Abstract
Better understanding of the dynamics of the current US overdose epidemic may aid in the development of more effective prevention and control strategies. We analyzed records of 599,255 deaths from 1979 through 2016 from the National Vital Statistics System in which accidental drug poisoning was identified as the main cause of death. By examining all available data on accidental poisoning deaths back to 1979 and showing that the overall 38-year curve is exponential, we provide evidence that the current wave of opioid overdose deaths (due to prescription opioids, heroin, and fentanyl) may just be the latest manifestation of a more fundamental longer term process. The 38+ year smooth exponential curve of total US annual accidental drug poisoning deaths is a composite of multiple distinctive sub-epidemics of different drugs (primarily prescription opioids, heroin, methadone, synthetic opioids, cocaine, and methamphetamine), each with its own specific demographic and geographic characteristics.
One Sentence Summary:
USA overdose epidemic dynamics are changing
The epidemic of substance use disorders and drug overdose deaths in the U.S. is a growing public health crisis. Every day 174 people in the United States die from drug overdoses (1). Currently, opioids (including prescription opioids, heroin, and synthetic opioids such as fentanyl and its chemical analogs) are the main causes of overdose deaths in the U.S., leading the US Government to declare the opioid crisis to be a public health emergency (2).
Knowledge of the opioid epidemic has been mostly limited to scattered statistics that only reveal selected aspects of the epidemic, such as specific geographic regions, specific time periods and/or specific drugs. For example, a recent NCHS data brief shows that the Appalachian region and southwest region have overdose death rates statistically higher than the national rate (3). Similarly, a recent study has identified geospatial clusters of heroin related overdose deaths in 2000 in Southern California, and emerging later in New England, the Mid-Atlantic, and the Great Lakes region between 2013-2014 (4).
We lack a detailed analysis of the opioid epidemic in the context of the larger drug epidemic that reveals the complex and evolving dynamics of drug use in the United States (5). This manuscript examines mortality patterns of all accidental (unintentional) drug poisonings as reported through the US National Vital Statistics System from 1979 to 2016. We describe the overall pattern of drug overdose deaths in the US and reveal specific aspects of these deaths by drug, demography and geography; we refer to these patterns as sub-epidemics.
1. The overdose epidemic is a composite of multiple sub-epidemics
Annual mortality rates attributed to prescription opioids, heroin, methadone, synthetic opioids other than methadone, cocaine, methamphetamine, unspecified narcotics, and unspecified drugs are shown in Fig. 1 Drug classes are defined in the supplementary materials and Table S1 which sorts the drugs by their International Classification of Diseases (ICD) codes. Accidental drug poisoning trend analyses begin in 1979 with the ninth revision (ICD-9) due to comparability issues with that cause of death in earlier revisions. Similarly, analyses by drug and drug class begin in 1999 (with ICD-10) because those classifications are not comparable with ICD-9.
Fig. 1.
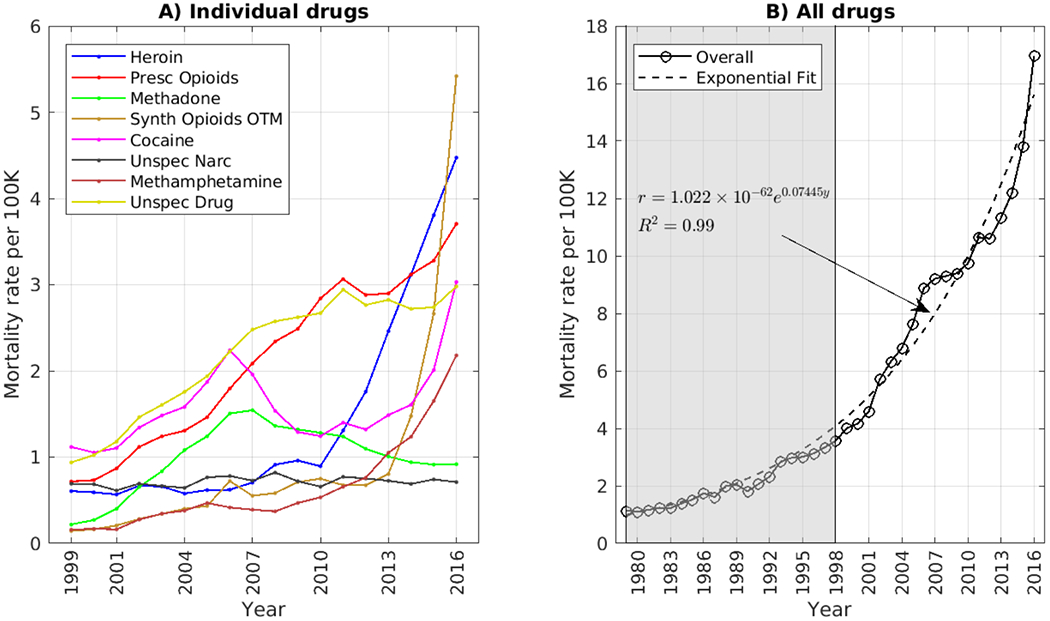
Mortality rates from unintentional drug overdoses for A) individual drugs, and B) all drugs. Detailed data from individual drugs are only available from 1999 to 2016, while additional data available since 1979 from all drugs [this area is greyed out]. The exponential equation and fit are shown for all drugs. r = overall mortality rate and y = year. [Synth Opioids OTM = Synthetic opioids other than methadone. This category includes fentanyl and its analogues].
