Abstract
Healthcare-associated infections are a major issue in public health. After several decades of hand hygiene programmes, it is time to admit that we have failed to achieve our goal. One of the reasons is the overuse of gloves, which is in part justified by the nature of the nursing care. Several experimental studies supported the effectiveness of disinfecting gloves, but evidence for routine feasibility and effectiveness is lacking. The aim of this study was to evaluate the effectiveness of alcohol-based disinfection of gloves during nursing care. Swabs were taken from the most contaminated part of both hands at different times: T0 (before wearing gloves), T10 (after 10 minutes of nursing care) from both gloves, T10A (just after the gloves were disinfected for 30 seconds with bedside disposable hydroalcoholic solution) and when possible at T20 and T20A. After 10 minutes of nursing care, gloves were contaminated in 72.5% of cases. After alcohol-based disinfection, gloves became free of microorganism in 79.3% of cases. Alcohol-based disinfection of gloves during routine care is effective and appears to be a reasonable alternative to current recommendations.
Keywords: Disinfection, gloves, hand hygiene, nosocomial infection, nursing research, pathogen
Introduction
Hand hygiene, particularly the use of alcohol-based hand rubs, is currently recognized as the main barrier against cross-transmission of infections. However, despite worldwide investment in hand hygiene promotion, hospital-acquired infections have not been significantly lowered. One of the reasons of the still-insufficient practice of alcohol-based hand rub is the overuse of gloves, which is derived from the healthcare behavioral adaptation of institutional protocols to routine care. A video analysis during routine care pointed out the complex behaviors of healthcare workers (HCWs) regarding hand hygiene and wearing gloves. HCWs consider hand disinfection and wearing gloves to be two different practices [1]. The World Health Organization recommends that gloves be changed between caring for patients and between providing different types of care [2]. However, these recommendations are not easily applicable in routine care; indeed, Chau et al. [3] reported that gloves were not changed in 75% of required situations.
Gloves are required when it can be reasonably anticipated that contact with blood or other potentially infectious materials could occur. These situations cannot be anticipated, which results in disposable gloves being unjustifiably worn and hand disinfection being compromised [1]. Contaminated gloves have been shown to support cross-transmission of methicillin-resistant Staphylococcus aureus [4]. Disinfecting gloves has been reported to significantly decrease catheter contamination and catheter-associated bloodstream infections [5]. Similarly, disinfecting gloves has reduced the incidence of methicillin-resistant S. aureus [6]. As a result, in their excellent review, Kampf and Lemmen [7] emphasized promoting disinfecting gloves with an alcohol-based solution, which might result in a significant reduction of cross-transmission. These authors concluded that disinfecting gloves is as efficient as hand disinfection for alcohol-sensitive microorganisms and suggested that this practice be promoted.
In the search for an alternative solution, and to complete the experimental effectiveness of glove disinfection with an alcohol-based rub reported in the literature, we decided to evaluate the effectiveness of the alcohol-based disinfection of gloves in clinical practice during routine care.
Materials and methods
We performed this experimental study in an infectious disease ward. During the study period (March 2019), 13 HCWs of the ward were followed for 40 nursing care visits. All provided informed consent, which constituted our sole inclusion criterion. Care was provided by nurses and assistant nurses in 22 and 18 cases. One of the researchers (AV) followed HCWs during routine nursing care in an infectious disease ward. Swabs (transwab M40 compliant; Medical Wire and Equipment, Corsham, UK) were taken from the most contaminated part of both hands at T0 (before wearing gloves), at T10 (after 10 minutes of nursing care) from both gloves, at T10A (just after the gloves were disinfected for 30 seconds with a bedside disposable hydroalcoholic solution with 70% ethanol or isopropyl alcohol) and when possible at T20 and T20A. Samples were cultivated on chocolate agar (bioMérieux, Marcy l’Etoile, France) and incubated for 48 to 72 hours at 37°C. Cultured microorganisms were identified by matrix-assisted desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) (Bruker Daltonics, Bremen, Germany) as previously reported [8].
