Abstract
Aim:
To compare the outcomes between the arthroscopic debridement of the extensor carpi radialis brevis (ECRB) tendon alone and repairs to the ECRB tendon with suture anchor for the treatment of refractory lateral epicondylitis (LE).
Methods:
We retrospectively reviewed our patients who underwent arthroscopic surgical treatment for refractory LE by a single surgeon from January 2008 to June 2018 with a minimum follow-up of 12 months. The visual analog scale (VAS), the Mayo Elbow Performance Score (MEPS), the Disability of the Arm, Shoulder, and Hand (DASH) questionnaire, the Patient-Rated Tennis Elbow Evaluation (PRTEE) scale, the Verhaar scoring system and the time of back to work were compared between two groups.
Results:
Both groups showed a significant postoperative improvement regarding the VAS, MEPS, DASH, PRTEE and the Verhaar scoring system (p < 0.05). The repair group showed better results regarding the MEPS, DASH, PRTEE and Verhaar scoring system comparing with the debridement group, which were statically significant (p < 0.05). There were no significant differences between the two groups regarding the VAS both at rest and activity at the final follow-up. There were no significant differences for the average time for return to work (p = 0.229). There were 11 patients in the debridement group and six patients in the repair group, who completed the MRI evaluation at 6 months postoperatively.
Conclusion:
Compared with arthroscopic release and debridement of the ECRB tendon, arthroscopic suture anchor repairing of the origin of the ECRB tendon provides better outcomes when addressing the refractory LE.
Level of Evidence:
Case Series: Level IV
Keywords: Lateral peicondylitis, extensor carpi radialis brevis, suture anchor, DASH, PRTEE, Verhaar scoring system
Introduction
Lateral epicondylitis (LE), also known as tennis elbow, is a common cause of elbow pain and disability, with a prevalence of 1–3% in the adult.1 Historically, LE may contribute to the overuse of or microtrauma to the tendon of the extensor carpi radialis brevis (ECRB) at the elbow lateral epicondyle. Recent research confirmed that LE is a degenerative condition occurring at the bone–tendon interface of the ECRB origin.2,3 Although conservative methods were reported to have excellent to good outcomes,4–9 4–11% of patients fail to response to non-operative treatments and need surgical treatment.10
Release and debridement of the ECRB tendons have been documented with satisfactory short- to long-term clinical outcomes.11–17 However, a failure rate of 15% was reported due to persistent pain and loss of function. Monto contributed the failure to no reattachment of the ECRB tendon back to the lateral epicondyle. He reported reattaching the ECRB tendon during open procedure with suture anchors in 2014. In his comparable study, the repair group showed significantly better results when compared with open tendon debridement technique alone.18
As a mini-invasive alternative, Baker and Cummings19 described the arthroscopic technique to release the ECRB in 1998 and reported satisfactory results:20 93.3% of their patients improved, and 71% had good or excellent results, which was comparable to open procedure.11 Since then, most studies provided similar clinical outcomes and shorter time to return to work and less complication rate compared with open procedure.21–23
It still remained unknown whether arthroscopic reattachment of the origin of ECRB after the debridement with suture anchors would have better outcomes than arthroscopic debridement technique alone, which occurred in open procedure as Monto reported. The purpose of the current study was to retrospectively compare the outcomes between the arthroscopic debridement of the ECRB tendon alone and repairs to the ECRB tendon with suture anchor arthroscopically for the treatment of refractory LE. Our hypothesis is that the additional arthroscopic suture anchor repairing ECRB may provide better outcomes than the arthroscopic debridement alone.
Methods
This was a retrospective comparative study of the ECRB arthroscopic releasing and debridement procedure and additionally ECRB repair with arthroscopic suture anchor for the treatment of refractory LE. Written informed consent was obtained from each patient preoperatively and the present study was approved by the Ethics Committee of Jishuitan Hospital (IRB number 20190115).
