Abstract
AIM
To investigate the distribution of intraocular pressure (IOP) and its relationship with refractive error and other factors in university students from Anyang, China.
METHODS
A university-based study was conducted. Subjects were invited to complete ophthalmic examinations, including visual acuity, noncontact tonometry (NCT), cycloplegic autorefraction, and ocular biometry. Univariable and multivariable analyses were used to evaluate the associations between IOP and other factors. Only data from right eyes were used in analysis.
RESULTS
A total of 7720 subjects aged 16 to 26 years old were included, and 2834 (36.4%) of the participants were male. The mean IOP of the right eye for all subjects was 15.52±3.20 mm Hg (95%CI: 15.45, 15.59). Using multivariate linear regression analysis, IOP was found to correlate significantly with younger age (P<0.001; standardized regression coefficient β, -0.061; regression coefficient β, -0.139; 95%CI: -0.18, -0.09), higher myopic refractive error (P=0.044; standardized β, -0.060; regression coefficient β, -0.770; 95%CI: -0.15, -0.002), higher central corneal thickness (P<0.001; standardized β, 0.450; regression coefficient β, 0.044; 95%CI: 0.04, 0.05), and shorter axial length (AL; P<0.001; standardized β, -0.061; regression coefficient β, -0.163; 95%CI: -0.25, -0.07).
CONCLUSION
This study described the normal distribution of IOP. In Chinese university students aged 16-26y, higher IOP is associated with younger age, higher myopic refractive error, higher thickness of the central cornea, and shorter AL.
Keywords: intraocular pressure, refractive errors, epidemiology, university students
INTRODUCTION
Intraocular pressure (IOP) is an important ocular parameter. High IOP is the most significant and treatable risk factor for the occurrence and development of glaucoma[1]. Since epidemiologic data are necessary for reasonable screening projects and treatment services, a number of comprehensive studies of IOP have been conducted in populations and schools[2]–[5]. However, the results vary by age and ethnicity. Compared with those in children and adults older than 40y[2]–[6], there have been few large-scale epidemiologic studies on the distribution of IOP in young adult populations aged approximately 20y. In addition, IOP has long been the mechanism of myopia development[7]. Most previous studies conducted in this age group included a small sample size or did not conduct cycloplegic refraction to evaluate the distribution of IOP and its relationship with refractive errors[2],[8].
Myopia is a major public health issue worldwide; it is the main cause of correctable visual impairment[9] and has been proven to be a significant cause of open angle glaucoma[10]. In cross-sectional studies, myopia was an independent risk factor for high IOP[8]. However, the relationship between refractive error and IOP is still controversial. A study reported that refractive error is negatively correlated with IOP[11]. A prevalence of myopia over 80% was found in Central Chinese university students. There is a relative paucity of information on the association of IOP in adult populations with a high myopia prevalence.
It has been reported that IOP is related to factors such as the central corneal thickness (CCT), corneal radius (CR), axial length (AL) and systemic factors, including age and blood pressure[2]–[5]. However, other reports have not found any relationship between IOP and age[3],[6], gender[3],[6], height, weight[3],[6] or even AL[2]. These associations are also inconsistent among different races. Thus, it is necessary to further explore the factors related to IOP in young Chinese adults.
Considering these differences, it is necessary to research the distribution of IOP and its related variables among young adults. To the best of our knowledge, this is the first large-scale study in mainland China to report the IOP distribution of university students. Our study focused on the distribution of IOP and its association with population characteristics and ocular parameters among college students.
SUBJECTS AND METHODS
Ethical Approval
The study was approved by the Ethics Committee and Institutional Review Board of Beijing Tongren Hospital, Capital Medical University. Subjects gave written informed consent, and this study adhered to the principles of the Declaration of Helsinki.
Study Design and Population
This university-based, cross-sectional study on ocular diseases in undergraduate students from Anyang was named the Anyang University Students Eye Study (AUSES). We recruited subjects from two public and comprehensive universities in Anyang. This study adopted the method of random cluster sampling, based on grade, enrolling first-year students to third-year students as participants. Students were admitted to these universities through the national college entrance examination. In short, 7971 students in years 1 to 3 were enrolled in the AUSES at these two universities. Students with systemic disease, eye disease or eye injury were excluded.
