Abstract
Background:
Systems of care emphasize parent-delivered intervention for children with autism spectrum disorder (ASD). Meanwhile, multiple studies document psychological distress within these parents.
Objectives:
This pilot longitudinal randomized controlled trial compared the Parent-implemented Early Start Denver Model (P-ESDM) to P-ESDM plus Mindfulness Based Stress Reduction (MBSR) for parents. We evaluated changes in parent functioning during active treatment and at follow-up.
Methods:
Participants included children (< 36 months) with ASD and caregivers. Participants were randomized to P-ESDM only (n = 31) or P-ESDM + MBSR (n = 30). Data were collected at baseline, mid-treatment, end of treatment, and one, three, and six-months post-treatment. Multilevel models with discontinuous slopes were used to test for group differences in change in outcomes over time.
Results:
Both groups improved during active treatment in all sub-domains of parent stress (Bs=−1.42, −1.25, −.92, ps < .001), depressive symptoms, and anxiety symptoms (Bs = −.62 and −.78, respectively, ps < .05). Parents who received MBSR had greater improvements than P-ESDM only in parental distress and parent-child dysfunctional interactions (Bs = −1.91 and −1.38, respectively, ps < .01). Groups differed in change in mindfulness during treatment (B = 3.15, p < .05), with P-ESDM+MBSR increasing and P-ESDM declining. Treatment group did not significantly predict change in depressive symptoms, anxiety symptoms, or life satisfaction. Differences emerged based upon parent sex, child age, and child behavior problems.
Conclusions:
Results suggest that manualized, low intensity stress reduction strategies may have long-term impacts on parent stress. Limitations and future directions are described.
Table of Contents Summary:
This study examined whether parents of children with ASD reported better functioning if they received stress reduction training as part of early behavioral intervention.
Symptoms of Autism Spectrum Disorder (ASD) may become evident by age 18 months.1–3 Emerging evidence suggests that early behavioral intervention improves outcomes,4,5 with some intervention models including parents in critical roles.5 Parent-delivered early intervention may promote skill generalization and allow systems of care to spread therapist time and cost across more children. In parallel, however, multiple studies have documented high levels of psychological stress and distress within the parents of children with ASD,6–12 more so than parents of children with other diagnoses.13–16 Although this distress may negatively impact families during a critical time of diagnostic understanding and service initiation, little has been done to deliberately study and support parents as part of early intervention delivery.
Parent involvement in intervention may generalize strategy utilization across settings.17,18 Incorporating parents into treatment is a core component of many state early intervention systems;19 as applied to autism, this framework offers opportunities for addressing not only child but also broader family functioning. However, rigorous studies of parent-mediated interventions for young children have yielded mixed results.5,17,20–27 Although undoubtedly influenced by variability within the autism phenotype, parent and family characteristics may affect how such training programs are perceived and implemented.28–30 Parent stress and coping strategies may be influenced by factors such as parent or child sex, child age, and child problem behaviors.28,29,31–41 Some of these relations may be reciprocal, with parenting stress changing as a function of, but then also directly impacting, child functioning over time.16,28,29,31,32,42–44 These chronic effects may therefore impact parent training paradigms, which emphasize increased parental responsivity and active provision of learning opportunities.22,23,45,46
Increasingly, studies have investigated ways to directly support parents of children with developmental disabilities.47 One promising avenue is Mindfulness Based Stress Reduction (MBSR).48 Several studies have documented that MBSR may reduce stress, improve sleep and health, and increase life satisfaction for parents of individuals with developmental disabilities.9,14,49–51 Parents trained in MBSR report more positivity toward their children, less negativity regarding their child’s impact on the family, lower reactivity, and more frequent use of positive reappraisal strategies.9,51–53 Parents who practice self-compassion report lower levels of depression and parenting stress,44 with two studies finding sustained effects of mindfulness practice on parent psychological distress and emotional and behavioral outcomes.50,53 Although promising, these works primarily delivered MBSR in isolation to parents of older children. One previous study combined mindfulness-based training for adolescents with ASD with parallel parent training, with improvements in parental stress and child behavior problems.53
Little is known about how the combination of MBSR and low levels of early parent-mediated behavioral intervention impacts functioning of parents of young children with new ASD diagnoses. This work attempted to address parent stress and distress by providing parents with skills-focused stress reduction strategies during the post-diagnostic period. The primary aim of this pilot randomized controlled trial was to compare the effectiveness of a parent-mediated behavioral intervention – the Parent-Implemented Early Start Denver Model Parent, or P-ESDM - to that intervention plus MBSR (P-ESDM + MBSR) in enhancing parent functioning. We hypothesized that both groups would improve in parent functioning over time, and that compared to the P-ESDM only group, parents in P-ESDM + MBSR would show greater reductions in stress, depression, and anxiety as well as increased self-reported life satisfaction and mindfulness. A second aim was to examine whether treatment response differed based on five covariates: child age at treatment initiation, child sex, parent sex, child autism severity, and behavior problems.
Methods
Participants
Participating parents were recruited from a diagnostic clinic from 2015–2017. Eligibility criteria included having a child (less than 36 months of age at consent) with a gold-standard ASD diagnosis and parental English fluency. Exclusion criteria included severe child sensorimotor impairment. All procedures were approved by the medical center Institutional Review Board.
We utilized a random number generator with a planned maximum enrollment of 70 participants. Allowing approximately 10% attrition, this provides 80% power to detect an effect size of 0.71 for one primary outcome or an effect size of 0.91 if a multiple comparison correction were applied for 7 co-primary outcomes. We placed half of the generated numbers into each group. Blinded staff obtained consent then accessed a unique computer file to determine group assignment.
Of 103 eligible families, 63 consented to participate (Figure 1). Two participants did not have data that could be included in analyses: One (P-ESDM only) provided inaccurate data and a second (P-ESDM +MBSR) withdrew without providing any parent data. This yielded a final sample of 61 families included in analyses (see Tables 1 and 2). Of these 61 participants, 7 withdrew before completing their third P-ESDM session. Reasons for withdrawal included: scheduling conflicts (n = 5) and repeatedly missed sessions (n = 2). An additional 8 families were lost to 6-month follow-up (moved away, n = 4; lost to contact, n = 4). This attrition rate is similar to other studies of parent implemented, low intensity ASD interventions,14,23,54,55 and did not differ by group or demographics.
Figure 1.
