germany.
High D-dimer levels combined with hypofibrinolysis/fibrinolysis shutdown as a strong predictor of thrombosis in COVID-19 patients
The combination of high D-dimer levels and hypofibrinolysis/fibrinolysis shutdown in VET showed the best predictive value for venous thromboembolism (VTE), thrombotic stroke, and renal failure with the need for dialysis in COVID-19 patients [42,43]. Here, Wright et al. [42] demonstrated that the receiver operating characteristics area under the curve (ROC AUC) values for predicting VTE were 0.742 (95% CI, 0.581, 0.903; P = 0.022) for TEG® lysis 30 (TEG® LY30 in % = decrease of clot firmness amplitude in percentage of maximum amplitude [MA] at 30 min after MA) and 0.582 (95% CI, 0.372, 0.792; P = 0.440) for D-dimer. The ROC AUC values for predicting renal failure with the need for dialysis were 0.799 (95% CI, 0.610, 0.949; P = 0.005) for D-dimer and 0.606 (95% CI, 0.414, 0.797; P = 0.292) for TEG® LY30. Combined analysis revealed the VTE, thrombotic stroke, and renal failure incidence rates of 5%, 7%, and 14%, respectively, with the need for dialysis in COVID-19 patients with a D-dimer concentration of ≤ 2,600 FEU and TEG® lysis 30 of > 0% (TEG® LY30 is defined as the reduction in clot firmness amplitude in percentage of [MA] 30 min after MA). If the D-dimer concentration was higher than 2,600 FEU or the TEG® LY30 was 0%, the incidence rates of VTE, thrombotic stroke, and renal failure with the need for dialysis increased to 30%, 10%, and 30%, respectively. If the D-dimer concentrations were higher than 2,600 FEU and the LY30 was 0%, the incidence rates of VTE, thrombotic stroke, and renal failure with the need for dialysis increased to 50% (P = 0.008), 30% (P = 0.274), and 80% (P = 0.004), respectively. These results are in line with the data published recently by Kruse et al. [43]. Here, EXTEM ML was inversely (ROC AUC, 0.8 [95% CI, 0.7, 0.9]; P = 0.002) and D-dimer concentration was directly (ROC AUC, 0.78 [95% CI, 0.6, 0.9]; P < 0.001) associated with an increased risk of VTE complications. The combination of EXTEM ML values and D-dimer concentrations showed high sensitivity and specificity for VTE risk prediction (D-dimer [mg/L] – EXTEM ML [%] cut-off, 3.7; ROC AUC, 0.92 [95% CI, 0.8, 1.0]; P < 0.001; sensitivity, 94%, specificity > 90%). Accordingly, the combination of hypofibrinolysis/fibrinolysis shutdown and increased D-dimer levels is actually the best predictor for VTE, thrombotic stroke, and renal failure with the need for dialysis in critically ill COVID-19 patients. Primarily, this combination resulted in some confusion since increased D-dimer levels have been misinterpreted as a biomarker of increased fibrinolysis [28]. However, both Almskog et al. [30] and Madathil et al. [44] reported that only 0.02%–0.2% of the fibrinogen mass was cleaved to D-dimers in COVID-19. Accordingly, increased D-dimer concentration in COVID-19 patients reflect an increased fibrin deposition but not an increased breakdown of fibrin (fibrinolysis). Finally, the combination of increased fibrin deposition in the microcirculation combined with hypofibrinolysis results in multiple organ failure (lungs, kidney, and brain).
Potential implications of hypofibrinolysis/fibrinolysis shutdown for the therapy of COVID-19-associated coagulopathy
These data suggest that COVID-19 patients with respiratory failure (PaO2/FiO2 < 150 mmHg for more than 4 h despite optimum mechanical ventilation and prone positioning) who experienced hypercoagulability and hypofibrinolysis/fibrinolysis shutdown might benefit from sub-therapeutic/therapeutic anticoagulation and/or additional thrombolytic therapy with r-tPA (Alteplase, Boehringer-Ingelheim, Germany) [34,45–49]. A recent case series showed that r-tPA therapy can improve oxygenation and may improve survival in this specific patient population [50–53].
The required r-tPA-dose can vary from patient to patient. Therefore, monitoring the effect of thrombolytic therapy in COVID-19 patients by rotational thromboelastometry is recommended [50,53]. Here, rotational thromboelastometry is not only important in selecting the COVID-19 patient population who might benefit from thrombolytic therapy, but it can also detect the patient population with a higher risk of developing bleeding complications under thrombolytic therapy. Symptomatic intracerebral hemorrhage usually occurs within 24–36 h after thrombolytic infusion and remains one of the most feared complications of thrombolytic therapy. Campello et al. [54] demonstrated that a baseline FIBTEM MCF of < 13.5 mm is an important biomarker that can be easily obtained to predict which patients have a higher risk of developing hemorrhagic events after r-tPA therapy (sensitivity: 94% and specificity: 80%). Furthermore, bleeders showed higher EXTEM ML after r-tPA infusion and borderline hyperfibrinolysis (median [Q1, Q3], 14% [10%, 18%] versus 6% [5%, 8.5%] P = 0.007). Accordingly, thrombolytic therapy might be harmful in patients with advanced stages of COVID-19, where the hemostatic status changed from hyper- to hypocoagulability and from hypo- to hyperfibrinolysis in case of disseminated intravascular coagulation (DIC) [55]. An ongoing phase IIa randomized controlled trial is aimed at evaluating the efficacy and safety of different doses of Alteplase (50–100 mg IV) for respiratory failure in patients with COVID-19 (STARS trial) [56]. In this trial, heparin infusion was administered following thrombolytic therapy for therapeutic anticoagulation.