We searched our institutional database for patients who underwent arthroscopic surgical treatment for refractory LE by a single surgeon from January 2008 to June 2018 with a minimum follow-up of 12 months. The study included participants of both genders, aged >18 years, who had a clinical diagnosis of unilateral LE and failure in conservative treatment at least 3 months. Our conservative treatment included rest, cryotherapy, physical therapy, massage, non-steroidal anti-inflammatories and bracing; no invasive managements were performed on this patient group. The following were excluded: individuals with local or generalized arthritis, neurologic deficit, steroid or biologic (i.e. platelet-rich plasma) injections used, combined medial epicondylitis or other elbow disorders, contraindications to the medication to be administered, pain or symptoms of unknown origin, received elbow surgery before or did not receive conservative treatment before the surgery.
Operative procedure
Arthroscopic ECRB debridement (debridement group)
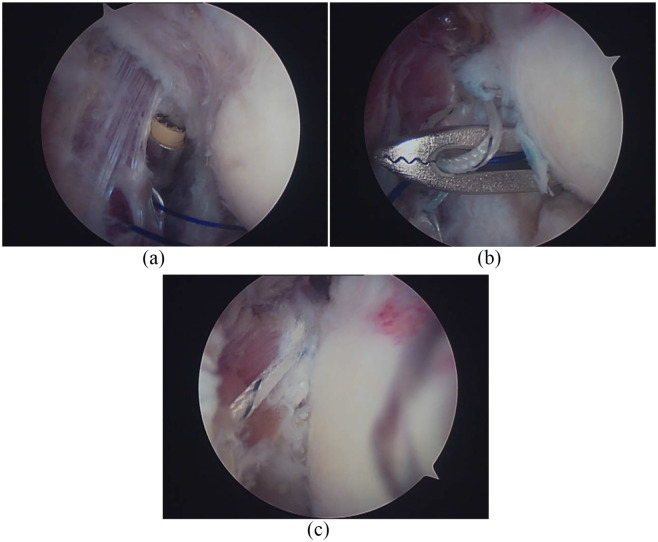
Patients were placed in lateral decubitus position on the operating table with the affected elbow at 90° of flexion. The limb was prepared and draped free in the usual operative manner. Four arthroscopic portals were set up: soft spot portal, accessory posterolateral portal, proximal anteromedial portal and proximal anterolateral portal. On introduction of the arthroscope through the soft spot portal, a full intra-articular joint inspection was performed and intra-articular pathology, especially radial-capitilum joint synovitis, was addressed. Synovectomy was performed by shaver through the accessory posterolateral portal when necessary. The lateral epicondyle and common extensor origin were visualized using the anteromedial portal. A 30° arthroscope allows excellent visualization of the lateral capsule and ECRB tendon, as well as the lateral epicondyle itself. The ECRB tendon was identified, release and debridement was performed from the most distal level of pathologic involvement proximally to the insertion site on the lateral epicondyle by radiofrequency through anterolateral portal [Figure 1(a) to (c)].
Figure 1.
Arthroscopic extensor carpi radialis brevis (ECRB) debridement: (a) ECRB degenerative change found arthroscopically, (b) ECRB releasing with radiofrequency though proximal anterolateral portal, (c) ECRB debridement.