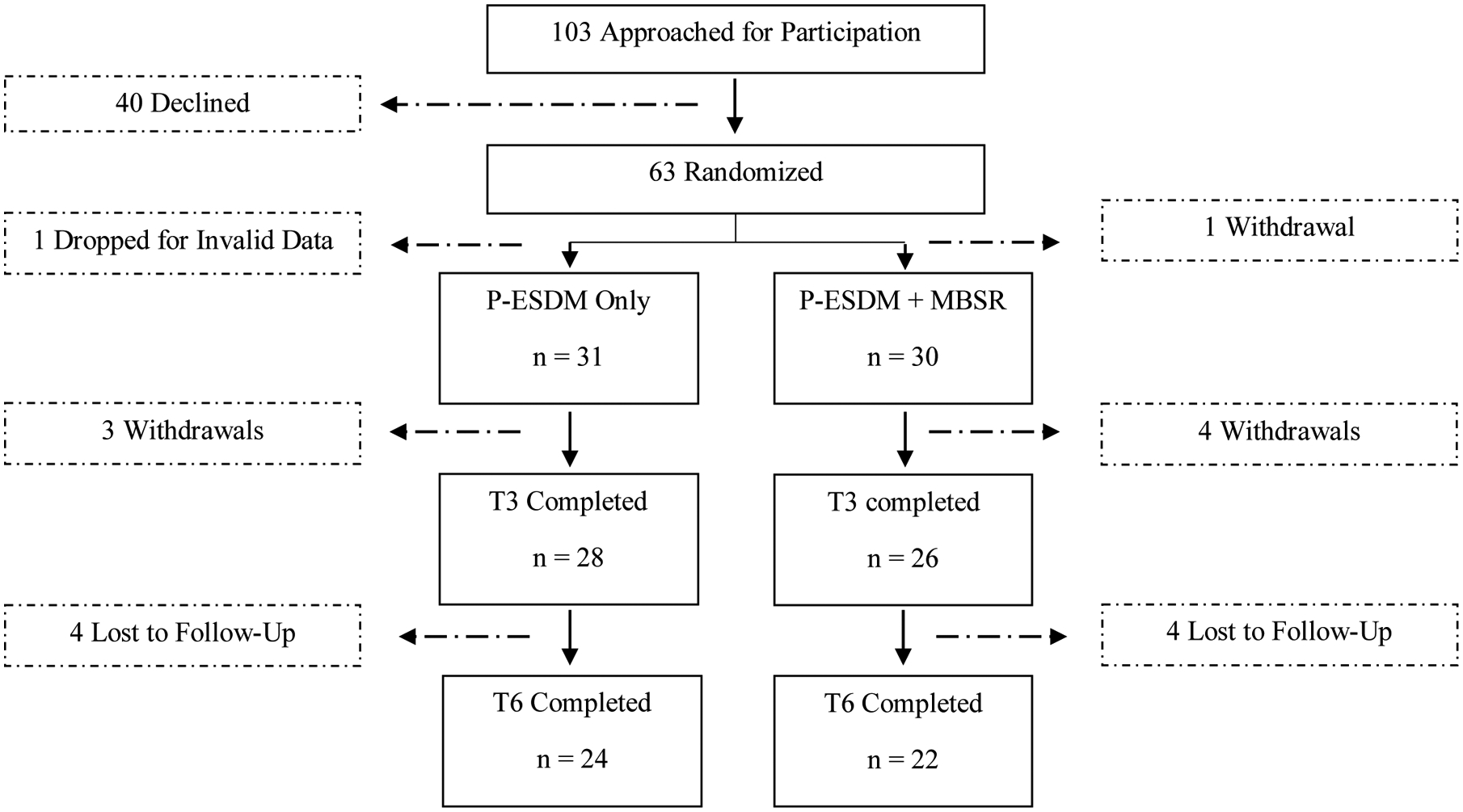
Participant recruitment and retention flowchart.
Table 1.
Baseline child demographics.
| P-ESDM N = 31 Mean (sd) or Count |
P-ESDM + MBSR N = 30 Mean (sd) or Count |
|
|---|---|---|
| Age treatment began, in years | 2.46 (1.64) | 2.30 (.45) |
| Sex | ||
| Male | 25 (81%) | 25 (83%) |
| Female | 6 (19%) | 5 (17%) |
| Race | ||
| Asian | 2 (6%) | 2 (7%) |
| Black or African American | 1 (3%) | 1 (3%) |
| Native Hawaiian or Other Pacific Islander | 2 (6%) | 0 (0%) |
| White | 26 (85%) | 27 (90%) |
| Ethnicity | ||
| Hispanic or Latino | 2 (7%) | 1 (3%) |
| Non-Hispanic or Latino | 29 (93%) | 29 (97%) |
| P-ESDM treatment length (weeks) | 16.25 (3.38) | 15.47 (3.30) |
| ADOS-2 Calibrated Severity Score | 8.38 (1.49) | 7.93 (1.76) |
| Child Behavior Checklist (Total Problems T-score) | 59.82 (8.65) | 57.70 (9.36) |
| Mullen Scales of Early Learning | ||
| Early Learning Composite | 55.97 (13.48) | 60.07 (10.18) |
| Visual Reception AE | 19.59 (4.23) | 21.71 (6.69) |
| Fine Motor AE | 20.67 (3.85) | 21.83 (5.19) |
| Receptive Language AE | 14.56 (6.89) | 21.46 (14.83) |
| Expressive Language AE | 15.30 (7.69) | 19.21 (11.19) |
| VABS-II | ||
| Adaptive Behavior Composite | 74.41 (11.93) | 75.79 (9.86) |
| Communication | 76.04 (17.83) | 81.00 (15.84) |
| Daily Living Skills | 77.33 (13.11) | 76.08 (11.19) |
| Socialization | 72.56 (11.50) | 73.50 (8.14) |
| Motor | 82.78 (7.99) | 84.71 (11.00) |
Note. P-ESDM = Parent-implemented Early Start Denver Model. ADOS-2 = Autism Diagnostic Observation Schedule, Second Edition. AE = Age Equivalent, in months. VABS-II ABC = Vineland Adaptive Behavior Scales-Second Edition, Adaptive Behavior Composite.
Table 2.
Baseline participating parent demographics.
| P-ESDM N = 31 |
P-ESDM + MBSR N = 30 |
|
|---|---|---|
| Mean age treatment began (sd) | 33.79 (5.53) | 33.27 (6.24) |
| Sex | ||
| Male | 4 (13%) | 4 (13%) |
| Female | 27 (87%) | 26 (87%) |
| Race | ||
| Asian | 2 (6%) | 3 (10.0%) |
| Black or African American | 1 (3%) | 1 (3%) |
| Native Hawaiian or Other Pacific Islander | 0 (0%) | 0 (0%) |
| White | 28 (91%) | 26 (87%) |
| Ethnicity | ||
| Hispanic or Latino | 4 (13%) | 2 (6%) |
| Non-Hispanic or Latino | 27 (87%) | 28 (93%) |
| Employed? | ||
| Yes | 18 (58%) | 24 (80%) |
| No | 12 (39%) | 3 (10%) |
| Did not answer | 1 (3%) | 3 (10%) |
| Annual Household Income | ||
| < 30000 | 3 (10%) | 4 (13%) |
| 30,000–60,000 | 6 (19%) | 7 (24%) |
| 60,000–90,000 | 9 (29%) | 6 (20%) |
| > 90,000 | 12 (39%) | 10 (33%) |
| Did not answer | 1 (3%) | 3 (10%) |
| Highest educational attainment | ||
| High school grad/GED | 4 (13%) | 5 (17%) |
| Some college or tech school | 5 (16%) | 8 (27%) |
| Associates degree | 2 (7%) | 2 (6%) |
| Bachelors degree | 12 (39%) | 5 (17%) |
| Some post graduate education | 1 (3%) | 2 (6%) |
| Graduate degree | 7 (23%) | 5 (17%) |
| Did not answer | 0 (0%) | 3 (10%) |
Measures
Dependent Variables: Parent Functioning.
Parent functioning variables were collected at each time point (see Procedure).
Parenting stress.
Parents completed the Parenting Stress Index – Short Form (PSI-SF), Third Edition. This 36-item measure yields three subscale scores (Parent Child Dysfunctional Interaction, PCDI; Parenting Distress, PD; Difficult Child, DC) used in present analyses. Higher scores indicate more stress.
Mental health.
Parents completed the Centers for Epidemiologic Studies – Depression scale (CES-D; 20 items) and the Beck Anxiety Inventory (BAI; 21 items).56 Higher scores on these measures reflect more symptoms.
Life Satisfaction.
Parents completed the Satisfaction with Life Scale (SLS),57 a measure of subjective wellbeing. Its 5 items are scored along a 7-point Likert scale (higher scores indicate more satisfaction).
Mindfulness.
Parents completed the Five Facet Mindfulness Questionnaire (FFMQ).58 The FFMQ consists of 44 items that yield five subscales. The total score was used in analyses. Higher scores indicate more mindfulness.
Demographic and Child Variables
Before randomization, parents provided the following baseline information: relationship to child, birth date, educational attainment, race/ethnicity of self and child, employment status, and annual household income.
