Abstract
Cecal volvulus is an uncommon cause of colonic obstruction. First-line treatment for cecal volvulus is surgery, as nonoperative management is rarely achievable. We herein report an extremely rare case of a patient with spontaneously resolved cecal volvulus; no recurrence occurred without elective surgery. A 47-year-old woman presented with acute lower abdominal pain. She was misdiagnosed with small bowel obstruction and treated conservatively. A few hours later, she was correctly diagnosed with cecal volvulus. Subsequently, her symptoms and computed tomography findings of cecal volvulus completely disappeared. She refused elective surgery, but no recurrence occurred during five months of follow-up.
Keywords: cecal volvulus, bowel dilatation, spontaneous, conservative treatment, mobile cecum syndrome
Introduction
Cecal volvulus describes the rotation or torsion of a mobile cecum that is commonly found in young to middle-aged woman (1, 2). It is the second most common site of colonic volvulus after the sigmoid (3). While the first-line treatment for sigmoid volvulus is endoscopic detorsion, the first-line treatment for cecal volvulus is surgery, even when there are no concerning symptoms of peritonitis or perforation. As the success rate of endoscopic detorsion is low (4), the rate of ischemia in the volvulized segment is high (5). Whether or not cecal volvulus can be treated conservatively and elective surgery avoided is unclear.
We herein report an extremely rare case of a patient with cecal volvulus that resolved spontaneously, with no recurrence occurring despite no elective surgery.
Case Report
A 47-year-old woman presented to the emergency department at midnight with acute lower abdominal pain. She had a history of constipation, but no history of abdominal surgery or atonia of the colon. She also had a history of repeated mild lower abdominal distention, but she had never presented to the emergency department because the symptoms were not severe.
The abdominal pain when she visited the emergency department was the most severe in her life. She did not have any history of violent cough or extreme exertion before hospital admission. Her vital signs were stable, with a blood pressure of 142/88 mmHg, a heart rate of 68 bpm, and a body temperature of 36.9ºC. An abdominal examination revealed tenderness in the lower abdomen without rebound and guarding. The laboratory tests including her blood cell counts, inflammatory marker levels, and deviation enzymes were normal (Table). Abdominal computed tomography (CT) revealed a dilated segment of the gastrointestinal tract with the air-fluid level on the left side of the abdomen. There were no abdominal pelvic masses. She was admitted to the hospital with a mistaken diagnosis of small bowel obstruction.
Table.
Blood Test.
| Peripheral blood | Blood chemistry | |||||||
|---|---|---|---|---|---|---|---|---|
| WBC | 5,700 | /μL | TP | 7 | mg/dL | CPK | 72 | mg/dL |
| Neu | 55 | % | Alb | 3.7 | mg/dL | BUN | 10.2 | mg/dL |
| Eos | 8 | % | AST | 14 | U/L | Cr | 0.52 | mg/dL |
| Lym | 29 | % | ALT | 10 | U/L | Na | 138 | mEq/L |
| Mono | 7 | % | LDH | 177 | U/L | K | 4.0 | mEq/L |
| RBC | 393×104 | /μL | ALP | 179 | U/L | Cl | 106 | mEq/L |
| Hb | 10.9 | g/dL | T-Bil | 0.2 | mg/dL | Ca | 8.4 | mg/dL |
| Ht | 34.3 | % | AMY | 100 | U/L | CRP | 0.24 | mg/dL |
| Plt | 30.4×104 | /μL | FBS | 107 | mg/dL | |||
WBC: white blood cells, Neu: neutrophils, Eos: eosinophils, Lym: lymphocyte, Mono: monocyte, RBC: red blood cells, Hb: hemoglobin, Ht: hematocrit, Plt: platelet, TP: total protein, Alb: albumin, AST: asparate aminotransferase, ALT: alanine aminotransferase, LDH: lactate dehydorogenase, ALP: alkaline phosphatase, T-Bil: total bilirubin, AMY: amylase, FBS: fasting blood sugar, CPK: creatinine phosphokinase, BUN: blood urea nitrogen, Cr: creatinine, Na: natrium, K: kalium, Cl: chlorine, Ca: calcium, CRP: C-reactive protein
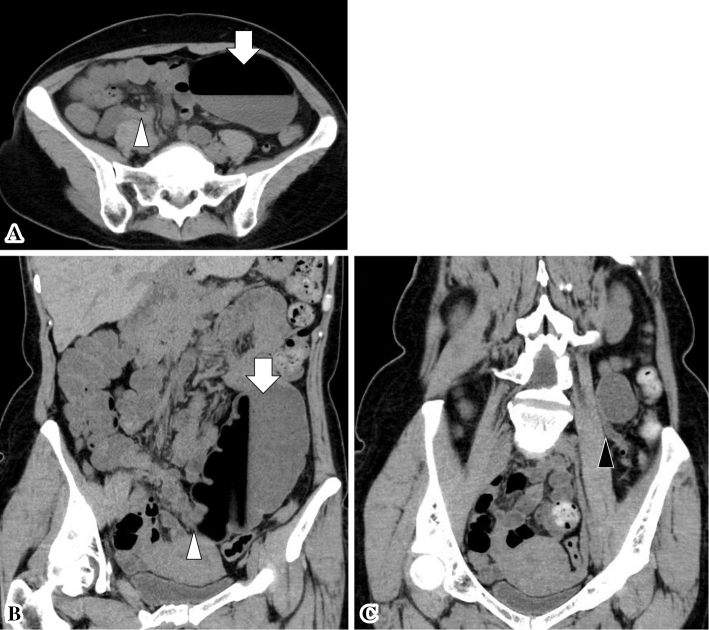
She was treated with nil per oral and intravenous infusion without any other invasive procedures. The CT scan was reevaluated the next morning. It became clear that the dilated part on the left side of the abdomen was the cecum, and it was along the ascending colon with bird beak sign (Fig. 1B) and central appendix sign (Fig. 1C). The CT scan also showed mild twisting of the mesentery around the ileocolic arteries by almost 180º. Subsequently, she was diagnosed with cecal volvulus.