Arthroscopic ECRB suture anchor repair (repair group)
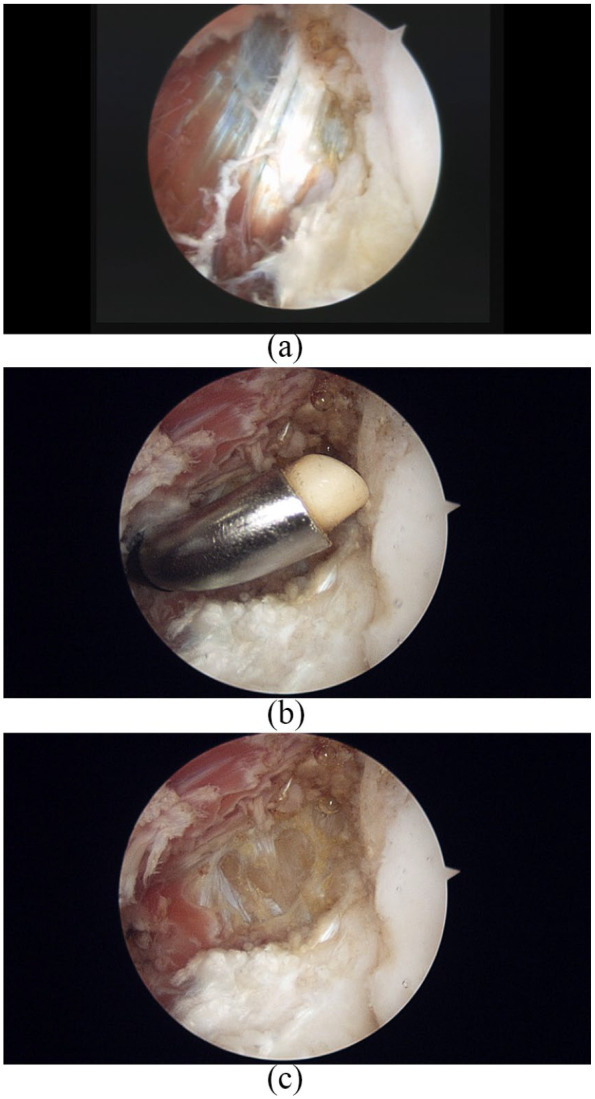
Patients randomized to the repair group received ECRB release and debridement in the same way as the debridement group. One additional anterolateral portal was set up for anchor suture repair after debridement. A pilot hole directed slightly upward was made with a 3.0-mm drill-bit before anchor fixation through the proximal anterolateral portal. The drill sleeve was kept in situ when the drill bit was removed. One 3.5 mm diameter PEEK anchor with double loaded thread (HEALICOIL, Smith & Nephew, Memphis, TN, USA) was inserted into the lateral epicondyle through the drill sleeve. A spinal needle was passed through the anterolateral portal to penetrate the distal ECRB tendon. A polydioxanone (PDS; Ethicon) suture was passed through the spinal needle and pulled out through the soft spot portal using a grasper together with the anchor thread. The shuttle relay was made by connecting the PDS with the thread and was then pulled out through the anterolateral portal. Two more sequences were repeated to make paired strands of one thread and one other strand of thread passed through the ECRB separately. A subcutaneous passageway between two lateral portals was made with a stab and then the two strands of each thread were pulled in a separate lateral portal. The knot was tied in modified Mason–Allen method [Figure 2(a) to (c)].
Figure 2.
Arthroscopic extensor carpi radialis brevis (ECRB) suture anchor repair: (a) normal tendon after ECRB debridement, (b) a polydioxanone suture was passed though anterolateral portal and pulled out through the soft spot portal using a grasper together with the anchor thread, (c) ECRB repair with threads tied.
Postoperative rehabilitation
All patients wore a brace for 1 week postoperatively and were instructed on active range-of-motion exercises for the digits, wrist and shoulder 1 day postoperatively. Passive range-of-motion exercises began when the brace was removed. Active assisted range-of-motion exercises for the elbow started 3 weeks after surgery. We encouraged patients to use their arms in daily activities and slowly progress to more difficult tasks as long as the pain was tolerable but did not allow them to return to work for 6 weeks. All patients were instructed to follow the same physiotherapy regimen.
