Abstract
Background
Myopia (near-sightedness) is increasing worldwide, especially in Asia. The aim of this study was to describe trends in the prevalence of myopia in Germany.
Methods
We analyzed data from the German Health Interview and Examination Survey for Children and Adolescents (KiGGS; baseline survey 2003-2006, N = 17 640; wave 2, 2014-2017, N = 15 023). The presence of myopia was determined from a parent questionnaire and validated by the use of a visual aid. The population prevalence of myopia was calculated. Based on the KiGGS wave 2 data, potential risk factors for myopia were identified by means of logistic regression.
Results
The prevalence of myopia at the age of 0–17 years in Germany was 11.6% (95% confidence interval [11.0; 12.2]) in the period 2003–2006 and 11.4% [10.7; 12.2] in 2014–2017. No age group of either sex exhibited a relevant, statistically significant change in the prevalence of myopia. In the adjusted model (adjusted for age, sex, family socioeconomic status, family history of migration), no association was found between myopia and use of digital media. More time spent reading books was associated with myopia: reading for more than 2 h/day showed an odds ratio of 1.69 [1.3; 2.2].
Conclusion
The prevalence of myopia in children and adolescents in Germany has remained virtually unchanged over a period of approximately 10 years. Changes in media consumption, such as the increased use of smartphones in this age group, have therefore had no detectable impact on the development of myopia, at least not so far. Future studies should investigate the influences of further increases in media use and examine the long-term effects.
Myopia (short-sightedness, near-sightedness) causes distance blur and is a refractive error where the eye is typically too long in relation to the refractive power of the anterior segment of the eye. The prevalence of myopia is increasing worldwide and it is discussed to be the most common cause of vision impairment without optical correction in developed countries (1).
At birth, the human eye is farsighted (2) and emmetropization typically continues into the school-aged years. Since the development of the refractive power of the cornea, the refractive power of the lens and the length of the eye is well coordinated, the farsighted refractive error of the eye present at birth is ultimately corrected. While myopia is uncommon in preschool children, its prevalence continues to increase with the number of education years, as shown in a population-based study on adults 35 to 74 years of age (3); the association between myopia und education is independent of genetic effects (4).
A systematic review on the prevalence of myopia published in 2016 reported a prevalence among white 5-year-olds of European origin of 1.6% and among North American natives of 11.3% (5). By contrast, the prevalence of myopia among adults is significantly higher. Especially in East Asian countries, prevalence of up to 80% has been reported, while in rural regions without formal education the prevalence of myopia is below 10% (6).
Information about the prevalence of myopia in Germany was reported by Jobke et al. in 2008 (7). The authors found a prevalence of 0% in children 2 to 6 years, 5.5% in children 7 to 11 years, and 21.0% in adolescents 12 to 17 years of age. These prevalence estimates were significantly lower than those reported in other European studies (7). An early publication found a myopia prevalence of 13.3% among children and adolescents 3 to 17 years of age based on data from the KiGGS baseline study conducted by the Robert Koch Institute (RKI) between 2003 and 2006 (8); time trends could not be evaluated. In a secondary data analysis, Wesemann looked at data on the strength of glasses in Germany between 2000 and 2015, analyzing a set of refractive power data (n = 1 223 410) of prescription glasses in Germany provided by medium-sized optometrists (approximately 10% of all optometrists) (9). Based on these results, Wesemann concluded that the prevalence of myopia among persons 5 to 30 years of age had not increased during the analyzed period (10). Recently, Yang et al. reported that the prevalence of myopia among young Austrian draftees (male, younger than 19 years) between 1983 and 2017 increased from 13.8% to 24.4%; however, since 2013 the increase has only been 2.2% (11).
The strong increase in the prevalence of myopia in Asia has largely been attributed to educational pressure and the reduced time spent outdoors. Besides genetic factors, these factors have an effect on the occurrence and the severity of myopia (6). Outdoor light exposure is considered to be protective, while indoor activities, such as watching TV, computer use and reading are viewed as potential risk factors (12– 14). The underlying mechanism is thought to be a low light exposure-related reduction in retinal dopamine concentrations, triggering increased axial growth of the eye with resulting myopia (15). Whether the use of smartphones has an effect on the development of myopia remains the subject of controversy (8, 16, 17).
The aim of this study is to evaluate the time trends in the prevalence of childhood and adolescence myopia in Germany during the period between the KiGGS baseline survey and the KiGGS wave 2 survey. In addition, potential risk factors of myopia, especially the use of media, are analyzed.
Method
The statistical analyses are based on data of the KiGGS study. The KiGGS baseline study was conducted by the RKI as part of nationwide population health monitoring between 2003 and 2006. The second wave of the study was conducted between 2014 and 2017. More detailed information about the study design and methods is provided in the eSupplement.
The prevalence of myopia was calculated based on data collected in the parent questionnaire. In order to substantiate the diagnosis of myopia, only those children and adolescents were defined as myopic in the primary analysis who, besides the mentioning of myopia by the parents, were reported to have a visual aid. Those children and adolescents were defined as non-myopic whose parents answered the visual impairment question with “shortsightedness: No“. Children and adolescents with parents-reported myopia, but no glasses were excluded from the analyses.
Statistical analysis
Prevalence estimators and their 95% confidence intervals were calculated and compared to each other between the two surveys. Using multivariable logistic regression, potential risk factors of myopia were explored in an unadjusted, partly adjusted and fully adjusted fashion based on KiGGS wave 2 data. However, no data on the intensity of smartphone use was collected in the survey; having a smartphone was regarded as a proxy for smartphone use.