Figure 1.
CT scan in axial (A) and coronal planes (B), (C) showing dilated cecum (arrow) along the ascending colon. (B) The bird beak sign (white arrowhead), and (C) the central appendix sign (abnormal position of the appendix near midline; black arrowhead) are presented. CT: computed tomography
Her symptoms completely disappeared at the time of diagnosis. A CT scan was reexamined, and the findings of cecal volvulus had disappeared (Fig. 2). She was allowed to eat orally on day 2, and was discharged on day 5 without recurrence symptoms. Colonoscopy and contrast enema (performed after discharge) revealed dilated cecum reaching the left side of abdomen without stenosis. These findings were suggestive of mobile cecum without volvulus (Fig. 3).
Figure 2.

CT scan performed after the cecal volvulus resolved spontaneously. The cecum is not dilated (arrowhead). CT: computed tomograpy
Figure 3.

Positional contrast enema showing dilated cecum reaching the left side of the abdomen without stenosis. These findings were suggestive of mobile cecum without volvulus.
We recommended elective surgery to prevent any chance of recurrence of cecal volvulus, but the patient refused. She sometimes experienced mild abdominal pain, but no recurrence of cecal volvulus occurred during the five months of follow-up (with treatment for constipation).
Discussion
This patient's course raised two important clinical issues: cecal volvulus can be resolved spontaneously, and elective surgery can be avoided.
Regarding the first point, cecal volvulus can resolve spontaneously. As mentioned above, the recommended treatment for cecal volvulus is surgery rather than nonoperative endoscopic reduction, but there are no recommendations regarding conservative treatment. There are few reports of successful endoscopic treatment for cecal volvulus, including detorsion (6), transanal ileus tube (7), transnasal ileus tube (8), and sigmoidoscopy with decompression (9). However, to our knowledge, no previous reports have described a case of spontaneously resolved cecal volvulus.
This case was misdiagnosed at the emergency department, and the chance to performe emergency surgery was missed. When we correctly diagnosed her with cecal volvulus, a few hours had already passed from the onset of symptoms, which subsequently resolved spontaneously. We suspect that three factors were responsible for the spontaneous resolution of the cecal volvulus: the degree of twisting of the ileocolic vessels, the length of the mobile cecum, and the severity of ischemia of the twisted cecum. In the present case, CT showed that the ileocolic vessels had twisted at approximately 180º, and the so called “whirl sign” was unclear. This might have been the first factor influencing the spontaneous resolution of the cecal volvulus. Gomes et al. classified the length of the mobile cecum for laparoscopic findings into three grades: grade I (cecum retroperitoneal or with little mobility), grade II (wide mobility, crossing the midline), and grade III (maximum mobility, reaching the left abdomen) (10). In the present case, the CT scan after resolution of the cecal volvulus showed shrinkage of the cecum, equivalent to grade I. The mobile cecum length would therefore have been short, which might have been the second factor influencing the spontaneous resolution of the cecal volvulus. The present case also showed no signs of peritonitis or perforation during the physical examination. This was not only the third factor associated with the spontaneous resolution of cecal volvulus, but also an essential condition for avoiding the need to perform emergency surgery.
