Abstract
A 22-year-old primigravida was diagnosed with an 18-cm splenic cyst during routine third-trimester routine ultrasound examination. She was referred to a tertiary obstetric hospital and after multidisciplinary consultation, expectant management was decided on. Induction of labour was performed at term and she delivered vaginally with vacuum extractor application without complications. Percutaneous aspiration and sclerotherapy of the cyst was performed one week after delivery. She was hemodynamically stable throughout.
Keywords: Expectant management, Pregnancy, Splenic cyst, Case report
Highlights
-
•
The diagnosis of large splenic cyst during pregnancy is a rare event and management is not standardized.
-
•
Different managements have been reported, but no strong evidence was found to support the superiority of any single treatment.
-
•
We report a case of a hemodynamically stable woman diagnosed with a large splenic cyst in the third trimester.
-
•
Expectant management was decided on, induction of labour was performed at term and the patient delivered vaginally.
-
•
Pregnant women diagnosed with a splenic cyst should be managed by a multidisciplinary team.
1. Introduction
Splenic cysts are rare clinical findings, often diagnosed incidentally upon imaging conducted for other complaints. The diagnosis of a large splenic cyst during pregnancy is rare and management is not standardized. A small number of cases have been reported in literature and different managements have been proposed. However, there is no strong evidence to support the superiority of any single treatment.
This case report documents the expectant management of a giant splenic cyst diagnosed in the third trimester. The patient had a vaginal delivery followed by postpartum sclerotherapy for the cyst.
2. Case Presentation
A 22-year-old primigravida, with no relevant clinical history except mild thrombocytopenia (96.000 platelets/ml) diagnosed during pregnancy, underwent a routine third-trimester ultrasound scan at 32 weeks. Foetal growth and anatomy were normal, with posterior placental location. During the examination, a large cyst (18 × 13 × 12 centimetres) was noted in the left hypochondrium between the spleen and the left pole of the liver (Fig. 1). The woman had no history of trauma and was asymptomatic. She was referred to a tertiary obstetric hospital for further assessment and an ultrasound examination there confirmed the presence of the giant cyst but its nature was still unclear. The following day, the patient was admitted as an emergency complaining of left hypochondrial pain. On admission, her vital signs were as follows: blood pressure 123/78 mmHg, heart rate 89 beats per minute and O2 saturation 100%. Serial measurements of vital signs were performed to exclude hemodynamic compromise due to the risk of cyst rupture and clinical stability was documented during hospitalization. Abdominal ultrasound scan and magnetic resonance imaging (MRI) were performed. MRI (Fig. 2) showed the mass to be an intra-parenchymal splenic cyst with high T1 signal intensity, suggestive of a possible previous haemorrhagic event. Four differential diagnoses were considered: epidermoid cyst, parasitic cyst, cystic lymphangioma and vascular lesion. The patient was temporarily hospitalized in the general surgery department for investigation, then returned to the obstetrics department for foetal and maternal monitoring. Both remained clinically stable. An infectious origin of the cyst was excluded by serological test results, including a test for antibodies against Echinococcus.
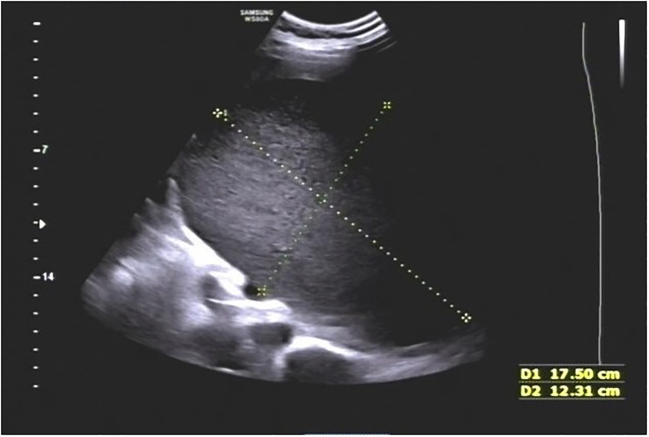
Fig. 1.
Ultrasound scan at 32 weeks of gestational age shows the cyst, 17,5 × 12,3 cm, located in the left hypochondrium.
Fig. 2.
MRI at 32 weeks of gestational age confirmed the diagnosis of splenic cyst.
