Abstract
Over the years, a number of authors have used different working definitions of instability in tuberculosis of the spine (TB spine). However, no clear consensus exists to define instability in TB spine. The current systematic review addresses the question ‘What defines instability in TB spine’?
A comprehensive medical literature search was carried out to identify all the studies which defined instability in the setting of spinal TB. The extracted data included the clinical, X-ray and CT or MRI-based definitions.
The current review identified lesser age, junctional region of the spine, mechanical pain and ‘instability catch’, kyphotic deformity above 40 degrees, pan-vertebral or bilateral facetal involvement and multifocal contiguous disease involving more than three vertebrae as predictors for spinal instability in the dorso-lumbar spine.
Cervical kyphosis more than 30 degrees and facetal or pan-vertebral involvement were found to be the factors used to define instability in subaxial cervical spine.
With respect to C1–C2 TB spine, migration of the tip of the odontoid above the McRae or McGregor line or anterior translation of C1 over C2 were considered as determinants for instability.
Although definitive conclusions could not be drawn due to lack of adequate evidence, the authors identified factors which may contribute towards instability in TB spine.
Cite this article: EFORT Open Rev 2021;6:202-210. DOI: 10.1302/2058-5241.6.200113
Keywords: deformity, instability, kyphosis, spinal tuberculosis, systematic review, tuberculosis
Introduction
Spinal instability constitutes an important indication for surgical stabilization in a number of spinal pathologies. Since the time of the description of the ‘middle path regime’ by Tuli in 1975, spinal instability has constituted an absolute indication for surgical management in tuberculosis of the spine (TB spine).1,2 Over the years, a number of authors have used different working definitions for spinal instability in TB. However, no clear consensus exists to date. Lack of a uniformly accepted working definition for instability in TB spine creates a wide variability in the surgical decision making in patients especially with no or minimal neurological deficit. Moreover, lack of an objective criteria to define instability in TB spine may lead to under-diagnosis of instability, especially in centres with limited exposure and relative inexperience of the treating physician. The consequences of under-diagnosis in such a scenario may be unforgiving, particularly if complicated with a rapid onset of neurological deficit which is found to have a poor prognosis with respect to neurological recovery. Additionally, mechanical instability is also an important source of severe pain in TB spine and does not resolve with anti-tubercular therapy (ATT). Therefore, it is imperative to define instability in the context of TB spine. The authors of the current article have employed a systematic review methodology to evaluate the factors considered by various researchers to define mechanical instability in TB spine.
Material and methods
The current systematic review aims to addresses the question ‘What defines mechanical instability in TB spine’?
Inclusion/exclusion criteria
The inclusion criteria were defined under three broad categories: study population, independent variable and outcome measured. With respect to the study population, the studies included described patients with TB spine. The independent variables included the epidemiological, clinical and radiological parameters in patients affected by TB spine whereas the measured outcome was considered as the definition of spinal instability in TB spine. Studies which did not include a clinical or radiological definition for instability in TB spine were excluded.
Literature search to identify primary studies
A comprehensive medical literature search was carried out to identify all the studies that matched the inclusion criteria. An electronic database search of Medline and Embase was performed using a combination of medical subject headings (MeSH) and text words. The MeSH search terms included “Tuberculosis, spine”, “Fusion, spinal” and “Surgical procedures, operative” whereas the non-MeSH terms included “Surgical management”, “Surgical indications”, “indications”, “Spine instability”, “Unstable” and “Collapse”. Various combinations of MeSH and non-MeSH search terms were used to carry out the literature search as shown in Table 1. Further, reference lists from all the included articles were searched for additional studies that met the inclusion criteria.
Table 1.
Search methodology used for literature search
| 1. (((Tuberculosis, spine) AND Surgical indications) AND fusion, spinal) AND Instability |
| 2. (((Tuberculosis, spinal) AND Fusion, spinal) AND surgical management) AND unstable |
| 3. ((Tuberculosis, spinal) AND surgical indications) AND instability |
| 4. ((Tuberculosis, spinal) AND Fusion, spinal) AND instability |
| 5. ((Tuberculosis, spinal) AND Fusion, spinal) AND collapse |
| 6. ((Tuberculosis, spinal) AND surgical management) OR surgical indications |
| 7. ((Tuberculosis, spinal) AND ((surgical management) OR surgical indications)) AND (((collapse) OR unstable) OR instability) |
Study selection
All the included studies were independently reviewed by two reviewers (KA and PK). Both the reviewers were fellowship-trained spine surgeons with considerable experience in the management of TB spine patients in a tertiary care teaching hospital. A special emphasis was laid on the description of instability in the included articles. At the first step for screening, all the articles in languages other than English and any duplicated articles were excluded. This was followed by abstract review, where irrelevant studies were excluded. Finally, a detailed review of the complete reports of the remaining studies was carried out to exclude articles with no description of spinal instability. Disagreements between the two reviewers were resolved by including a third reviewer (SI) followed by a discussion.