Inhalation therapy with thrombolytic agents in severe COVID-19 patients
Furthermore, nebulizer r-tPA may provide a targeted approach in COVID-19 patients to degrade fibrin and improve oxygenation with limited bleeding risk in critically ill patients [57]. The administration of thrombolytic drugs by inhalation might improve alveolar ventilation by resolving fibrin-containing exudates in the pulmonary alveolar space and dissolving fibrin thrombi at the microcirculatory level near the alveoli. Inhalation therapy with tPA is reported to be effective for various cases of acute respiratory distress syndrome (ARDS) or plastic bronchitis. Actually, a phase II clinical trial of r-tPA inhalation is currently underway (PLATyPuS; Alteplase, NCT02315898). Other studies reported promising results of plasminogen inhalation in COVID-19 patients [58]. If r-tPA is not available, nebulization of streptokinase can be used as an alternative method. Abdelaal Ahmed Mahmoud et al. [59] performed a randomized controlled trial comparing nebulized streptokinase with nebulized heparin and the standard of care in patients with severe ARDS; (PaO2/FiO2 < 100 mmHg) nonresponsive to recruitment maneuvers and prone positioning. Streptokinase (250,000 IU/4 h by nebulizer, with a total daily dose of 1,500,000 IU) or heparin (dose of 10,000 IU/4 h by nebulizer, with a total daily dose of 60,000 IU UFH) prepared in 3 ml volume of distilled water and nebulized for a period of 15 min every 4 h was administered. Nebulized streptokinase resulted in an improvement in oxygenation (increased PaO2/FiO2), decreased PaCO2 (P < 0.001), improved lung compliance, reduced plateau pressure, and decreased ICU mortality compared with nebulized heparin and standard of care therapy [59].
COVID-19, heparin resistance, and anticoagulation monitoring with rotational thromboelastometry
Heparin resistance can be defined as a decrease in the heparin dose-response curve. It can also be defined as the need for more than 35,000 IU UFH per 24 h to prolong the aPTT or activated clotting time to its therapeutic range [60,61]. An antithrombin activity of less than 60%, age above 65 years, increased factor VIII and fibrinogen levels, and platelet level of > 300,000/μl were the predictors of heparin resistance [62]. Although antithrombin activity rarely drops below 60% in COVID-19 patients, increased age, factor VIII and fibrinogen levels, and high platelet counts commonly occur in those with severe COVID-19 [25,27,63,64].
LMWH (e.g., enoxaparin, 20–30 mg subcutaneously (SC) once a day) is used as a thromboprophylactic treatment in COVID-19 patients with low thrombotic risk and fibrinogen plasma concentrations of < 500 mg/dl provided that an anti-Xa activity target of 0.1–0.4. IU/ml is achieved 2–4 h after SC injection. For sub-therapeutic or therapeutic anticoagulation in COVID-19 patients with moderate to high risk of VTE, 0.5 to 1 mg/kg enoxaparin SC twice per day can be used if the anti-Xa activity targets of 0.4–0.6 IU/ml and 0.6–1.0 IU/ml are achieved 2–4 hours after SC injection. In critically ill COVID-19 patients who require vasopressor therapy, SC injection of LMWH might be inappropriate as the vasopressor can lead to peripheral vasoconstriction and reduced resorption of the drug. Here, IV infusion of UFH or LMWH can be used as an alternative treatment. However, the effect might be limited by heparin resistance; the anti-Xa activity targets for sub-therapeutic (200 IU/kg/24 h) and therapeutic anticoagulation (400 IU/kg/24 h) with UFH are 0.15–0.30 IU/ml and 0.3–0.7 IU/ml, respectively.
To monitor the effect of heparin anticoagulation or to diagnose heparin resistance with rotational thromboelastometry, it is important to consider that INTEM is not highly sensitive to the effect of LMWH. The INTEM/HEPTEM CT-ratio correlates well with anti-Xa activity for UFH (r = 0.72 compared to 0.36 for aPTT) [65]. The native rotational thromboelastometry test (NATEM) is more sensitive to LMWH, and the NATEM/NAHEPTEM CT-ratio (NAHEPTEM = native test with heparinase) correlates well with the anti-Xa activity calibrated for LMWH [unpublished data].
The direct factor Xa inhibitor apixaban can be used thromboprophylaxis or alternative anticoagulation in patients with COVID-19 who developed heparin resistance and in whom oral administration is preferred [66–69]. Notably, the plasma concentrations of direct oral anticoagulant (DOAC) can increase substantially if DOACs are used in combination with antiviral drugs in COVID-19 patients [70]. Therefore, these combinations should be avoided or DOAC concentrations should be monitored. To monitor the effect of apixaban with rotational thromboelastometry, modified assays with lower tissue factor concentrations are needed [71,72].