Modified cross-sectional weights of the KiGGS baseline study and KiGGS wave 2 were used for trend analyses, and, in that way, an adaption to the official population structure was accomplished.
A p-value <0.05 was regarded as statistically significant; no correction for multiple testing was performed. The myopia prevalence trend analysis and the regression analysis were defined as primary analyses. All further analyses are sensitivity analyses. The statistical analyses were performed using the statistical software package SPSS version 24.0.
Results
The KiGGS baseline study (2003 to 2006) included 17 640 children and adolescents 0 to 17 years of age. Parents reported myopia in 1720 children and adolescents, in 13 547 no myopia, in 1321 “do not know“, and in 1052 children and adolescents this information was missing. For 1604 (93.3%) of these myopic children and adolescents, the information of the parents that their child has a visual aid was available. In KiGGS wave 2 (2014 to 2017), 15 023 children and adolescents were included in the study. Here, the parents reported myopia in 1725 children and adolescents, no myopia in 11 244, “do not know” in 596, and this information was missing in 1458 children and adolescents. For 1582 (91.7%) of these myopic children and adolescents, the information of the parents that their child has a visual aid was available. The analyzed samples of the two surveys (myopic and non-myopic children and adolescents 0 to 17 years of age) are each detailed in Table 1.
Table 1. Description of sample.
|
KiGGS baseline study (2003–2006) N = 15 151 |
KiGGS wave 2 (2014–2017) N = 12 826 |
|
| Sex | 49.0 % female (7 425) | 49.6 % female (6 368) |
| Age | 8.53 ± 5.01 (0–17 years) | 9.20 ± 4.81 (0–17 years) |
| Place of residence – Rural – Small town – Medium-sized town – Metropolitan |
22.9 % 26.3 % 28.7 % 22.1 % |
17.8 % 32.6 % 28.4 % 21.2 % |
| Migration background (yes) | 10.6 % (1 604) | 10.0 % (1 287) |
| Socioeconomic status – Low – Middle – High – Missing data |
14.8 % (2 243) 59.8 % (9 054) 24.5 % (3 713) 0.9 % (141) |
11.6 % (1 484) 61.5 % (7 892) 26.6 % (3 411) 0.3 % (39) |
The socioeconomic status was determined based on occupation, education and parental income data. Children and adolescents without myopia or with corrected myopia are included in this sample.
In the age group 0 to 17 years, the prevalence of myopia in Germany was 11.6% (95% confidence interval: [11.0; 12.2]) during the period from 2003 to 2006. The sex-stratified analysis showed that the prevalence of myopia was 9.6% [8.9; 10.4] in boys and 13.7% in girls [11.8; 14.6].
In Germany in the period from 2014 to 2017, the prevalence of myopia among children and adolescents 0 to 17 years of age was 11.4% [10.7; 12.2]. The prevalence in boys was 9.6% [8.6; 10.5], in girls 13.5% [12.4; 14.6].
The trend analysis found no statistically significant change in myopia prevalence between the two survey periods. This applies to the total study population (p = 0.45) and also to the subgroups of boys (p = 0.54) and girls (p = 0.62). The sensitivity analyses are presented in eTabelle 1 and in the eFigure.
eTable 1. Sensitivity analyses (S1–S4) on the time trend of myopia development in the KiGGS study based on different definitions.
| Myopia | No myopia | Exclusion | Trend (p-value) | |
| Primary analysis | Parent questionnaire answers “myopic“ + glasses | Parent questionnaire answer “non-myopic“ | Parent answer “do not know“, missing data, parent questionnaire answers “myopic“ without glasses | 0.45 |
| S1 | Parent questionnaire answer “myopic“ | Parent questionnaire answer “non-myopic“ | Parent questionnaire answer “do not know“, missing data | 0.16 |
| S2 | Parent questionnaire answer “myopic“ | Parent questionnaire answer “non-myopic“, “do not know” | Missing data | 0.03 |
| S3 | Parent questionnaire answer “myopic“+ glasses | Parent questionnaire answer “non-myopic“, “do not know“, “myopic“ without glasses | Missing data | 0.17 |
| S4 | Parent answer “myopic“+ glasses | Parent questionnaire answer “non-myopic“, “do not know” | Missing data, parent questionnaire answers “myopic“ without glasses | 0.15 |
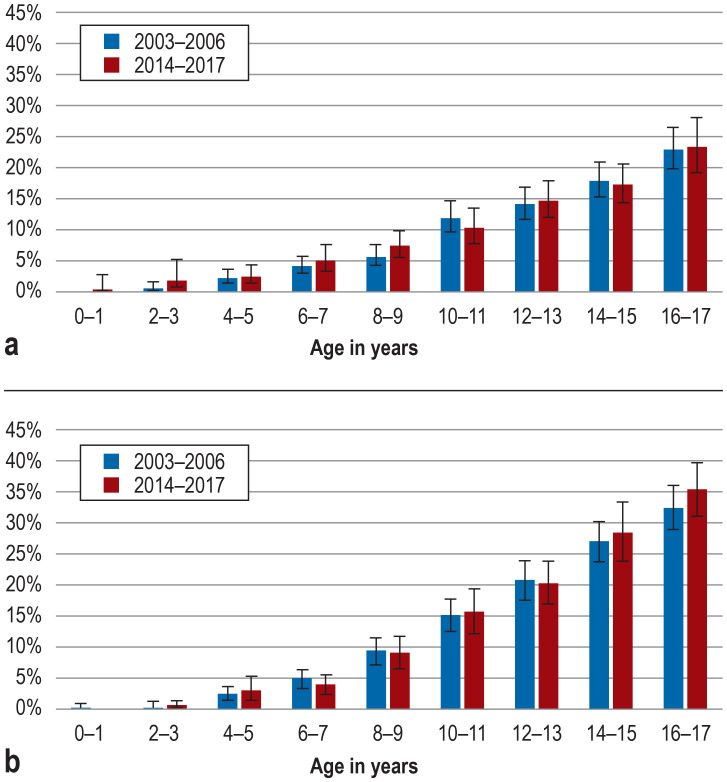
eFigure.