Quality assessment
The included studies were subject to quality assessment by two independent reviewers after blinding the authors and their affiliations. The quality assessment tool used by the authors has been used previously by researchers in systematic reviews (Table 2).3 Based on the score, the included studies were classified in two categories – ‘good’ with scores more than 50% and ‘average’ with scores less than 50%. Disagreements between the two reviewers were resolved by including a third reviewer (SI) followed by a discussion.
Table 2.
The methodological quality assessment tool used to rate studies derived from the literature search3
| Is there a clear statement of purpose? |
| Was the study design a randomized controlled trial or a prospective cohort? |
| Was the assessor blinded? |
| Is the outcome defined and method of diagnosis stated? |
| Did the authors account for every patient (or sample) that was eligible but was not entered? |
| Is the method clearly defined and replicable? |
| Were all patients (or samples) accounted for? |
| Were outcome measures relevant to the primary question? |
| Was statistical significance considered? |
| Were tests applied appropriately? |
| Was sample size calculated prior to study? |
| Were the results/conclusions clinically significant? |
Data extraction
Data were extracted manually and included the clinical, X-ray and CT or MRI-based definitions used in the included studies to define spinal instability in TB spine (Table 3).
Table 3.
Included studies describing spinal instability in terms of clinical symptoms and radiological finding
| Authors | Clinical criteria | X-ray criteria | CT/MRI criteria |
|---|---|---|---|
| 1. Nene A, Bhojraj S 20054
2. Bhojraj S, Nene A 20025 |
Severe back pain, paraspinal muscle spasm, painfully restricted movements of the thoracolumbar spine and an ‘instability catch’ | Kyphosis in dorsal > 40 degrees | – |
| 3. Jain AK 20026
4. Jain AK 20107 |
– | Pan-vertebral involvement as suggested on plain radiographs by associated scoliosis, severe kyphosis, or both | The CT and MRI scans show global destruction of the vertebral body |
| 5. Jain AK, Dhammi IK 20078 | – | Long-segment disease (more than three-vertebral-body affection) with severe kyphosis or an increasing kyphosis in active disease. The spine with tuberculosis is also unstable when facets and posterior complex are destroyed along with vertebral bodies (pan-vertebral lesion). | CT/MRI shows destruction of anterior and posterior column of the vertebral bodies |
| 6. Rajasekaran S 20019 | – | Spinal instability score: dislocation of the facets, posterior retropulsion of the diseased fragments, lateral translation of the vertebrae in the anteroposterior view and toppling of the superior vertebra | – |
| 7. Rajasekaran S 201310
8. Rajasekaran S 201211 |
An age below 10 years | Vertebral body loss of more than 1–1.5, A pre-treatment deformity angle of greater than 30°, especially in children, cervical thoracic and thoracolumbar junctional lesions, the presence of ‘spine-at-risk’ radiological signs | – |
| 9. Shetty AP et al 201712 | – | Instability: vertebral loss of more than 30%, translational displacement and kyphosis of more than 30 degrees | – |
| 10. Chandra SP et al 201313 | Severe incapacitating pain | Instability: destruction of all the 3 columns, deformity > 40° | Severe cord compression (> 50%) |
| 11. Jutte PC, van Loenhout-Rooyackers JH 200614 | – | Destruction or collapse of the vertebrae, destruction of two or more vertebrae, or kyphosis of more than 30° | – |
| 12. Hou K et al 201515 | Atlantoaxial dislocation or subluxation during the course of Step II | ||
| 13. He M et al 201416 | Cervical kyphosis > 30° | ||
| 14. Djientcheu VP et al 201317 | Injury to the disc, there was lysis of the adjacent vertebral end plates, resulting in collapse of the vertebrae of more than 50% (Fig. 1) or an associated deformity | ||
| 15. Mehta JS, Bhojraj SY 200118 | Kyphosis > 30° and involvement of both anterior and posterior column at the same level | ||
| 16. Kandwal P et al 201219 | Anteroposterior or lateral translation; kyphosis | ||
| 17. Chaudhary K et al 201220 | AP instability – posterior arch of C1 was anterior to the extrapolated spino-laminar line. Vertical instability (basilar impression) – tip of odontoid process (or projected tip in cases with odontoid destruction) was above the McRae line with gross destruction of the lateral weight-bearing columns (lateral mass of atlas and occipital condyles). | ||
| 18. Jain AK, Jain S 201221 | Two of three columns involved with pathological fracture. Junctional area (CD, DL, LS) | ||
| 19. Jain AK 200822 | Pan-vertebral disease, involvement of 3 or destruction of more than one and a half, predicted kyphosis more than 60 degrees | ||
| 20. Bapat MR et al 200723 | Atlanto-dens interval of more than 8 mm was observed in all cases (range 8–16 mm). A vertical migration was considered significant if the dens was located 4 mm above the McGregor line (n = 16). Rotatory dislocation was seen on the open mouth radiograph. | ||
| 21. Christodoulou AG et al 200624 | Structural destruction of the anterior and middle vertebral columns | ||
| 22. Nussbaum ES et al 199525 | Extensive destruction of vertebral body | ||
Statistical analysis
All the included studies were reviewed for data extraction; however, only ‘good’ quality studies were used for final compilation of the results to ensure valid results. Only a systematic review could be performed due to lack of homogenous data and high-quality randomized control trials (RCTs).