Results
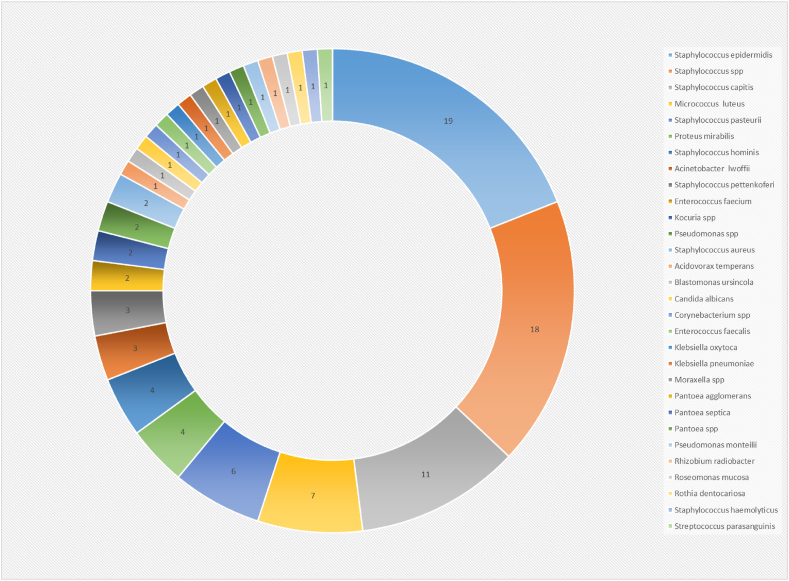
During the study period, 13 HCWs were followed for 40 nursing care visits. The care was provided by nurses and assistant nurses in 22 and 18 cases respectively. We collected samples 40 times, with two samples collected at times T0, T10 and T10A and ten supplementary samples collected at T20. These 250 samples were cultured, yielding 100 microorganisms that were identified by 750-peptide spectra provided by MALDI-TOF (Fig. 1).
Fig. 1.
Microorganisms cultured from hand and gloves of healthcare workers and identified by matrix-assisted desorption ionization–time of flight mass spectrometry (MALDI-TOF MS). Number of each microorganism is provided.
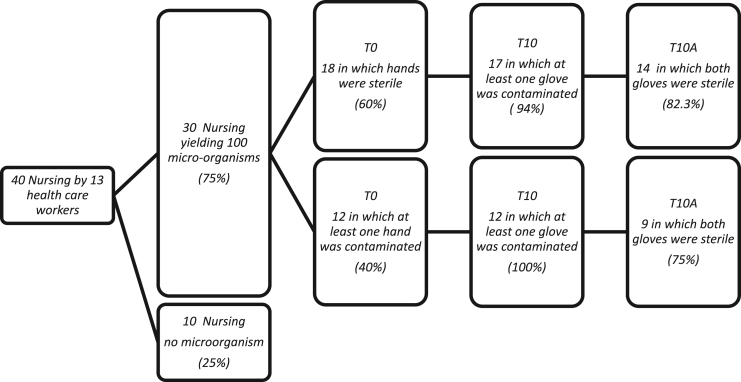
At T0, among the 40 nursing care visits, no microorganism was recovered in ten (25%), and at least one sample was recovered in 30 (75%) of 40 visits (Fig. 2). In 12 (40%) of 30 nursing care visits, at least one hand yielded one microorganism. Among them, two (6.6%) of 30 were identified as a pathogenic agent such as Acinetobacter lwoffii, Pseudomonas putida or Proteus mirabilis, meaning that HCWs' hands were contaminated by pathogenic bacteria before providing care to their patients. In four situations, the same bacteria that were recovered on the nurses' hands were also recovered at T10 on the gloves, suggesting possible cross-contamination of the gloves by the caregivers' hands (two Staphylococcus pasteuri; one each Staphylococcus epidermidis and Micrococcus luteus).
Fig. 2.
Microorganisms on nurses' hands and gloves. Samples were collected 40 times: time T0 (before wearing gloves), T10 (after 10 minutes of nursing care) and T10A (just after gloves were disinfected for 30 seconds with bedside disposable hydroalcoholic solution).