Since 2010 the mortality curves for all drug types have been increasing, except for methadone and for unspecified drugs and narcotics. Each drug’s mortality curve shows some variability. For example, the mortality rate from prescription opioids decreased slightly in 2011 while the mortality rates from heroin and synthetic opioids have been rapidly increasing. These trends may be related because several epidemic interventions may have reduced the impact of prescription opioids around 2010, including the reformulation of OxyContin in 2010 (6), implementation of pain clinic laws and mandatory checking Prescription Drug Monitoring Program data by prescribers (7), the reduction in the amount of opioids prescribed (8), and the rescheduling of hydrocodone compounds in 2014 (9). While these changes may have reduced the overdose deaths from prescription opioids, it is possible that they may have led some opioid dependent persons to switch to illicit opioids, such as heroin and fentanyl (10–12). Economic factors may also have contributed to the transition from prescription opioids to heroin; heroin is increasingly more available, easier to use through non-oral routes, and becoming purer and less expensive than prescription opioids (13). In addition, the subsequent sharp increase in fentanyl overdose deaths after 2013 is consistent with law enforcement data showing increased seizures of illicitly manufactured fentanyl (14, 15).
Several other fluctuations observed in the drug-specific mortality curves may also, in retrospect, be explainable. For example, in 2006, a spike in overdose deaths in the U.S. associated with fentanyl was traced to a production laboratory in Mexico (16). Similarly, the decline of methadone deaths after 2007 may be attributed to the removal of methadone from preferred drug list by state Medicaid programs which used to be major sources of methadone prescriptions for pain management (17). The rise and fall of cocaine related overdose deaths in the U.S. appears to be linked to production and supply in Columbia, which in turn have reflected diplomatic turns of events in a decades-long civil war (18). While opioids are the major offenders, drugs other than opioids, such as cocaine and methamphetamine, now also contribute significantly to the rising counts of overdose deaths in the U.S (19).
We also examined the mortality rates for deaths reported as being due to unspecified narcotics and unspecified drugs. Mortality rates from the unspecified narcotics have remained stable during the study period, but unspecified drugs closely follow prescription opioid mortality rates until 2008 and start to diverge after 2013 possibly indicating improvements in vital statistics reporting by some states.
None of the mortality curves from individual drugs has shown a regular or predictable pattern over the past 38 years. Nonetheless, we observed that the annual sum of all drug overdose mortality rates follows a remarkably smooth mathematical trajectory. Figure 1B plots changes in the total accidental poisoning mortality rate, from all drugs. Note that the total mortality rate per year is less than the sum of the mortality rates reported for individual drugs, due to listing of more than one drug on the death certificate in many individual cases(see Supplemental Figure 2).
The total accidental poisoning mortality rate closely tracks along an exponential growth curve defined as: annual overall mortality rate (r) = a × exp (b × year), where a = 1.022e-64 [CI = (−8.57e-64, 1.06e-63)], and b = 0.07445 [CI = (0.06978, 0.07912)]. Of particular interest is the observation that the first half of this long term smooth exponential growth curve pre-dates the current opioid epidemic.
2. The drug-specific sub-epidemics differ significantly with respect to their time course, geographic spread, and demographic groups affected.
Next, we examined death record data available from 1999 to 2016 to determine if there were any patterns in the demography or geography of mortality by drug that might explain how these variable individual drug curves might meld into a single smooth exponential process. To reveal patterns in this data, we use visualization techniques consisting of heatmaps (Fig. 2) and geospatial hot-spot analyses (Fig. 3).
Fig. 2.