Study Protocols and Examination Methods
Students received ocular examination at the university clinic, including visual acuity, cycloplegic refraction, IOP, and ocular biometry. In addition, a detailed questionnaire was administered to collect the subjects' information, such as age and gender.
The IOP of both eyes was obtained by a noncontact tonometer (NCT; Havitz, HNT-7000, Gunpo, Republic of Korea). Each eye was measured three times, and the mean IOP was calculated. We used a Lenstar LS900 (Haag-Streit Koeniz, Switzerland) to measure ocular biometric parameters, including AL, CCT, keratometry power (K), anterior chamber depth (AD), and lens thickness (LT). Five repeated measurements were taken and averaged. Corneal radius (CR) was extracted from the K value using the formula CR (mm)=1000×0.3375/K (D). The AL to corneal radius (AL/CR) ratio was calculated with both AL and CR expressed in millimeters.
Cycloplegic refraction was measured with an autorefractor (HRK-7000A, HUVITZ, South Korea). Three autorefraction readings were taken, and the average was recorded. Each participant was first administered one drop of 1% cyclopentolate (Alcon), followed by one drop of Mydrin P (tropicamide 0.5%, phenylephrine HCl 0.5%; Santen Pharmaceutical, Shiga, Japan) and one drop of cyclopentolate after a 5-minute interval[12]. Thirty minutes after the last drop, if the pupil size was <6.0 mm or the pupillary light reflex was still present, a third drop of cyclopentolate was administered, and the examination was repeated after 15min.
Definitions
The spherical equivalent (SE) was computed by the formula of the algebraic sum of the dioptric powers of the sphere and half of the cylinder (sphere+0.5×cylinder). Hyperopia, high myopia, and myopia were defined as ≥+2.0 D, ≤-6.0 D and ≤-0.5 D, respectively[13]. Myopia was classified as high (SE≤-6.0 D), moderate (-6.0 D<SE≤-3.0 D) or low (-3.0 D<SE≤-0.5 D)[14].
Statistical Analysis
Two researchers entered the data into the Epidata software 3.1 database (The Epidata Association, Odense, Denmark). We used SAS software (version 9.4, SAS Inc, Cary, North Carolina, USA) to clean, logically check, merge, and analyze the data. The software package SPSS for Windows (version 22.0, IBM-SPSS, Chicago, IL, USA) was used for statistical analysis.
Due to the high correlation between the IOPs of the right and left eyes (Pearson's correlation coefficient r=0.73, P<0.001), the data from the right eyes were used for analysis. Continuous variables were expressed as mean±SD. We used χ2 tests to compare categorical variables between different groups. Independent-sample t tests and analysis of variance (ANOVA) were applied to compare the different ages and genders in the included and excluded groups. We evaluated the relationships between IOP and other ocular and systemic parameters in univariate models. We reexamined the relationship between IOP and all parameters significantly related to IOP in the univariate analysis in the multivariate analysis. Two-sided P-values less than 0.05 were considered statistically significant at 95% confidence intervals (CI) level.
RESULTS
A total of 7971 students completed ophthalmologic examinations (response rate 82.1%). Furthermore, because there were only 73 students aged 16, 25, or 26y, they were excluded from this analysis. Finally, 7720 (79.5%) subjects were included for analysis. The mean age was 20.17±1.44y (median, 20y; range, 17 to 24y), with 63.6% (4886/7720) female participants. Table 1 describes the distribution and comparison of age and gender between the included and excluded participants, with no significant differences in these demographic parameters (P>0.05 for all).
Table 1. Comparison of subjects included in and excluded from data analyses.