Furthermore, the spontaneous resolution of the cecal volvulus may have been an aspect of mobile cecum syndrome. The clinical presentation patterns of cecal volvulus are categorized as recurrent intermittent, acute obstructive and acute fulminant patterns (4, 11). The recurrent intermittent pattern is also referred to as mobile cecum syndrome. It is characterized by repeated lower abdominal pain caused by mobile cecum (12), and the intermittent abdominal pain resolves spontaneously after the passage of flatus (13). The acute obstructive patterns is characterized by cramping abdominal pain and vomiting that do not resolve spontaneously. Without timely recognition and surgical treatment, this condition may progress to intestinal strangulation and perforation, eventually resulting in the acute fulminant patterns. The abdominal pain in this case may have been associated with the recurrent intermittent pattern. However, previous reports of mobile cecum syndrome mainly described cases of chronic recurrent abdominal pain, and the typical CT findings of cecal volvulus were not detected in any case. In the present case, CT performed in the emergency department revealed a dilated cecum in an abnormal position (located outside the right lower quadrant), bird beak sign (progressive tapering of the intestinal tract), and central appendix sign (abnormal position of the appendix near midline). These CT findings were reported to be diagnostic tools for cecal volvulus and a judgement tool for emergency surgery (14). Accordingly, to our knowledge, this may be the first report of the recurrent intermittent pattern with the typical CT findings of cecal volvulus.
Regarding the second point, elective surgery can be avoided when a cecal volvulus resolves spontaneously. In this case, we recommended performing of elective surgery to prevent any chance of recurrence of cecal volvulus. We considered the recurrence rate of cecal volvulus to be high in this case, as the mobile cecum had been revealed in the findings of contrast enema, and the patient had a history of repeated abdominal discomfort. However, she refused surgery, and no recurrence of cecal volvulus has occurred thus far. The need for elective surgery for spontaneously resolving cecal volvulus remains unclear, as these cases are extremely rare, and the follow up period is short. At present, elective surgery should be avoided only if the patient refuses.
Conclusion
We herein report a patient with spontaneously resolved cecal volvulus. Although the first-line treatment for cecal volvulus is surgery, conservative treatment and avoiding elective surgery may comprise acceptable management for cecal volvulus without signs of peritonitis or perforation.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Halabi WJ, Jafari MD, Kang CY, et al. Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann Surg 259: 293-301, 2014. [DOI] [PubMed] [Google Scholar]
- 2. Rabinovici R, Simansky DA, Kaplan O, Mavor E, Manny J. Cecal volvulus. Dis Colon Rectum 33: 765-769, 1990. [DOI] [PubMed] [Google Scholar]
- 3. Hiltunen KM, Syrjä H, Matikainen M. Colonic volvulus. Diagnosis and results of treatment in 82 patients. Eur J Surg 158: 607-611, 2020. [PubMed] [Google Scholar]
- 4. Friedman JD, Odland MD, Bubrick MP. Experience with colonic volvulus. Dis Colon Rectum 32: 409-416, 1989. [DOI] [PubMed] [Google Scholar]
- 5. Lau KCN, Miller BJ, Schache DJ, Cohen JR. A study of large-bowel volvulus in urban Australia. Can J Surg 49: 203-207, 2006. [PMC free article] [PubMed] [Google Scholar]
- 6. Itatani Y, Miyoshi M, Mitsudo D. A case of successful colonoscopic detorsion in cecal volvulus. Ann Kurashiki Cent Hosp 68: 151-155, 2005. [Google Scholar]
- 7. Miyano M, Takahashi T, Okusa M, et al. Reurrent bowe obstruction caused by cecal volvulus: a case report. J Nippon Med Sch 86: 183-186, 2019. [DOI] [PubMed] [Google Scholar]
- 8. Sakamoto Y, Hiyoshi Y, Sakata K, et al. Case of cecal volvulus successfully treated with endoscopic colopexy. Asian J Endosc Surg 11: 402-404, 2018. [DOI] [PubMed] [Google Scholar]
- 9. Shah F, Elsayed M, Sekhar A. Cecal bascule as a cause of postoperative nausea and abdominal pain. Radiol Case Reports 14: 697-699, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gomes CA, Soares C, Catena F, et al. Laparoscopic management of mobile cecum. JSLS 20: e2016.00076, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Consorti ET, Liu TH. Diagnosis and treatment of caecal volvulus. Postgrad Med J 81: 772-776, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cesaretti M, Trotta M, Leale I, et al. Surgery to treat symptomatic mobile cecum syndrome is safe and associated with good recovery outcomes. Case Rep Gastrointest Med 2018: 1-6, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rogers RL, Harford FJ. Mobile cecum syndrome. Dis Colon Rectum 27: 399-402, 1984. [DOI] [PubMed] [Google Scholar]
- 14. Dane B, Hindman N, Johnson E, Rosenkrantz AB. Utility of CT findings in the diagnosis of cecal volvulus. Am J Roentgenol 209: 762-766, 2017. [DOI] [PubMed] [Google Scholar]