In critically ill patients with high VTE risk and fibrinogen plasma concentrations of > 500 mg/dl, the off-label use of argatroban can be implemented as an alternative anticoagulation particularly in patients with heparin resistance [60]. Argatroban is a direct thrombin inhibitor approved for thromboprophylaxis or treatment of thrombosis in patients with heparin-induced thrombocytopenia. The argatroban plasma concentrations needed for therapeutic anticoagulation range from 0.2 IU/ml to 0.5 IU/ml of anti-IIa activity. Here, EXTEM CT correlated better with argatroban plasma concentrations than aPTT (r = 0.71; P < 0.001 and r = 0.214; P = 0.117, respectively) [73,74]. Furthermore, the importance of VET in patients treated with direct thrombin inhibitors was highlighted by Ranucci et al. [75] and Maier et al. [76]. They pointed out that fibrinogen plasma concentration assessed using the Clauss method is not reliable if direct thrombin inhibitors have been used and results in falsely low values. Therefore, they recommend using FIBTEM and TEG® functional fibrinogen measurements to assess the fibrinogen plasma concentration in these patients and to determine the appropriate argatroban or bivalirudin dosage [75,76].
Bleeding in patients with COVID-19
In hospitalized COVID-19 patients receiving standard-dose thromboprophylaxis, Al-Samkari et al. [77] reported an overall and major bleeding rate of 4.8% (95% CI, 2.9, 7.3) and 2.3% (95% CI, 1.0, 4.2), respectively. Similar results were reported by Jiménez et al. [78]. In this systematic review, the pooled incidence of VTE was 17.0% (95% CI, 13.4, 20.9), 12.1% (95% CI, 8.4, 16.4) for deep vein thrombosis, 7.1% (95% CI, 5.3, 9.1) for pulmonary embolism, 7.8% (95% CI, 2.6, 15.3) for bleeding, and 3.9% (95% CI, 1.2, 7.9) for major bleeding. The highest estimated pooled incidence of bleeding was reported in patients receiving intermediate-dose or full-dose anticoagulation (21.4%).
Patients with COVID-19 have an increased risk of developing thrombosis, and mortality can be reduced in hospitalized patients by providing thromboprophylaxis [48,68,79,80]. On the contrary, patients receiving therapeutic anticoagulation have an increased incidence of major bleeding (11% versus 4%; P = 0.04) and significantly higher mortality (41.6% versus 15.3%; P < 0.001) compared with those receiving pharmacological thromboprophylaxis [81]. After conducting a multivariate logistic regression analysis, therapeutic anticoagulation was still associated with increased mortality, with an odds ratio of 6.16 (95% CI, 2.96, 12.83; P < 0.001). Major bleeding and central nervous system bleeding were associated with increased mortality (40% versus 21.5%; P = 0.054 and 100% versus 21.9%; P = 0.001, respectively), while gastrointestinal bleeding was not associated with increased mortality (16.7% versus 22.7%; P = 1.000). Dogra et al. [82] reported 33 COVID-19-positive patients with intracerebral hemorrhage (ICH). Almost all patients with ICH received either therapeutic anticoagulation (66.7%) or a prophylactic dose (9.1%) prior to ICH discovery. Accordingly, the risk of ICH should be considered when developing an anticoagulation regimen for patients with COVID-19. Usman et al. [83] reported a case series of COVID-19 patients treated with veno-venous extracorporeal membrane oxygenation (ECMO). Four of ten patients had hemorrhagic stroke, three of whom died. Schmidt et al. [84] confirmed a major bleeding incidence of 42%, a hemorrhagic stroke incidence of 5%, and a mortality rate of 36% in COVID-19 patients treated with ECMO. Accordingly, close monitoring of all hematologic parameters, including VET and personalized antithrombotic therapy, is recommended in patients with severe COVID-19, particularly during ECMO support [29]. The degree of anticoagulation can be assessed based on the anti-Xa activity or INTEM/HEPTEM CT-ratio for UFH, anti-Xa activity or NATEM/NAHEPTEM CT-ratio for LMWH, and anti-IIa activity, EXTEM CT, or ECATEM/ECA-test CT for IV direct thrombin inhibitors such as argatroban and bivalirudin [65,73,74,85–90]. Furthermore, the hemostatic phenotype of COVID-19 patients may change from hyper- to hypocoagulability and from hypo- to hyperfibrinolysis during advanced stages of COVID-19 in case of DIC [21,55]. The combination of rotational thromboelastometry and SCT enables the monitoring of these dynamic changes in COVID-19-associated coagulopathy and its corresponding therapy.
Conclusion
A multimodal diagnostic approach that includes SCT, such as fibrinogen plasma concentration and D-dimers, as well as rotational thromboelastometry, is required for the detection, monitoring, and management of COVID-19-associated coagulopathy. Fibrinogen plasma concentrations, D-dimer levels, and FIBTEM clot firmness play an important role in the risk stratification, prediction of the level of care needed during hospitalization, and determination of outcomes in hospitalized COVID-19 patients. SCTs such as aPTT and PT/INR may fail to detect hypercoagulability. In contrast, the combination of increased D-dimer levels and the hypofibrinolysis/fibrinolysis shutdown detected by rotational thromboelastometry is actually the best predictor for thromboembolic complications in COVID-19 patients. Rotational thromboelastometry should be utilized to guide personalized management and monitor individual responses to treatment. Therefore, there is an urgent need to develop rotational thromboelastometry-guided protocols and algorithms for the management of COVID-19-associated coagulopathy.