| Variable | Excluded | Included | IOP, mm Hg (right eyes) |
IOP, mm Hg (left eyes) |
Mean intraocular difference in IOP, mm Hg absolute amount | Pa | ||||
| Mean±SD | 95%CI | Mean±SD | 95%CI | |||||||
| Age (y) | 0.562b | |||||||||
| 16 | 11 (4.4) | - | ||||||||
| 17 | - | 56 (0.7) | 15.57±3.31 | 14.69, 16.46 | 16.38±3.55 | 15.42, 17.33 | 0.804±1.81 | |||
| 18 | 18 (7.2) | 786 (10.2) | 16.17±3.22 | 15.95, 16.40 | 16.30±3.31 | 16.07, 16.53 | 0.131±2.31 | |||
| 19 | 45 (19.7) | 1933 (25.0) | 15.73±3.23 | 15.58, 15.87 | 16.03±3.27 | 15.89,1 6.18 | 0.308±2.41 | |||
| 20 | 55 (21.9) | 2041 (26.4) | 15.55±3.23 | 15.41, 15.69 | 15.89±3.16 | 15.75, 16.03 | 0.339±2.37 | |||
| 21 | 23 (9.2) | 1469 (19.0) | 15.25±3.08 | 15.09, 15.41 | 15.37±3.09 | 15.21, 15.53 | 0.116±2.31 | |||
| 22 | 20 (8.0) | 921 (11.9) | 15.10±3.11 | 14.90, 15.30 | 15.30±3.12 | 15.09, 15.50 | 0.199±2.28 | |||
| 23 | 8 (3.2) | 380 (4.9) | 15.25±3.19 | 14.93, 15.57 | 15.36±3.32 | 15.02, 15.69 | 0.108±2.37 | |||
| 24 | 2 (0.8) | 134 (1.7) | 14.98±3.26 | 14.42, 15.53 | 15.49±3.48 | 14.89, 16.08 | 0.507±2.49 | |||
| 25 | 45 (17.9) | - | ||||||||
| 26 | 24 (9.6) | - | ||||||||
| Gender | 0.055 | |||||||||
| M | 107 (42.6) | 2833 (36.7) | 15.58±3.26 | 15.46, 15.70 | 15.58±3.26 | 15.46, 15.70 | 0.252±2.42 | |||
| F | 144 (57.4) | 4886 (63.3) | 15.48±3.17 | 15.40, 15.57 | 15.48±3.17 | 15.40, 15.57 | 0.242±2.31 | |||
| All | 251 (100.0) | 7720 (100.0) | 15.52±3.20 | 15.52±3.20 | 0.246±2.35 | |||||
aχ2 test; bOnly for those age 17-24y.
n (%)
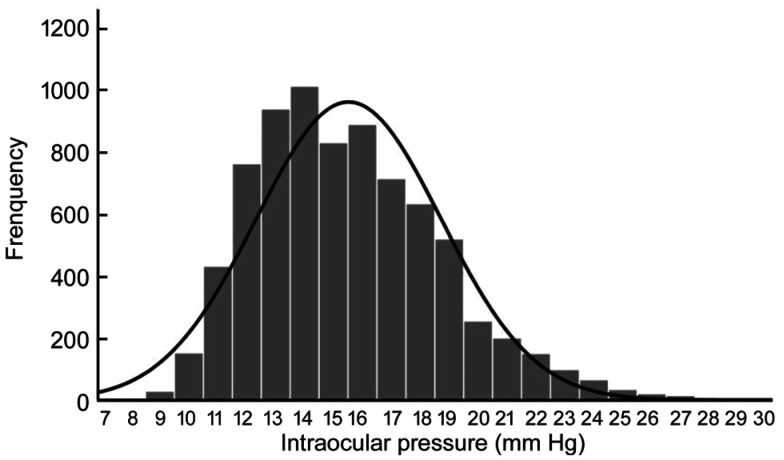
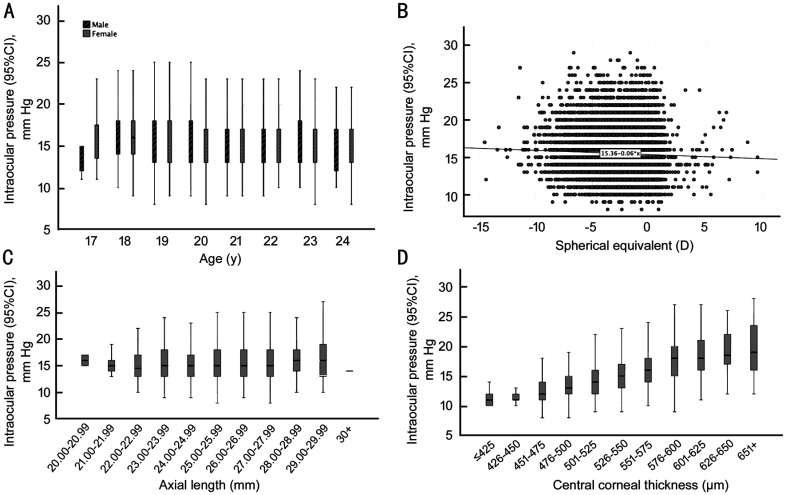
The mean IOP of the right eye for all subjects was 15.52±3.20 mm Hg (95%CI: 15.45, 15.59; median, 15.00; range, 8 to 29 mm Hg; Figure 1). The IOP was normally distributed (Figure 1). There was no statistical difference of mean IOP between male subjects (mean, 15.58±3.26 mm Hg; 95%CI: 15.46, 15.70; median, 15.00; range, 8 to 29 mm Hg) and female subjects (15.48±3.17 mm Hg; 95%CI: 15.40, 15.57; median, 15.00; range, 8 to 29 mm Hg; P=0.183). IOP initially increased from 17 to 18 years of age, followed by a decrease from 19 to 21 years of age, and then again increased from 22 to 23 years of age, after which it declined at the age of 24y. The IOP values stratified by age and gender are shown in Table 1. After stratified by age, the IOP of female subjects was higher than that of male subjects at ages 17, 18, and 24y, and male subjects had higher IOPs than female subjects at ages 19 to 23y (Figure 2).
