Abstract
This article describes a program developed to improve the process of planned induction of labour and to reduce the rates of inappropriate induction. The setting is a tertiary-care maternity hospital in urban Vancouver, BC, in which 7000 deliveries take place annually. Approximately 65% of these can be considered primary care; the remainder are secondary- or tertiary-level cases. Continuous quality improvement (CQI) methods were used by a multidisciplinary team, which included nursing staff, physicians, health records personnel and a CQI facilitator. Interventions included the development of a new induction-booking process, clear criteria for induction, feedback to caregivers about changes and a peer review system to oversee and maintain improvement. The overall induction rate for the institution decreased, and this change has been maintained.
Induction of labour is indicated when the potential risks of continuing a pregnancy outweigh the benefits. At times this is very clear (e.g., when severe pre-eclampsia threatens the health of mother and baby);1,2 however, often the situation is not well defined and is influenced by the beliefs of individual caregivers.3,4,5,6,7,8 Elective nonmedically indicated inductions (i.e., for convenience) cannot be condoned because induction has been associated with increased risk for fetal distress, hyperstimulation of the uterus and cesarean section.1,2,3 Several guidelines have been proposed for the induction of labour.9,10,11
British Columbia's Women's Hospital and Health Centre is a 93-bed obstetrical facility in Vancouver, BC. With over 7000 births per year, it is the busiest maternity hospital in Canada. Delivery suite staff include 125 nurses, 36 obstetricians and 124 family physicians. Since 1996 family physicians have been able to initiate inductions for the indications of premature rupture of membranes (PROM) and post-term pregnancies; all other inductions required obstetrical consultation. Before this program was initiated the induction rate was 23%–25% for all births. Although there is little in the literature to indicate an appropriate institutional rate, these rates were thought to be too high in a setting where 65% of the patient population is described as low risk and where 66% of the inductions were for post-term pregnancies or when PROM was indicated.
Initial attempts by physician managers to decrease the induction rates produced minimal change. These efforts included an attempt to draft some guidelines for induction and a new booking form. However, the guidelines were unclear and were often ignored — physicians bypassed the booking system and directly approached nursing leaders to arrange for an induction. It was clear that another approach to the problem was required. As part of an overall initiative to reduce cesarean section rates at British Columbia's Women's Hospital and Health Centre,12 induction was identified as one of the processes that needed review. An audit revealed that 33% of patients induced for post-term pregnancies did not meet the criteria set by consensus in the institution (i.e., 41 weeks, 3 days). In addition, the booking system was inconsistently applied, key entry points were often bypassed, and there were delays that affected both patients and physicians.
To address the complex system issues we identified and involve all members of the team, we chose to use the continuous quality improvement (CQI) approach to initiate changes. We modelled the project on the work of Donald Berwick, who applied quality management to health care.13,14,15,16,17,18,19 It was felt that using this approach, the system problems could be reviewed, analyzed and improved by our multidisciplinary group. Changes would be based on data collected from our hospital and outcomes could be monitored.
Program description
In July of 1996 a multidisciplinary team led by a nurse perinatal clinical educator (B.B.) began using CQI methods to review the induction process. The objective of the project was to improve the process of labour induction and eliminate all inappropriate inductions. Team members included a nursing team leader, 2 nurse clinicians, 2 family practice physicians, an obstetrician, perinatalogist, obstetrical resident, clinical epidemiologist, CQI consultant and an information analyst from the Health Records Department. Patients who had labour induced were interviewed and their input was recorded. Medical staff were remunerated for their participation in the process with an honorarium, and nursing staff were paid for their attendance.
The team created a flow diagram to document the existing process and identified a “vital few” key areas to focus their strategies on. These included: (a) a lack of clear criteria for induction, (b) a lack of a well-defined booking process for induction, (c) little accountability in the system and (d) a need for communication and feedback to all caregivers in the system. The following improvements were undertaken.