Footnotes
Conflicts of Interest
Klaus Gorlinger is working as the Medical Director of Tem Innovations GmbH, Munich, Germany, since July 2012. All other authors declared no conflict of interest relevant to this manuscript.
Author Contributions
Klaus Görlinger (Conceptualization; Methodology; Supervision; Visualization; Writing – review & editing)
Hawra Almutawah (Methodology; Writing – original draft)
Fatimah Almutawaa (Methodology; Writing – original draft)
Maryam Alwabari (Methodology; Writing – original draft)
Zahra Alsultan (Methodology; Writing – original draft)
Jumanah Almajed (Methodology; Writing – original draft)
Mahmoud Alwabari (Methodology; Writing – original draft)
Maryam Alsultan, Doctor Internship (Methodology; Writing – original draft)
Duri Shahwar (Conceptualization; Methodology; Supervision; Writing – review & editing)
Khaled Ahmed Yassen (Conceptualization; Methodology; Supervision; Writing – review & editing)
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–3. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mondal S, Quintili AL, Karamchandani K, Bose S. Thromboembolic disease in COVID-19 patients: a brief narrative review. J Intensive Care. 2020;8:70. doi: 10.1186/s40560-020-00483-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klok FA, Kruip MJ, van der Meer NJ, Arbous MS, Gommers DA, Kant KM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singhania N, Bansal S, Nimmatoori DP, Ejaz AA, McCullough PA, Singhania G. Current overview on hypercoagulability in COVID-19. Am J Cardiovasc Drugs. 2020;20:393–403. doi: 10.1007/s40256-020-00431-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pavoni V, Gianesello L, Pazzi M, Stera C, Meconi T, Frigieri FC. Evaluation of coagulation function by rotation thromboelastometry in critically ill patients with severe COVID-19 pneumonia. J Thromb Thrombolysis. 2020;50:281–6. doi: 10.1007/s11239-020-02130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421–4. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alarbash M, Alotaibi A, Alzaid Z, Alamoudi A, Alomair M, Alabdulqadir A, et al. Severe COVID-19 infection and hypercoagulation. A narrative review. EC Anaesth. 2020;6:03–5. [Google Scholar]
- 8.Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18:1738–42. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yao Y, Cao J, Wang Q, Shi Q, Liu K, Luo Z, et al. D-dimer as a biomarker for disease severity and mortality in COVID-19 patients: a case control study. J Intensive Care. 2020;8:49. doi: 10.1186/s40560-020-00466-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X, Du B, Li J, Wang S, Wang X, Guo M, Yang B, Si D, Bai O. D-dimer surge and coagulation disorders in COVID-19 related pneumonia patients with cardiac injury: a case series. Medicine (Baltimore) 2020;99:e21513. doi: 10.1097/MD.0000000000021513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mortus JR, Manek SE, Brubaker LS, Loor M, Cruz MA, Trautner BW, et al. Thromboelastographic results and hypercoagulability syndrome in patients with coronavirus disease 2019 who are critically ill. JAMA Netw Open. 2020;3:e2011192. doi: 10.1001/jamanetworkopen.2020.11192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raval JS, Burnett AE, Rollins-Raval MA, Griggs JR, Rosenbaum L, Nielsen ND, et al. Viscoelastic testing in COVID-19: a possible screening tool for severe disease? Transfusion. 2020;60:1131–2. doi: 10.1111/trf.15847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iwasaki Y, Shiga T, Konno D, Saito K, Aoyagi T, Oshima K, et al. Screening of COVID-19-associated hypercoagulopathy using rotational thromboelastometry. J Clin Anesth. 2020;67:109976. doi: 10.1016/j.jclinane.2020.109976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Boscolo A, Spiezia L, Correale C, Sella N, Pesenti E, Beghetto L, et al. Different hypercoagulable profiles in patients with COVID-19 admitted to the internal medicine ward and the intensive care unit. Thromb Haemost. 2020;120:1474–7. doi: 10.1055/s-0040-1714350. [DOI] [PubMed] [Google Scholar]
- 16.Görlinger K, Pérez-Ferrer A, Dirkmann D, Saner F, Maegele M, Calatayud ÁA, et al. The role of evidence-based algorithms for rotational thromboelastometry-guided bleeding management. Korean J Anesthesiol. 2019;72:297–322. doi: 10.4097/kja.19169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dimitrova-Karamfilova A, Patokova Y, Solarova T, Petrova I, Natchev G. Rotation thromboelastography for assessment of hypercoagulation and thrombosis in patients with cardiovascular diseases. J Life Sci. 2012;6:28–35. [Google Scholar]