Prevalence and time trends in myopia among male (a) and female (b) children and adolescents in Germany without taking account of the presence of a visual aid
Data source: KiGGS baseline study (2003–2006), KiGGS wave 2 (2014–2017)
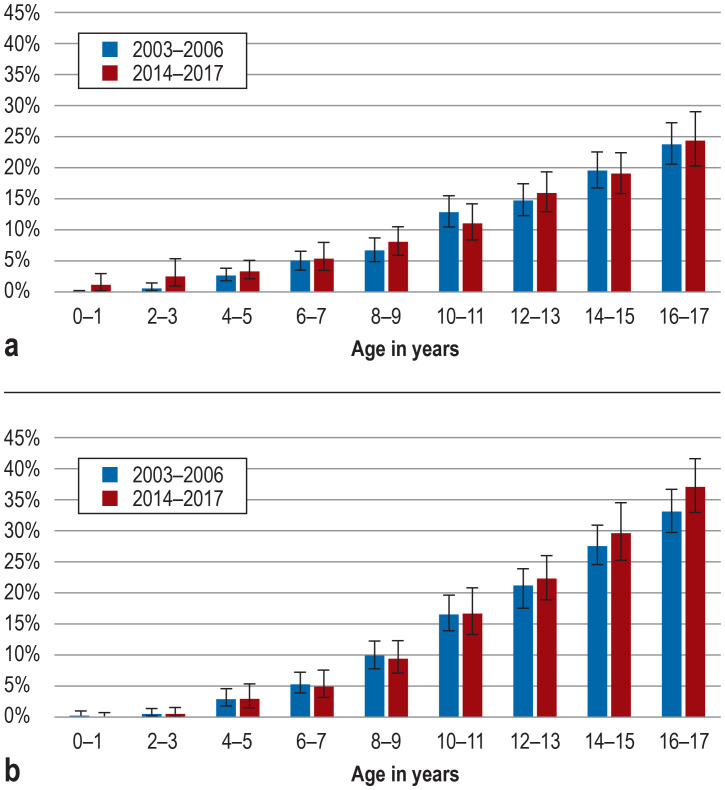
At both survey time points, a comparable increase in myopia prevalence with age was observed; starting from the age of 8 to 9 years, myopia was more common in girls than boys (figure).
Figure.
Prevalence and time trends in myopia among male (a) and female (b) children and adolescents in Germany
Data source: KiGGS baseline study (2003–2006), KiGGS wave 2 (2014–2017); myopia was defined based on parent questionnaire answer and presence of a visual aid.
The analysis of KiGGS wave 2 (2014 to 2017) showed that older age and female sex were associated with increases in the prevalence of myopia. Socioeconomic status (SES) and migration background were not associated with increased myopia prevalence. Neither the assessed media use parameters (TV/video, game console, computer/internet) nor the possession of a smartphone showed an association with myopia in the multivariable model. However, prolonged reading of books was associated with myopia (table 2). In the unadjusted analysis, a dose effect was found with TV/video, computer/internet and reading; in the partly adjusted model, this effect was only present with reading (table 2).
Table 2. Association between media use and myopia among 3 to 17-year-old children and adolescents in Germany; results of multivariable binary logistic regressions (odds ratios [OR]); data source: KiGGS wave 2 (2014–2017).
| Unadjusted | Partly adjusted | Fully adjusted | |||||||
| OR | 95% confidence interval | p value | OR | 95% confidence interval | p value | OR | 95% confidence interval | p value | |
| Age (years) | 1.24 | [1.21; 1.27] | <0.001 | 1.24* | [1.21; 1.28] | <0.001 | 1.24 | [1.19; 1.29] | <0.001 |
| Sex (male) | 0.68 | [0.58; 0.81] | <0.001 | 0.71* | [0.58; 0.85] | <0.001 | 0.69 | [0.56; 0.85] | <0.001 |
| Socioeconomic status | 0.99 | [0.97; 1.01] | 0.15 | 1.00* | [0.98; 1.02] | 0.94 | 1.00 | [0.98; 1.02] | 0.88 |
| Migration background (yes) | 1.04 | [0.82; 1.31] | 0.75 | 0.93* | [0.73; 1.19] | 0.56 | 0.94 | [0.74; 1.21] | 0.65 |
| Media use | |||||||||
| Television | |||||||||
| – Not at all | Ref. | − | <0.001 | Ref. | − | 0.35 | Ref. | − | 0.34 |
| – Up to 1 hour per day | 0.99 | [0.68; 1.44] | 1.30 | [0.89; 1.89] | 1.28 | [0.88; 1.87] | |||
| – 1 to <2 hours per day | 1.47 | [1.01; 2.16] | 1.42 | [0.97; 2.07] | 1.40 | [0.96; 2.06] | |||
| – >2 hours per day | 1.90 | [1.33; 2.73] | 1.28 | [0.88; 1.86] | 1.25 | [0.86; 1.83] | |||
| Game console | |||||||||
| – Not at all | Ref. | − | <0.001 | Ref. | − | 0.29 | Ref. | − | 0.39 |
| – Up to 1 hour per day | 1.25 | [1.04; 1.50] | 1.20 | [1.00; 1.44] | 1.17 | [0.98; 1.40] | |||
| – 1 to <2 hours per day | 1.55 | [1.22; 1.98] | 1.10 | [0.84; 1.43] | 1.06 | [0.82; 1.38] | |||
| – >2 hours per day | 1.90 | [1.46; 2.47] | 1.09 | [0.81; 1.48] | 1.07 | [0.79; 1.45] | |||
| Computer | |||||||||
| – Not at all | Ref. | − | <0.001 | Ref. | − | 0.92 | Ref. | − | 0.91 |
| – Up to 1 hour per day | 2.59 | [2.13; 3.14] | 1.04 | [0.81; 1.35] | 1.00 | [0.77; 1.29] | |||
| – 1 to <2 hours per day | 3.63 | [2.86; 4.61] | 0.99 | [0.72; 1.35] | 0.97 | [0.71; 1.32] | |||
| – > 2 hours per day | 4.72 | [3.81; 5.84] | 1.06 | [0.79; 1.42] | 1.05 | [0.78; 1.43] | |||
| Reading | |||||||||
| – Not at all | Ref. | − | <0.001 | Ref. | − | 0.001 | Ref. | − | 0.001 |
| – Up to 1 hour per day | 0.61 | [0.52; 0.72] | 1.10 | [0.90; 1.34] | 1.09 | [0.89; 1.33] | |||
| – 1 to <2 hours per day | 0.89 | [0.69; 1.14] | 1.29 | [0.98; 1.70] | 1.30 | [0.99; 1.71] | |||
| – > 2 hours per day | 1.50 | [1.17; 1.91] | 1.69 | [1.30; 2.20] | 1.69 | [1.30; 2.20] | |||
| Possession of a smartphone (yes) | 4.28 | [3.60; 5.08] | <0.001 | 1.04 | [0.80; 1.34] | 0.77 | 1.02 | [0.79; 1.31] | 0.89 |