Figure 1. Distribution of IOP of right eyes for all subjects in the Anyang University Students Eye Study.
Figures 2. Distribution of means and 95%CI for IOP of right eyes, stratified by different factors, in subjects enrolled in the Anyang University Students Eye Study.
A: Stratified by age and gender; B: Stratified by SE; C: Stratified by AL; D: Stratified by CCT.
The mean CCT, mean CR, mean AL, mean LT, mean AD, and mean AL/CR in the right eye were 539.84±33.02 µm, 7.70±0.27 mm, 24.78±1.20 mm, 3.47±0.178 mm, 3.23±0.248 mm, and 3.22±0.15 in right eyes, respectively. With increasing AL, IOP decreased and then increased, presenting a U-shaped relationship in this study (Figure 2). With increasing CCT, IOP increased gradually (Figure 2).
The association between IOP and participants parameters using univariate analyses is reported in Table 2. The univariate analysis showed that IOP was significantly related to age (P<0.05; β, -0.093; 95%CI, -0.26, -0.16), SE (P<0.05; β, -0.043; 95%CI, -0.09, -0.03), CCT (P<0.05; β, 0.447; 95%CI, 0.04, 0.05), AD (P<0.05; β, -0.039; 95%CI, -0.79, -0.21), AL (P<0.05; β, 0.028; 95%CI, 0.01,0.13) and AL/CR (P<0.05; β, 0.034; 95%CI; 0.23, 1.16). However, Table 2 shows that IOP was not significantly associated with gender, LT or CR.
Table 2. Univariate analysis and multivariate analysis of associations between IOP and nonocular and ocular parameters.
| Statistical analysis | n | β | 95%CI | P | |||
| Univariate models | |||||||
| Male/female | 7720 | -0.15 | -0.25, 0.05 | 0.183 | |||
| Age, y | 7720 | -0.093 | -0.26, -0.16 | 0.000 | |||
| SE, D | 7720 | -0.043 | -0.09, -0.03 | 0.000 | |||
| CCT, µm | 7567 | 0.447 | 0.04, 0.05 | 0.000 | |||
| AD, mm | 7459 | -0.039 | -0.79, -0.21 | 0.001 | |||
| LT, mm | 7268 | 0.977 | -0.21, 0.62 | 0.329 | |||
| AL, mm | 7567 | 0.028 | 0.01, 0.13 | 0.016 | |||
| CR, mm | 7720 | -0.009 | -0.37, 0.15 | 0.412 | |||
| AL/CR | 7567 | 0.034 | 0.23, 1.16 | 0.003 | |||
| Multivariate model | |||||||
| Age, y | 7720 | -0.061 | -0.18, -0.09 | 0.000 | |||
| SE, D | 7720 | -0.060 | -0.15, -0.002 | 0.044 | |||
| CCT, µm | 7567 | 0.450 | 0.04, 0.05 | 0.000 | |||
| AL, mm | 7567 | -0.061 | -0.25, 0.07 | 0.000 | |||
| AD, mm | 7459 | 0.005 | -0.28, 0.41 | 0.710 | |||
| AL/CR | 7567 | 0.050 | -0.13, 2.19 | 0.081 | |||
SE: Spherical equivalent; CCT: Central cornea thickness; AD: Anterior chamber depth; LT: Lens thickness; CR: Corneal radius; AL: Axial length.