At T10, among the 18 nursing care visits for which both hands were sterile at T0, 17 (94%) of 18 had at least one contaminated glove, and five (29.4%) of 17 were contaminated by pathogenic Enterococcus faecium (n = 3), P. mirabilis (n = 1) and A. lwoffii (n = 1), suggesting that during the first 10 minutes of nursing care, a third of the HCWs contaminated at least one of their gloves with pathogenic bacteria, mostly enterobacteria, from the digestive tract. Among 12 nursing care visits for which a hand was contaminated at T0, all 12 were contaminated at T10.
Finally, in the first 10 minutes of nursing care, 29 (72.5%) of 40 HCWs had at least one glove contaminated. Disinfection of the gloves with a hydroalcoholic solution for 30 seconds sterilized both gloves in 79.3% (23/29) of cases. No difference was found between nurses and assistant nurses in the ratio of glove contamination or in the efficacy of alcohol-based rubs.
Discussion
In this study, 70% (28/40) of HCWs had both hands free of microorganism before coming into contact with patients, which likely reflects the specificity of this ward in which hand hygiene is regularly promoted [9]. Our average hand hygiene compliance rate, as measured by our automated surveillance system (last 6 months), is 35%; one of the explanations for this result is the overuse and misuse of gloves, as revealed by a video survey. Gloves should be used only in case of contact with dirty matter. This situation during nursing should be anticipated; nurses who prefer to wear gloves in any circumstances should be challenged [1].
It is unrealistic to believe that campaigns promoting better use of gloves will be more effective than promoting hand hygiene. Some authors, among them nurse practitioners, suggested disinfecting gloves as an alternative, and several experimental studies have supported the effectiveness of disinfecting gloves [10,11]. We showed that glove disinfection with hydroalcoholic solution is efficient in 79.3% of cases. Although the disinfection rate in experimental studies is higher than that reported here, the experimental context, such as the bacterial loads and disinfection protocols used in these studies, is not transferrable to clinical practice and does not take into consideration the quality of hand-rub practice during care [7,[12], [13], [14], [15]]. Our data only reflect practice in our ward; larger observational studies are needed to confirm the feasibility of such an alternative practice.
Compliance with hand hygiene was reported to be impaired by wearing gloves [16]. It has been recently reported that disinfecting gloved hands significantly improved compliance with hand hygiene, from 31% to 65% [17]. In addition to the growing body of literature on the effectiveness of glove disinfection with hydroalcoholic solution, our data convinced us, as well as our colleagues [7,17], that regular disinfection of gloves during care visits might be an alternative to avoid glove misuse and will be more easily accepted by HCWs.
Conclusions
In routine care, disinfection with hydroalcoholic solution is a feasible and efficient way to decontaminate gloves, which suggests that cross-transmission to the environment and patients can be lowered by using this method.
Conflict of interest
None declared.
Acknowledgements
The authors thank the HCWs of the medical unit for their investment and participation in this study. English-language editing services were provided by cookietrad@gmail.com. Funded in part by ANR-15-CE36-0004-01 entitled MediHandTrace (MHT) and Agence Nationale de la Recherche (ANR), IHU Mediterranée Infection 10-IAHU-03.
