Abstract
Children’s hospitals responded to COVID-19 by limiting nonurgent healthcare encounters, conserving personal protective equipment, and restructuring care processes to mitigate viral spread. We assessed year-over-year trends in healthcare encounters and hospital charges across US children’s hospitals before and during the COVID-19 pandemic. We performed a retrospective analysis, comparing healthcare encounters and inflation-adjusted charges from 26 tertiary children’s hospitals reporting to the PROSPECT database from February 1 to June 30 in 2019 (before the COVID-19 pandemic) and 2020 (during the COVID-19 pandemic). All children’s hospitals experienced similar trends in healthcare encounters and charges during the study period. Inpatient bed-days, emergency department visits, and surgeries were lower by a median 36%, 65%, and 77%, respectively, per hospital by the week of April 15 (the nadir) in 2020 compared with 2019. Across the study period in 2020, children’s hospitals experienced a median decrease of $276 million in charges.
To benefit patients and the public health of their communities, children’s hospitals across the United States prepared for and responded to COVID-19 by conserving personal protective equipment, suspending noncritical in-person healthcare encounters (including outpatient visits and elective surgeries), and implementing socially distanced essential care.1,2 These measures were promptly instituted during a time of both substantial uncertainty about the pandemic’s behavior in children—including its severity and duration—and extreme variation in local and state governments’ responses to the pandemic.
Congruent with other healthcare institutions, children’s hospitals calibrated their clinical operations to the evolving nature of the pandemic, prioritizing the safety of patients and staff while striving to maintain financial viability in the setting of increased costs and decreased revenue. In some cases, children’s hospitals aided adult hospitals and health systems by admitting young and middle-aged adult patients and by centralizing all pediatric patients requiring intensive care within a region. These efforts occurred while many children’s hospitals remained the sole source of specialized pediatric care, including care for rare complex health problems.
As the COVID-19 pandemic continues, there is a critical need to assess how the initial phase of the pandemic affected healthcare encounters and related finances in children’s hospitals. Understanding these trends will position children’s hospitals to project and prepare for subsequent COVID-19 surges, as well as future related public health crises that necessitate widespread social distancing. Therefore, we compared year-over-year trends in healthcare encounters and hospital charges across US children’s hospitals before and during the COVID-19 pandemic, focusing on the beginning of COVID-19 in the United States, which was defined as February through June 2020.
METHODS
This is a retrospective analysis of 26 children’s hospitals (22 freestanding, 4 nonfreestanding) from all US regions (12 South, 7 Midwest, 5 West, 2 Northeast) contributing encounter and financial data to the PROSPECT database (Children’s Hospital Association, Lenexa, Kansas) from February 1 to June 30 in both 2019 (before COVID-19) and 2020 (during COVID-19). In response to COVID-19, hospitals participating in PROSPECT increased the efficiency of data centralization and reporting in 2020 during the period February 1 to June 30 to expedite analysis and dissemination of findings.
The main outcome measures were the percentage of change in weekly encounters (inpatient bed-days, emergency department [ED] visits, and surgeries) and inflation-adjusted charges (categorized as inpatient care and outpatient care, such as ambulatory surgery, clinics, and ED visits) before vs during COVID-19. Number of encounters and charges were compared using the Wilcoxon signed-rank test. The distribution of weekly change in outcome measures from 2019 vs 2020 across hospitals was reported with medians and interquartile ranges (IQRs). The threshold of statistical significance was set at P < .05. All analyses were performed with SAS version 9.4 (SAS Institute). This study was considered exempt from human subjects research by the Institutional Review Board of Children’s Mercy Hospital (Kansas City, Missouri).