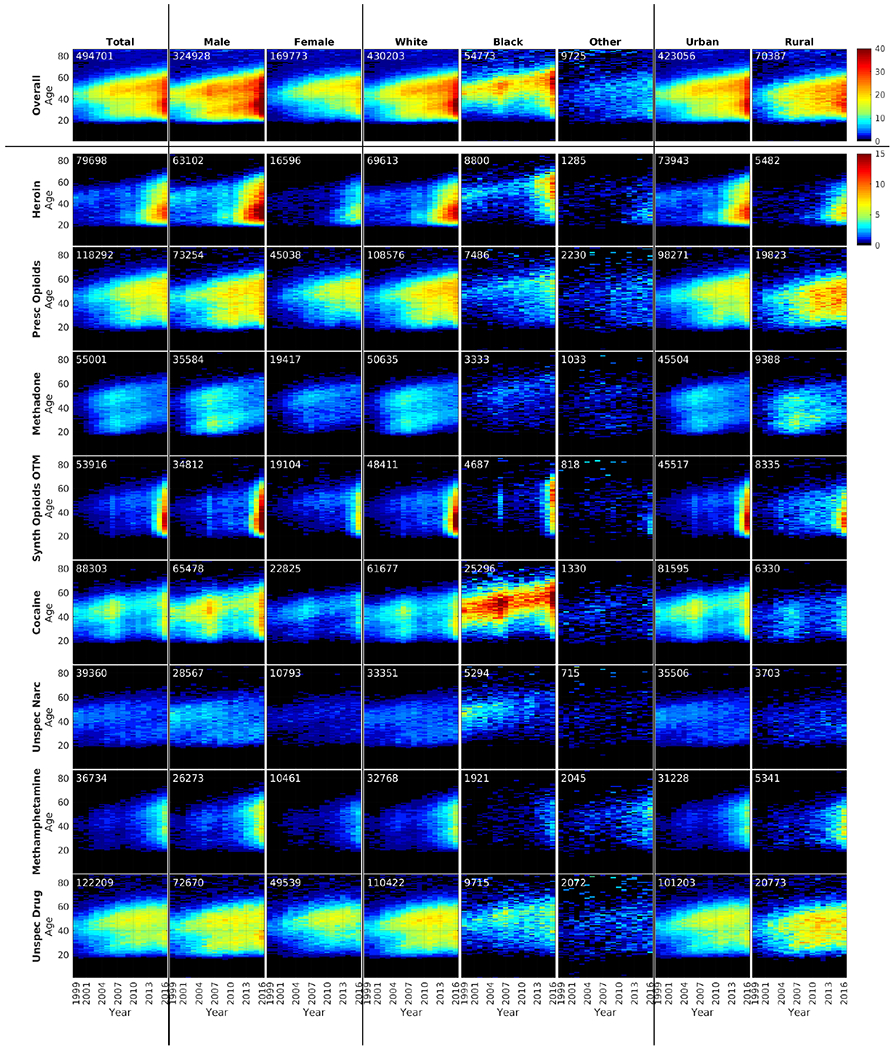
Heatmaps showing the sub-epidemic by demographics and urbanicity. Total number of deaths in each category from 1999 through 2016 are shown in the upper left corner of each plot. The colors indicate age-adjusted mortality rates per 100K people. [Synth Opioids OTM = Synthetic opioids other than methadone. This category includes fentanyl and its analogues].
Fig. 3.
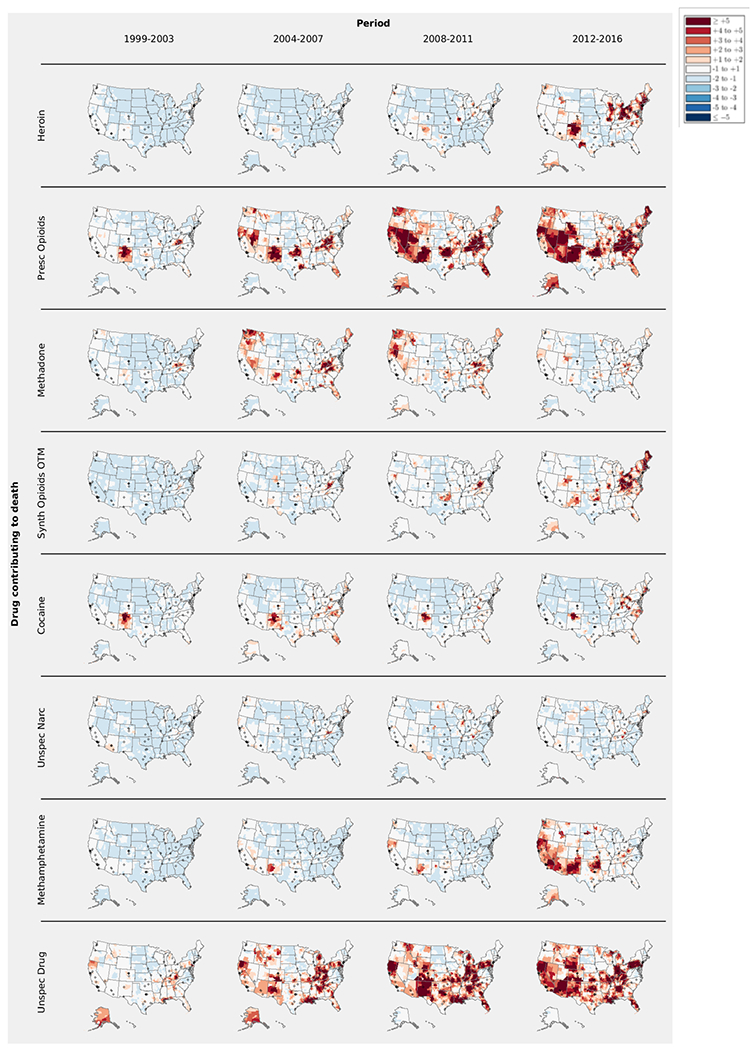
Geospatial hot-spot analysis by drug and period. The Gi* statistics are standardized using pooled statistics across all drugs and periods. The various shades of red and blue indicate pooled standard deviations above and below the pooled mean, respectively as shown in the legend. The small black circles indicate major cities with population greater than 300K people. None of the regions were less than 2 pooled standard deviations below the pooled average. [Synth Opioids OTM = Synthetic opioids other than methadone. This category includes fentanyl and its analogues].