References
- 1.Boudjema S., Tarantini C., Peretti-Watel P., Brouqui P. Merging video coaching and an anthropologic approach to understand health care provider behavior toward hand hygiene protocols. Am J Infect Contr. 2017;45:487–491. doi: 10.1016/j.ajic.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) 15 January 2009. WHO guidelines on hand hygiene in health care.https://www.who.int/publications/i/item/9789241597906 Available at: [Google Scholar]
- 3.Chau J.P., Thompson D.R., Twinn S., Lee D.T., Pang S.W. An evaluation of hospital hand hygiene practice and glove use in Hong Kong. J Clin Nurs. 2011;20:1319–1328. doi: 10.1111/j.1365-2702.2010.03586.x. [DOI] [PubMed] [Google Scholar]
- 4.McBryde E.S., Bradley L.C., Whitby M., McElwain D.L. An investigation of contact transmission of methicillin-resistant Staphylococcus aureus. J Hosp Infect. 2004;58:104–108. doi: 10.1016/j.jhin.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Kocent H., Corke C., Alajeel A., Graves S. Washing of gloved hands in antiseptic solution prior to central venous line insertion reduces contamination. Anaesth Intensive Care. 2002;30:338–340. doi: 10.1177/0310057X0203000312. [DOI] [PubMed] [Google Scholar]
- 6.Matsumoto K., Shigemi A., Yaji K., Shimodozono Y., Takeda Y., Ikawa K. Reduction in the incidence of MRSA with use of alcohol-based hand rub solutions and gloves. J Infect Chemother. 2012;18:269–271. doi: 10.1007/s10156-011-0291-5. [DOI] [PubMed] [Google Scholar]
- 7.Kampf G., Lemmen S. Disinfection of gloved hands for multiple activities with indicated glove use on the same patient. J Hosp Infect. 2017;97:3–10. doi: 10.1016/j.jhin.2017.06.021. [DOI] [PubMed] [Google Scholar]
- 8.Seng P., Drancourt M., Gouriet F., La S.B., Fournier P.E., Rolain J.M. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clin Infect Dis. 2009;49:543–551. doi: 10.1086/600885. [DOI] [PubMed] [Google Scholar]
- 9.Dufour J.C., Reynier P., Boudjema S., Soto A.A., Giorgi R., Brouqui P. Evaluation of hand hygiene compliance and associated factors with a radio-frequency-identification–based real-time continuous automated monitoring system. J Hosp Infect. 2017;95:344–351. doi: 10.1016/j.jhin.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Assadian O., Humphreys P.N., Ousey K.J. Disinfection of artificially contaminated gloved hands reduces transmission of Staphylococcus epidermidis to catheter valves. J Hosp Infect. 2018;100:e57–e59. doi: 10.1016/j.jhin.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Newsom S.W., Rowland C. Application of the hygienic hand-disinfection test to the gloved hand. J Hosp Infect. 1989;14:245–247. doi: 10.1016/0195-6701(89)90041-8. [DOI] [PubMed] [Google Scholar]
- 12.Pitten F.A., Muller P., Heeg P., Kramer A. [The efficacy of repeated disinfection of disposable gloves during usage] Zentralbl Hyg Umweltmed. 1999;201:555–562. [PubMed] [Google Scholar]
- 13.Janota J., Šebková S., Višňovská M., Kudláčková J., Hamplová D., Zach J. Hand hygiene with alcohol hand rub and gloves reduces the incidence of late onset sepsis in preterm neonates. Acta Paediatr. 2014;103:1053–1056. doi: 10.1111/apa.12731. [DOI] [PubMed] [Google Scholar]
- 14.Ng P.C., Wong H.L., Lyon D.J., So K.W., Liu F., Lam R.K.Y. Combined use of alcohol hand rub and gloves reduces the incidence of late onset infection in very low birthweight infants. Arch Dis Child Fetal Neonatal. 2004;89:F336–F340. doi: 10.1136/adc.2003.031104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scheithauer S., Häfner H., Seef R., Seef S., Hilgers R.D., Lemmen S. Disinfection of gloves: feasible, but pay attention to the disinfectant/glove combination. J Hosp Infect. 2016;94:268–2672.1. doi: 10.1016/j.jhin.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Florea O., Dufour J.-C., Magnin C., Brouqui P., Boudjema S. Improving health care workers compliance with traceability by recording the nursing process at the point of care using a personal digital assistant with a barcode. J Nurs Care. 2020;9:500. [Google Scholar]
- 17.Fehling P., Hasenkamp J., Unkel S., Thalmann I., Hornig S., Trümper L. Effect of gloved hand disinfection on hand hygiene before infection-prone procedures on a stem cell ward. J Hosp Infect. 2019;103:321–327. doi: 10.1016/j.jhin.2019.06.004. [DOI] [PubMed] [Google Scholar]