RESULTS
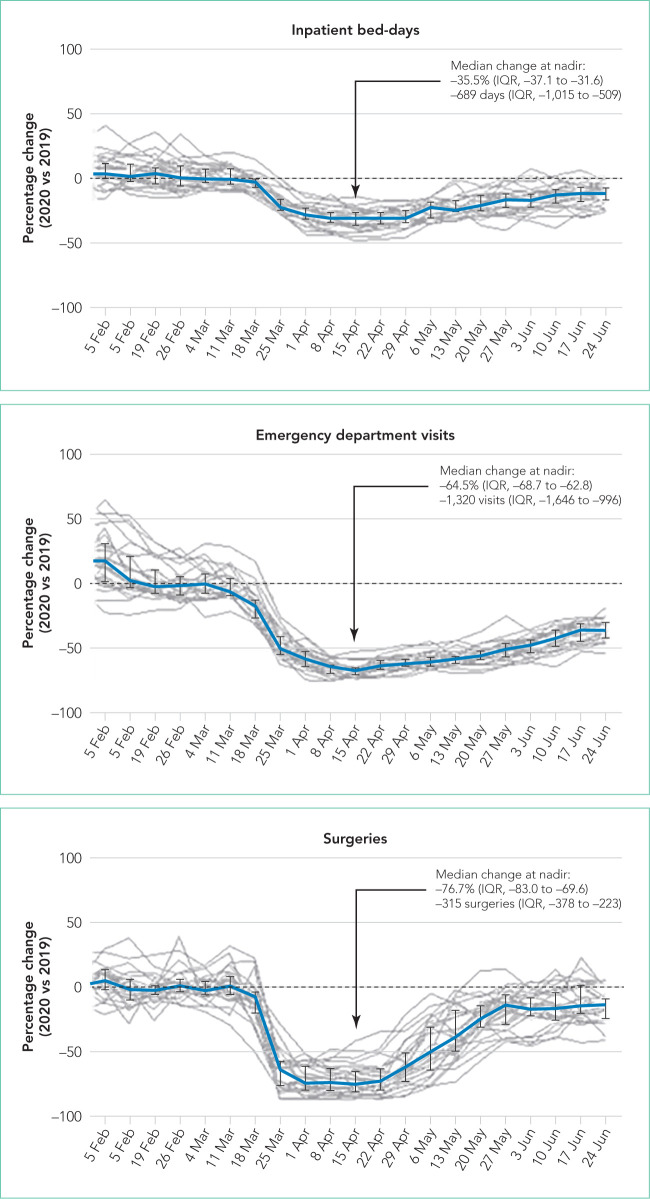
All 26 children’s hospitals experienced similar trends in healthcare encounters and charges during the study period (Figure and Table). From February 1 to March 10, 2020, the volume of healthcare encounters in the children’s hospitals remained the same as that for the same period in 2019 (P > .1) (Figure). Compared with 2019, a significant decrease in healthcare encounters began around the week of March 18, 2020, with a nadir observed around April 15. Although the timing of the nadir was similar across health services, its magnitude varied. Inpatient bed-days, ED visits, and surgeries were lower than in 2019 by a median of 36%, 65%, and 77%, respectively, per hospital during the week of the nadir. Following the nadir, inpatient bed-days and ED encounters increased modestly, returning to –12% and –25% of 2019 volumes by June 30. Surgery encounters increased more intensely, returning to –13% of 2019 volumes by June 30. Compared with 2019, a median 2,091 (IQR 1,306-3,564) fewer surgeries were performed during the study period in 2020.
FIG.
February Through June Trends in 2019 vs 2020 for Inpatient Bed-Days, Emergency Department (ED) Visits, and Surgeries in 26 US Children’s Hospitals. Daily counts for encounters were summed weekly and reported on the Wednesday of each week. The relative differences in 2020 vs 2019 encounters across hospitals, expressed as median change, are plotted in blue with interquartile ranges (IQR; bars). Individual trends for each hospital are presented in grey. Nadir for each service is marked with an arrow; percentage of change and absolute value change at arrow are reported. Changes from 2020 vs 2019 became and remained statistically significant at P < .001 throughout the study period for ED visits and surgeries beginning the week of March 18 and inpatient bed-days beginning March 25. The only exception to this was the week of June 17, when surgical volume was not significantly different in 2020 vs 2019.
TABLE.