Outcome assessment
A 0–10 visual analog scale (VAS) was used to assess pain at rest and pain during daily life activity, which 0 indicates no pain and 10 indicates the maximum possible pain. The functional measurements recorded included Mayo Elbow Performance Score (MEPS),24 Disability of the Arm, Shoulder, and Hand (DASH) questionnaire,25 Patient-Rated Tennis Elbow Evaluation (PRTEE) scale,26 scoring system of Verhaar et al.13 The Verhaar13 scoring system was rated as excellent, good, fair and poor, based on the patients’ pain, power of the grip and satisfactory to the treatment postoperatively. The time of back to work from surgery was recorded. Clinical evaluations were conducted preoperatively and at a final time followed up postoperatively, which was more than 12 months postoperatively. Patients who had magnetic resonance imaging (MRI) and followed up for more than 6 months were recorded and classified in four grades:27 grade 0, normal signal at the ECRB site; grade 1, focal increased signal without tendon thickness; grade 2, increased signal involving ⩽50% of tendon cross section with thickness; grade 3, increased signal involving >50% of tendon cross section with thickness. Two previously trained independent researchers performed the evaluation protocols.
Statistical analysis
All analyses were conducted on SPSS software for Windows, version 13.0 (Chicago, IL, USA). Preoperatively, the χ2 test was used to compare the gender, involved side of arm, rate of dominant side, heavy labor, smoker, and Verhaar scoring system between the two groups. After calculation of the distribution by the Shapiro–Wilk test, the Mann–Whitney U test was used to compare the age, body mass index, the time from injury to surgery, the follow-up time between the groups. The Mann–Whitney U test was used for the comparison between preoperative and postoperative VAS, MEPS, DASH, PRTEE within the groups. The Mann–Whitney U test was also used to compare the VAS, MEPS, DASH, PRTEE and time back to work between the two groups at the follow-up time. The χ2 test was used to compare the Verhaar scoring system between the two groups. The statistic significance difference was considered as p value below 0.05.
Results
We identified a total of 56 consecutive patients. Of these, four patients were excluded because of a short follow-up period. Finally, 52 patients were included in the study cohort. There were 33 patients in the debridement group and 19 patients in the repair group. The debridement group consisted of seven men and 26 women with a mean age of 50.1 years (range, 39–72 years). The repair group included seven men and 12 women with a mean age of 49.6 years (range, 39–69 years). There were no significant differences in clinical characteristics or any subjective or objective evaluations between the two groups preoperatively (Table 1).
Table 1.
Demographic and clinical characteristics.
| Variable | Debridement group n = 33 |
Repair group n = 19 |
p value |
|---|---|---|---|
| Age, years | 50.1 ± 8.1 | 49.6 ± 6.9 | 0.886 |
| Gender, M/F, n | 7/26 | 7/12 | 0.331 |
| BMI, kg/m2 | 24.0 ± 3.1 | 23.8 ± 3.0 | 0.887 |
| Affected | 0.205 | ||
| Arm, n (%) | |||
| Right | 23 (69.7) | 16 (84.2) | |
| Left | 10 (30.3) | 3 (15.8) | |
| Dominant | 0.534 | ||
| Arm, n (%) | |||
| Right | 30 (90.9) | 18 (94.7%) | |
| Left | 3 (9.1) | 1 (5.3%) | |
| Heavy labor, Y/N, n | 7/26 | 4/15 | 0.638 |
| Smoker, Y/N, n | 4/29 | 4/15 | 0.316 |
| Duration time, months | 21.4 ± 17.8 | 21.5 ± 18.9 | 0.199 |
| Follow-up time, months | 21.5 ± 18.9 | 22.8 ± 17.7 | 0.566 |
Data are reported as mean ± SD (95% confidence interval) unless noted otherwise.
BMI, body mass index; F, female; M, male; Y/N, yes/no.
Both groups showed a significant improvement for all outcome measures at the last follow-up postoperatively compared with those preoperatively (Tables 2 and 3). The repair group showed better results compared with the debridement group regarding the MEPS, DASH, PRTEE and Verhaar scoring system, which were statically significant (p < 0.05) (Tables 2 and 3). There were no significant differences between the two groups regarding the VAS both at rest and activity at the final follow-up. The average time for return to work was 8.0 ± 2.4 weeks for the debridement group and 7.2 ± 2.0 weeks for the repair group respectively, for which no significant difference (p = 0.229) was found between the two groups (Table 2).