To eliminate nonsignificant factors, multivariate linear regression analysis was conducted. IOP was no longer associated with AD or AL/CR (Table 2). Higher IOP was significantly related to younger age, higher myopic refractive error, higher CCT, and shorter AL.
DISCUSSION
In Chinese university students, there was an M-shaped relationship between IOP and age. The mean IOP for all subjects, male subjects and female subjects was 15.52±3.20 mm Hg, 15.58±3.26 mm Hg and 15.48±3.17 mm Hg, respectively. Higher IOP was significantly associated with younger age, higher myopic diopter, higher CCT and shorter AL. Previous studies on the distribution of IOP have mainly focused on children and adults over the age of 40y[2]–[6]. In addition, there were other population-based and university-based samples, but these studies did not conduct cycloplegic refraction or recruited only a small sample to investigate the distribution of IOP and its relationship with refractive errors[2],[8]. To the best of our knowledge, this was among the first large-sample study, focusing on the distribution of IOP values and its relationship with cycloplegic refraction and other factors in undergraduate students in mainland China, which may provide new insight into IOP.
The mean IOP in our study was higher than that in Korean young adults and Latino adults (>40y)[2],[4],[8]. Compared with the mean IOP of children in Turkey and British adults (>40y), the mean IOP of undergraduate students in China was lower[5]–[6]. The differences in age and race between different studies may also be important reasons for these differences. Some differences may be related to the measurement methods; NCT, Goldman applanation tonometry and handheld tonometry were used in different studies.
In the Shandong Children Eye study, which included children aged 10 years old, the mean IOP was 17.6±2.7 mm Hg. The mean IOP of Chinese children was higher than that of Chinese university students. Compared to older adults in northern China, Xu et al[15] found that the mean IOP was 16.1±3.4 mm Hg in adults over the age of 40. In different studies of Chinese adults, the mean IOP reported varied from 13.53 mm Hg to 16.1 mm Hg[3],[15]. In general, IOP is more consistent in adults, may be higher in children, decreases with age, and then stabilizes in adults. We hypothesized that eyeball growth and scleral elasticity lead to high IOP in children, and high blood pressure and obesity might be the causes of high IOP in the higher age groups. To determine the exact mechanism, further stratified investigation by age and other systemic factors is required.
In our research, we found a relationship between higher IOP and younger age in university students. This result is consistent with the findings of previous studies. In Asian studies, an association between higher IOP and younger age was reported[16]–[17]. In Japanese adults over the age of 40y, the mean IOP was 14.5 mm Hg, and IOP was negatively associated with age[18]. However, in Caucasians, there was a positive correlation between IOP and age. The increasing trend in IOP with age is more obvious in people aged 40 years or older. This may be associated with other parameters, such as blood pressure and/or body mass index (BMI)[19].
The main finding in our research was that a correlation between higher IOP and a larger myopic diopter was found in university students. Information is relatively scarce on the correlation between IOP and myopic diopter in young adults. The Tajimi study[18] reported the same result. However, this finding is not consistent with findings from other studies. The mechanism of myopia and elevated IOP is still unclear. This association may occur via two mechanisms: the effect of myopia on the true IOP and the effect of myopia on the ocular or corneal bioproperties that affect the measurement of true IOP. This positive association between myopic diopter and IOP emphasizes the necessity of glaucoma monitoring in the myopic population[12].
The association between higher IOP and shorter AL may have important significance. Some studies agreed on the association between higher IOP and shorter AL[4],[20]. One possible reason for this association is related to differences in organizational compliance. There are differences in the mechanical strain of the sclera, especially the tensile strain of the posterior sclera, which is higher than that of the adjacent mid-peripheral sclera[21]. The sclera tissue has certain compliance. Below a certain degree, there is a negative correlation between IOP and AL, and above a certain threshold, there is a positive correlation between IOP and AL[5].
Higher IOP is associated with thicker CCT[22]. Previous investigations have reported that CCT is also an important factor[23]. A Chinese population-based study showed a positive relationship between IOP and CCT[24]. In our study, the association between CCT and IOP was the same as in previous studies.