Trends in Charges of Health Services in 26 US Children’s Hospitals: February Through June in 2019 vs 2020
| Health Service | Charge Comparison | Comparison of Median (IQR) Charges Per Hospital From 2020 vs 2019a,b | |||||
|---|---|---|---|---|---|---|---|
| By Month | Aggregate | ||||||
| February | March | April | May | June | February-June | ||
| Inpatient | US $, Millions | –4.2 (–11.6 to 1.6) |
–11.0 (–18.3 to –4.9) |
–57.2 (–73.4 to –27.6) |
–27.4 (–39.0 to –15.6) |
–19.4 (–37.8 to –8.7) |
–109.7 (–161.4 to –58.1) |
| Percentage | –4.9% (–8.6 to 2.0) |
–11.4% (–15.5 to –5.7) |
–33.6% (–38.0 to –29.4) |
–22.2% (–29.9 to –16.7) |
–18.8% (–23.8 to –7.8) |
–18.9% (–20.5 to –13.8) |
|
| Outpatientc | US $, Millions | –3.1 (–10.0 to 5.6) |
–16.6 (–36.1 to –7.3) |
–86.4 (–110.2 to –41.0) |
–29.6 (–46.8 to –14.9) |
–14.3 (–39.4 to –7.1) |
–153.6 (–259.4 to –78.1) |
| Percentage | –3.0% (–11.0 to 7.4) |
–20.7% (–27.8 to –12.6) |
–63.2% (–67.3 to –55.3) |
–38.0% (–47.1 to –27.7) |
–20.3% (–33.6 to –10.3) |
–29.3% (–40.6 to –25.7) |
|
| Total | US $, Millions | –5.9 (–23.0 to 6.3) |
–24.8 (–49.7 to –12.1) |
–146.8 (–174.5 to –67.3) |
–68.9 (–85.7 to –27.4) |
–37.6 (–64.7 to –15.8) |
–276.3 (–404.0 to –126.0) |
| Percentage | –4.7% (–9.1 to 2.7) |
–14.7% (–19.4 to –9.4) |
–46.9% (–51.0 to –40.2) |
–29.0% (–35.5 to –24.0) |
–19.0% (–26.9 to –11.3) |
–23.6% (–28.7 to –19.1) |
|
Charges were summed across each day and reported monthly. Charges from 2019 were inflated using the ratio of total charges in January 2020 to those in January 2019 for each hospital.
All comparisons of charges were statistically significant between 2019 and 2020 at P < .001.
Outpatient health services included ambulatory surgery, clinic, and emergency department visits and observation-status admissions.
Charges that accrued from February 1 to June 30 were lower in 2020 by a median 23.6% (IQR, –28.7% to –19.1%) per children’s hospital than they were in 2019, corresponding to a median decrease of $276.3 million (IQR, $404.0-$126.0 million) in charges per hospital (Table). Forty percent of this decrease was attributable to decreased charges resulting from fewer inpatient healthcare encounters.
DISCUSSION
During the initial phase of the COVID-19 pandemic in the United States, children’s hospitals experienced a substantial decrease in healthcare encounters and charges. Greater decreases were observed for ED visits and surgery encounters than for inpatient bed-days. Nonetheless, inpatient bed-days decreased by more than one-third, consistent with the decrease in inpatient resource use reported for adult hospitals.3 Remarkably, these trends were consistent across children’s hospitals, despite variation in the content and installation of and adherence with social distancing policies in their surrounding local areas.
These findings beg the question of how well children’s hospitals are positioned to weather a recurrent surge in COVID-19. Because the severity of illness of COVID-19 has been lower to date in the pediatric vs adult populations, an increase in COVID-19-related visits to EDs and admissions to offset the decreased resource use of other pediatric healthcare problems is not anticipated. Existing hospital financial reserves as well as federal aid from the Coronavirus Aid, Relief, and Economic Security Act that helped mitigate the initial encounter and financial losses during the beginning of COVID-19 may not be readily available over time.4,5 Certainly, the findings from the current study support continued lobbying for additional state and federal funds allocated through future relief packages to children’s hospitals.