Partly-adjusted analyses are adjusted for age, sex, socioeconomic status (based on the reported occupation, education and parental income) and migration background, separately for each type of media use; fully-adjusted analyses comprise the same parameters, including all types of media use.
* These estimators vary slightly between the partly-adjusted models and are reported for the model with “reading books”.
The first sensitivity analysis using the myopia definition independent of a visual aid confirmed the results of the primary analysis. In the second sensitivity analysis, the screen index was associated with myopia in the unadjusted analysis (odds ratio [OR]: 1.21 per hour screen use [1.18; 1.25]; p<0.001). After adjusting for age, sex, SES, migration background, reading books, and possession of a smartphone, this association was no longer demonstrable (OR: 1.00 per hour [0.96; 1.04]; p = 0.94); likewise, it was not detectable in the multivariable analysis without the possession of a smartphone (OR: 1.00 [0.96; 1.05]; p = 0.90).
Discussion
The prevalence of myopia among children and adolescents in Germany as well as the effect of new digital media, such as smartphones and tablets, on the development of myopia is as yet poorly understood. The KiGGS data show that the prevalence of myopia among children and adolescents did no meaningfully change between 2003–2006 and 2014–2017. Since the method of data collection was identical in both periods, comparability is ensured. Thus, it can be assumed that, for example, the continuously increasing use of smartphone since the 2003–2006 KiGGS baseline study has, at least so far, had no effect on the prevalence of myopia among children and adolescents in Germany. According to these data, there is no association between myopia and the use of other media, such as TV, game console and computer. In contrast, the known association between the reading of books and myopia was confirmed by the KiGGS data.
In the age group 14 to 17 years, 23% of the boys and 35% of the girls are myopic; only among girls 14 to 17 years of age a minor increase in myopia prevalence was noted. Based on projections, Holden et al. assume that, in 2020, 36.7% of the population in Western Europe will be myopic, increasing to 51.0% by 2040 (18).
Especially patients with high myopia are at risk of retinal changes in the macula (19) or developing glaucoma (20). In Germany, too, the prevalence of myopia among young adults is likely to increase as apparently more tertiary students develop myopia over the course of their studies (4). However, since the KiGGS surveys covered only children and adolescents up to 17 years of age, no prevalence estimate can be provided for young adults.
Based on the results of studies published between 1958 and 2015, a 2016 systematic review looked at variations and time trends in the prevalence of myopia among populations of different ethnic origins. While it found an increase in myopia prevalence in Asia, especially in East Asia, a marginal decline was modelled for white children and adolescents of European origin. Due to the broad confidence interval, however, it is also possible that the prevalence of myopia has remained stable over time in whites (5).
Relatively stable prevalence estimators for myopia were reported by Chiang et al. for 12– to 19-year-old US citizens based on a comparison of data from the National Health and Nutrition Examination Surveys (NHANES) of 2001 and 2007, especially in the non-Hispanic white population (21). This study showed that TV and computer use are associated with myopia. These findings are in conflict with the KiGGS wave 2 results. Even though we found a dose-effect relationship between TV/computer use and myopia in the unadjusted analysis, this was no longer present after adjustment for age and sex—two parameters associated with media use time. Likewise, a recent meta-analysis of five studies showed no association between screen time and myopia (22). In KiGGS wave 2, by contrast, increased reading time was associated with myopia.