The advantages of our research lie in the large sample size. Meanwhile, this study was first large-scale investigation of IOP values in undergraduate students in mainland China. Potential limitations of this research should be discussed. First, this is a university-based study, not a population-based study. Second, the use of NCT instead of Goldmann applanation tonometry may have led to a higher reading of IOP[25].
In conclusion, the mean IOP of undergraduate students was 15.52±3.20 mm Hg in Central China. This study discovered that higher IOP was significantly associated with younger age, higher myopic refractive error, higher CCT, and shorter AL.
Acknowledgments
Conflicts of Interest: Ma DD, None; Wei SF, None; Sun YY, None; Li SM, None; An WZ, None; Hu JP, None; Cao K, None; Yang XH, None; Lin CX, None; Guo JY, None; Li H, None; Fu J, None; Wang NL, None.
REFERENCES
- 1.Baneke AJ, Aubry J, Viswanathan AC, Plant GT. The role of intracranial pressure in glaucoma and therapeutic implications. Eye (Lond) 2020;34(1):178–191. doi: 10.1038/s41433-019-0681-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim MJ, Park KH, Kim CY, Jeoung JW, Kim SH. The distribution of intraocular pressure and associated systemic factors in a Korean population: the Korea National Health and Nutrition Examination Survey. Acta Ophthalmol. 2014;92(7):e507–e513. doi: 10.1111/aos.12327. [DOI] [PubMed] [Google Scholar]
- 3.Han X, Yang T, Zhang J, Yu S, Guo X, Yan W, Hu Y, He M. Longitudinal changes in intraocular pressure and association with systemic factors and refractive error: Lingtou Eye Cohort Study. BMJ Open. 2018;8(2):e019416. doi: 10.1136/bmjopen-2017-019416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Memarzadeh F, Ying-Lai M, Azen SP, Varma R, Los Angeles Latino Eye Study Group Associations with intraocular pressure in latinos: the Los Angeles Latino Eye Study. Am J Ophthalmol. 2008;146(1):69–76. doi: 10.1016/j.ajo.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan MP, Grossi CM, Khawaja AP, Yip JL, Khaw KT, Patel PJ, Khaw PT, Morgan JE, Vernon SA, Foster PJ, UK Biobank Eye and Vision Consortium Associations with intraocular pressure in a large cohort: results from the UK Biobank. Ophthalmology. 2016;123(4):771–782. doi: 10.1016/j.ophtha.2015.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yildirim N, Sahin A, Basmak H, Bal C. Effect of central corneal thickness and radius of the corneal curvature on intraocular pressure measured with the Tono-Pen and noncontact tonometer in healthy schoolchildren. J Pediatr Ophthalmol Strabismus. 2007;44(4):216–222. doi: 10.3928/01913913-20070701-02. [DOI] [PubMed] [Google Scholar]
- 7.Quinn GE, Berlin JA, Young TL, Ziylan S, Stone RA. Association of intraocular pressure and myopia in children. Ophthalmology. 1995;102(2):180–185. doi: 10.1016/s0161-6420(95)31038-x. [DOI] [PubMed] [Google Scholar]
- 8.Choi JA, Han K, Park YM, Park CK. Age-related association of refractive error with intraocular pressure in the Korea National Health and Nutrition Examination Survey. PLoS One. 2014;9(11):e111879. doi: 10.1371/journal.pone.0111879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739–1748. doi: 10.1016/S0140-6736(12)60272-4. [DOI] [PubMed] [Google Scholar]
- 10.Dhingra N, Manoharan R, Gill S, Nagar M. Peripapillary schisis in open-angle glaucoma. Eye (Lond) 2017;31(3):499–502. doi: 10.1038/eye.2016.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong TY, Klein BE, Klein R, Knudtson M, Lee KE. Refractive errors, intraocular pressure, and glaucoma in a white population. Ophthalmology. 2003;110(1):211–217. doi: 10.1016/s0161-6420(02)01260-5. [DOI] [PubMed] [Google Scholar]