A multidisciplinary team composed of obstetricians, general surgeons and anaesthetists discussed clinical management. Expectant management was decided on, with induction of labour at 37 weeks in an operating theatre so as to be ready for emergency laparotomy in case of cyst rupture. At 37 weeks and 4 days of gestation, a cervical ripening balloon was placed. It was removed after 12 h and, since the obstetric finding was still unfavourable (Bishop score < 6), according to the hospital protocols, vaginal dinoprostone was administered. Induction of labour was continued in the operating theatre with amniotomy and oxytocin infusion, with the constant presence of a team of anaesthetists, obstetricians and midwives. A general surgeon joined the team at the beginning of the second stage of labour. In order to limit the increase in intra-abdominal pressure during expulsive efforts, after determining the station and position of the foetal head with transabdominal sonography [1], a vacuum extractor was applied when the largest diameter of the foetal head reached the ischial spines. A healthy baby of 2990 g was delivered vaginally. Maternal condition remained stable and no clinical signs of cystic rupture were detected. The volume reduction of the uterus immediately after delivery allowed the palpation of the cyst to the umbilical transverse line. Five days after delivery, an upper abdominal computed tomography (CT) scan with contrast medium showed the lesion was unchanged. Fine-needle aspiration of a sample of the cystic liquid produced amorphous material and the culture test was negative. Due to clinical stability and the result of the cytological examination, a minimally invasive approach was decided on. Percutaneous aspiration and sclerotherapy of the cyst was performed under US/CT guidance: 1900 ml of blood-stained fluid was drained and 300 ml of alcohol was infused and aspirated using a French size 6 catheter. Twenty-four hours later, sclerotherapy was repeated. Before each procedure, contrast examination was performed to exclude abdominal leakage; at the end, tigecycline 80 mg was infused into the empty cyst cavity and the drainage was removed. The patient was discharged and her clinical condition remained stable over the following months.
3. Literature Review
Splenic cysts affect approximately 0.07% of the general population [2]. In the literature, of 800 cases, only 13 were described in pregnancy [[3], [4], [5], [6], [7], [8]] (Table 1). Usually, they are clinically asymptomatic, except for 30% of patients who experience pain in left hypochondrium, nausea and weight loss, hypertension due to renal artery compression, thrombocytopenia and anaemia [9].
Table 1.
Management of splenic cyst during pregnancy: review of the literature.
| Author | Type | Dimension (CM) | GA (weeks) | Management | Outcomes |
|---|---|---|---|---|---|
| Elit, 1989 | Epidermoid Ca | – | – | Oncological Surgery | – |
| Bar-Hozar, 1998 | Epidermoid cyst | – | 34 | Splenectomy LPT at term | – |
| Mendez-Arzac, 2002 | Hydatid cyst | – | – | Splenectomy II trimester | – |
| Ceglowska, 2003 | Infective cyst | – | – | TTP and splenectomy | – |
| Can, 2003 | Hydatid cyst | – | 25 | Exeresis at 25w | – |
| Rotas, 2007 | Epidermoid cyst | 17 | 9 | Percutaneous drainage at 14w and 16w, sepsis, Antibiotic therapy, Fenestration LPS and omentopexy at 17w | Spontaneous delivery at 38w without complications |
| Montasser, 2010 | – | 20 | 24 | Percutaneous drainage, infection, Antibiotic therapy, anaemia and trasfusion | Spontaneous delivery at 40w. Percutaneous aspiration 6w after delivery, spontaneous resolution after 1 year |
| Hamm,2012 | Epidermoid cyst | 14 | 27 | Expectant management till 33w, intracystic haemorrhage without rupture, Emergency C-Section and splenectomy | No complications |
| Hamm, 2012 | Epidermoid cyst | 9 | 20 | Percutaneous aspiration and drainage at 34w, recurrence and drainage at 38w | C-section at 40w for dystocia. Alcohlization 2 days post-partum. Recurrence a 2 months post-partum. |
| Farouzesh, 2013 | Epidermoid cyst | 20 | 15 | Splenectomy at 17w | No complications |
| Varban, 2013 | Multilocular epidermoid cyst | 11 | 18 | Vaccination (Meningo, Pneumo and Haemophilus) and LPS Splenectomy | Spontaneous delivery at term |
| Lederrey, 2016 | – | 13 | 10 | Expectant management | Spontaneous delivery at term. Splenectomy 6 months after delivery. |
| Kapp, 2016 | Epithelial cyst | 15 | 8 | LPS exeresis of cyst | No complications |
Legend: LPT: laparotomy, LPS: laparoscopy, TTP: therapeutic termination of pregnancy.