Autism severity.
The Autism Diagnostic Observation Schedule – Second Edition (ADOS-2) is a standardized clinical observation system for use with people with developmental ages of 12 months and older.59 Each module yields Calibrated Severity Scores (CSS; range: 1–10) based on age group and language level, which were used in these analyses. Higher scores reflect higher levels of autism symptoms.
Cognitive Assessment.
The Mullen Scales of Early Learning (MSEL) is a standardized developmental test for children up to age five years.60 It provides four domain scores (Visual Reception, Fine Motor, Receptive Language, Expressive Language; M=50, SD=10) and yields an overall ability index (Early Learning Composite, ELC; M=100, SD=15). Higher scores reflect higher ability levels.
Adaptive Functioning.
The Vineland Adaptive Behavior Scales – Second Edition (VABS-II), Interview Form is a semistructured interview.61 It yields four domain standard scores: Communication, Daily Living Skills, Socialization, and Motor Skills (M = 100, SD = 15), and an overall Adaptive Behavior Composite (M = 100, SD = 15). Higher scores reflect better adaptive behavior skills.
Behavior Problems.
The Child Behavior Checklist for Ages 1 ½ −5 (CBCL)62 is a parent-completed checklist of internalizing and externalizing behaviors. It includes 100 symptoms scored from 0–2 (higher scores = more symptom presence) within the past two months. T-scores ≥ 64 are considered clinically significant for broadband scales. Because of the high correlation between internalizing and externalizing subscales in this work (r = .61, p < .001), we used the Total Problems scale (T-score).
Procedure
After randomization, families were scheduled for their first P-ESDM session and, where applicable, paired with an MBSR therapist. MBSR sessions began after the second P-ESDM session. Data were collected at six time points: baseline (prior to treatment), mid-treatment (6 weeks), end of treatment (12 weeks), and one, three, and six-months post-treatment
Intervention: P-ESDM.
P-ESDM consisted of 12 consecutive weekly clinic-based sessions, approximately 1 hour long. P-ESDM began an average of 1.35 months after diagnosis (sd = 1.45). Because of variable family schedules, it took an average of 15.87 weeks (sd = 3.33) to complete 12 sessions. Six P-ESDM therapists (separate from MBSR therapists, blinded to group assignment) were licensed Board Certified Behavior Analysts trained to fidelity by ESDM-certified trainers. This manualized intervention has a detailed parent-training curriculum and a specific coaching intervention method.5 Therapists introduce skills through descriptions, modeling, and coaching, with embedded emphasis on skill generalizability. Fidelity was monitored using the ESDM Fidelity Checklist. Therapists covered 94% of intended content across sessions, with no significant differences between groups (p > .10).
Intervention: P-ESDM + MBSR.
Parents randomized to P-ESDM + MBSR attended six additional one-hour individual sessions. Childcare was provided to maximize attendance. The four MBSR therapists were clinicians with at least a Master’s degree with expertise in behavioral intervention and ASD, supervised by a licensed clinical psychologist with formal MBSR training. Fidelity was monitored by therapist-completed content checklists.
The MBSR protocol was based upon the work of Dykens et al.14 and modified for individual administration for parents of young children with ASD. It was introduced as a skills-focused stress reduction program, rather than individual therapy. The clinic-based sessions covered topics such as: an introduction to mindfulness for managing stress, awareness of the present moment, and cultivating gratitude. Weekly handouts offered written and pictorial practice cues for the home. Suggested homework exercises included formal practice (e.g., guided meditation) as well as activities easily incorporated into daily routines (e.g., breath awareness). Weekly homework logs tracked strategy utilization.
Data Analysis
Multilevel models with discontinuous slopes, using Hierarchical Linear Modeling software,63 were used to test for group differences in change in outcomes over time. This allowed for inclusion of all participants with at least one time point of data. We modeled discontinuous rates of individual change with two time epochs:64 1) linear slope from the first to third time point (baseline, six weeks into treatment, immediately post-treatment) representing change during active treatment, and 2) change in linear slope from immediately post-treatment through the 6-month follow-up (immediately post-treatment, 1-, 3-, and 6-months post-treatment) reflecting change post-treatment. We estimated multilevel models for each outcome that included the between-subjects variable of treatment group, with groups centered on zero (P-ESDM = −0.5, P-ESDM + MBSR = 0.5). Overall slope estimates in these models reflect change across the entire sample. Including treatment group allowed us to determine whether any of the slope estimates (slope representing change during active treatment, change in slope during post-treatment) significantly differed by treatment group. Additional between-persons covariates included: child age at treatment initiation; sex of child, sex of parent; baseline autism severity, and child behavior problems. Because this is pilot work, no corrections were multiple comparisons were made. All covariates were grand-mean centered.