- 12.Sun YY, Wei SF, Li SM, et al. Cycloplegic refraction by 1% cyclopentolate in young adults: is it the gold standard? The Anyang University Students Eye Study (AUSES) Br J Ophthalmol. 2018:bjophthalmol-bjophtha2018-312199. doi: 10.1136/bjophthalmol-2018-312199. [DOI] [PubMed] [Google Scholar]
- 13.Li SM, Liu LR, Li SY, et al. Anyang Childhood Eye Study Group Design, methodology and baseline data of a school-based cohort study in Central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol. 2013;20(6):348–359. doi: 10.3109/09286586.2013.842596. [DOI] [PubMed] [Google Scholar]
- 14.Tai ELM, Ling JL, Gan EH, Adil H, Wan-Hazabbah WH. Comparison of peripapillary retinal nerve fiber layer thickness between myopia severity groups and controls. Int J Ophthalmol. 2018;11(2):274–278. doi: 10.18240/ijo.2018.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu L, Li J, Zheng Y, Cui T, Zhu J, Ma K, Yang H, Ma B, Jonas JB. Intraocular pressure in Northern China in an urban and rural population: the Beijing eye study. Am J Ophthalmol. 2005;140(5):913–915. doi: 10.1016/j.ajo.2005.04.050. [DOI] [PubMed] [Google Scholar]
- 16.Nomura H, Ando F, Niino N, Shimokata H, Miyake Y. The relationship between age and intraocular pressure in a Japanese population: the influence of central corneal thickness. Curr Eye Res. 2002;24(2):81–85. doi: 10.1076/ceyr.24.2.81.8161. [DOI] [PubMed] [Google Scholar]
- 17.Cui Y, Yang XH, Zhang GR, Guo HK, Zhang M, Zhang LX, Zeng J, Liu QY, Zhang L, Meng QL. Intraocular pressure in general and diabetic populations from Southern China: the Dongguan Eye Study. Invest Ophthalmol Vis Sci. 2019;60(2):761–769. doi: 10.1167/iovs.18-25247. [DOI] [PubMed] [Google Scholar]
- 18.Kawase K, Tomidokoro A, Araie M, Iwase A, Yamamoto T, Tajimi Study Group, Japan Glaucoma Society Ocular and systemic factors related to intraocular pressure in Japanese adults: the Tajimi study. Br J Ophthalmol. 2008;92(9):1175–1179. doi: 10.1136/bjo.2007.128819. [DOI] [PubMed] [Google Scholar]
- 19.McLeod SD, West SK, Quigley HA, Fozard JL. A longitudinal study of the relationship between intraocular and blood pressures. Invest Ophthalmol Vis Sci. 1990;31(11):2361–2366. [PubMed] [Google Scholar]
- 20.Tomoyose E, Higa A, Sakai H, Sawaguchi S, Iwase A, Tomidokoro A, Amano S, Araie M. Intraocular pressure and related systemic and ocular biometric factors in a population-based study in Japan: the Kumejima Study. Am J Ophthalmol. 2010;150(2):279–286. doi: 10.1016/j.ajo.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Fazio MA, Grytz R, Bruno L, Girard MJ, Gardiner S, Girkin CA, Downs JC. Regional variations in mechanical strain in the posterior human sclera. Invest Ophthalmol Vis Sci. 2012;53(9):5326–5333. doi: 10.1167/iovs.12-9668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ma YZ, Ma YP, Feng CL, Shen MQ, Yuan YZ. Ocular biometric parameters are associated with non-contact tonometry measured intraocular pressure in non-pathologic myopic patients. Int Ophthalmol. 2020;40(2):431–437. doi: 10.1007/s10792-019-01203-8. [DOI] [PubMed] [Google Scholar]
- 23.Rimayanti U, Kiuchi Y, Uemura S, Takenaka J, Mochizuki H, Kaneko M. Ocular surface displacement with and without contact lenses during non-contact tonometry. PLoS One. 2014;9(4):e96066. doi: 10.1371/journal.pone.0096066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baboolal SO, Smit DP. South African Eye Study (SAES): ethnic differences in central corneal thickness and intraocular pressure. Eye (Lond) 2018;32(4):749–756. doi: 10.1038/eye.2017.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ito K, Tawara A, Kubota T, Harada Y. IOP measured by dynamic contour tonometry correlates with IOP measured by Goldmann applanation tonometry and non-contact tonometry in Japanese individuals. J Glaucoma. 2012;21(1):35–40. doi: 10.1097/IJG.0b013e31820275b4. [DOI] [PubMed] [Google Scholar]