- 18.Hincker A, Feit J, Sladen RN, Wagener G. Rotational thromboelastometry predicts thromboembolic complications after major non-cardiac surgery. Crit Care. 2014;18:549. doi: 10.1186/s13054-014-0549-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zanetto A, Senzolo M, Vitale A, Cillo U, Radu C, Sartorello F, et al. Thromboelastometry hypercoagulable profiles and portal vein thrombosis in cirrhotic patients with hepatocellular carcinoma. Dig Liver Dis. 2017;49:440–5. doi: 10.1016/j.dld.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 20.Kamel Y, Hassanin A, Ahmed AR, Gad E, Afifi M, Khalil M, et al. Perioperative thromboelastometry for adult living donor liver transplant recipients with a tendency to hypercoagulability: a prospective observational cohort study. Transfus Med Hemother. 2018;45:404–12. doi: 10.1159/000489605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kong R, Hutchinson N, Görlinger K. Hyper- and hypocoagulability in COVID-19 as assessed by thromboelastometry. Two case reports. doi: 10.4097/kja.20327. Korean J Anesthesiol 2020. Advance Access published on Aug 10, 2020. doi: 10.4097/kja.20327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Görlinger K, Dirkmann D, Gandhi A, Simioni P. COVID-19-associated coagulopathy and inflammatory response: what do we know already and what are the knowledge gaps? Anesth Analg. 2020;131:1324–33. doi: 10.1213/ANE.0000000000005147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gomez-Builes JC, Acuna SA, Nascimento B, Madotto F, Rizoli SB. Harmful or physiologic: diagnosing fibrinolysis shutdown in a trauma cohort with rotational thromboelastometry. Anesth Analg. 2018;127:840–9. doi: 10.1213/ANE.0000000000003341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Creel-Bulos C, Auld SC, Caridi-Scheible M, Barker NA, Friend S, Gaddh M, et al. Fibrinolysis shutdown and thrombosis in a COVID-19 ICU. Shock. 2021;55:316–20. doi: 10.1097/SHK.0000000000001635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spiezia L, Boscolo A, Poletto F, Cerruti L, Tiberio I, Campello E, et al. COVID-19-Related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020;120:998–1000. doi: 10.1055/s-0040-1710018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Collett LW, Gluck S, Strickland RM, Reddi BJ. Evaluation of coagulation status using viscoelastic testing in intensive care patients with coronavirus disease 2019 (COVID-19): an observational point prevalence cohort study. doi: 10.1016/j.aucc.2020.07.003. Aust Crit Care 2020. Advance Access published on Jul 21, 2020. doi: 10.1016/j.aucc.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoechter DJ, Becker-Pennrich A, Langrehr J, Bruegel M, Zwissler B, Schaefer S, et al. Higher procoagulatory potential but lower DIC score in COVID-19 ARDS patients compared to non-COVID-19 ARDS patients. Thromb Res. 2020;196:186–92. doi: 10.1016/j.thromres.2020.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ibañez C, Perdomo J, Calvo A, Ferrando C, Reverter JC, Tassies D, et al. High D dimers and low global fibrinolysis coexist in COVID19 patients: what is going on in there? J Thromb Thrombolysis. 2021;51:308–12. doi: 10.1007/s11239-020-02226-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chaudhary R, Kreutz RP, Bliden KP, Tantry US, Gurbel PA. Personalizing antithrombotic therapy in COVID-19: role of thromboelastography and thromboelastometry. Thromb Haemost. 2020;120:1594–6. doi: 10.1055/s-0040-1714217. [DOI] [PubMed] [Google Scholar]
- 30.Almskog LM, Wikman A, Svensson J, Wanecek M, Bottai M, van der Linden J, et al. Rotational thromboelastometry results are associated with care level in COVID-19. J Thromb Thrombolysis. 2021;51:437–45. doi: 10.1007/s11239-020-02312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spiezia L, Campello E, Cola M, Poletto F, Cerruti L, Poretto A, et al. More severe hypercoagulable state in acute COVID-19 pneumonia as compared with other pneumonia. Mayo Clin Proc Innov Qual Outcomes. 2020;4:696–702. doi: 10.1016/j.mayocpiqo.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Veenendaal N, Scheeren TW, Meijer K, van der Voort PH. Rotational thromboelastometry to assess hypercoagulability in COVID-19 patients. Thromb Res. 2020;196:379–81. doi: 10.1016/j.thromres.2020.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blasi A, von Meijenfeldt FA, Adelmeijer J, Calvo A, Ibañez C, Perdomo J, et al. In vitro hypercoagulability and ongoing in vivo activation of coagulation and fibrinolysis in COVID-19 patients on anticoagulation. J Thromb Haemost. 2020;18:2646–53. doi: 10.1111/jth.15043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roh DJ, Eiseman K, Kirsch H, Yoh N, Boehme A, Agarwal S, et al. Hypercoagulable viscoelastic blood clot characteristics in critically ill coronavirus disease 2019 patients and associations with thrombotic complications. J Trauma Acute Care Surg. 2021;90:e7–12. doi: 10.1097/TA.0000000000002963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adamzik M, Eggmann M, Frey UH, Görlinger K, Bröcker-Preuss M, Marggraf G, et al. Comparison of thromboelastometry with procalcitonin, interleukin 6, and C-reactive protein as diagnostic tests for severe sepsis in critically ill adults. Crit Care. 14:R178. doi: 10.1186/cc9284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schmitt FC, Manolov V, Morgenstern J, Fleming T, Heitmeier S, Uhle F, et al. Acute fibrinolysis shutdown occurs early in septic shock and is associated with increased morbidity and mortality: results of an observational pilot study. Ann Intensive Care. 2019;9:19. doi: 10.1186/s13613-019-0499-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stettler GR, Moore EE, Moore HB, Nunns GR, Silliman CC, Banerjee A, et al. Redefining postinjury fibrinolysis phenotypes using two viscoelastic assays. J Trauma Acute Care Surg. 2019;86:679–85. doi: 10.1097/TA.0000000000002165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weiss E, Roux O, Moyer JD, Paugam-Burtz C, Boudaoud L, Ajzenberg N, et al. Fibrinolysis resistance: a potential mechanism underlying COVID-19 coagulopathy. Thromb Haemost. 