Table 2.
Comparison between preoperative and postoperative function scores.
| Variable | Debridement group n = 33 |
Repair group n = 19 |
p value |
|---|---|---|---|
| VAS at rest | |||
| Preoperative | 1.5 ± 2.4 | 2.4 ± 2.8 | 0.14 |
| Final follow-up | 0.3 ± 0.8 | 0.2 ± 0.7 | 0.312 |
| p value | 0.01 | 0.02 | |
| VAS in daily life | |||
| Preoperative | 4.9 ± 2.2 | 5.5 ± 2.1 | 0.356 |
| Final follow-up | 1.9 ± 1.7 | 0.8 ± 1.3 | 0.23 |
| p value | 0.000 | 0.000 | |
| MEPS | |||
| Preoperative | 69.2 ± 11.6 | 70.5 ± 15.0 | 0.714 |
| Final follow-up | 87.3 ± 12.5 | 96.1 ± 6.8 | 0.006 |
| p value | 0.000 | 0.000 | |
| DASH | |||
| Preoperative | 44.5 ± 7.3 | 44.4 ± 8.4 | 0.805 |
| Final follow-up | 12.6 ± 9.2 | 5.9 ± 3.9 | 0.011 |
| p value | 0.000 | 0.000 | |
| PRTEE | |||
| Preoperative | 51.4 ± 17.4 | 52.4 ± 21.0 | 0.939 |
| Final follow-up | 12.8 ± 13.4 | 4.7 ± 6.8 | 0.019 |
| p value | 0.000 | 0.000 | |
| Time back to work, weeks | 8.0 ± 2.4 | 7.2 ± 2.0 | 0.229 |
Data are reported as mean ± SD (95% confidence interval) unless noted otherwise.
DASH, Disability of the Arm, Shoulder, and Hand; MEPS, Mayo Elbow Performance Score; PRTEE, Patient-Rated Tennis Elbow Evaluation; VAS, visual analog scale.
Table 3.
Comparison between preoperative and postoperative on the scoring system of Verhaar et al.13
| Debridement group n = 11 |
Repair group n = 6 |
p value | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Excellent | Good | Fair | Poor | Excellent | Good | Fair | Poor | ||||||||
| Preoperative | 0 | 0 | 14 | 19 | 0 | 0 | 10 | 9 | 0.336 | ||||||
| Final follow-up | 11 | 19 | 3 | 0 | 14 | 5 | 0 | 0 | 0.015 | ||||||
| p value | 0.000 | 0.000 | |||||||||||||
There were 11 patients in the debridement group and six patients in the repair group who completed the MRI evaluation at 6 months postoperatively. There were six patients classified to grade 0, four patients to grade 1 and one patient to grade 2 in the debridement group. Four patients showed grade 0, one patient showed grade 1 and one patient showed grade 2 in the repair group. The normal rate (grade 0 with grade 1) was 90.9% (10/11) in the debridement group and 83.3% (5/6) in the repair group. No further statistical analysis was performed due to limited cases in each group (Table 4).
Table 4.
Results of postoperative magnetic resonance imaging evaluation.
| Grade | Debridement group n = 11 |
Repair group n = 6 |
|---|---|---|
| 0 | 6 | 4 |
| 1 | 4 | 1 |
| 2 | 1 | 1 |
| 3 | 0 | 0 |
No complications were reported except for one case of ulnar nerve symptom in the debridement group. The patient complained of mild paresthesia of the ulnar side of the forearm at the second day postoperatively with no limitation of movement or numbness of finger, which resolved at 1 month postoperatively without any further treatment.
Discussion
The most important finding of our study is that reattachment of the ECRB tendon back to the lateral epicondyle with suture anchors arthroscopically after debridement provides better functional scores compared with ECRB arthroscopic debridement alone. The current study is the first to compare the clinical outcomes between arthroscopic ECRB debridement and arthroscopic ECRB debridement combined with reattachment of the tendon to its origin with suture anchors for the treatment of refractory LE.