Clear criteria for induction
After a review of the literature and the use of consensus strategies, 5 indications were identified as appropriate for induction. Clear criteria were established for post-term pregnancies, term PROMs, pregnancy-induced hypertension (PIH), fetal jeopardy and maternal disease.
Improved booking process
The booking process was further reviewed, and clear guidelines describing how inductions were to be booked were given to physicians. A new booking form was developed (available from the authors), and the new booking process and form were implemented in April, 1997.
Peer review system
A group of 4 physicians (3 obstetricians and 1 family physician) reviewed and approved each induction. This involved daily review of all booked inductions; those meeting the criteria were approved, and those that did not meet the criteria were refused and the physician was notified. Initially, there was some resistance to this review by physicians who were uneasy about having their “clinical judgements” and decisions questioned by another physician. However, this resistance decreased considerably when staff recognized that the criteria for induction had been established by a committee that included their peers and were based on the best evidence available in the literature. Nursing staff felt supported by the physician review process; previously, nursing team leaders had been given the task of “policing” the induction process, and this often placed them in conflict with physicians. Nursing team leaders are now gradually reassuming the role of induction approval, with the support of the revised process.
Communication and education regarding changes
During each step of the process, various methods of communication and feedback were established. Storyboards were posted in the labour and delivery units and in the staff lounge. Frequently asked questions were answered biweekly via email and were posted in the labour delivery area and in a communication book used by staff. The changes in the process were communicated in a hospital newsletter and at staff meetings, inservices and professional rounds. Information describing the new forms and processes was mailed to physicians who were given the opportunity to voice their opinions either in writing or at departmental rounds before the process was implemented. Once the changes were implemented, monthly induction rates were posted so staff members could see changes in rates. The new criteria and booking and peer review process were legitimized in a new institutional policy for induction.19
The primary outcome measure was overall rate of induction within the institution. Indications for induction were also tracked. In addition, newborn outcomes were reported for nulliparous women with singleton, term, cephalic presentation to identify any changes in adverse neonatal outcome rates (i.e., Apgar score less than 7 at 5 minutes, perinatal death or level II/level III nursery admissions). It was felt that caregivers needed to be reassured that changes in induction practices did not negatively affect outcomes.
Outcomes
Changes were implemented in April of 1997. Induction rates before and after are presented in Fig. 1. Rates are reported in 6-month blocks for 3 years before implementation and 28 months after. Induction rates were already declining before the project was initiated, possibly because of early efforts by physician managers to establish induction criteria. Rates continued to fall after the intervention and then levelled off. The lower induction rate has been maintained over the last 6 observation periods.
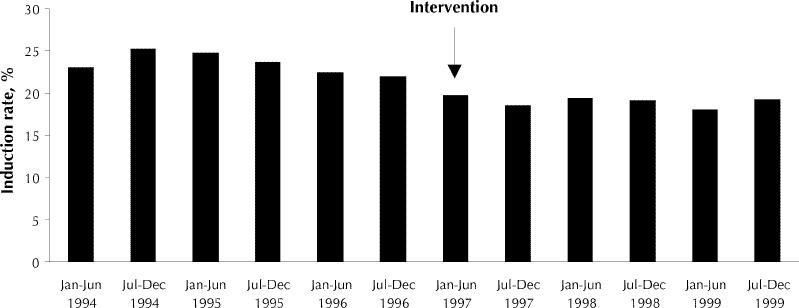
Fig. 1: Labour induction rates at British Columbia's Women's Hospital and Health Centre, 1994–1999. The continuous quality improvement and peer review program was implemented in April 1997.