Results
Sample characteristics
No adverse events were reported. Baseline demographic and diagnostic information about children and participating parents is in Table 1 and Table 2.
Aim 1: Treatment effects on parent outcomes
Estimates from the longitudinal models conditioned on treatment group and covariates for each of the outcome variables are presented in Table 3.
Table 3.
Estimates (Coefficients and standard errors of coefficients) from conditional multilevel models of change in parent outcomes
| Independent Variables | Model Estimates: Coefficient (SE) | ||||||
|---|---|---|---|---|---|---|---|
| PSI: Parental Distress | PSI: Parent-Child Dysfunctional Interaction | PSI: Difficult Child | Depressive symptoms | Anxiety symptoms | Life Satisfaction | Mindfulness | |
| Initial status intercept (random) | 29.13 (0.68)*** | 31.11 (0.82)*** | 32.55 (0.64)*** | 10.53 (0.74)*** | 9.12 (0.77)*** | 26.20 (0.79)*** | 134.82 (2.20)*** |
| P-ESDM+MBSR (vs. P-ESDM) | 3.24 (1.50)* | 1.19 (1.90) | 1.08 (1.37) | 0.33 (1.50) | 0.97 (1.76) | 0.20 (1.62) | −5.66 (4.53) |
| Child age | −0.45 (1.36) | −5.34 (2.11)* | −2.71 (1.27)* | −2.24 (1.61) | −3.18 (1.73)† | 4.96 (2.23)* | 5.64 (5.50) |
| Male child (vs. female) | −0.53 (1.78) | 1.75 (2.08) | 2.22 (1.55) | −2.27 (2.58) | 1.53 (1.88) | 2.08 (2.42) | −0.49 (5.00) |
| Male parent (vs. female) | 4.40 (2.03)* | 1.70 (2.00) | 0.82 (2.19) | −0.98 (1.34) | −2.68 (2.03) | −2.88 (2.33) | 1.73 (6.93) |
| Parent education | 0.41 (0.44) | 0.36 (0.52) | 0.42 (0.43) | −0.10 (0.80) | 0.08 (0.52) | 0.61 (0.61) | −1.32 (1.36) |
| Autism severity | 0.18 (0.42) | −0.18 (0.55) | 0.13 (0.44) | −0.74 (0.63) | −0.28 (0.52) | 0.60 (0.57) | −1.60 (1.46) |
| Behavior problems | 0.52 (.07)*** | 0.50 (0.10)*** | 0.47 (0.06)*** | 0.34 (0.12)** | 0.41 (0.10)*** | −0.20 (0.11)† | −1.17 (0.26)*** |
| Active treatment slope (random) | −1.42 (0.23)*** | −1.25 (0.23)*** | −0.92 (0.22)*** | −0.62 (0.21)** | −0.78 (0.29)* | 0.07 (0.17) | −0.65 (0.58) |
| P-ESDM+MBSR (vs. P-ESDM) | −1.91 (0.45)*** | −1.38 (0.44)** | −0.48 (0.48) | −0.35 (0.45) | −0.62 (0.65) | 0.57 (0.40) | 3.15 (1.44)* |
| Child age | −0.38 (0.49) | 1.08 (0.60)† | 0.46 (0.46) | 0.16 (0.46) | 0.03 (0.71) | −1.08 (0.39)** | 0.95 (1.15) |
| Male child (vs. female) | −0.27 (0.64) | −0.51 (0.66) | −0.73 (0.58) | 0.47 (0.57) | −0.60 (0.65) | 0.66 (0.41) | −1.00 (1.51) |
| Male parent (vs. female) | −2.91 (0.87)** | −1.29 (0.86) | −1.26 (0.91) | 0.46 (0.38) | 1.00 (0.67) | −0.44 (0.42) | −4.23 (1.97)* |
| Parent education | 0.09 (0.14) | 0.02 (0.16) | −0.01 (0.18) | −0.13 (0.18) | −0.13 (0.20) | 0.03 (0.14) | 0.41 (0.43) |
| Autism severity | −0.13 (0.15) | 0.01 (0.19) | −0.18 (0.17) | 0.07 (0.16) | −0.09 (0.19) | 0.14 (0.14) | 0.69 (0.48) |
| Behavior problems | −0.05 (0.02)* | −0.07 (0.03)* | −0.05 (0.03)† | −0.07 (0.03)* | −0.06 (0.04) | 0.02 (0.03) | 0.07 (0.07) |
| Post-treatment slope (random) | 1.67 (0.32)*** | 1.52 (0.36)*** | 1.19 (0.32)** | 0.73 (0.24)** | 0.58 (0.39) | −0.22 (0.23) | 0.80 (0.63) |
| P-ESDM+MBSR (vs. P-ESDM) | 1.68 (0.69)* | 1.13 (0.75) | 0.03 (0.69) | 0.46 (0.56) | 0.76 (0.88) | −0.53 (0.54) | −3.18 (1.61)† |
| Child age | 0.83 (0.64) | −1.49 (0.75) † | −0.57 (0.60) | −0.36 (0.54) | 0.28 (0.98) | 1.72 (0.56)** | −0.86 (1.31) |
| Male child (vs. female) | 0.04 (0.83) | 0.64 (0.75) | 0.63 (0.68) | −0.62 (0.71) | 0.72 (0.81) | −1.42 (0.51)** | 1.19 (1.65) |
| Male parent (vs. female) | 4.42 (1.48)** | 1.67 (1.65) | 2.08 (1.52) | −0.30 (0.43) | −1.43 (0.90) | 0.24 (0.55) | 4.41 (1.82)* |
| Parent education | −0.24 (0.25) | −0.10 (0.31) | −0.05 (0.29) | 0.15 (0.23) | 0.25 (0.30) | 0.05 (0.19) | −0.58 (0.49) |
| Autism severity | 0.10 (0.24) | −0.05 (0.30) | 0.27 (0.25) | −0.14 (0.20) | 0.20 (0.27) | −0.15 (0.18) | −0.72 (0.52) |
| Behavior problems | 0.05 (0.04) | 0.06 (0.05) | 0.06 (0.04)† | 0.07 (0.04)† | 0.07 (0.06) | 0.01 (0.04) | −0.16 (0.09)† |
p < .05
p < .01*
p < .001
Note. Slope estimates are additive. Thus, the average slope at follow-up can be calculated by adding the active treatment slope and the post-treatment slope offset (e.g., −1.42 + 1.67 = 0.25 for Parental Distress). PSI = Parenting Stress Index.
Overall change.
Model estimates (including beta-weights and standard errors) for overall change across the sample for each outcome variable are plotted in Figure 2 (see also Table 3). Across the sample, there was statistically significant average improvement during active treatment in all sub-domains of parenting stress (PD, PCDI, DC), depression symptoms, and anxiety symptoms. For the parenting stress subscales and depression symptoms, symptoms worsened slightly during post-treatment data collection (see Figure 2). Change in post-treatment slope for anxiety was not statistically significant, indicating that improvement continued. There were no statistically significant average changes during active treatment or post-treatment in life satisfaction or mindfulness.
Figure 2.
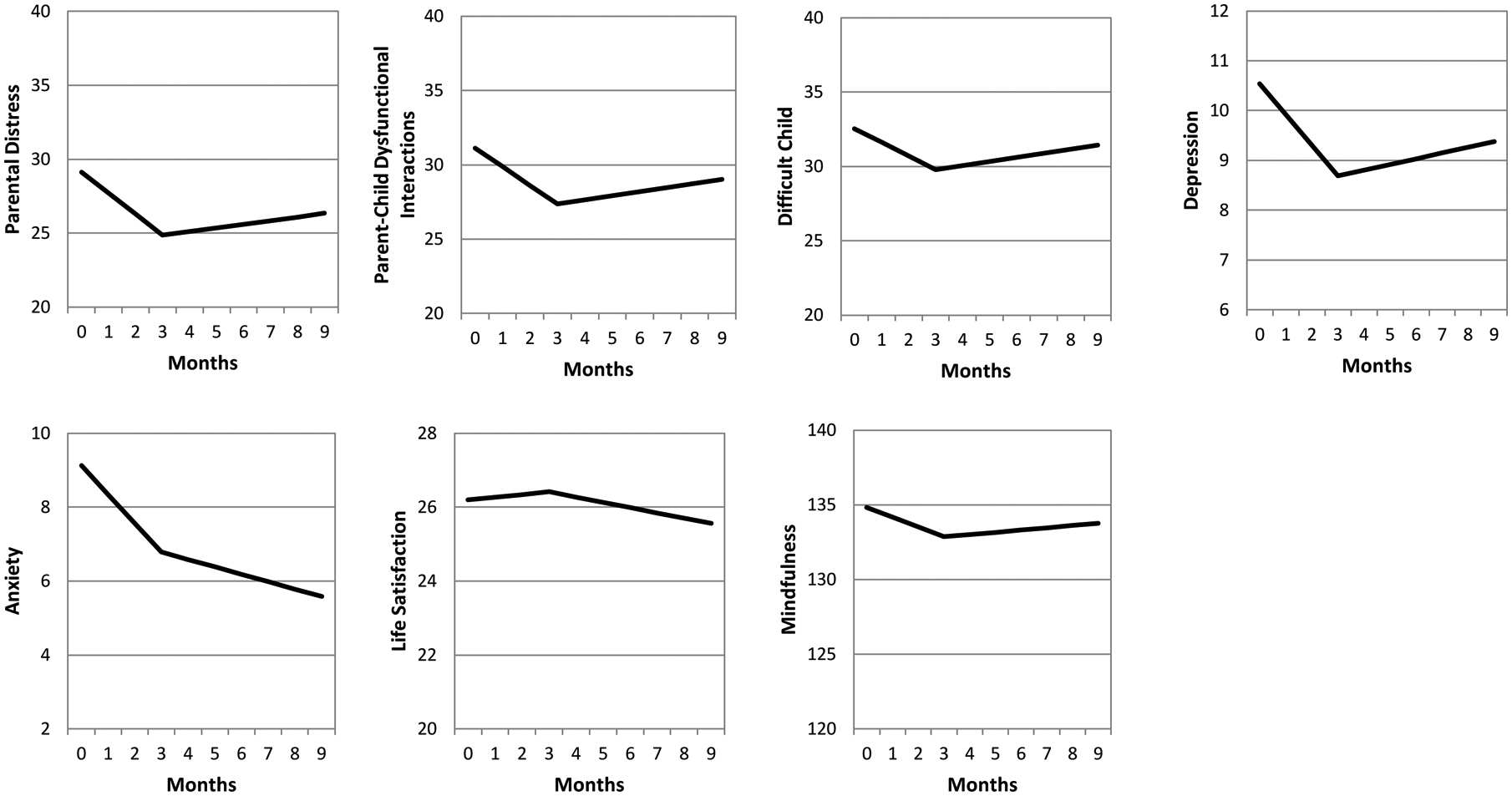
Model score plots showing average change across the sample during active treatment and follow-up
Treatment group differences.