Fig. 2 is a matrix of 72 individual age distribution heatmaps depicting how the age of overdose decedents have historically changed over time, as analyzed by drugs, gender, race and urbanicity. Age has been recognized as an important predictor in transitions from non-use or asymptomatic use to problematic drug use (20, 21) of illicit drugs, and the middle aged have had higher rates of prescription opioid deaths than other age groups (3, 22–24). In addition, significant increases in heroin overdose related hospitalizations among age groups of 20-29 and 50-59 have recently been identified, suggesting potential new cohorts of heroin users among age groups of 20-29 and 50-59 years (25, 26).
These age distribution heatmaps reveal some distinct patterns. One pattern is a clear bi-modal distribution of unintentional drug overdoses; a younger group (age 20-40 years) and an older group (age 40-60 years). The relative amplitudes of these groupings vary according to drug, gender, race and urbanicity. The younger age group predominates among deaths due to heroin and synthetic opioids, and especially among males, whites, and in urban counties. Mortality rates from prescription opioids and unspecified drugs were higher among the older age group, especially among females, whites and in rural counties.
Recent studies have examined the unspecified drug overdose death category and attributed some deaths in this category to prescription opioids because many states have drastically underreported prescription opioid related overdose deaths due to lack of toxicology testing for drug specificity in overdose deaths (27). From 1999-2016, 112,480 drug overdose deaths in which unspecified drugs were identified as the contributory cause of death, as compared to 106,193 deaths in which prescription opioids were a contributory cause of death. The patterns of overdose mortality rates for which the drug was unspecified closely resemble the patterns for prescription opioids across age, gender, race and urbanicity. The heatmaps clearly present these similarities.
Mortality differences between males and females rates are associated with age and type of drug. Prior reports of prescription opioid mortality rates have shown nearly four times higher rates in younger males than younger females, in contrast to only 1.3 fold higher rates in older males relative to older females (28). The heatmaps reveal that these differences can be mostly explained by the type of drug. The higher risk among young males relative to young females is mostly attributable to the heroin and synthetic drugs while the risk of death among older females are mostly attributable to prescription opioids and unspecified drugs. These differences by age, sex and type of drug have generally become more apparent in recent years.
The description of the association between drug overdose deaths and race in the literature has been mostly limited to the reports that show increased mortality rates, especially for opioids among whites (22–24, 29–31). In addition to the increased overdose deaths among whites, the heatmaps reveal that the peak mortality rate for cocaine among blacks has increased with each year, indicating a cohort aging effect. This pattern is especially noticeable among men and in urban counties. Among whites, the younger age group is at greatest risk for heroin and synthetic opioid deaths, while among blacks the older age group is at greater risk.
The increase of drug poisoning mortality in 2016 is due to increased mortality from multiple drug-specific sub-epidemics: synthetic opioids (most likely fentanyl) among males, whites and those in urban counties; heroin among young adults; prescription opioids among the middle aged, and blacks; and cocaine and methamphetamine among a wider age range, males, and whites.