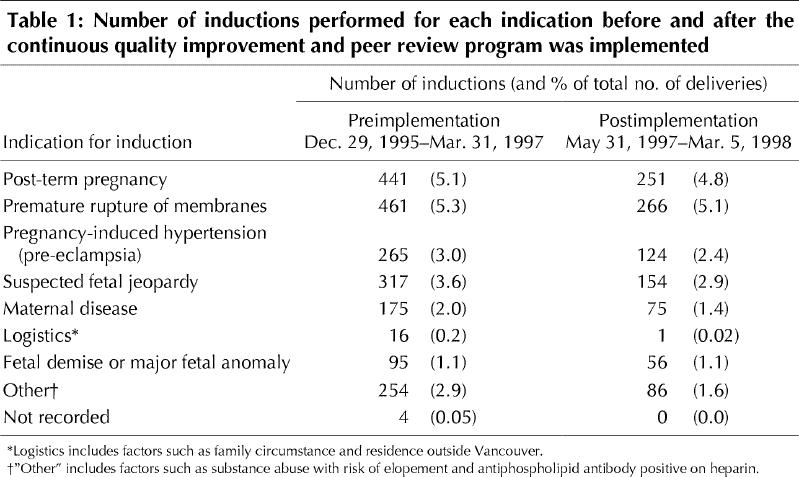
Induction rates declined for all indications for induction except fetal demise and major fetal anomaly (Table 1). There was no change in newborn outcomes for Apgar scores less than 7 at 5 minutes, perinatal deaths or level II/level III nursery admissions following implementation.
Table 1
Because of the peer review process, 100% of the inductions after the program was implemented met the criteria. The only exception occurred initially on weekends when there was no physician available to review cases; this number has decreased as nursing team leaders have become more comfortable with the criteria and the process.
Interpretation
Major system problems at our hospital included an ineffective booking system and unclear guidelines for when induction was appropriate. Using CQI methods and supported by our own data, we confirmed the problems, initiated changes and continue to monitor our progress. Continuous feedback to caregivers facilitated ongoing modification, which, in turn, allowed for increased flexibility and improvement within the framework of a large tertiary setting.
The inclusion of obstetricians, family physicians, perinatologists, nurses and patients ensured that all those involved had representation at the table when problems were identified and changes were planned. Previous hospital initiatives had left nursing staff feeling unsupported at times; this was avoided with this project. The physician peer review process, which made daily attendance on the unit by a reviewing physician mandatory, also enhanced support for nursing staff.
One of the limitations of the approach we chose to use is that it is a very time-consuming process. Numerous meetings were required to reach implementation. This represents a significant cost to the institution. Although it might be expedient to use some accelerated form of quality improvement using the literature and experience of other institutions, to be successful it is necessary to consider the “local” environment and its unique character.
In addition, such change requires ongoing maintenance; it was not enough to produce clear indications and a new booking process. It was critical to the success of this project that there were review and accountability built into the system, and the physician peer review process has facilitated this. In view of the current recognition of the limitations of the role of generic guidelines in effecting change, perhaps it is this aspect of our project that was the most critical. It is, however, impossible to precisely pinpoint the reasons for the changes observed.
We recommend that similar projects be undertaken at other institutions. In fact, this strategy is currently being used to address other patient care issues within our institution.
Conclusion
A CQI process with peer review, developed to improve the process of labour induction, led to the development of clear criteria for induction, a new booking form and a revised hospital induction policy. These changes have been associated with a sustained reduction in induction rates in our tertiary-care institution.
Footnotes
This article has been peer reviewed.
Acknowledgements: We thank the following people for their thoughtful support and input: the delivery suite nursing staff; Kim Shearer, Birthing Program Director; Selina Pope, Quality Improvement Coordinator; Dr. Barry Sanders, Obstetrical Consultant to the Low-Risk Birthing Program; David Thompson, Acting Director of Quality Improvement; Corrine Nishi and Donna Wong, Health Records Administrators; and Dr. Michael Klein, Director of the Family Health Program.
Funding was provided by British Columbia's Women's Health Executive.