Model estimates (including beta-weights and standard errors) for each outcome variable by treatment condition are plotted in Figure 3 (see also Table 3). Groups were similar at baseline on all outcome variables except for PD. During active treatment, P-ESDM + MBSR had greater improvements than P-ESDM in PD and PCDI. There was also a statistically significant treatment effect on mindfulness, with the P-ESDM + MBSR parents increasing during active treatment and the P-ESDM group declining (see Table 3 and Figure 3). For PD, treatment group significantly impacted the change in slope post-treatment: the P-ESDM + MBSR had greater slowing of improvement post-treatment, resulting in post-treatment slopes similar to the P-ESDM group (see Figure 3). Treatment group did not significantly predict slopes (during active treatment or post-treatment) for DC, depressive symptoms, anxiety symptoms, or life satisfaction.
Figure 3.
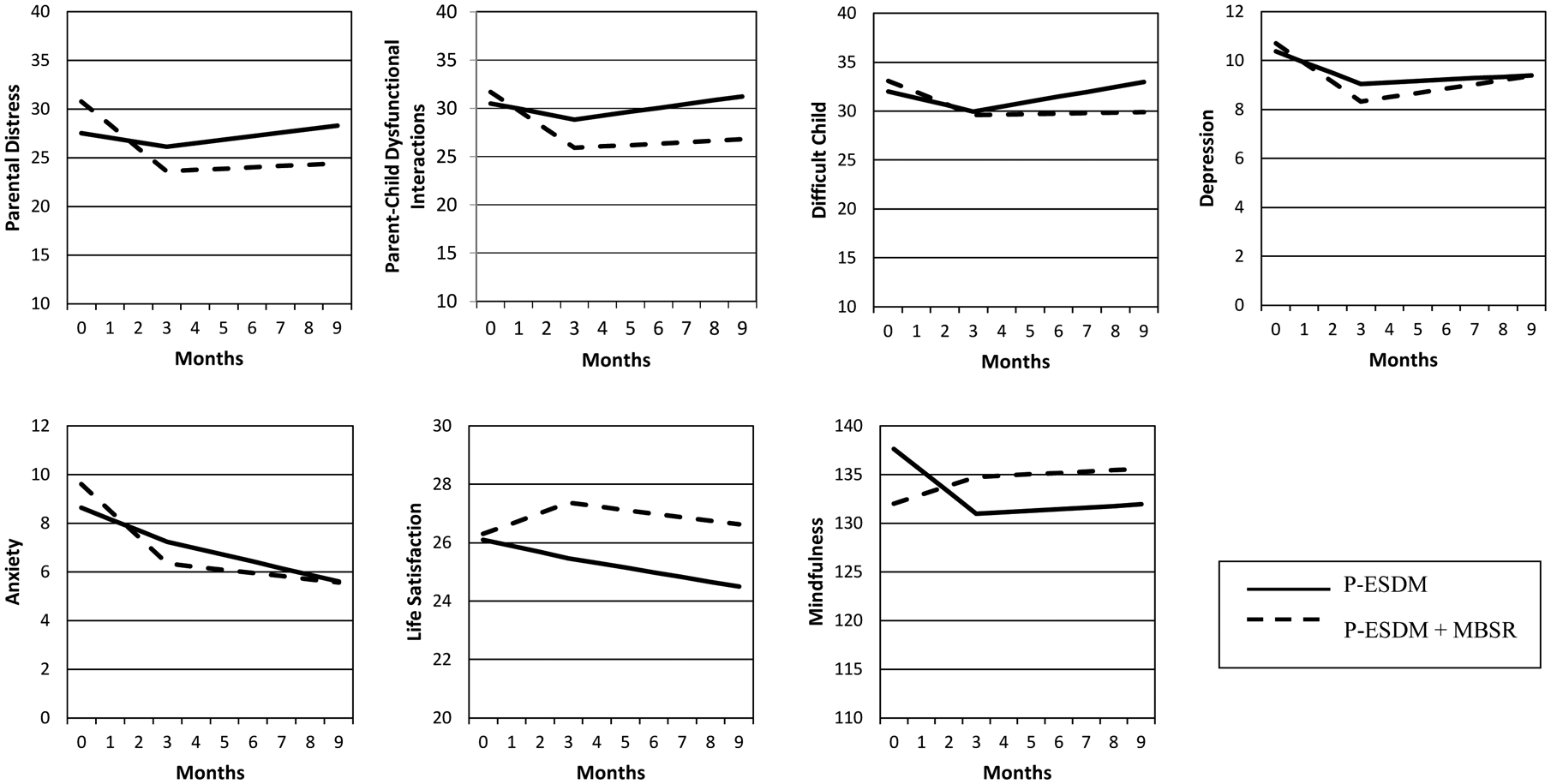
Model score plots showing change during active treatment and follow-up by treatment condition (P-ESDM+MBSR versus P-ESDM) controlling for covariates
Note. Covariates included age the child began treatment, child sex, parent sex, parent education, autism severity, and behavior problems.
Aim 2: Covariate effects on treatment response
A second aim was to examine how key covariates impacted response to treatment. As seen in Table 3, the covariate most consistently related to parental functioning was child behavior problems. Higher levels of behavior problems related to poorer parental functioning on all baseline variables. Relative to parents of children with low behavior problems, parents of those with high behavior problems were higher on PD, PCDI, and depression at baseline, but experienced significantly greater response to intervention during active treatment (see Supplement Figure 1).
Parent sex significantly predicted all estimates of PD (Table 3 and Supplement Figure 2). Relative to mothers, fathers started out with higher PD scores at baseline, improved more rapidly during active treatment, but then had greater slowing of improvement during post-treatment with scores that began rising during this time (whereas mothers stayed more constant during post-treatment). Parent sex also predicted slopes for mindfulness. Only mothers in the P-ESDM + MBSR group increased in mindfulness during active treatment. Fathers declined in mindfulness regardless of treatment group, though that decline was less pronounced if they were in P-ESDM + MBSR. Change was attenuated in all groups during post-treatment.
Child age predicted initial life satisfaction, change in slope during active treatment, and change in slope post-treatment. Parents of younger children at baseline had life satisfaction scores that improved during treatment but then declined post-treatment. Parents of older children showed the opposite pattern, with scores that declined during treatment but improved post-treatment (see Supplement Figure 2).
Other covariates had minimal or no impact on treatment response. The sex of the child predicted post-treatment response for life satisfaction, but not response during active treatment. Child autism severity did not relate to initial status or slopes for any parental outcome variables.
Follow-Up Analyses
In addition to our primary analyses, we ran multi-level models to examine whether the point estimates of parent functioning at the end of active treatment (3 months) and the end of follow-up (9 months) differed by group. To do this, we reran the multi-level models for each outcome that included treatment group and covariates, but changed the intercept from baseline to the 3-month follow-up, and from baseline to the 9-month follow-up. Estimates representing the difference between groups at each of these time points are presented in Table 4. At the end of active treatment, the P-ESDM+MBSR had marginally lower scores on PD and PCDI. These marginally significant differences persisted through the end of follow-up for PCDI. Note that none of the group differences in point estimates reached statistical significance at p < .05.
Table 4.