To reveal geographic hotspots of each of the drugs over time, we also performed geospatial hotspot analyses of deaths due to each drug, broken into historical time intervals [summarized in the supplementary material]. Fig. 3 shows the geographic distribution of eight drug classes at each of four periods. Taken together these maps provide a synoptic view of changing landscape of drug mortality hotspots. Prior reports have been mostly limited to specific geographic regions, specific time periods and/or specific drugs. For example, a recent NCHS data brief shows that the Appalachian region and southwest region have overdose death rates statistically higher than the national rate (3). Similarly, a recent study has identified geospatial clusters of heroin related overdose deaths in 2000 in Southern California, and emerging later in New England, the Mid-Atlantic, and the Great Lakes region between 2013-2014 (4). Our geospatial hot-spots reveals the bigger picture by comparing hot-spots of all the drugs over space and time. [Please refer to the supplementary material for a detailed description of the methodology].
From 1999 to 2016 the epidemic intensity as well as the spatial distribution of deaths attributed to prescription drugs, heroin, synthetic opioids other than methadone, cocaine, and methamphetamine have all increased. Only for methadone has the epidemic intensity and spatial distribution peaked and then declined. Although the overall national epidemic may be smooth and continuous, during this 18-year period each drug has shown a specific geospatial pattern of spread. Heroin hotspots have changed from being closely clustered around large cities to be distributed more widely, especially in the Northeast and the Southwest. Prescription opioid hotspots initially were prominent in southwest U.S. and Appalachia, but subsequently spread to involve much of the western U.S., Oklahoma, Florida, and New England. Fentanyl and its analogues hot-spots have centered in opioid hotspots, especially in the Appalachian and Northeast regions. Cocaine hotspots have also centered around large cities but have diffused more broadly in the recent years. Methamphetamine deaths have increased most dramatically in the west and southwest U.S. Almost every region in the country is a hotspot for mortality from one or more drugs. The only large region that appears to have been relatively spared (a relative “cold spot” for all drugs) is composed of the north central states.
These detailed demographic and geographic analyses do not suggest obvious mechanisms as to how multiple drug-specific sub-epidemics have merged into a single smooth exponential 38+ year process. Indeed, these findings add to the paradox by revealing how disparate the individual drug epidemics are.
Effective public health responses will be crucial to address the USA drug crisis. Understanding the demographic and geographic characteristics of the sub-epidemics as reflected by overdose death patterns may be valuable in designing and strengthening “up-stream” public health surveillance systems for substance abuse and non-fatal overdoses among living persons (32), and elucidation of the underlying complexity of the drug-specific sub-epidemics may facilitate development of more effective, locally tailored primary, secondary, and tertiary prevention strategies (33, 34). For the large existing population of persons with substance use disorder or addiction (35), availability of and access to treatments and harm reduction services that are sub-epidemic specific may be valuable in preventing more overdose deaths. Lastly, better understanding of local drug death patterns may lead to innovative collaborations between public health and law enforcement which could include data sharing (36), partnership at local and community level on harm reduction, and linking people with addiction to treatment (37).
3. Caveats
Our findings should be interpreted with caution. First, there is substantial variation in the level of specificity of drug reporting for vital statistics across states and/or counties. A recent analysis found that in 2015, the percent of overdose deaths with the drug unspecified ranged from 0% in the District of Columbia to just over 50% in Pennsylvania (38). The geographic distribution of these deaths not attributed to specified drugs can be seen in Fig. 3. This analysis and others (39) have found that states with centralized medico-legal systems have more complete drug reporting than states with decentralized systems. Fig. S1 in the supplementary material reproduces Fig. 2 with data only from states that produce good quality data with less unspecified drug overdose diagnoses, and the results are almost identical, supporting the validity of the national level data analyses.
Second, our categories of specific drug mortality rates are not mutually exclusive, therefore, overdose deaths that involve multiple drugs could be counted more than once. Multi-drug abuse and overdose is increasing, and it is not always clear which drug or drugs are responsible for the overdose. Fig. S2 in the supplementary material shows how the relationships among various drugs have changed over time. In this figure we show that the percentage of death certificates including synthetic opioids OTM, cocaine and methamphetamine as a secondary drug has increased dramatically in the recent years, regardless of the index drug. While, the percentage of deaths attributed to heroin in addition to another drug is showing early signs of decline, but this decline is, of course, is only relative to the rapid rise in deaths due to the index drug. Additionally, the 10th revision of the international classification of diseases (ICD-10) only has a set number of codes for drug classes. Overdoses are now being attributed to new drugs, such as fentanyl analogs, but the drug class codes have not changed (eg, acryl fentanyl would be coded as T40.4), meaning that even with complete drug reporting, death certificates lose some drug specificity during the coding process. Additionally, coroners and medical examiners may not be able to identify newer psychoactive substances, indicating that these drugs will not be recorded on the death certificate. Such ambiguities in diagnostics do not affect our main finding of the exponential increase rate for overall drug overdose as each overdose death is counted once.