This is in line with other studies showing that time spent doing near-work activities is a risk factor for developing myopia (23). Gene-environment interactions play a role in myopia. For example, the effect of reading habits (24), education (25) and near-work activities (26) varies in size with genetic predisposition. There is evidence showing that exposure to bright light can reduce the risk of myopia (27). Children learning in an outdoors setting developed myopia less frequently and showed less myopia progression (28). Furthermore, a meta-analysis published in 2017 found an inverse non-linear association between time spent outdoors and risk of developing myopia (29). Our analysis could not evaluate this factor as no data on the time spent outdoors were available in the KiGGS datasets. Rose et al. reported that spending two hours outdoors per day eliminated the near-work-related additional myopia risk in Australian students (30). It should also be noted that there are significant differences between East Asian and Western educational systems which are reflected in the prevalence of myopia (6); such differences are likely to exist in leisure activities, too. Our study looked at a conceivable association between smartphone possession and myopia, but no such association was found.
Limitations
With regard to the KiGGS study, several limitations have to be taken into account: First, the definition of myopia is not based on measurements of the refractive error, but on parent questionnaire answers. In order to prevent measuring errors, cycloplegic refraction (prevention of accommodation) should be performed to determine refractive errors in children and adolescents. This is part of the routine examination ophthalmologists perform when writing out eyeglass prescriptions for children. Thus, we used the information about the child having a visual aid to further support the diagnosis. Furthermore, the large number of visual aids among myopic study participants confirms the validity of the parental information. However, overall 13.5% of parents provided no information about myopia and 13.7% did not know whether or not their child was myopic. Especially in the KiGGS baseline study, the number of “do not know” answers was considerably higher. This could be due to altered response behavior or wider use of the term myopia during KiGGS wave 2 and exert an effect on the trend analyses. We therefore conducted the sensitivity analyses with different definitions of myopia (with/without glasses). A sensitivity analysis which interpreted the parental statements “non-myopic” and “do not know“ as “no myopia“ showed a trend to an increase in myopia in KiGGS wave 2 (p = 0.03) (etable 1). However, this result should be interpreted with caution, given the considerable difference in the number of “do not know” answers between the two surveys as well as the risk of bias due to misclassification of “do not know” answers (etable 2).
eTable 2. Distribution of the answers on myopia in the parent questionnaire (PQ) of the KiGGS baseline study (2003–2006) and KiGGS wave 2 (2014–2017).
| Age group | ||||||
| 0–2 years | 3–6 years | 7–10 years | 11–13 years | 14–17 years | ||
| KiGGS baseline survey: myopia (PQ) | ||||||
| Refractive error: Myopia | Do not know | 466 | 243 | 235 | 168 | 209 |
| Yes | 4 | 90 | 339 | 453 | 834 | |
| No | 2264 | 3376 | 3328 | 2224 | 2355 | |
| Missing data | 71 | 166 | 246 | 231 | 338 | |
| Total | 2805 | 3875 | 4148 | 3076 | 3736 | |
| KiGGS wave 2: myopia (PQ) | ||||||
| Refractive error: Myopia | Do not know | 238 | 160 | 90 | 59 | 49 |
| Yes | 7 | 94 | 276 | 469 | 879 | |
| No | 1169 | 2944 | 2788 | 2153 | 2190 | |
| Missing data | 41 | 239 | 378 | 345 | 455 | |
| Total | 1455 | 3437 | 3532 | 3026 | 3573 | |
The extent of media use was established based on parent-reported and self-reported information from questionnaires. Here, in particular, social desirability may have had an effect on the responses and the actual time of use may have exceeded the reported time. Since no specific data on smartphone use were collected, this factor was operationalized as the possession of a smartphone—a strategy which is fraught with limitations. The use of new media may indirectly have had a negative effect which could not be further analyzed in this study: When it comes to leisure activities, outdoor activities compete with the use of media or with reading. It is also possible that reading behavior as well as behavior related to the use of new media have changed in recent year. The increasing digitization could possibly be linked to increasing media consumption and more frequent smartphone use, especially among small children. According to this survey, only 2% of the children up to seven years of age had a smartphone, while 89% of the 12– to 13-year-olds and 98% of the 16– to 17-year-old had one. Furthermore, it remains unclear whether a market penetration of pediatric relevance was present during the survey years, to what extent children were exposed to smartphones, and whether the follow-up period was long enough to detect a potential smartphone effect, especially since myopia does not occur before children reach primary school age.
In conclusion, the prevalence of myopia among children and adolescents in Germany has remained essentially constant over a period of about ten years. Therefore, it can be assumed that lifestyle changes, such as the increased use of smartphones, have as yet had little impact on the development of myopia.
Supplementary Material
eMethods
The statistical analyses are based on data of the KiGGS study. The baseline study was conducted by the Robert Koch Institute (RKI) as part of nationwide health monitoring between 2003 and 2006. The second wave of the study was conducted between 2014 and 2017. The study was designed as a combined cross-sectional and cohort study (31). In the periods 2003–2006 (N = 17 640) and 2014–2017 (N = 15 023), population-representative cross-sectional surveys were conducted. The aim of the KiGGS study is to obtain information on the health status of children and adolescents 0 to 17 years of age as well as development trends over time. The individuals to be invited were randomly drawn from 167 resident registers of cities and communities which are representative of the Federal Republic of Germany. These had already been selected for the KiGGS baseline study in collaboration with now GESIS – Leibniz Institute for the Social Sciences. One of the measures taken to ensure a high number of respondents and a largely representative composition of the survey sample was oversampling of children and adolescents without German citizenship to offset the lower response rate expected in this segment despite the processes to improve the participation of respondents with migration background.