Splenic cysts can be classified as parasitic and non-parasitic, according to the cause, or as primary and secondary, according to the presence or absence of an epithelial lining [10]. Primary cysts are classified as parasitic, congenital and neoplastic types. The parasitic type is most commonly caused by Echinococcus granulosus larvae and rupture of the cyst may result in anaphylactic shock. Congenital cysts occur mainly in children and young adults and can be epidermoid, dermoid or endodermoid, depending on the tissue of origin. [9] Neoplastic cysts are divided in dermoid type and endodermoid type (hemangiomas and lymphangiomas). Secondary cysts are the most common; they are pseudocysts without epithelial wall, and 75% are post-traumatic while 25% are caused by mononucleosis, tuberculosis or malaria [10,11].
First-level imaging consists of ultrasound, which can show the lesion as solid or fluid-filled, unilocular or multilocular, with or without calcifications or vascularization. Second-level imaging is by MRI, which has greater sensitivity and specificity than ultrasound, to provide the exact location of the cyst and help to plan the operative approach. When cancer is suspected, cytological examination through fine-needle aspiration is generally contraindicated because of the high risk of leakage of malignant cells during procedure.
The main complication of splenic cysts is rupture. In pregnancy, this happens in 4.5% of cases, mostly in the third trimester, with a high perinatal mortality rate (about 70%) [12]. Rupture of the cyst can lead to hemoperitoneum, peritonitis, sepsis and anaphylactic shock (in the case of parasitic cysts) [10,11].
Regarding treatment, the literature shows that the main criteria are dimensions of the cyst, gestational age, patient condition and level of available hospital care [4]. For small asymptomatic cysts (<5 cm), the literature supports a conservative approach with monthly ultrasound [10] because of frequent spontaneous resolution of the cyst. Larger symptomatic cysts (more than 5 cm) should be managed surgically, in the second trimester, as they are more likely to result in complications in the third trimester. Two main strategies are described in the literature: percutaneous drainage and surgery. Percutaneous drainage under ultrasound guidance can replace or precede surgery; it is effective in 80% of cases and can also be combined with sclerotherapy with alcohol [13,14]. However, some authors do not recommend this approach because of the risk of infection and recurrence [10]. Laparoscopic surgery can be performed during the second trimester. Surgical approaches include fenestration with omentopexy, which has minimal risk of bleeding [10], and marsupialization [6]. Partial splenectomy for a cyst located at the poles of the spleen preserves the immune function of the organ [5,8], while total splenectomy represents the gold standard for posterior or hilum cysts, for big or suspicious formations and in the case of rupture [[4], [5], [6]]. At present, the literature is sparse and there are no official guidelines on the management of this rare condition [7] and whether vaginal delivery should be preferred if there are no obstetric indications. Table 1 shows details of 13 cases reported in the literature, with characteristics of the cysts, gestational age at diagnosis, treatments and outcomes.
4. Case Discussion
In this case, we elected for expectant management since the diagnosis was made in the third trimester, a time during which surgical intervention would have been more harmful. As an alternative, we could have performed percutaneous drainage; however, the patient was stable and the risk of spontaneous rupture is slight. There was concern that percutaneous drainage could have been complicated by sepsis, major bleeding, recurrence and preterm labour; thus, after discussion and agreement with the patient, we opted for expectant management and induction of labour.
The hospital was equipped with 8 delivery rooms and 3 operating theatres, which meant that labour could be readily managed in an operating theatre and that extra staff were available if necessary.
The decision to perform vacuum extraction was taken when the largest diameter of the foetal head reached the plane of the ischial spines (leading point of the skull at +1/+2) to reduce expulsive efforts.
5. Conclusions
This is the second case described in the literature on the expectant management of a large splenic cyst with vaginal delivery at term performed without complications. Since the risk of spontaneous rupture is low, we believe that a pregnant woman diagnosed with a splenic cyst should be given the chance of vaginal delivery. The patient should be referred to a tertiary hospital as it can provide a safe setting for labour with a multidisciplinary team ready to perform emergency caesarean section and splenectomy in the event of cystic rupture.