Excision of diseased tissue at the origin of the ECRB tendon was first described by Nirschl and Pettrone11 in 1979 and then was universally accepted. An overall improvement rate of 97.7% with 85.2% of the patients returned to full activity was reported.11 Dunn et al.12 reported that 84% of 83 patients had good or excellent scores with a mean follow-up of 12.6 years. Although many studies reported that satisfactory results can be achieved by open technique regarding the functional outcome scores, grip strength, patient satisfaction, time for return to work, and complications such as wound hematoma, persistent pain, stiffness and neurological problems cannot be avoided.28,29
With the advancement of the arthroscopy technique, arthroscopic management for LE was developed and showed promising outcomes. Baker et al.20 reported 95% improvement with an average follow-up of 2.8 years, with grip strength returned to 97% of the opposite side. Patients returned to work in an average of 2.2 weeks postoperatively. Other authors also confirmed improvement of functional scores and recovery of the grip and pinch strength with the arthroscopic technique.21,22 The present study demonstrated significant improvement in function scores, including MEPS, DASH, PRTEE and Verhaar scoring system, in both groups after arthroscopic procedure. Our results showed promising outcomes and were comparable to previous study on arthroscopic treatment on refractory LE.
Besides demonstration of the general efficacy of both ECRB debridement alone and in combination with anchored repair of the ECRB tendon arthroscopically, the additional procedure of reattachment of the ECRB tendon with suture anchors was found to be clinically superior to arthroscopic debridement alone in MEPS, DASH, PRTEE and Verhaar scoring system. Our results also showed lower VAS scores (both at rest and activity) and quicker time of returning to work in the repair group compared with the debridement group, although the differences were not statistically significant. Our results are in accordance with those of Monto’s in treating refractory LE. In his study, at every follow-up time, the suture anchor group showed better MEPS and DASH functional scores and grip and pinch strength than those of the debridement group. The author contributed the better results of the suture anchor group to the firm reestablishment of the extensor tendon attachment to its humeral origin, which maybe had a better biomechanical effect for the healing of the origin of the ECRB tendon.18 We found this advantage also present in arthroscopic procedure.
Although reattaching the ECRB back to the lateral epicondyle with suture anchor arthroscopically is a time consuming procedure, it was proved by the present study that this additional procedure is safe and effective. With the scope staying in the proximal anteromedial portal, we can supervise the anchor insertion through the proximal anterolateral portal and threads passing though the anterolateral portal and soft spot portal. In our series, there was no radial nerve injury or posterolateral rotational instability occurring postoperatively. Although the most part of the repairing procedure was performed on the lateral side of the joint, we did not find any important structure such as lateral collateral ligament or profound branch of radial nerve violated. Only one patient (1.8%) complained of mild ulnar nerve syndrome in our series, which recovered without any further treatment 3 month after the operation. The possible reason is transient irritation due to the edema of the irrigation during the procedure.
Eleven patients in the debridement group and six patients in the repair group completed the MRI evaluation at 6 months postoperatively. Ten patients (90.9%) in the debridement group and five patients (83.3%) in the repair group showed intact ECRB tendon on MRI 6 months postoperative. Both groups showed high healing capacity of the ECRB tendon after the surgery. One patient in each group showed partial tear of ECRB, with abnormal signal involving ⩽50% of tendon cross section with thickness. These two patients showed satisfactory postoperative functional scores and no complain at the last follow-up.