2020;120:1343–5. doi: 10.1055/s-0040-1713637. [DOI] [PubMed] [Google Scholar]
- 39.Nougier C, Benoit R, Simon M, Desmurs-Clavel H, Marcotte G, Argaud L, et al. Hypofibrinolytic state and high thrombin generation may play a major role in SARS-COV2 associated thrombosis. J Thromb Haemost. 2020;18:2215–9. doi: 10.1111/jth.15016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuiper GJ, Kleinegris MC, van Oerle R, Spronk HM, Lancé MD, Ten Cate H, et al. Validation of a modified thromboelastometry approach to detect changes in fibrinolytic activity. Thromb J. 2016;14:1. doi: 10.1186/s12959-016-0076-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bachler M, Bösch J, Stürzel DP, Hell T, Giebl A, Ströhle M, et al. Impaired fibrinolysis in critically ill COVID-19 patients. Br J Anaesth. 2021;126:590–8. doi: 10.1016/j.bja.2020.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wright FL, Vogler TO, Moore EE, Moore HB, Wohlauer MV, Urban S, et al. Fibrinolysis shutdown correlation with thromboembolic events in severe COVID-19 infection. J Am Coll Surg. 2020;231:193-203.e1. doi: 10.1016/j.jamcollsurg.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kruse JM, Magomedov A, Kurreck A, Münch FH, Koerner R, Kamhieh-Milz J, et al. Thromboembolic complications in critically ill COVID-19 patients are associated with impaired fibrinolysis. Crit Care. 2020;24:676. doi: 10.1186/s13054-020-03401-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Madathil RJ, Tabatabai A, Rabin J, Menne AR, Henderson R, Mazzeffi M, et al. Thromboelastometry and D-dimer elevation in coronavirus-2019. J Cardiothorac Vasc Anesth. 2020;34:3495–6. doi: 10.1053/j.jvca.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seheult JN, Seshadri A, Neal MD. Fibrinolysis shutdown and thrombosis in severe COVID-19. J Am Coll Surg. 2020;231:203–4. doi: 10.1016/j.jamcollsurg.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsantes AE, Frantzeskaki F, Tsantes AG, Rapti E, Rizos M, Kokoris SI, et al. The haemostatic profile in critically ill COVID-19 patients receiving therapeutic anticoagulant therapy: an observational study. Medicine (Baltimore) 2020;99:e23365. doi: 10.1097/MD.0000000000023365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Corrêa TD, Cordioli RL, Campos Guerra JC, Caldin da Silva B, Dos Reis Rodrigues R, de Souza GM, et al. Coagulation profile of COVID-19 patients admitted to the ICU: an exploratory study. PLoS One. 2020;15:e0243604. doi: 10.1371/journal.pone.0243604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van der Linden J, Almskog L, Liliequist A, Grip J, Fux T, Rysz S, et al. Thromboembolism, hypercoagulopathy, and antiphospholipid antibodies in critically ill coronavirus disease 2019 patients: a before and after study of enhanced anticoagulation. Crit Care Explor. 2020;2:e0308. doi: 10.1097/CCE.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barrett CD, Moore HB, Moore EE, McIntyre RC, Moore PK, Burke J, et al. Fibrinolytic therapy for refractory COVID-19 acute respiratory distress syndrome: scientific rationale and review. Res Pract Thromb Haemost. 2020;4:524–31. doi: 10.1002/rth2.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kichloo A, Dettloff K, Aljadah M, Albosta M, Jamal S, Singh J, et al. COVID-19 and hypercoagulability: a review. Clin Appl Thromb Hemost. 2020;26:1076029620962853. doi: 10.1177/1076029620962853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bakchoul T, Hammer S, Lang P, Rosenberger P. Fibrinolysis shut down in COVID-19 patients: report on two severe cases with potential diagnostic and clinical relevance. Thrombosis Update. 2020;1:100008. doi: 10.1016/j.tru.2020.100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goyal A, Saigal S, Niwariya Y, Sharma J, Singh P. Successful use of tPA for thrombolysis in COVID related ARDS: a case series. J Thromb Thrombolysis. 2021;51:293–6. doi: 10.1007/s11239-020-02208-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost. 2020;18:1752–5. doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Campello E, Farina F, Spiezia L, Maggiolo S, Palmieri A, Sartorello F, et al. Thromboelastometry profiles in patients undergoing thrombolytic therapy for acute ischaemic stroke. Thromb Haemost. 2016;115:1231–4. doi: 10.1160/TH15-10-0798. [DOI] [PubMed] [Google Scholar]