Results
Details of the included studies
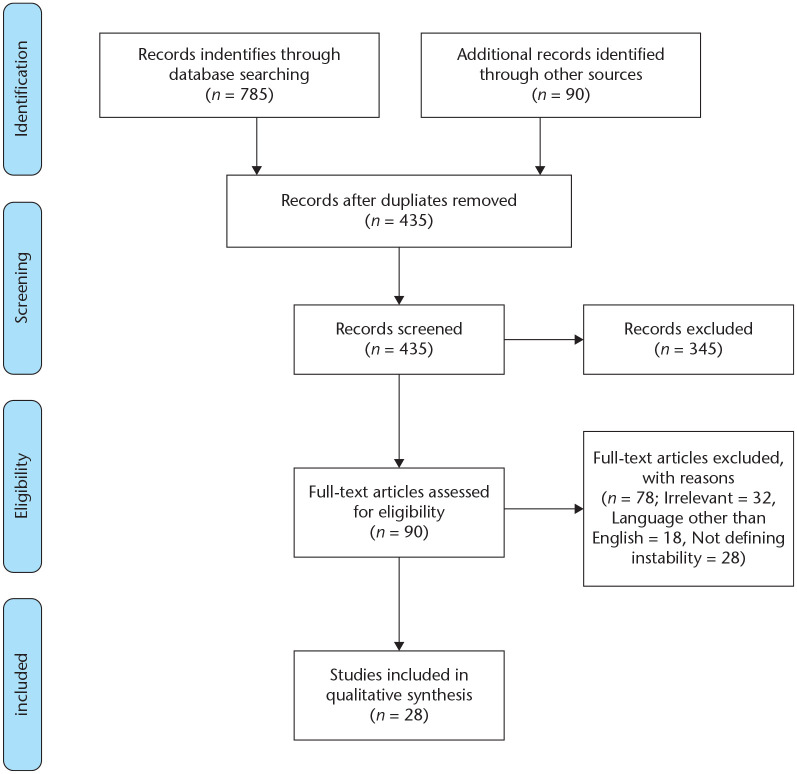
A literature search for the potential studies was carried out in May 2020 and 435 studies were identified after excluding duplicated studies. Further, irrelevant studies and articles in languages other than English were excluded and relevant studies from the references of the included studies were also added. Subsequently 90 studies were short-listed for full-text analysis by the authors. Of 90 short-listed studies, 22 studies were selected for final evaluation after exclusion of articles with partial or no mention of the concept of spinal instability (Fig. 1). Of the included studies, four evaluated various aspects of TB in the cervical spine whereas 18 evaluated dorso-lumbar and sacral spinal TB.
Fig. 1.
PRISMA flowchart for study selection.
Methodological qualitative assessment
Of the included 22 articles, three were narrative reviews and 19 were found to be clinical studies. All 19 studies were classified as good by the reviewers, however, most of the studies had glancing lacunae such as lack of a prospective or an RCT design, ambiguities in inclusion and outcome criteria and limited information about loss to follow-up. Moreover, none of the studies evaluated the instability in TB spine as the primary objective.
Features attributed to instability in selected studies (Table 4)
Table 4.