In an invitation letter, the parents received a comprehensive information brochure on the study and a response card/telephone number to arrange an appointment. About three days later, children and adolescents eleven years and older received an invitation letter directed at them personally with an enclosed age-appropriate information leaflet. Participant recruitment was followed by further steps of enrolling subjects. First, parents received a reminder letter after about ten days. Two weeks later, study staff started to contact parents by phone to promote survey participation. If nobody answered the phone or no phone number could be obtained, the parents were visited at home to establish contact (32).
The participation rates were 66.6% (33) and 40.1% (32) in the KiGGS baseline study (2003–2006) and in KiGGS wave 2 (2014–2017), respectively (32).
The prevalence of myopia was calculated based on data collected in the parent questionnaire. In order to substantiate the diagnosis of myopia, only those children and adolescents were defined as myopic in this analysis who, besides the mentioning of myopia by the parents, were reported to have a visual aid. Those children and adolescents were defined as non-myopic whose parents answered the visual impairment question with “shortsightedness: No“. Children and adolescents with parents-reported myopia, but no possession of glasses were excluded from the analyses.
Information about sex, age, socioeconomic status (SES) (based on parent-reported information on occupation, education and parental income [34]) and migration background (35) were also obtained from the parent questionnaire. Media use was determined in children 3 to 10 years of age based on parent-reported information and in adolescents 11 to 17 years of age based on self-reported information. Data were collected on how many hours per day the children and adolescents used TV/video, game consoles, computer/internet, and books and whether the children or adolescents had their own smartphones. However, no data on the intensity of smartphone use was collected in the survey; having a smartphone was regarded as a proxy for smartphone use. Use times of more than two hours were aggregated.
Statistical analysis
All prevalence estimators and their 95% confidence intervals were calculated using complex samples weighting (32, 36). This involves that study participants are weighted in a way that the sample is representative of the German population and differing participation rates with respect to age, sex etc. are adjusted. Prevalence estimators were calculated for 2-year age groups for girls and boys and compared to each other between the two surveys. Furthermore, a sensitivity analysis was performed using an alternative definition of myopia (myopia answer independent of visual aid answer) as well as different definitions of non-myopic participants (etable 1). Using multivariable binary logistic regression, potential risk factors of myopia were explored in an unadjusted, partly adjusted and fully adjusted fashion based on KiGGS wave 2 data. Sex, age, SES, migration background, media use, reading behavior, and the possession of a smartphone were evaluated as potential factors. The possession of a smartphone was regarded as a proxy for its use. Odds ratios and their 95% confidence intervals were calculated as measures of association. One further sensitivity analysis was conducted using a screen index based on TV, game console and computer/internet use times, similar to Lampert et al. (33).
Modified cross-sectional weights of the KiGGS baseline study and KiGGS wave 2 were used for trend analyses, and, in that way, an adaption to the official population structure was accomplished. Differences were calculated using chi-square statistic.
A p-value <0.05 was regarded as statistically significant; no correction for multiple testing was performed. The myopia prevalence trend analysis and the regression analysis were defined as primary analyses. All further analyses are sensitivity analyses. The statistical analyses were performed using the statistical software package SPSS version 24.0.
Key Messages.
The German Health Interview and Examination Survey for Children and Adolescents (KiGGS) conducted by the Robert Koch Institute provides nationwide data which can be used to describe the health status of children and adolescents up to 17 years of age and time trends.
The prevalence of myopia remained constant between 2003–2006 and 2014–2017. Both surveys found a higher prevalence of myopia among girls and an increase in prevalence with increasing age.
As a limitation, it should be noted that the presence of myopia was determined based on parent-reported information, not by means of cycloplegic measurement of the refractive error.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest
Prof. Schuster holds the endowed chair for “Ophthalmic Health Care Research“, endowed by the Eye Foundation “Stiftung Auge” and supported by the German Ophthalmological Society (DOG, Deutsche Ophthalmologische Gesellschaft) and the Professional Association of Ophthalmologists in Germany (Berufsverband der Augenärzte Deutschlands e.V.). Prof. Schuster received funds and device support for research projects he initiated from Allergan, Bayer Vital, Heidelberg Engineering, Novartis, and PlusOptix.
The remaining authors declare no conflict of interest.
Parts of this article are excerpts of the dissertation of Clara Kuchenbäcker.