Third, the intent of an overdose death is not always easy to determine by a medical examiner or coroner. Our study only focused on unintentional or accidental drug overdoses that constitutes roughly 85% of all drug overdoses every year; however, we recognize that the practice or capacity of determining intent varies by states.
Lastly, the dynamics of the substance use epidemic are not fully captured in drug overdose mortality data alone. A more complete analysis would also describe the initiation, natural history, treatment, and progression of drug use.
4. The opioid crisis may be part of a greater, longer-term process
The epidemic of drug overdoses in the U.S. has been inexorably tracking along an exponential growth curve since at least 1979, well before the surge in opioid prescribing in the mid 1990’s. While there have been transient periods of minor acceleration or deceleration, the overall drug overdose mortality rate has regularly returned to the exponential growth curve. This historical pattern of predictable growth for at least 38 years strongly suggests that the epidemic will continue along this path for several more years. In contrast, the recent historical variability with which some specific drugs have waxed and waned makes predictions about the future role of specific drugs far more uncertain. Indeed, it is possible that in the future the drug overdose epidemic may be driven by a new or heretofore obscure psychoactive substance.
Understanding the forces that are holding multiple sub-epidemics together into a smooth exponential trajectory may be important in revealing the root causes of the epidemic, and this understanding may be crucial to implementation of prevention and intervention strategies. Economic and technological “push” factors may be at work to increase supply, such as improved communications and supply chains, efficiencies in drug manufacturing, and expanding drug markets leading to lower prices and higher drug purities (40, 41). Sociological and psychological “pull” forces may be operative to accelerate demand, such as despair, loss of purpose, and dissolution of communities (42, 43). Elucidation of the dynamics of the “deep” drivers of the overdose epidemic may provide valuable new insights.
Materials and Methods:
This section provides a summary of the materials and methods. For a more detailed explanation we refer the reader to the supplementary materials where the materials and methods are described in detail. Death information was obtained from the Mortality Multiple Cause Microdata Files from 1979 to 2016. This data uses ICD-9 since 1979 enabling us to identify accidental drug poisoning deaths. In addition, we are able to identify specific drugs as contributory causes of accidental overdose deaths since 1999 because the data starts using ICD-10. For example, the ICD-10 code for heroin is T40.1, and for natural and semi-synthetic opioids (including prescription opioids) is T40.2.
To illustrate the changing dynamics of the drug-overdose deaths on multiple levels, we examined overdose mortality rates using three levels of detail: (1) National level, by drug, over time, (2) National level, by drug, over time, with detailed analysis by demographic groups of age, sex, race, and urbanicity, and (3) County-level cluster analysis, by drug, over time (hotspot analysis).
For national level analyses, we computed mortality rates for individuals by drug codes and by age, sex, race, and urbanicity. For each computation, we used the appropriate denominator from the US census population estimates from 1999 through 2016. To distinguish rural from urban counties, we used the 2013 Rural-Urban Continuum Codes (RUCC).
In the county-level analysis we used the Getis-Ord Gi* statistic to show geospatial clustering of hot (high) and cold (low) spots of mortality rates. The Gi* statistic identifies these hot and cold spots based on contiguous counties. The Gi* statistic is essentially a Z-score standardized by a mean and standard deviation of mortality rates in all the counties. Typically, the Gi* statistic can display geospatial information on one dimension such as mortality rates. To add additional dimensions and compare mortality rates by drug and time, we re-standardized the Gi* statistics using the pooled mean and standard deviations of the Gi* statistics across all drugs and over time. This re-standardization allowed us to produce a set of comparable maps across time and drugs.
Supplementary Material
Acknowledgments:
We thank reviewers from the National Center for Injury Prevention and Control, and the National Centers for Health Statistics, for improvements to the manuscript.
Funding:
This study was in part supported by CDC grant #IPA 16IPA1605230 and NIH/NCATS grant #1KL2TR0001856 (H.J.), and Robert Wood Johnson Foundation Grant # 72858 (J.B. and D.S.B.).
Footnotes
Competing interests: The authors declare no competing interests.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Data and materials availability: (1) Multiple Cause of Death Data from the Center of Disease Control and Prevention available by request at https://wonder.cdc.gov/mcd.html. (2) Population demographics from the US Census available at https://www.census.gov/ces/dataproducts/demographicdata.html. strategies.
References and Notes:
- 1.Center for Disease Control and Prevention; Atlanta, GA, U.S. drug overdose deaths continue to rise; increase fueled by synthetic opioids; (2018. (https://www.cdc.gov/media/releases/2018/p0329-drug-overdose-deaths.html). [Google Scholar]
- 2.HHS Acting Secretary Declares Public Health Emergency to Address National Opioid Crisis (2017. https://www.hhs.gov/about/news/2017/10/26/hhs-acting-secretary-declares-public-health-emergency-address-national-opioid-crisis.html).