List of factors predictive of spinal instability in tuberculosis of the spine
| Variables | Risk | Number of times discussed in literature |
|---|---|---|
| Age | Higher in younger age | 3 |
| Location (junctional, cervico-dorsal, dorso-lumbar, lumbo-sacral) | Higher in junctional region | 4 |
| Pain (mechanical on loading and movements, relieved on recumbency) | Higher with more pain | 2 |
| Pan-vertebral involvement (suggested by translation or scoliosis or direct evidence on CT/MRI) | Higher | 9 |
| Kyphosis | Higher with increasing deformity | 8 |
| Multilevel-contiguous (more than three levels involved) | Higher | 2 |
Age
Rajasekaran has considered young age to be an important predictor for the progression of deformity. The immaturity and flexibility of paediatric spine may render spine unstable even in the presence of minor deformity and consequently may lead to progressive kyphosis especially in the presence of ‘spine at risk’ signs (Fig. 2).11 He identified three categories of paediatric spinal TB based on progression of kyphosis – Type 1 showing an increase in deformity until growth had ceased, Type 2 showed a decrease in the deformity with growth whereas Type 3 showed minimal change in active or healed phases and was seen with limited destruction.10,26 Finally, paediatric patients with TB spine were found to have a higher degree of deformity at presentation and a greater tendency of collapse during the active phase of the disease.11
Fig. 2.
Thirteen-year-old girl with tuberculosis of the spine (TB spine) demonstrating ‘spine at risk’ signs such as lateral translation and facet separation/subluxation at the transitional dorso-lumbar region suggesting TB spine instability. The girl presented without any neurological deficits, but should undergo surgical stabilization.
Location of the disease
The region of the spine involved was considered an important predictor for spinal instability in four of the 22 articles by three different authors. The presence of spinal TB with vertebral destruction at the junction between a rigid and a flexible region of spine such as the cervico-dorsal, dorso-lumbar or lumbo-sacral regions of the spine led to exaggerated displacements under normal axial or rotatory movements leading to significant pain or neurological deficit (Fig. 2).
Clinical features
Of 22, two articles were found to describe diagnosis of instability on a clinical basis. Nene and Bhojraj in their articles describing management of dorsal and lumbo-sacral TB focussed on clinical findings such as severe back pain, paraspinal muscle spasm, painful restriction of movements and an ‘instability catch’ as described previously for degenerative spinal pathologies to diagnose instability. Instability catch has been described as a sudden painful ‘snap’ that occurs when one extends from a forward bent to an upright position.27 In their series, they diagnosed the presence of instability using clinical features in about 10–13% of their patients with TB spine. Other researchers have clinically defined instability by the presence of persistent pain or pain on spinal loading.
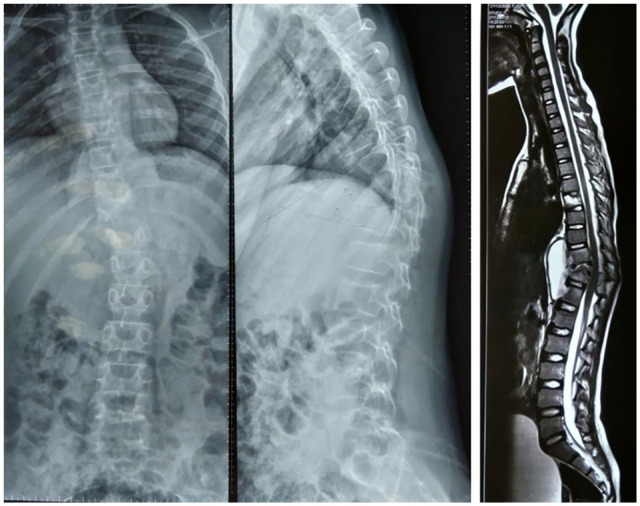
Kyphosis (Fig. 3)
Fig. 3.

Eighteen-year-old boy with dorso-lumbar tuberculosis of the spine (TB spine). The boy presented with intact neurology but involvement of posterior elements and facet joints imparts significant instability to the spine. Also note the significant kyphosis at the dorso-lumbar junctional region. Surgical stabilization is necessary to prevent progression of deformity and neurological complications.