There are several limitations in this study. First, there were obvious differences of case numbers due to the retrospective design. There were 33 cases in the debridement group and 19 cases in the repair group. However, 19 cases may fulfill the demand of the minimum number of patients required to have at least 80% power to detect the minimum clinically important difference (MCID) for functional scores.6 Second, most of the patients in the debridement group were operated on in the early time of the study, while most patients in the repair group were operated on at a later time of the study. The surgeon’s experience should be considered as a factor in the result, which cannot be avoided in most clinical studies. Third, we did not include muscle strength as one of measurements between the two groups. However, we took different elbow functional scores together, which included elbow and forearm strength already. And we found many patients may go fully back to work and life without limitation regardless of decreased muscle strength. Fourth, most patients lacked an MRI evaluation due to their satisfaction with the surgical procedure and reluctance to receive further image investigation. As a result, there were limited MRI results at the follow-up so it was not possible to compare the MRI results between the groups, which may reflect the healing status of the two techniques. Further study is needed to confirm whether there is a relationship between the MRI findings and clinical function postoperatively.
Conclusion
Compared with arthroscopic debridement of the ECRB, additionally repair to the origin of the ECRB with suture anchor arthroscopically provided better clinical outcomes when treating refractory LE.
Footnotes
Author contributions: LY participated in generating original ideas and in study design. Other co-authors participated in (1) conception and design or analysis and interpretation of data, or both: LX, ZT, LY and ZHL; (2) drafting of the manuscript or revising it critically for important intellectual content: LX, ZT, LY and ZHL; (3) data acquirement and statistics performing: LX and ZT; (4) final approval of the manuscript submitted: LX and LY.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Capital’s Fund for Health Improvment and Research, PR China, 2020-2-2073.
ORCID iDs: Xu Li  https://orcid.org/0000-0002-2255-4114
https://orcid.org/0000-0002-2255-4114
Contributor Information
Xu Li, Department of Sports Medicine, Beijing Jishuitan Hospital, Beijing, China.
Tong Zheng, Department of Sports Medicine, Beijing Jishuitan Hospital, Beijing, China.
Yue Li, Department of Sports Medicine, Beijing Jishuitan Hospital, Beijing, China.
Hailong Zhang, Department of Sports Medicine, Beijing Jishuitan Hospital, Beijing, China.
Yi Lu, Department of Sports Medicine, Beijing Jishuitan Hospital, No. 31, Xin Jie Kou East Street, Xi Cheng District, Beijing, 100035, China.
References
- 1. Verhaar JA. Tennis elbow: anatomical, epidemiological and therapeutic aspects. Int Orthop 1994; 18: 263–267. [DOI] [PubMed] [Google Scholar]
- 2. Nirschl RP, Ashman ES. Elbow tendinopathy: tennis elbow. Clin Sports Med 2003; 22: 813–836. [DOI] [PubMed] [Google Scholar]
- 3. Benjamin M, Toumi H, Ralphs JR, et al. Where tendons and ligaments meet bone: attachment sites (“entheses”) in relation to exercise and/or mechanical load. J Anat 2006; 208: 471–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lenoir H, Mares O, Carlier Y. Management of lateral epicondylitis. Orthop Traumatol Surg Res 2019; 105: S241–S246. [DOI] [PubMed] [Google Scholar]
- 5. Meyer NJ, Walter F, Haines B, et al. Modeled evidence of force reduction at the extensor carpi radialis brevis origin with the forearm support band. J Hand Surg Am 2003; 28: 279–287. [DOI] [PubMed] [Google Scholar]
- 6. Paoloni J, Appleyard R, Nelson J, et al. Topical nitric oxide application in the treatment of chronic extensor tendinosis at the elbow: a randomized, double-blinded, placebo-controlled clinical trial. Am J Sports Med 2003; 31: 915–920. [DOI] [PubMed] [Google Scholar]