Relations between group and parent outcomes at 3 months and 9 months after the start of treatment.
| 3 mos. | 9 mos. | |||
|---|---|---|---|---|
| Estimate | Standard Error | Estimate | Standard Error | |
| PSI: Parental Distress | −2.49† | 1.47 | −3.88 | 2.53 |
| PSI: Parent-Child Dysfunctional Interaction | −2.95† | 1.59 | −4.45† | 2.40 |
| PSI: Difficult Child | −0.36 | 1.35 | −3.08 | 1.93 |
| Depressive Symptoms | −0.72 | 1.01 | −0.03 | 1.86 |
| Anxiety Symptoms | −0.89 | 1.81 | −0.05 | 1.52 |
| Life satisfaction | 1.89 | 1.59 | 2.12 | 2.00 |
| Mindfulness | 3.80 | 4.34 | 3.65 | 4.79 |
p < .10
Note. The estimate is the difference between the P-ESDM + MBSR (coded as 1) and P-ESDM (coded as 0) groups.
Discussion
This study provided Mindfulness Based Stress Reduction to the parents of newly diagnosed young children with ASD undergoing low intensity, parent-mediated early behavioral intervention. This combination treatment approach addressed the well-established risk for increased parenting stress and psychopathology while also teaching parents foundational skills for interacting with their children.
Relative to parents who received P-ESDM only, parents who received P-ESDM + MBSR showed significantly greater reductions in parental distress and perceptions of dysfunctional child interactions. Other work has documented that parent training may stabilize65 or reduce66 parenting stress. Our results suggest that giving parents stress reduction strategies may enhance that potential. Although there were differences in rate of change, three months was not long enough for that to translate into statistically significant group differences in parent functioning at the end of treatment. This suggests that detecting specific point-in-time group-level differences may require a larger sample size or prolonged treatment exposure.
Self-rated mindfulness improved for P-ESDM + MBSR but decreased for P-ESDM only. Gains in mindfulness made by the P-ESDM+MBSR group during active treatment were maintained during follow-up, suggesting that the impact of brief, targeted MBSR training may persist past the intervention period. Both groups showed reduced depression and anxiety symptoms during active treatment. However, with the exception of anxiety, most improvements made during active treatment were slowly lost over time, with scores that approached baseline levels by 6-month follow-up. Thus, families may benefit from ongoing treatment to maintain initial gains. This contrasts with the findings of Dykens et al.,14 who noted sustained gains in most outcomes other than anxiety, especially for mothers of children with ASD.
Covariates emerged as significant predictors of some outcome variables. Fathers improved more during active treatment but had greater slowing of improvement during follow-up. Fathers may warrant specific attention within the literature as an understudied group with potentially different pathways of stress and coping.39–41,67–69 Parents who initiated treatment at a younger age reported higher levels of stress and distress at baseline, improved quickly during treatment, but had slowed progress during follow-up relative to slightly older children. Of note, children within our study were on the cusp of transitioning from Part C to Part B services within the Department of Education. The impact of changes in concurrent intervention utilization on parent outcomes will be examined in future publications.
Baseline child behavior problems related to higher baseline levels of parenting stress and depression, as well as more rapid improvements in these outcomes during intervention. It is unclear to what degree this may be a function of all three variables being self-report, or the phenomenon of regression to the mean. The relation between child behavior problems and parenting stress in ASD is well-established70–73 but complex, with recent work suggesting an iterative, interactive process.37 Future work should consider how all of these variables may interact over time, given the potential bidirectional nature of these relationships.37
This initial diagnostic period for very young children represents a critical point worthy of attention. Higher levels of parent stress may impact a family’s ability to obtain and implement intervention.28,46,65 This period also represents an opportunity for increased understanding and relationship building between parents and young children, whose core social and communication symptoms may be especially challenging for parents to interpret. Importantly, however, baseline autism severity did not significantly impact initial scores on parenting outcomes, nor change in outcomes over time. Rather, it was parent-reported levels of behavioral challenges that significantly related to parental stress and depression.
Although this work was longitudinal, its follow-up timeframe was relatively brief. Our sample size was underpowered to conduct sub-group analyses and test mechanisms of treatment response. Several participations were lost to attrition, which was similar across groups and split between families lost to contact and families that moved away. This suggests that adding an extra weekly MBSR visit was not too great a scheduling burden relative to P-ESDM only. Parents were allowed to reschedule missed sessions, which added variability to treatment length. Additionally, analyses included all participants that provided valid data, regardless of level of participation; this provided a more conservative estimate of treatment effects. Though we collected information on fidelity of clinician P-ESDM implementation, fidelity of parent implementation was not tracked, preventing us from drawing conclusions about the impact of MBSR on parents’ treatment implementation. Most participants self-identified as White women, limiting generalizability of results to other groups, and information on parenting self-efficacy was not collected. Most participating families had limited access to high intensity treatments, and it is unclear how MBSR would pair with other intervention models. Also, though random assignment of children to a “no treatment” group would be unethical, without an untreated group questions remain about which longitudinal effects are because of treatment versus maturation or another time-related correlate.
Finally, by nature of the study design, the P-ESDM + MBSR group received more intervention sessions than the P-ESDM group. Thus, it is unclear whether additional parent functioning gains made by the P-ESDM + MBSR group are due to greater attention or to the MBSR program itself. Future work should include attention-matched groups to further evaluate standalone intervention impact. Examining mindfulness as a mediator of treatment on parenting stress will also be important when determining whether MBSR is the mechanism of action, as will investigating the impact of child response to intervention on parent outcomes.
This study suggests that high-quality, low-intensity early intervention was associated with improvements in parental distress and parenting stress. Adding MBSR resulted in further improvements in parenting stress. At no points were parents in P-ESDM + MBSR showing more symptoms of stress than parents in P-ESDM only, suggesting that the additional requirements on parents’ time did not seem to be harmful within this time-limited intervention study. Findings may have implications for systems that partner with parents to care for young children, as well as practitioners that work directly with parents independent of child intervention. Future analyses will explore whether particular profiles of children and families are more amenable to this combination.
Supplementary Material
What’s Known on This Subject:
Parents play an integral role in early intervention for young children with autism spectrum disorder. They also report high levels of stress and psychopathology. Training in mindfulness practice may help parents of older children with ASD.
What This Study Adds:
This pilot randomized controlled trial compares functioning of parents who participated in child-focused, parent-mediated behavioral intervention alone, to parents who also received stress reduction training.
Funding Source:
All phases of this study were supported by the Health Resources & Services Administration Maternal & Child Health Bureau, R40MC27706. Manuscript preparation received core support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (U54 HD08321).
Abbreviations:
- ASD
Autism Spectrum Disorder
- MBSR
Mindfulness Based Stress Reduction
- P-ESDM
Parent-implemented Early Start Denver Model
- ADOS-2
Autism Diagnostic Observation Schedule, Second Edition
- MSEL
Mullen Scales of Early Learning
- VABS-II
Vineland Adaptive Behavior Scales, Second Edition
- PSI
Parenting Stress Index
- PD
Parent Distress
- PCDI
Parent Child Dysfunctional Interaction
- DC
Difficult Child
- BAI
Beck Anxiety Inventory
- CES-D
Center for Epidemiologic Studies Depression Scale
- CBCL
Child Behavior Checklist
- SLS
Satisfaction with Life Scale
- FFMQ
Five Facet Mindfulness Questionnaire
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Potential Conflicts of Interest: The authors have no financial relationships relevant to this article to disclose.
Clinical Trial Registration: This trial has been registered at www.clinicaltrials.gov (identifier NCT03889821).