Kyphotic deformity in TB spine constitutes an important indication of surgical stabilization. Progressive failure of the anterior column due to the disease process and repetitive loading may eventually lead to the failure of a healthy posterior column resulting in spinal instability. Different researchers have considered different degrees of kyphotic deformity as a cut-off for spinal fixation. Chandra et al and Nene et al have taken 40 degrees whereas Jutte et al have considered 30 degrees of pre-treatment kyphosis as a cut-off for spinal fixation. Jain et al on the other hand have considered a predicted kyphotic deformity of 60 degrees calculated at the start of the treatment using the formula Y = a + bx (where Y represents the final predicted kyphosis, ‘a’ and ‘b’ are constants and x represents the initial loss of vertebral height) in the thoracic and thoraco-lumbar spine as an indication for surgery.22,28 Rajasekaran also considered a pre-treatment kyphosis of 30 degrees, especially in the paediatric population, as an indication for surgical stabilization.10
Number of involved vertebrae
Multilevel contiguous TB spine has also been considered as an important indicator of instability by various researchers. Number of involved or destroyed vertebrae at the beginning of the treatment has been shown to correlate with the final kyphosis in the natural history of progression in TB spine and, therefore, to indirectly affect the spinal stability. Jain et al considered involvement of three or more vertebrae or destruction of more than one and a half vertebrae as ‘long-segment disease’ and indicators of spinal instability.22 Rajasekaran described different types of collapse and subsequent restabilization of vertebrae based on the amount of vertebral body destruction. Vertebral body loss of more than 0.75 was considered as an indicator of facet joint disruption and unstable spine. Jutte et al described unstable spine as involvement of more than two vertebrae, whereas in a paradiscal disease destruction of more than 50% of both the involved vertebrae was considered as unstable by Djientcheu et al.14,17
Facet joint involvement/pan-vertebral disease (Fig. 3)
Involvement of all three columns of the vertebrae in the form of pan-vertebral disease or facet joint destruction by the disease process was the most widely used criteria to define instability. Pan-vertebral involvement as indicated by lateral or antero-posterior translation, scoliosis or severe kyphosis in radiographs was considered as an indication for surgery by a number of researchers.7,18,19,21 Others considered involvement of facet joints as evident in CT/MRI findings or facet joint subluxation or dislocation an important indicator of pan-vertebral involvement and spinal instability.9,29 Rajasekaran analysed the natural history of kyphosis in TB spine in the paediatric population and introduced the four ‘spine at risk’ signs including dislocation of the facets, posterior retropulsion of the diseased fragments, lateral translation of the vertebrae in the anteroposterior view and toppling of the superior vertebra. Presence of two or more signs signified instability in children.9,10
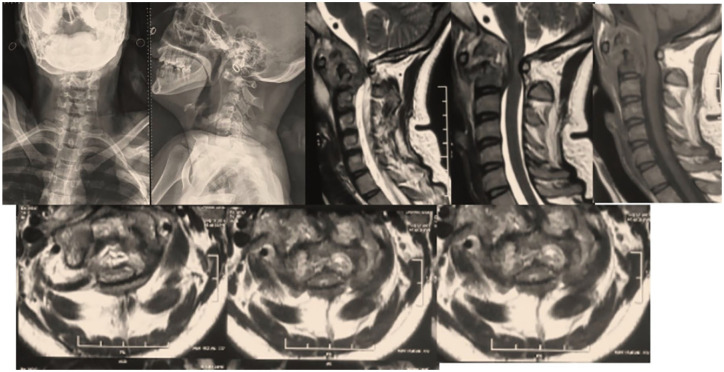
Instability in cervical spine TB (Fig. 4)
Fig. 4.
A 38-year-old lady with tuberculosis of the cranio-vertebral junction. Notice increased atlanto-axial distance with scoliosis at the pathological site. The lesion is unstable and should be stabilized surgically.
Of 22, four studies defined instability in cervical spine TB. Chaudhary et al defined instability in C1–C2 TB as migration of the C1 posterior arch anterior to the extrapolated spino-laminar line, migration of the tip of the odontoid (or projected tip in cases with odontoid destruction) above the McRae line with gross destruction of lateral weight-bearing columns. Bapat et al considered an atlanto-dens interval more than 8 mm or migration of the odontoid tip 4 mm above the McGregor line as unstable. With respect to the subaxial spine, He et al considered cervical kyphosis of more than 30 degrees indicative of instability, whereas Hou et al described facetal subluxation or dislocation with cervical kyphosis as unstable.