- 55.Asakura H, Ogawa H. Perspective on fibrinolytic therapy in COVID-19: the potential of inhalation therapy against suppressed-fibrinolytic-type DIC. J Intensive Care. 2020;8:71. doi: 10.1186/s40560-020-00491-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Moore HB, Barrett CD, Moore EE, Jhunjhnuwala R, McIntyre RC, Moore PK, et al. Study of Alteplase for Respiratory failure in SARS-Cov2/COVID-19: study design of the phase IIa STARS trial. Res Pract Thromb Haemost. 2020;4:984–96. doi: 10.1002/rth2.12395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Whyte CS, Morrow GB, Mitchell JL, Chowdary P, Mutch NJ. Fibrinolytic abnormalities in acute respiratory distress syndrome (ARDS) and versatility of thrombolytic drugs to treat COVID-19. J Thromb Haemost. 2020;18:1548–55. doi: 10.1111/jth.14872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Y, Wang T, Guo C, Zhang D, Ge X, Huang Z, et al. Plasminogen improves lung lesions and hypoxemia in patients with COVID-19. QJM. 2020;113:539–45. doi: 10.1093/qjmed/hcaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Abdelaal Ahmed Mahmoud A, Mahmoud HE, Mahran MA, Khaled M. Streptokinase versus unfractionated heparin nebulization in patients with severe acute respiratory distress syndrome (ARDS): a randomized controlled trial with observational controls. J Cardiothorac Vasc Anesth. 2020;34:436–43. doi: 10.1053/j.jvca.2019.05.035. [DOI] [PubMed] [Google Scholar]
- 60.Bachler M, Hell T, Bösch J, Treml B, Schenk B, Treichl B, et al. A prospective pilot trial to assess the efficacy of Argatroban (Argatra®) in critically ill patients with heparin resistance. J Clin Med. 2020;9:963. doi: 10.3390/jcm9040963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maurin N. Heparin resistance and antithrombin deficiency. Med Klin (Munich) 2009;104:441–9. doi: 10.1007/s00063-009-1093-8. [DOI] [PubMed] [Google Scholar]
- 62.Durrani J, Malik F, Ali N, Jafri SI. To be or not to be a case of heparin resistance. J Community Hosp Intern Med Perspect. 2018;8:145–8. doi: 10.1080/20009666.2018.1466599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hardy M, Michaux I, Lessire S, Douxfils J, Dogné JM, Bareille M, et al. Prothrombotic disturbances of hemostasis of patients with severe COVID-19: a prospective longitudinal observational study. Thromb Res. 2021;197:20–3. doi: 10.1016/j.thromres.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.White D, MacDonald S, Bull T, Hayman M, de Monteverde-Robb R, Sapsford D, et al. Heparin resistance in COVID-19 patients in the intensive care unit. J Thromb Thrombolysis. 2020;50:287–91. doi: 10.1007/s11239-020-02145-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ichikawa J, Kodaka M, Nishiyama K, Hirasaki Y, Ozaki M, Komori M. Reappearance of circulating heparin in whole blood heparin concentration-based management does not correlate with postoperative bleeding after cardiac surgery. J Cardiothorac Vasc Anesth. 2014;28:1003–7. doi: 10.1053/j.jvca.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 66.Koleilat I, Galen B, Choinski K, Hatch AN, Jones DB, Billett H, et al. Clinical characteristics of acute lower extremity deep venous thrombosis diagnosed by duplex in patients hospitalized for coronavirus disease 2019. J Vasc Surg Venous Lymphat Disord. 2021;9:36–46. doi: 10.1016/j.jvsv.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang X, Du B, Li J, Wang S, Wang X, Guo M, et al. D-dimer surge and coagulation disorders in COVID-19 related pneumonia patients with cardiac injury: a case series. Medicine (Baltimore) 2020;99:e21513. doi: 10.1097/MD.0000000000021513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Billett HH, Reyes-Gil M, Szymanski J, Ikemura K, Stahl LR, Lo Y, et al. Anticoagulation in COVID-19: effect of enoxaparin, heparin, and apixaban on mortality. Thromb Haemost. 2020;120:1691–9. doi: 10.1055/s-0040-1720978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wenzler E, Engineer MH, Yaqoob M, Benken ST. Safety and efficacy of apixaban for therapeutic anticoagulation in critically ill ICU patients with severe COVID-19 respiratory disease. TH Open. 2020;4:e376–82. doi: 10.1055/s-0040-1720962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Testa S, Prandoni P, Paoletti O, Morandini R, Tala M, Dellanoce C, et al. Direct oral anticoagulant plasma levels' striking increase in severe COVID-19 respiratory syndrome patients treated with antiviral agents: the Cremona experience. J Thromb Haemost. 2020;18:1320–3. doi: 10.1111/jth.14871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Adelmann D, Wiegele M, Wohlgemuth RK, Koch S, Frantal S, Quehenberger P, et al. Measuring the activity of apixaban and rivaroxaban with rotational thrombelastometry. Thromb Res. 2014;134:918–23. doi: 10.1016/j.thromres.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 72.Vedovati MC, Mosconi MG, Isidori F, Agnelli G, Becattini C. Global thromboelastometry in patients receiving direct oral anticoagulants: the RO-DOA study. J Thromb Thrombolysis. 2020;49:251–8. doi: 10.1007/s11239-019-01956-0. [DOI] [PubMed] [Google Scholar]