- 3.Hedegaard H, Warner M, Miniño AM, Drug Overdose Deaths in the United States, 1999-2015. NCHS Data Brief, US Department of Health and Human Services No. 273, (2017). [PubMed] [Google Scholar]
- 4.Stewart K, Cao Y, Hsu MH, Artigiani E, Wish E, Geospatial Analysis of Drug Poisoning Deaths Involving Heroin in the USA, 2000–2014. Journal of Urban Health 94, 572–586 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burke DS, Forecasting the opioid epidemic. Science 354, 529 (2016). [DOI] [PubMed] [Google Scholar]
- 6.Cicero TJ, Ellis MS, Abuse-Deterrent Formulations and the Prescription Opioid Abuse Epidemic in the United States: Lessons Learned From OxyContin. JAMA Psychiatry 72, 424–430 (2015). [DOI] [PubMed] [Google Scholar]
- 7.Dowell D, Zhang K, Noonan RK, Hockenberry JM, Mandatory Provider Review And Pain Clinic Laws Reduce The Amounts Of Opioids Prescribed And Overdose Death Rates. Health Aff (Millwood) 35, 1876–1883 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guy GP Jr. et al. , Vital Signs: Changes in Opioid Prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep 66, 697–704 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones CM, Lurie PG, Throckmorton DC, Effect of US Drug Enforcement Administration’s Rescheduling of Hydrocodone Combination Analgesic Products on Opioid Analgesic Prescribing. JAMA Intern Med 176, 399–402 (2016). [DOI] [PubMed] [Google Scholar]
- 10.Alpert A, Powell D, Pacula RL, “Supply-Side Drug Policy in the Presence of Substitutes: Evidence from the Introduction of Abuse-Deterrent Opioids,” (National Bureau of Economic Research, 2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cicero TJ, Ellis MS, Surratt HL, Effect of abuse-deterrent formulation of OxyContin. N Engl J Med 367, 187–189 (2012). [DOI] [PubMed] [Google Scholar]
- 12.Becker WC, Sullivan LE, Tetrault JM, Desai RA, Fiellin DA, Non-medical use, abuse and dependence on prescription opioids among U.S. adults: psychiatric, medical and substance use correlates. Drug Alcohol Depend 94, 38–47 (2008). [DOI] [PubMed] [Google Scholar]
- 13.National drug control strategy: data supplement 2016. (Office of National Drug Control Policy Executive, Office of the President of the United States Washington, DC, 2016). [Google Scholar]
- 14.Gladden RM, Martinez P, Seth P, Fentanyl Law Enforcement Submissions and Increases in Synthetic Opioid-Involved Overdose Deaths - 27 States, 2013-2014. MMWR Morb Mortal Wkly Rep 65, 837–843 (2016). [DOI] [PubMed] [Google Scholar]
- 15.Peterson AB et al. , Increases in Fentanyl-Related Overdose Deaths - Florida and Ohio, 2013-2015. MMWR Morb Mortal Wkly Rep 65, 844–849 (2016). [DOI] [PubMed] [Google Scholar]
- 16.Public Health Advisory: Methadone Use for Pain Control May Result in Death and Life-Threatening Changes in Breathing and Heart Beat (2006. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm124346.htm).
- 17.Faul M, Bohm M, Alexander C, Methadone Prescribing and Overdose and the Association with Medicaid Preferred Drug List Policies - United States, 2007-2014. MMWR Morb Mortal Wkly Rep 66, 320–323 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miroff N, in A side effect of peace in Colombia? A cocaine boom in the U.S. (The Washington Post, 2017).