Discussion
The management strategy for TB spine has been controversial, more so in patients without significant neurological deficit. The introduction of the ‘middle path regime’ by Tuli in 70s marked an important event in formulating the widely followed management guidelines that are practiced today.2 The regime spoke of TB spine as a primarily medical disease to be managed with anti-tubercular therapy and bed rest, whereas surgery was reserved for patients who showed no clinical or neurological improvement or worsening on conservative management.1 The other indications described in the regime included posterior spinal disease, doubtful diagnosis or instability.2 Despite its excellent results, there were some glancing lacunae and ambiguities in the described regime. A major shortcoming was the lack of an objective criteria to define the surgical indications, particularly in patients without significant neurological deficit. For instance, the authors defined spinal instability as an indication for surgery under the regime, however, the authors have not clearly defined what constitutes instability. Since then a number of authors have used various clinical and radiological criteria to define spinal instability in TB spine. However, no clear consensus exists with respect to a working definition for instability in TB spine. This ambiguity is an important factor responsible for wide variability in surgical decision making among surgeons. The current systematic review evaluates clinical and radiological parameters used by various researchers to define instability in TB spine. The Cochrane Review Group has accepted systematic reviews as an important study methodology for answering a specific scientific question by objectively summarizing the body of literature.30
Instability is a mechanical entity, and an unstable structure that is not in an optimal state of equilibrium.31 With respect to the spine, broadly, spinal stability is regarded as the ability of the spine to maintain its alignment and protect the neural structures under normal physiological loads. This definition is a general definition encompassing all spinal pathologies. The concept of spinal stability in traumatic conditions of the spine was introduced in the Watson-Jones classification in 1931 and then by Nicoll in 1949.32,33 Denis in 1983 introduced the three-column theory of the spine to define instability.34 A number of other theories along with the above-mentioned theories paved the way for the currently practiced TLICS (thoraco-lumbar injury classification severity score) which indirectly represents a stable or an unstable spine. Punjabi and White introduced a checklist to score spinal instability which is currently widely used to evaluate instability in degenerative conditions.35 Similarly, to evaluate instability in a metastatic spine disease, SINS (spinal instability neoplastic score) was developed by Fisher et al.36 However, none of the classifications or scoring criteria can be applied to TB spine to objectively evaluate spinal instability owing to the uniqueness and complexity of the disease.
Demographic factors
In the current study, age and location of the lesion were identified as the two most important demographic factors contributing to instability in TB spine. Vertebral destruction at a younger age leads to progressive deformity in a significant proportion of patients owing to the flexibility and ligamentous laxity of the paediatric spine.28 Age less than 10 years was found by Rajasekaran to be an important independent predictor for ‘buckling collapse’ in post-tubercular kyphosis.11 With respect to location, TB spine of the junctional region was considered an important factor to determine instability. Junctional region of the spine represents the junction of a highly mobile spine segment with a relatively immobile segment and is characterized by higher stresses and displacement as compared to non-junctional spine. TB spine at cervico-dorsal or dorso-lumbar regions of the spine have a higher propensity for progression due to the resultant instability.
Clinical factors
Clinical symptoms such as mechanical back pain, pain associated with movement or loading and relief with recumbency are identified as important predictors of spinal instability. However, in the current review, the use of clinical symptoms for diagnosis of spinal instability was limited to only two articles. Nene and Bhojraj diagnosed spinal instability in TB spine on the basis of presence or absence of clinical symptoms such as severe back pain, paraspinal muscle spasm, painfully restricted movements of the thoracolumbar spine and an ‘instability catch’.4 Although persistent pain not resolving with a trial of ATT for four to eight weeks has been addressed as instability pain by a few researchers, the authors have not included this definition in the review.1,2,21,37,38 Spinal instability in TB spine is an emergent and absolute indication for surgery and a trial of four to eight weeks of medical management is unreasonable, especially considering the associated potential complications. Therefore, the diagnosis of spinal instability in TB spine and subsequent surgical stabilization should be carried out as early as possible.
Radiological factors
A number of radiological features have been defined in various spinal pathologies to address and diagnose spinal instability. The current review shows similar results with respect to the number of articles considering various radiological features as diagnostic criteria for spinal instability in spinal TB. The involvement of facet joints and the posterior column leading to a pan-vertebral involvement was found to be the most widely used criteria to define instability in the present study. Pan-vertebral involvement can be identified in plain radiographs as disturbed sagittal or coronal alignment such as severe kyphosis, scoliosis or antero-posterior or lateral translation.5,19,37 Rajasekaran defined the ‘spine at risk’ signs as predictors for progression of deformity in the paediatric age group. The risk signs indirectly signify pan-vertebral involvement and spinal instability.9 A few researchers considered CT or MRI findings suggestive of global destruction of vertebrae or bilateral facet joint destruction for the diagnosis of spinal instability.5,21
With respect to kyphosis, different researchers considered varying degrees of deformity as the cut-off for surgical stabilization. Destruction of the vertebral bodies due to the disease process results in failure of the anterior column and subsequent kyphosis. The amount of destruction of the vertebral bodies is directly proportional to the amount of deformity. Progression of deformity due to various factors such as disturbed biomechanics and loading characteristics, subsequent spinal growth and the magnitude of initial deformity indirectly indicates spinal instability. To summarize, an initial kyphotic angle of 40 degrees or projected kyphotic angle of 60 degrees was considered as the cut-off for defining instability. Apart from kyphosis, multilevel contiguous TB spine involving over three bodies or leading to a destruction of more than one and a half bodies were also considered as criteria for defining instability.8
Instability in cervical spine TB
Criteria used to define instability in C1–C2 TB spine were described in two articles. Both the articles used routine craniovertebral junction landmarks such as distance of the tip of the odontoid from the McRae line or the McGregor line to define instability. One study considered migration of the posterior arch of the atlas anterior to the spino-laminar line, whereas the other considered an atlanto-dens interval of more than 8 mm for defining instability. None of the studies defined instability using clinical criteria. Literature defining instability in the subaxial spine was rather limited an insufficient. A cervical kyphosis of 30 degree was found to be the only criteria considered for defining instability.