Additional approaches to financial solvency in children’s hospitals during the sustained COVID-19 pandemic include addressing surgical backlogs and sharing best practices for safe and sustained reopening of clinical operations and financial practices across institutions. Although the PROSPECT database does not contain information on the types of surgeries present within this backlog, our experiences suggest that both same-day and inpatient elective surgeries have been affected, especially lengthy procedures (eg, spinal fusion for neuromuscular scoliosis). Spread and scale of feasible and efficient solutions to reengineer and expand patient capacities and throughput for operating rooms, postanesthesia recovery areas, and intensive care and floor units are needed. Enhanced analytics that accurately predict postoperative length of hospital stay, coupled with early recovery after surgery clinical protocols, could help optimize hospital bed management. Effective ways to convert hospital rooms from single to double occupancy, to manage family visitation, and to proactively test asymptomatic patients, family, and hospital staff will mitigate continued COVID-19 penetration through children’s hospitals.
One important limitation of the current study is the measurement of hospitals’ charges. The charge data were not positioned to comprehensively measure each hospital’s financial state during the COVID-19 pandemic. However, the decrease in hospital charges reported by the children’s hospitals in the current study is comparable with the financial losses reported for many adult hospitals during the pandemic.6,7 It is important to recognize that the amount of the charges may not be equivalent to the cost of care or revenue collected by the hospitals. PROSPECT does not contain information on cost, and current cost-to-charge ratios are based on historical (ie, pre-COVID-19) data; therefore, they do not account for increased cost of personal protective equipment and other related costs that occurred during the pandemic, which makes use of these ratios challenging. Nevertheless, it is possible that the relative difference in costs incurred and revenue collected before and during COVID-19 may have been similar to the differences observed in hospital charges.
CONCLUSION
Children’s hospitals’ ability to serve the nation’s pediatric patients depends on the success of the hospitals’ plans to manage current and future COVID-19 surges and to reopen and recover from the surges that have passed. Additional investigation is needed to identify best operational and financial practices among children’s hospitals that have enabled them to endure the COVID-19 pandemic.
Footnotes
Disclosures: Dr Williams is the recipient of grants from the Centers for Disease Control and Prevention, National Institutes of Health, and Agency for Healthcare Research and Quality, payable to his institution, and nonfinancial support to the institution from Biomerieux, all outside the submitted work. Dr Auger is the recipient of a K08 grant from the National Institutes of Health Agency for Healthcare Research and Quality, payable to her institution. The other authors have nothing to disclose.
References
- 1.Children’s Hospital Association; Mar 12, 2020. [Accessed June 30, 2020]. COVID-19: ways to prepare your children’s hospital now. https://www.childrenshospitals.org/Newsroom/Childrens-Hospitals-Today/Articles/2020/03/COVID-19-11-Ways-to-Prepare-Your-Hospital-Now. [Google Scholar]
- 2.Chopra V, Toner E, Waldhorn R, Washer L. How should U.S. hospitals prepare for coronavirus disease 2019 (COVID-19)? Ann Intern Med. 2020;172(9):621–622. doi: 10.7326/m20-0907. doi: 10.7326/m20-0907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oseran AS, Nash D, Kim C, et al. Changes in hospital admissions for urgent conditions during COVID-19 pandemic. Am J Manag Care. 2020;26(8):327–328. doi: 10.37765/ajmc.2020.43837. doi: 10.37765/ajmc.2020.43837. [DOI] [PubMed] [Google Scholar]
- 4.Coronavirus Aid, Relief, and Economic Security Act or the CARES Act. 15 USC Chapter 116 (2020). Pub L No. 116-36, 134 Stat 281. https://www.congress.gov/bill/116th-congress/house-bill/748
- 5.US Department of Health Human Services; Jun 25, 2020. [Accessed June 30, 2020]. The Coronavirus Aid, Relief, and Economic Security (CARES) Act Provider Relief Fund: general information. https://www.hhs.gov/coronavirus/cares-act-provider-relief-fund/general-information/index.html. [Google Scholar]
- 6.American Hospital Association; May, 2020. [Accessed July 13, 2020]. Hospitals and health systems face unprecedented financial pressures due to COVID-19. https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf. [Google Scholar]
- 7.Birkmeyer J, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood) 2020;39(11):2010–2017. doi: 10.1377/hlthaff.2020.00980. doi: 10.1377/hlthaff.2020.00980. [DOI] [PMC free article] [PubMed] [Google Scholar]