Acknowledgments
Contributors
Chiara Germano contributed to manuscript writing/editing and literature revision.
Lorenza Attamante contributed to manuscript writing/editing and literature revision.
Michela Chiadò Fiorio Tin contributed to manuscript revision.
Paolo Petruzzelli contributed to manuscript revision.
Guido Menato contributed to manuscript revision.
Bianca Masturzo contributed to manuscript writing and literature revision.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
No funding from an external source supported the publication of this case report.
Patient Consent
Informed consent has been obtained from the patient. No personal information that could identify the patient is included.
Provenance and Peer Review
This case report was peer reviewed.
References
- 1.Ghi T., Dall’Asta A., Masturzo B. Randomised Italian Sonography for occiput POSition Trial Ante vacuum (R.I.S.POS.T.A.) Ultrasound Obstet. Gynecol. 2018 Dec;52(6):699–705. doi: 10.1002/uog.19091. [DOI] [PubMed] [Google Scholar]
- 2.Golmohammadzadeh H., Maddah G., Shams Hojjati Y. Splenic cysts: analysis of 16 cases. Caspian J. Intern. Med. 2016;7(3):217–221. [PMC free article] [PubMed] [Google Scholar]
- 3.Dabrowski W., Luterek K., Szczepanik A. Management of a large splenic cyst in pregnancy – a case report. Ginekol. Pol. 2012;83:862–864. [PubMed] [Google Scholar]
- 4.Hamm J.A., Delomenie M., Derniaux E. Splenic cyst during pregnancy: a rare disease with difficult management. J. Gynecol. Obstet. Biol. Reprod. 2013;42:191–194. doi: 10.1016/j.jgyn.2012.11.008. (in French) [DOI] [PubMed] [Google Scholar]
- 5.Forouzesh M., Ghanbarzadegan L., Rahimi M. Splenic epidermoid cyst during pregnancy; case report and review of the literature. Bull. Emerg. Trauma. 2013 Oct;1(4):179–181. [PMC free article] [PubMed] [Google Scholar]
- 6.Varban O. Splenic cyst during pregnancy. Int. J. Surg. Case Rep. 2014;5:315–318. doi: 10.1016/j.ijscr.2014.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lederrey J., Schäfer M., de Rham M. When the spleen meets the fetus. J. Matern. Fetal Neonatal Med. 2016;29(3):510–511. doi: 10.3109/14767058.2015.1009440. [DOI] [PubMed] [Google Scholar]
- 8.Kapp J., Lewis T., Glasgow S., Khalil A. Spleen preserving management of a non-parasitic splenic cyst in pregnancy. Ann. R. Coll. Surg. Engl. 2016 Sep;98(7):e114–e117. doi: 10.1308/rcsann.2016.0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cowles R.A., Yahanda A.M. Epidermoid cyst of the spleen. Am. J. Surg. 2000;180:227. doi: 10.1016/s0002-9610(00)00446-3. [DOI] [PubMed] [Google Scholar]
- 10.Rotas M., Ossowski R., Lutchman G. Pregnancy complicated with a giant splenic cyst: a case report and review of the literature. Arch. Gynecol. Obstet. 2007;275:301–305. doi: 10.1007/s00404-006-0229-9. [DOI] [PubMed] [Google Scholar]
- 11.Balzan S.M., Riender C.E., Santos L.M. Posttraumatic splenic cysts and partial splenectomy: report of a case. Surg. Today. 2001;31:262–265. doi: 10.1007/s005950170183. [DOI] [PubMed] [Google Scholar]
- 12.Aubrey-Bassler F.K., Sowers N. 613 cases of splenic rupture without risk factors or previously diagnosed disease: a systematic review. BMC Emerg. Med. 2012;12:11. doi: 10.1186/1471-227X-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montasser A.M., Roger B., Marwan F. Conservative management of gigantic splenic cyst during pregnancy; a differential diagnosis for chest pain caused by the forgotten organ. Gynecol. Surg. 2010;7:49–51. [Google Scholar]
- 14.Singh A.K., Shankar S., Gervais D.A. Image-guided percutaneous splenic interventions. Radiographics. 2012;32:523–534. doi: 10.1148/rg.322115135. [DOI] [PubMed] [Google Scholar]