Reprint requests to: Dr. Susan Harris, Medical Director, Birthing Program, British Columbia's Women's Hospital and Health Centre, 4500 Oak St., Vancouver BC V6H 3N1; fax 604 875-3197; sharris@cw.bc.ca
References
- 1.Bebbington MW, Dansereau J, Effer SB, Farquharson D, Galerneau F, Walker MPR, et al. Induction of labour: current concepts. Vancouver: BC Women's Hospital and Health Centre, Department of Obstetrics and Gynecology, Division of Maternal Fetal Medicine (a scope publication by Upjohn); 1996.
- 2.Walker MPR, Resnik R. Prolonged pregnancy, cervical ripening and induction of labour. In: Moore TR, Reiter RC, Rebar RW, Baker VV, editors. Gynecology & obstetrics: a longitudinal approach. New York: Churchill Livingstone; 1993. p. 541-59.
- 3.Hannah ME, Hannah WJ, Hallmark J, Hewson S, Milner R, Willan A. The Canadian multicentre post-term pregnancy trial. N Engl J Med 1992;326(24): 1587-92. [DOI] [PubMed]
- 4.Hannah ME, Ohlsson A, Farine D, Hewson SA, Hodnett ED, Myhr TL, et al. Induction of labor compared with expected management for prelabour rupture of membranes at term. TERMPROM Study Group. N Engl J Med 1996;334(16):1005-10. [DOI] [PubMed]
- 5.Hannah ME, Huh C, Hewson S, Hannah WJ. Post-term pregnancy: putting the merits of a policy of induction of labour into perspective. Birth 1996; 23(1):13-9. [DOI] [PubMed]
- 6.Duff P. Premature rupture of the membranes at term [editorial]. N Engl J Med 1996;334(16):1053-4. [DOI] [PubMed]
- 7.Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ. Do practice guidelines guide practice? N Engl J Med 1989;321(19):1306-11. [DOI] [PubMed]
- 8.David DA, Thomson MA, Oxman D, Haynes B. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA 1995;274(9):700-4. [DOI] [PubMed]
- 9.British Columbia Reproductive Care Program. Obstetric guideline 1: Induction of labour. Revised April, 1999. Available: www.rcp.gov.bc.ca/Master[1].OB1.Induction.April99.pdf
- 10.Society of Obstetricians and Gynecologists of Canada. SOGC Clinical practice guidelines. No. 57: Induction of labour. Ottawa: The Society; 1996. Available: sogc.medical.org/SOGCnet/sogc_docs/common/guide/pdfs/ps57.pdf
- 11.American College of Obstetricians and Gynecologists. Induction and augmentation of labor. Technical bulletin no. 125. Washington: The College; 1987.
- 12.British Columbia's Women's Hospital and Health Centre. The first births manual. Vancouver: The Hospital; 1998.
- 13.British Columbia's Children's Hospital. Quality for kids training manual. Vancouver: The Hospital; 1995.
- 14.Kritchevsky SB, Simmons BP. Continuous quality improvement; concepts and applications for physician care. JAMA 1991;266(13):1817-23. [DOI] [PubMed]
- 15.O'Malley S. Total quality now! Putting QJ on the fast track Qual Lett Healthc Lead 1997;9(11):2-10. [PubMed]
- 16.Berwick DM. Heal thyself or heal the system: Can doctors help to improve medical care? Qual Med Care J 1992;1(Suppl):S1-7.
- 17.Black ER, Weiss, KD, Erban S, Chulkin D. Innovations in patient care: changing clinical practice and improving quality. Jt Comm J Qual Improv 1995;21(8):376-93. [DOI] [PubMed]
- 18.Berwick DM, Godfrey AB, Roessner J. Curing health care: New strategies for quality improvement. San Francisco: Jossey-Bass Publishers; 1990.
- 19.British Columbia's Women's Hospital and Health Centre. Induction/augmentation of labour using oxytocin or prostaglandin E2: Policy C10 225. In: British Columbia's Women's Hospital and Health Centre policy and procedures manual. Fetal/Maternal/Newborn and Family Health Services. Vancouver: The Hospital; 1998.