References
- 1.Bourne RR, Jonas JB, Flaxman SR, et al. Prevalence and causes of vision loss in high-income countries and in Eastern and Central Europe: 1990-2010. Br J Ophthalmol. 2014;98:629–638. doi: 10.1136/bjophthalmol-2013-304033. [DOI] [PubMed] [Google Scholar]
- 2.Herrnheiser J. Verlag von Fischer‘s Medic. Berlin: 1892. Die Refractionsentwicklung des menschlichen Auges. [Google Scholar]
- 3.Mirshahi A, Ponto KA, Hoehn R, et al. Myopia and level of education: results from the Gutenberg Health Study. Ophthalmology. 2014;121:2047–2052. doi: 10.1016/j.ophtha.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 4.Mountjoy E, Davies NM, Plotnikov D, et al. Education and myopia: assessing the direction of causality by mendelian randomisation. BMJ. 2018;361 doi: 10.1136/bmj.k2022. k2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rudnicka AR, Kapetanakis VV, Wathern AK, et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br J Ophthalmol. 2016;100:882–890. doi: 10.1136/bjophthalmol-2015-307724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morgan IG, French AN, Ashby RS, et al. The epidemics of myopia: aetiology and prevention. Prog Retin Eye Res. 2018;62:134–149. doi: 10.1016/j.preteyeres.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Jobke S, Kasten E, Vorwerk C. The prevalence rates of refractive errors among children, adolescents, and adults in Germany. Clin Ophthalmol. 2008;2:601–607. doi: 10.2147/opth.s2836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schuster AK, Elflein HM, Pokora R, Urschitz MS. [Prevalence and risk factors of myopia in children and adolescents in Germany—results of the KiGGS survey] Klin Padiatr. 2017;229:234–240. doi: 10.1055/s-0043-102938. [DOI] [PubMed] [Google Scholar]
- 9.Ziemssen F. [No increase in myopia?] Ophthalmologe. 2018;115:418–421. doi: 10.1007/s00347-018-0697-x. [DOI] [PubMed] [Google Scholar]
- 10.Wesemann W. [Analysis of spectacle lens prescriptions shows no increase of myopia in Germany from 2000 to 2015] Ophthalmologe. 2018;115:409–417. doi: 10.1007/s00347-017-0601-0. [DOI] [PubMed] [Google Scholar]
- 11.Yang L, Vass C, Smith L, Juan A, Waldhor T. Thirty-five-year trend in the prevalence of refractive error in Austrian conscripts based on 15 million participants. Br J Ophthalmol. 2020;104:1338–1344. doi: 10.1136/bjophthalmol-2019-315024. [DOI] [PubMed] [Google Scholar]
- 12.Guo Y, Liu LJ, Xu L, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120:277–283. doi: 10.1016/j.ophtha.2012.07.086. [DOI] [PubMed] [Google Scholar]
- 13.Li SM, Li SY, Kang MT, et al. Near work related parameters and myopia in chinese children: the anyang childhood eye study. PLoS One. 2015;10 doi: 10.1371/journal.pone.0134514. e0134514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saxena R, Vashist P, Tandon R, et al. Prevalence of myopia and its risk factors in urban school children in Delhi: the North India Myopia Study (NIM Study) PLoS One. 2015;10 doi: 10.1371/journal.pone.0117349. e0117349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ashby RS, Schaeffel F. The effect of bright light on lens compensation in chicks. Invest Ophthalmol Vis Sci. 2010;51:5247–5253. doi: 10.1167/iovs.09-4689. [DOI] [PubMed] [Google Scholar]
- 16.Liu S, Ye S, Xi W, Zhang X. Electronic devices and myopic refraction among children aged 6-14 years in urban areas of Tianjin, China. Ophthalmic Physiol Opt. 2019,;39:282–293. doi: 10.1111/opo.12620. [DOI] [PubMed] [Google Scholar]
- 17.Hansen MH, Laigaard PP, Olsen EM, et al. Low physical activity and higher use of screen devices are associated with myopia at the age of 16-17 years in the CCC2000 Eye Study. Acta Ophthalmol. 2020;98:315–321. doi: 10.1111/aos.14242. [DOI] [PubMed] [Google Scholar]
- 18.Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 19.Hopf S, Korb C, Nickels S, et al. Prevalence of myopic maculopathy in the German population: results from the Gutenberg health study. Br J Ophthalmol. 2020;104:1254–1259. doi: 10.1136/bjophthalmol-2019-315255. [DOI] [PubMed] [Google Scholar]
- 20.Xu L, Wang Y, Wang S, Wang Y, Jonas JB. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology. 2007;114:216–220. doi: 10.1016/j.ophtha.2006.06.050. [DOI] [PubMed] [Google Scholar]
- 21.Chiang SY, Weng TH, Lin CM, Lin SM. Ethnic disparity in prevalence and associated risk factors of myopia in adolescents. J Formos Med Assoc. 2020;119:134–143. doi: 10.1016/j.jfma.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Lanca C, Saw SM. The association between digital screen time and myopia: a systematic review. Ophthalmic Physiol Op. 2020;40:216–229. doi: 10.1111/opo.12657. [DOI] [PubMed] [Google Scholar]
- 23.Qi LS, Yao L, Wang XF, et al. Risk factors for incident myopia among teenaged students of the experimental class of the air force in China. J Ophthalmol. 2019;2019 doi: 10.1155/2019/3096152. 3096152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen CJ, Cohen BH, Diamond EL. Genetic and environmental effects on the development of myopia in Chinese twin children. Ophthalmic Paediatr Genet. 1985;6:353–359. [PubMed] [Google Scholar]
- 25.Pozarickij A, Williams C, Hysi PG, Guggenheim JA. Quantile regression analysis reveals widespread evidence for gene-environment or gene-gene interactions in myopia development. Commun Biol. 2019;2 doi: 10.1038/s42003-019-0387-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fan Q, Guo X, Tideman JW, et al. Childhood gene-environment interactions and age-dependent effects of genetic variants associated with refractive error and myopia: The CREAM Consortium. Sci Rep. 2016;6 doi: 10.1038/srep25853. 25853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lingham G, Mackey DA, Lucas R, Yazar S. How does spending time outdoors protect against myopia? A review. Br J Ophthalmol. 2020;104:593–599. doi: 10.1136/bjophthalmol-2019-314675. [DOI] [PubMed] [Google Scholar]
- 28.Wu PC, Chen CT, Lin KK, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125:1239–1250. doi: 10.1016/j.ophtha.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 29.Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95:551–566. doi: 10.1111/aos.13403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–1285. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 31.Holling H, Schlack R, Kamtsiuris P, Butschalowsky H, Schlaud M, Kurth BM. [The KiGGS study Nationwide representative longitudinal and cross-sectional study on the health of children and adolescents within the framework of health monitoring at the Robert Koch Institute] Bundesgesundheitsbl. 2012;55:836–842. doi: 10.1007/s00103-012-1486-3. [DOI] [PubMed] [Google Scholar]