- 7. Bisset L, Coombes B, Vicenzino B. Tennis elbow. BMJ Clin Evid 2011; 27; 1117. [PMC free article] [PubMed] [Google Scholar]
- 8. Thiele S, Thiele R, Gerdesmeyerb L. Lateral epicondylitis: this is still a main indication for extracorporeal shockwave therapy. Int J Surg 2015; 24: 165–170. [DOI] [PubMed] [Google Scholar]
- 9. Lim W, Park SH, Kim B, et al. Relationship of cytokine levels and clinical effect on platelet-rich plasma-treated lateral epicondylitis. J Orthop Res 2018; 36: 913–920. [DOI] [PubMed] [Google Scholar]
- 10. Gregory BP, Wysocki RW, Cohen MS. Controversies in surgical management of recalcitrant enteropathy of the extensor carpi radialis brevis. J Hand Surg Am 2016; 4: 856–859. [DOI] [PubMed] [Google Scholar]
- 11. Nirschl RP, Pettrone FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J Bone Joint Surg Am 1979; 61: 832–839. [PubMed] [Google Scholar]
- 12. Dunn JH, Kim JJ, Davis L, et al. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med 2008; 36: 261–266. [DOI] [PubMed] [Google Scholar]
- 13. Verhaar J, Walenkamp G, Kester A, et al. Lateral extensor release for tennis elbow. A prospective long-term follow-up study. J Bone Joint Surg Am 1993; 75: 1034–1043. [DOI] [PubMed] [Google Scholar]
- 14. Rayan GM, Coray SA. V-Y slide of the common extensor origin for lateral elbow tendonopathy. J Hand Surg 2001; 26: 1138–1144. [DOI] [PubMed] [Google Scholar]
- 15. Das D, Maffulli N. Surgical management of tennis elbow. J Sports Med Phys Fitness 2002; 42: 190–197. [PubMed] [Google Scholar]
- 16. Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc 2011; 19: 1023–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jeavons R, Berg AJ, Richards I, et al. The Boyd–McLeod procedure for tennis elbow: mid- to long-term results. Shoulder Elbow 2014; 6: 276–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Monto R. Tennis elbow repair with or without suture anchors: a randomized clinical trial. Tech Should Surg 2014; 15: 92–97. [Google Scholar]
- 19. Baker CL, Cummings PD. Arthroscopic management of miscellaneous elbow disorders. Oper Tech Sports Med 1998; 6: 16–21. [Google Scholar]
- 20. Baker CL, Murphy KP, Gottlob CA, et al. Arthroscopic classification and treatment of lateral epicondylitis: two-year clinical results. J Shoulder Elbow Surg 2000; 9: 475–482. [DOI] [PubMed] [Google Scholar]
- 21. Owens BD, Murphy KP, Kuklo TR. Arthroscopic release for lateral epicondylitis. Arthroscopy 2001; 17: 582–587. [DOI] [PubMed] [Google Scholar]
- 22. Sarem i H, Seydan MA, Seifrabiei MA. Midterm results of arthroscopic treatment for recalcitrant lateral epicondylitis of the elbow. Arch Bone Jt Surg 2020; 8: 184–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Solheim E, Hegna J, Øyen J. Arthroscopic versus open tennis elbow release: 3- to 6-year results of a case-control series of 305 elbows. Arthroscopy 2013; 29: 854–859. [DOI] [PubMed] [Google Scholar]
- 24. Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow. In: Morrey BF. (ed.) The elbow and its disorders. 2nd ed. Philadelphia: Saunders, 1993, pp.86–89. [Google Scholar]
- 25. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996; 29: 602–608. [DOI] [PubMed] [Google Scholar]
- 26. Rompe JD, Overend TJ, MacDermid JC. Validation of the patient-rated tennis elbow evaluation questionnaire. J Hand Ther 2007; 20: 3–10; quiz 11. [DOI] [PubMed] [Google Scholar]
- 27. Steinborn M, Heuck A, Jessel C, et al. Magnetic resonance imaging of lateral epicondylitis of the elbow with a 0.2-T dedicated system. Eur Radiol 1999; 9: 1376–1380. [DOI] [PubMed] [Google Scholar]
- 28. Karkhanis S, Frost A, Maffulli N. Operative management of tennis elbow: a quantitative review. Br Med Bull 2008; 88: 171–188. [DOI] [PubMed] [Google Scholar]
- 29. Pomerantz ML. Complications of lateral epicondylar release. Orthop Clin North Am 2016; 47: 445–469. [DOI] [PubMed] [Google Scholar]