- 73.Beiderlinden M, Werner P, Bahlmann A, Kemper J, Brezina T, Schäfer M, et al. Monitoring of argatroban and lepirudin anticoagulation in critically ill patients by conventional laboratory parameters and rotational thromboelastometry - a prospectively controlled randomized double-blind clinical trial. BMC Anesthesiol. 2018;18:18. doi: 10.1186/s12871-018-0475-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schaden E, Schober A, Hacker S, Kozek-Langenecker S. Ecarin modified rotational thrombelastometry: a point-of-care applicable alternative to monitor the direct thrombin inhibitor argatroban. Wien Klin Wochenschr. 2013;125:156–9. doi: 10.1007/s00508-013-0327-1. [DOI] [PubMed] [Google Scholar]
- 75.Ranucci M, Ballotta A, Di Dedda U, Bayshnikova E, Dei Poli M, Resta M, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost. 2020;18:1747–51. doi: 10.1111/jth.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maier CL, Barker NA, Sniecinski RM. Falsely low fibrinogen levels in COVID-19 patients on direct thrombin inhibitors. Anesth Analg. 2020;131:e117–9. doi: 10.1213/ANE.0000000000004949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JC, Fogerty AE, Waheed A, et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood. 2020;136:489–500. doi: 10.1182/blood.2020006520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jiménez D, García-Sanchez A, Rali P, Muriel A, Bikdeli B, Ruiz-Artacho P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Chest. 2020;159:1182–96. doi: 10.1016/j.chest.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020;18:1094–9. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kollias A, Kyriakoulis KG, Dimakakos E, Poulakou G, Stergiou GS, Syrigos K. Thromboembolic risk and anticoagulant therapy in COVID-19 patients: emerging evidence and call for action. Br J Haematol. 2020;189:846–7. doi: 10.1111/bjh.16727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Musoke N, Lo KB, Albano J, Peterson E, Bhargav R, Gul F, et al. Anticoagulation and bleeding risk in patients with COVID-19. Thromb Res. 2020;196:227–30. doi: 10.1016/j.thromres.2020.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dogra S, Jain R, Cao M, Bilaloglu S, Zagzag D, Hochman S, et al. Hemorrhagic stroke and anticoagulation in COVID-19. J Stroke Cerebrovasc Dis. 2020;29:104984. doi: 10.1016/j.jstrokecerebrovasdis.2020.104984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Usman AA, Han J, Acker A, Olia SE, Bermudez C, Cucchiara B, et al. A case series of devastating intracranial hemorrhage during venovenous extracorporeal membrane oxygenation for COVID-19. J Cardiothorac Vasc Anesth. 2020;34:3006–12. doi: 10.1053/j.jvca.2020.07.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schmidt M, Hajage D, Lebreton G, Monsel A, Voiriot G, Levy D, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med. 2020;8:1121–31. doi: 10.1016/S2213-2600(20)30328-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yassen K, Refaat E, Helal S, Metwally A, Youssef S, Görlinger K. Perioperative heparinase rotational thromboelastometry monitoring during and after adult living related liver transplantation. Eur J Anaesth. 2018;35(e-Suppl 56):286. [Google Scholar]
- 86.Al-Jazairi A, Raslan S, Al-Mehizia R, Dalaty HA, De Vol EB, Saad E, et al. Performance assessment of a multifaceted unfractionated heparin dosing protocol in adult patients on extracorporeal membrane oxygenator. Ann Pharmacother 2020. doi: 10.1177/1060028020960409. Advance Access published on Sep 22, 2020. doi: 10.1177/1060028020960409. [DOI] [PubMed] [Google Scholar]
- 87.Willems A, Roeleveld PP, Labarinas S, Cyrus JW, Muszynski JA, Nellis ME, et al. Anti-Xa versus time-guided anticoagulation strategies in extracorporeal membrane oxygenation: a systematic review and meta-analysis. Perfusion 2020. doi: 10.1177/0267659120952982. Advance Access published on Aug 29, 2020. doi: 10.1177/0267659120952982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Buscher H, Zhang D, Nair P. A pilot, randomised controlled trial of a rotational thromboelastometry-based algorithm to treat bleeding episodes in extracorporeal life support: the TEM Protocol in ECLS Study (TEMPEST) Crit Care Resusc. 2017;19(Suppl 1):29–36. [PubMed] [Google Scholar]
- 89.Schaden E, Schober A, Hacker S, Spiss C, Chiari A, Kozek-Langenecker S. Determination of enoxaparin with rotational thrombelastometry using the prothrombinase-induced clotting time reagent. Blood Coagul Fibrinolysis. 2010;21:256–61. doi: 10.1097/MBC.0b013e328337014c. [DOI] [PubMed] [Google Scholar]
- 90.Jilma-Stohlawetz P, Fritsche-Polanz S, Quehenberger P, Schörgenhofer C, Bartko J, Ristl R, et al. Evaluation of between-, within- and day-to-day variation of coagulation measured by rotational thrombelastometry (ROTEM) Scand J Clin Lab Invest. 2017;77:651–7. doi: 10.1080/00365513.2017.1394487. [DOI] [PubMed] [Google Scholar]