The current review brings to light several lacunae in the literature with respect to defining instability in TB spine. Instability is a biomechanical entity and good quality evidence is now possible using computational biomechanics techniques such as finite element analysis. Further, subaxial cervical spine TB is a relatively unresearched entity, and more evidence is needed to define spinal instability. Early identification of instability in TB spine is crucial for both treating physicians and patients. Expedited surgical stabilization can prevent many potential troublesome complications in such patients. Additionally, identifying the factors to determine instability may provide the necessary assistance to the relatively inexperienced surgeon for surgical decision making in patients with unstable spinal TB.
Conclusion
Various researchers have defined instability using clinical and radiological criteria. The current review identified lesser age, junctional region of spine, mechanical pain and ‘instability catch’, kyphotic deformity above 40 degrees, pan-vertebral or bilateral facetal involvement and multifocal contiguous disease involving more than three vertebrae as predictors for spinal instability in the dorso-lumbar spine. Cervical kyphosis more than 30 degrees and facetal or pan-vertebral involvement were found to be the factors used to define instability in the subaxial cervical spine. With respect to C1–C2 TB spine, migration of the tip of the odontoid above the McRae line or the McGregor line, or anterior translation of C1 over C2 were considered as determinants for instability.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Tuli SM. Treatment of neurological complications in tuberculosis of the spine. J Bone Joint Surg Am 1969;51:680–692. [PubMed] [Google Scholar]
- 2. Tuli SM. Results of treatment of spinal tuberculosis by ‘middle-path’ regime. J Bone Joint Surg Br 1975;57:13–23. [PubMed] [Google Scholar]
- 3. Weber MH, Burch S, Buckley J, et al. Instability and impending instability of the thoracolumbar spine in patients with spinal metastases: a systematic review. Int J Oncol 2011;38:5–12. [PubMed] [Google Scholar]
- 4. Nene A, Bhojraj S. Results of nonsurgical treatment of thoracic spinal tuberculosis in adults. Spine J 2005;5:79–84. [DOI] [PubMed] [Google Scholar]
- 5. Bhojraj S, Nene A. Lumbar and lumbosacral tuberculous spondylodiscitis in adults: redefining the indications for surgery. J Bone Joint Surg Br 2002;84:530–534. [DOI] [PubMed] [Google Scholar]
- 6. Jain AK. Treatment of tuberculosis of the spine with neurologic complications. Clin Orthop Relat Res 2002;398:75–84. [DOI] [PubMed] [Google Scholar]
- 7. Jain AK. Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br 2010;92:905–913. [DOI] [PubMed] [Google Scholar]
- 8. Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop Relat Res 2007;460:39–49. [DOI] [PubMed] [Google Scholar]
- 9. Rajasekaran S. The natural history of post-tubercular kyphosis in children: radiological signs which predict late increase in deformity. J Bone Joint Surg Br 2001;83:954–962. [DOI] [PubMed] [Google Scholar]
- 10. Rajasekaran S. Natural history of Pott’s kyphosis. Eur Spine J 2013;22:634–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rajasekaran S. Kyphotic deformity in spinal tuberculosis and its management. Int Orthop 2012;36:359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shetty AP, Viswanathan VK, Kanna RM, Shanmuganathan R. Tubercular spondylodiscitis in elderly is a more severe disease: a report of 66 consecutive patients. Eur Spine J 2017;26:3178–3186. [DOI] [PubMed] [Google Scholar]
- 13. Chandra SP, Singh A, Goyal N, et al. Analysis of changing paradigms of management in 179 patients with spinal tuberculosis over a 12-year period and proposal of a new management algorithm. World Neurosurg 2013;80:190–203. [DOI] [PubMed] [Google Scholar]
- 14. Jutte PC, van Loenhout-Rooyackers JH. Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev 2006;1. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004532.pub2/full (date last accessed 3 May 2020). [DOI] [PubMed] [Google Scholar]