- 19.McCall Jones C, Baldwin GT, Compton WM, Recent Increases in Cocaine-Related Overdose Deaths and the Role of Opioids. Am J Public Health 107, 430–432 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Compton WM, Jones CM, Baldwin GT, Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. N Engl J Med 374, 154–163 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Compton WM, Dawson DA, Conway KP, Brodsky M, Grant BF, Transitions in illicit drug use status over 3 years: a prospective analysis of a general population sample. Am J Psychiatry 170, 660–670 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Buchanich JM et al. , Patterns and trends in accidental poisoning death rates in the US, 1979-2014. Preventive medicine 89, 317–323 (2016). [DOI] [PubMed] [Google Scholar]
- 23.Chen LH, Hedegaard H, Warner M, Drug-Poisoning deaths involving opioid analgesics: United States, 1999–2011. NCHS data brief, No. 166. (National Center for Health Statistics., Hyattsville, MD, 2014). [PubMed] [Google Scholar]
- 24.Paulozzi LJ, Jones CM, Mack KA, Rudd RA, Vital Signs: Overdoses of Prescription Opioid Pain Relievers - United States, 1999-2008. MMWR: Morbidity and Mortality Weekly Report. 2011. [PubMed] [Google Scholar]
- 25.Tedesco D et al. , Opioid Abuse And Poisoning: Trends In Inpatient And Emergency Department Discharges. Health Aff (Millwood) 36, 1748–1753 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guy GP Jr., Pasalic E, Zhang K, Emergency Department Visits Involving Opioid Overdoses, U.S., 2010–2014. Am J Prev Med 54, e37–e39 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruhm CJ, Geographic Variation in Opioid and Heroin Involved Drug Poisoning Mortality Rates. American journal of preventive medicineIn Press. [DOI] [PubMed] [Google Scholar]
- 28.Calcaterra S, Glanz J, Binswanger IA, National Trends in Pharmaceutical Opioid Related Overdose Deaths Compared to other Substance Related Overdose Deaths: 1999-2009. Drug and alcohol dependence 131, 263–270 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Balmert LC et al. , Patterns and Trends in Accidental Poisoning Deaths: Pennsylvania’s Experience 1979-2014. PLoS ONE 11, e0151655 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Warner M, Chen LH, Makuc DM, Increase in fatal poisonings involving opioid analgesics in the United States, 1999-2006. NCHS data brief, 1–8 (2009). [PubMed] [Google Scholar]
- 31.Paulozzi L, Annest J, Unintentional Poisoning Deaths-United States, 1999–2004. MMWR Morb Mortal Wkly Rep 56, 93–96 (2007). [PubMed] [Google Scholar]
- 32.Vivolo-Kantor AM et al. , Vital Signs: Trends in Emergency Department Visits for Suspected Opioid Overdoses - United States, July 2016-September 2017. MMWR Morb Mortal Wkly Rep 67, 279–285 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kolodny A et al. , The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health 36, 559–574 (2015). [DOI] [PubMed] [Google Scholar]
- 34.Epidemic: Responding to America’s Prescription Drug Abuse Crisis (2011).
- 35.2016 National Survey on Drug Use and Health: Detailed Tables (2017).
- 36.While Greater Attention Given to Combating Synthetic Opioids Agencies Need to Better Assess their Efforts (2018).
- 37.The Unprecedented Opioid Epidemic (2017).
- 38.Buchanich JM, Balmert LC, Williams KE, Burke DS, The Effect of Incomplete Death Certificates on Estimates of Unintentional Opioid-Related Overdose Deaths in the United States, 1999-2015. Public Health Rep, 33354918774330 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Warner M, Paulozzi LJ, Nolte KB, Davis GG, Nelson LS, State Variation in Certifying Manner of Death and Drugs Involved in Drug Intoxication Deaths. Academic Forensic Pathology 3, 231–237 (2013). [Google Scholar]
- 40.Mars SG et al. , Heroin-related overdose: The unexplored influences of markets, marketing and source-types in the United States. Soc Sci Med 140, 44–53 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Unick G, Rosenblum D, Mars S, Ciccarone D, The relationship between US heroin market dynamics and heroin-related overdose, 1992-2008. Addiction 109, 1889–1898 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Case A, Deaton A, Mortality and morbidity in the 21(st) century. Brookings Pap Econ Act 2017, 397–476 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vega OA et al. , Wnt/beta-Catenin Signaling Activates Expression of the Bone-Related Transcription Factor RUNX2 in Select Human Osteosarcoma Cell Types. J Cell Biochem 118, 3662–3674 (2017). [DOI] [PubMed] [Google Scholar]
- 44.National S Center for Health, Mortality Multiple Cause Data Files. Centers for Disease Control, US Department of Health and Human Services. 2000. [Google Scholar]
- 45.E. R. S. U.S. Department of Agriculture, Rural-Urban Continuum Codes. 2013. [Google Scholar]
- 46.Seth P, Scholl L, Rudd RA, Bacon S, Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants - United States, 2015-2016. MMWR Morb Mortal Wkly Rep 67, 349–358 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jones CM, Einstein EB, Compton WM, Changes in Synthetic Opioid Involvement in Drug Overdose Deaths in the United States, 2010-2016. JAMA 319, 1819–1821 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Getis A, Ord JK, The Analysis of Spatial Association by Use of Distance Statistics. Geographical Analysis 24, 189–206 (1992). [Google Scholar]
- 49.Ord JK, Getis A, Local Spatial Autocorrelation Statistics: Distributional Issues and an Application. Geographical Analysis 27, 286–306 (1995). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