References
- 1.Landa R Early communication development and intervention for children with autism. Ment Retard Dev Disabil Res Rev. 2007;13(1):16–25. [DOI] [PubMed] [Google Scholar]
- 2.Franchini M, Hamodat T, Armstrong VL, et al. Infants at Risk for Autism Spectrum Disorder: Frequency, Quality, and Variety of Joint Attention Behaviors. J Abnorm Child Psychol. 2018. [DOI] [PubMed] [Google Scholar]
- 3.Sacrey LR, Zwaigenbaum L, Bryson S, et al. Parent and clinician agreement regarding early behavioral signs in 12- and 18-month-old infants at-risk of autism spectrum disorder. Autism Res. 2018;11(3):539–547. [DOI] [PubMed] [Google Scholar]
- 4.Dawson G, Jones EJ, Merkle K, et al. Early behavioral intervention is associated with normalized brain activity in young children with autism. J Am Acad Child Adolesc Psychiatry. 2012;51(11):1150–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rogers SJ, Estes A, Lord C, et al. Effects of a brief Early Start Denver model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2012;51(10):1052–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Estes A, Munson J, Dawson G, Koehler E, Zhou XH, Abbott R. Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism. 2009;13(4):375–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Estes A, Olson E, Sullivan K, et al. Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain Dev. 2013;35(2):133–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fernandez-Alcantara M, Garcia-Caro MP, Perez-Marfil MN, Hueso-Montoro C, Laynez-Rubio C, Cruz-Quintana F. Feelings of loss and grief in parents of children diagnosed with autism spectrum disorder (ASD). Res Dev Disabil. 2016;55:312–321. [DOI] [PubMed] [Google Scholar]
- 9.Jones L, Hastings RP, Totsika V, Keane L, Rhule N. Child behavior problems and parental well-being in families of children with autism: the mediating role of mindfulness and acceptance. Am J Intellect Dev Disabil. 2014;119(2):171–185. [DOI] [PubMed] [Google Scholar]
- 10.Tomeny TS. Parenting stress as an indirect pathway to mental health concerns among mothers of children with autism spectrum disorder. Autism. 2017;21(7):907–911. [DOI] [PubMed] [Google Scholar]
- 11.Weitlauf AS, Vehorn AC, Taylor JL, Warren ZE. Relationship satisfaction, parenting stress, and depression in mothers of children with autism. Autism. 2014;18(2):194–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carter AS, Martinez-Pedraza Fde L, Gray SA. Stability and individual change in depressive symptoms among mothers raising young children with ASD: maternal and child correlates. J Clin Psychol. 2009;65(12):1270–1280. [DOI] [PubMed] [Google Scholar]
- 13.Hamlyn-Wright S, Draghi-Lorenz R, Ellis J. Locus of control fails to mediate between stress and anxiety and depression in parents of children with a developmental disorder. Autism. 2007;11(6):489–501. [DOI] [PubMed] [Google Scholar]
- 14.Dykens EM, Fisher MH, Taylor JL, Lambert W, Miodrag N. Reducing distress in mothers of children with autism and other disabilities: a randomized trial. Pediatrics. 2014;134(2):e454–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valicenti-McDermott M, Lawson K, Hottinger K, et al. Parental Stress in Families of Children With Autism and Other Developmental Disabilities. J Child Neurol. 2015;30(13):1728–1735. [DOI] [PubMed] [Google Scholar]
- 16.Picardi A, Gigantesco A, Tarolla E, et al. Parental Burden and its Correlates in Families of Children with Autism Spectrum Disorder: A Multicentre Study with Two Comparison Groups. Clin Pract Epidemiol Ment Health. 2018;14:143–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carter AS, Messinger DS, Stone WL, Celimli S, Nahmias AS, Yoder P. A randomized controlled trial of Hanen’s ‘More Than Words’ in toddlers with early autism symptoms. J Child Psychol Psychiatry. 2011;52(7):741–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strauss K, Mancini F, Group SPC, Fava L. Parent inclusion in early intensive behavior interventions for young children with ASD: a synthesis of meta-analyses from 2009 to 2011. Res Dev Disabil. 2013;34(9):2967–2985. [DOI] [PubMed] [Google Scholar]
- 19.Wainer AL, Hepburn S, McMahon Griffith E. Remembering parents in parent-mediated early intervention: An approach to examining impact on parents and families. Autism. 2017;21(1):5–17. [DOI] [PubMed] [Google Scholar]
- 20.Green J, Charman T, Pickles A, et al. Parent-mediated intervention versus no intervention for infants at high risk of autism: a parallel, single-blind, randomised trial. Lancet Psychiatry. 2015;2(2):133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schreibman L, Dawson G, Stahmer AC, et al. Naturalistic Developmental Behavioral Interventions: Empirically Validated Treatments for Autism Spectrum Disorder. J Autism Dev Disord. 2015;45(8):2411–2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kasari C, Gulsrud AC, Wong C, Kwon S, Locke J. Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. J Autism Dev Disord. 2010;40(9):1045–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kasari C, Lawton K, Shih W, et al. Caregiver-mediated intervention for low-resourced preschoolers with autism: an RCT. Pediatrics. 2014;134(1):e72–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wetherby AM, Guthrie W, Woods J, et al. Parent-implemented social intervention for toddlers with autism: an RCT. Pediatrics. 2014;134(6):1084–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nevill RE, Lecavalier L, Stratis EA. Meta-analysis of parent-mediated interventions for young children with autism spectrum disorder. Autism. 2018;22(2):84–98. [DOI] [PubMed] [Google Scholar]
- 26.Tarver J, Palmer M, Webb S, et al. Child and parent outcomes following parent interventions for child emotional and behavioral problems in autism spectrum disorders: A systematic review and meta-analysis. Autism. 2019:1362361319830042. [DOI] [PubMed] [Google Scholar]
- 27.Rogers SJ, Estes A, Lord C, et al. A Multisite Randomized Controlled Two-Phase Trial of the Early Start Denver Model Compared to Treatment as Usual. J Am Acad Child Adolesc Psychiatry. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karp EA, Dudovitz R, Nelson BB, et al. Family Characteristics and Children’s Receipt of Autism Services in Low-Resourced Families. Pediatrics. 2018;141(Suppl 4):S280–S286. [DOI] [PubMed] [Google Scholar]
- 29.Carr T, Shih W, Lawton K, Lord C, King B, Kasari C. The relationship between treatment attendance, adherence, and outcome in a caregiver-mediated intervention for low-resourced families of young children with autism spectrum disorder. Autism. 2016;20(6):643–652. [DOI] [PubMed] [Google Scholar]
- 30.Strauss K, Vicari S, Valeri G, D’Elia L, Arima S, Fava L. Parent inclusion in Early Intensive Behavioral Intervention: the influence of parental stress, parent treatment fidelity and parent-mediated generalization of behavior targets on child outcomes. Res Dev Disabil. 2012;33(2):688–703. [DOI] [PubMed] [Google Scholar]
- 31.Hartley SL, Papp LM, Bolt D. Spillover of Marital Interactions and Parenting Stress in Families of Children With Autism Spectrum Disorder. J Clin Child Adolesc Psychol. 2016:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Croen LA, Shankute N, Davignon M, Massolo ML, Yoshida C. Demographic and Clinical Characteristics Associated with Engagement in Behavioral Health Treatment Among Children with Autism Spectrum Disorders. J Autism Dev Disord. 2017;47(11):3347–3357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seymour M, Giallo R, Wood CE. The psychological and physical health of fathers of children with Autism Spectrum Disorder compared to fathers of children with long-term disabilities and fathers of children without disabilities. Res Dev Disabil. 2017;69:8–17. [DOI] [PubMed] [Google Scholar]