- 15. Hou K, Yang H, Zhang L, Zhang X, Xiao S, Lu N. Stepwise therapy for treating tuberculosis of the upper cervical spine: a retrospective study of 11 patients. Eur Neurol 2015;74:100–106. [DOI] [PubMed] [Google Scholar]
- 16. He M, Xu H, Zhao J, Wang Z. Anterior debridement, decompression, bone grafting, and instrumentation for lower cervical spine tuberculosis. Spine J 2014;14:619–627. [DOI] [PubMed] [Google Scholar]
- 17. Djientcheu VP, Mouafo Tambo FF, Ndougsa IS, et al. The role of surgery in the management of Pott’s disease in Yaoundé: a review of 43 cases. Orthop Traumatol Surg Res 2013;99:419–423. [DOI] [PubMed] [Google Scholar]
- 18. Mehta JS, Bhojraj SY. Tuberculosis of the thoracic spine: a classification based on the selection of surgical strategies. J Bone Joint Surg Br 2001;83:859–863. [DOI] [PubMed] [Google Scholar]
- 19. Kandwal P, Garg B, Upendra B, Chowdhury B, Jayaswal A. Outcome of minimally invasive surgery in the management of tuberculous spondylitis. Indian J Orthop 2012;46:159–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chaudhary K, Potdar P, Bapat M, Rathod A, Laheri V. Structural odontoid lesions in craniovertebral tuberculosis: a review of 15 cases. Spine (Phila Pa 1976) 2012;37:E836–E843. [DOI] [PubMed] [Google Scholar]
- 21. Jain AK, Jain S. Instrumented stabilization in spinal tuberculosis. Int Orthop 2012;36:285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jain AK, Dhammi IK, Prashad B, Sinha S, Mishra P. Simultaneous anterior decompression and posterior instrumentation of the tuberculous spine using an anterolateral extrapleural approach. J Bone Joint Surg Br 2008;90:1477–1481. [DOI] [PubMed] [Google Scholar]
- 23. Bapat MR, Lahiri VJ, Harshavardhan NS, Metkar US, Chaudhary KC. Role of transarticular screw fixation in tuberculous atlanto-axial instability. Eur Spine J 2007;16:187–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Christodoulou AG, Givissis P, Karataglis D, Symeonidis PD, Pournaras J. Treatment of tuberculous spondylitis with anterior stabilization and titanium cage. Clin Orthop Relat Res 2006;444:60–65. [DOI] [PubMed] [Google Scholar]
- 25. Nussbaum ES, Rockswold GL, Bergman TA, Erickson DL, Seljeskog EL. Spinal tuberculosis: a diagnostic and management challenge. J Neurosurg 1995;83:243–247. [DOI] [PubMed] [Google Scholar]
- 26. Rajasekaran S. The problem of deformity in spinal tuberculosis. Clin Orthop Relat Res. 2002. May;(398):85-92. doi: 10.1097/00003086-200205000-00012. PMID: 11964635. [DOI] [PubMed] [Google Scholar]
- 27. Lee T-C, Lu K, Yang L-C, Huang H-Y, Liang C-L. Transpedicular instrumentation as an adjunct in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg 1999;91:163–169. [DOI] [PubMed] [Google Scholar]
- 28. Rajasekaran S, Shanmugasundaram TK. Prediction of the angle of gibbus deformity in tuberculosis of the spine. J Bone Joint Surg Am 1987;69:503–509. [PubMed] [Google Scholar]
- 29. Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop Relat Res 2007;460:39–49. https://www.ncbi.nlm.nih.gov/pubmed/17438468/ (accessed 3 May 2020). [DOI] [PubMed] [Google Scholar]
- 30. van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for Spinal Disorders. Spine (Phila Pa 1976) 1997;22:2323–2330. [DOI] [PubMed] [Google Scholar]
- 31. Pope MH, Panjabi M. Biomechanical definitions of spinal instability. Spine (Phila Pa 1976) 1985;10:255–256. [DOI] [PubMed] [Google Scholar]
- 32. Watson-Jones R. Fracture and joint injuries. Baltimore: Williams and Wilkins, 1943. [PubMed] [Google Scholar]
- 33. Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br 1949;31B:376–394. [PubMed] [Google Scholar]
- 34. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817–831. [DOI] [PubMed] [Google Scholar]
- 35. Panjabi MM, White AA, III. Basic biomechanics of the spine. Neurosurgery 1980;7:76–93. [DOI] [PubMed] [Google Scholar]
- 36. Fisher CG, DiPaola CP, Ryken TC, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976) 2010;35:E1221–E1229. [DOI] [PubMed] [Google Scholar]
- 37. Jain AK, Kumar J. Tuberculosis of spine: neurological deficit. Eur Spine J 2013;22:624–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rajasekaran S, Soundararajan DCR, Shetty AP, Kanna RM. Spinal tuberculosis: current concepts. Global Spine J 2018;8:96S–108S. [DOI] [PMC free article] [PubMed] [Google Scholar]