- 34.Moody EJ, Reyes N, Ledbetter C, et al. Screening for Autism with the SRS and SCQ: Variations across Demographic, Developmental and Behavioral Factors in Preschool Children. J Autism Dev Disord. 2017;47(11):3550–3561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neuhaus E, Beauchaine TP, Bernier RA, Webb SJ. Child and family characteristics moderate agreement between caregiver and clinician report of autism symptoms. Autism Res. 2018;11(3):476–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McStay RL, Dissanayake C, Scheeren A, Koot HM, Begeer S. Parenting stress and autism: the role of age, autism severity, quality of life and problem behaviour of children and adolescents with autism. Autism. 2014;18(5):502–510. [DOI] [PubMed] [Google Scholar]
- 37.Rodriguez G, Hartley SL, Bolt D. Transactional Relations Between Parenting Stress and Child Autism Symptoms and Behavior Problems. J Autism Dev Disord. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Falk NH, Norris K, Quinn MG. The factors predicting stress, anxiety and depression in the parents of children with autism. J Autism Dev Disord. 2014;44(12):3185–3203. [DOI] [PubMed] [Google Scholar]
- 39.Dardas LA, Ahmad MM. Predictors of quality of life for fathers and mothers of children with autistic disorder. Res Dev Disabil. 2014;35(6):1326–1333. [DOI] [PubMed] [Google Scholar]
- 40.Foody C, James JE, Leader G. Parenting stress, salivary biomarkers, and ambulatory blood pressure: a comparison between mothers and fathers of children with autism spectrum disorders. J Autism Dev Disord. 2015;45(4):1084–1095. [DOI] [PubMed] [Google Scholar]
- 41.McStay RL, Trembath D, Dissanayake C. Stress and family quality of life in parents of children with autism spectrum disorder: parent gender and the double ABCX model. J Autism Dev Disord. 2014;44(12):3101–3118. [DOI] [PubMed] [Google Scholar]
- 42.Bessette Gorlin J, McAlpine CP, Garwick A, Wieling E. Severe Childhood Autism: The Family Lived Experience. J Pediatr Nurs. 2016;31(6):580–597. [DOI] [PubMed] [Google Scholar]
- 43.Hsiao YJ, Higgins K, Pierce T, Whitby PJS, Tandy RD. Parental stress, family quality of life, and family-teacher partnerships: Families of children with autism spectrum disorder. Res Dev Disabil. 2017;70:152–162. [DOI] [PubMed] [Google Scholar]
- 44.Neff KD, and Faso DJ Self-Compassion and Well-Being in Parents of Children with Autism. Mindfulness. 2015;6:938–947. [Google Scholar]
- 45.Davlantis KS, Estes A, Dawson G, Rogers SJ. A novel method for measuring learning opportunities provided by parents to young children with autism spectrum disorder. Autism. 2019:1362361318817303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Watson LR, Crais ER, Baranek GT, et al. Parent-Mediated Intervention for One-Year-Olds Screened as At-Risk for Autism Spectrum Disorder: A Randomized Controlled Trial. J Autism Dev Disord. 2017;47(11):3520–3540. [DOI] [PubMed] [Google Scholar]
- 47.Catalano D, Holloway L, Mpofu E. Mental Health Interventions for Parent Carers of Children with Autistic Spectrum Disorder: Practice Guidelines from a Critical Interpretive Synthesis (CIS) Systematic Review. Int J Environ Res Public Health. 2018;15(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kabat-Zinn J An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry. 1982;4(1):33–47. [DOI] [PubMed] [Google Scholar]
- 49.Da Paz NS, Wallander JL. Interventions that target improvements in mental health for parents of children with autism spectrum disorders: A narrative review. Clin Psychol Rev. 2017;51:1–14. [DOI] [PubMed] [Google Scholar]
- 50.Lunsky Y, R PH, Weiss JA, A MP, Hutton S, White K. Comparative Effects of Mindfulness and Support and Information Group Interventions for Parents of Adults with Autism Spectrum Disorder and Other Developmental Disabilities. J Autism Dev Disord. 2017;47(6):1769–1779. [DOI] [PubMed] [Google Scholar]
- 51.Neece CL. Mindfulness-based stress reduction for parents of young children with developmental delays: implications for parental mental health and child behavior problems. J Appl Res Intellect Disabil. 2014;27(2):174–186. [DOI] [PubMed] [Google Scholar]
- 52.Rayan A, Ahmad M. Effectiveness of mindfulness-based interventions on quality of life and positive reappraisal coping among parents of children with autism spectrum disorder. Res Dev Disabil. 2016;55:185–196. [DOI] [PubMed] [Google Scholar]
- 53.Ridderinkhof A, de Bruin EI, Blom R, Bogels SM. Mindfulness-Based Program for Children with Autism Spectrum Disorder and Their Parents: Direct and Long-Term Improvements. Mindfulness (N Y). 2018;9(3):773–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rogers SJ, Estes A, Vismara L, et al. Enhancing Low-Intensity Coaching in Parent Implemented Early Start Denver Model Intervention for Early Autism: A Randomized Comparison Treatment Trial. J Autism Dev Disord. 2019;49(2):632–646. [DOI] [PubMed] [Google Scholar]
- 55.Kasari C, Gulsrud A, Paparella T, Hellemann G, Berry K. Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. J Consult Clin Psychol. 2015;83(3):554–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–897. [DOI] [PubMed] [Google Scholar]
- 57.Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49(1):71–75. [DOI] [PubMed] [Google Scholar]
- 58.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. [DOI] [PubMed] [Google Scholar]
- 59.Lord C, Risi S, Lambrecht L, et al. The Autism Diagnostic Observation Schedule-Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30(3):205–223. [PubMed] [Google Scholar]
- 60.Mullen EL. Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- 61.Sparrow SS, Cicchetti DV. Diagnostic uses of the Vineland Adaptive Behavior Scales. J Pediatr Psychol. 1985;10(2):215–225. [DOI] [PubMed] [Google Scholar]
- 62.Achenbach TM. Achenbach Child Behavior Checklist. In. Burlington, VT: ASEBA; 2001. [Google Scholar]
- 63.Raudenbush SW, Bryk AS. Hierarchical linear models : applications and data analysis methods Vol 1. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 64.Singer JD, Willett JB. Applied longitudinal data analysis : Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- 65.Estes A, Vismara L, Mercado C, et al. The impact of parent-delivered intervention on parents of very young children with autism. J Autism Dev Disord. 2014;44(2):353–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Iadarola S, Levato L, Harrison B, et al. Teaching Parents Behavioral Strategies for Autism Spectrum Disorder (ASD): Effects on Stress, Strain, and Competence. J Autism Dev Disord. 2018;48(4):1031–1040. [DOI] [PubMed] [Google Scholar]
- 67.Jones L, Totsika V, Hastings RP, Petalas MA. Gender differences when parenting children with autism spectrum disorders: a multilevel modeling approach. J Autism Dev Disord. 2013;43(9):2090–2098. [DOI] [PubMed] [Google Scholar]
- 68.Langley E, Totsika V, Hastings RP. Parental relationship satisfaction in families of children with autism spectrum disorder (ASD): A multilevel analysis. Autism Res. 2017;10(7):1259–1268. [DOI] [PubMed] [Google Scholar]
- 69.Hastings RP, Kovshoff H, Ward NJ, degli Espinosa F, Brown T, Remington B. Systems analysis of stress and positive perceptions in mothers and fathers of pre-school children with autism. J Autism Dev Disord. 2005;35(5):635–644. [DOI] [PubMed] [Google Scholar]
- 70.Shattuck PT, Seltzer MM, Greenberg JS, et al. Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. J Autism Dev Disord. 2007;37(9):1735–1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lounds J, Seltzer MM, Greenberg JS, Shattuck PT. Transition and change in adolescents and young adults with autism: longitudinal effects on maternal well-being. Am J Ment Retard. 2007;112(6):401–417. [DOI] [PubMed] [Google Scholar]
- 72.Argumedes M, Lanovaz MJ, Larivee S. Brief Report: Impact of Challenging Behavior on Parenting Stress in Mothers and Fathers of Children with Autism Spectrum Disorders. J Autism Dev Disord. 2018;48(7):2585–2589. [DOI] [PubMed] [Google Scholar]
- 73.Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res. 2006;50(Pt 3):172–183. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