- 32.Hoffmann R, Lange M, Butschalowsky H, et al. Querschnitterhebung von KiGGS Welle 2 - Teilnehmendengewinnung, Response und Repräsentativität. Health Monit. 2018;3:82–96. [Google Scholar]
- 33.Lampert T, Sygusch R, Schlack R. [Use of electronic media in adolescence Results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS)] Bundesgesundheitsbl. 2007;50:643–652. doi: 10.1007/s00103-007-0225-7. [DOI] [PubMed] [Google Scholar]
- 34.Lampert T, Muters S, Stolzenberg H, Kroll LE. [Measurement of socioeconomic status in the KiGGS study: first follow-up (KiGGS Wave 1)] Bundesgesundheitsbl. 2014;57:762–770. doi: 10.1007/s00103-014-1974-8. [DOI] [PubMed] [Google Scholar]
- 35.Frank L, Yesil-Jürgens R, Born S, Hoffmann R, Santos-Hövener C, Lampert T. Maßnahmen zur verbesserten Einbindung und Beteiligung von Kindern und Jugendlichen mit Migrationshintergrund in KiGGS Welle 2. Health Monit. 2018;3:134–151. [Google Scholar]
- 36.Kamtsiuris P, Lange M, Schaffrath Rosario A. [The German Health Interview and Examination Survey for Children and Adolescents (KiGGS): sample design, response and nonresponse analysis] Bundesgesundheitsbl. 2007;50:547–556. doi: 10.1007/s00103-007-0215-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
The statistical analyses are based on data of the KiGGS study. The baseline study was conducted by the Robert Koch Institute (RKI) as part of nationwide health monitoring between 2003 and 2006. The second wave of the study was conducted between 2014 and 2017. The study was designed as a combined cross-sectional and cohort study (31). In the periods 2003–2006 (N = 17 640) and 2014–2017 (N = 15 023), population-representative cross-sectional surveys were conducted. The aim of the KiGGS study is to obtain information on the health status of children and adolescents 0 to 17 years of age as well as development trends over time. The individuals to be invited were randomly drawn from 167 resident registers of cities and communities which are representative of the Federal Republic of Germany. These had already been selected for the KiGGS baseline study in collaboration with now GESIS – Leibniz Institute for the Social Sciences. One of the measures taken to ensure a high number of respondents and a largely representative composition of the survey sample was oversampling of children and adolescents without German citizenship to offset the lower response rate expected in this segment despite the processes to improve the participation of respondents with migration background.
In an invitation letter, the parents received a comprehensive information brochure on the study and a response card/telephone number to arrange an appointment. About three days later, children and adolescents eleven years and older received an invitation letter directed at them personally with an enclosed age-appropriate information leaflet. Participant recruitment was followed by further steps of enrolling subjects. First, parents received a reminder letter after about ten days. Two weeks later, study staff started to contact parents by phone to promote survey participation. If nobody answered the phone or no phone number could be obtained, the parents were visited at home to establish contact (32).
The participation rates were 66.6% (33) and 40.1% (32) in the KiGGS baseline study (2003–2006) and in KiGGS wave 2 (2014–2017), respectively (32).
The prevalence of myopia was calculated based on data collected in the parent questionnaire. In order to substantiate the diagnosis of myopia, only those children and adolescents were defined as myopic in this analysis who, besides the mentioning of myopia by the parents, were reported to have a visual aid. Those children and adolescents were defined as non-myopic whose parents answered the visual impairment question with “shortsightedness: No“. Children and adolescents with parents-reported myopia, but no possession of glasses were excluded from the analyses.
Information about sex, age, socioeconomic status (SES) (based on parent-reported information on occupation, education and parental income [34]) and migration background (35) were also obtained from the parent questionnaire. Media use was determined in children 3 to 10 years of age based on parent-reported information and in adolescents 11 to 17 years of age based on self-reported information. Data were collected on how many hours per day the children and adolescents used TV/video, game consoles, computer/internet, and books and whether the children or adolescents had their own smartphones. However, no data on the intensity of smartphone use was collected in the survey; having a smartphone was regarded as a proxy for smartphone use. Use times of more than two hours were aggregated.
Statistical analysis
All prevalence estimators and their 95% confidence intervals were calculated using complex samples weighting (32, 36). This involves that study participants are weighted in a way that the sample is representative of the German population and differing participation rates with respect to age, sex etc. are adjusted. Prevalence estimators were calculated for 2-year age groups for girls and boys and compared to each other between the two surveys. Furthermore, a sensitivity analysis was performed using an alternative definition of myopia (myopia answer independent of visual aid answer) as well as different definitions of non-myopic participants (etable 1). Using multivariable binary logistic regression, potential risk factors of myopia were explored in an unadjusted, partly adjusted and fully adjusted fashion based on KiGGS wave 2 data. Sex, age, SES, migration background, media use, reading behavior, and the possession of a smartphone were evaluated as potential factors. The possession of a smartphone was regarded as a proxy for its use. Odds ratios and their 95% confidence intervals were calculated as measures of association. One further sensitivity analysis was conducted using a screen index based on TV, game console and computer/internet use times, similar to Lampert et al. (33).
Modified cross-sectional weights of the KiGGS baseline study and KiGGS wave 2 were used for trend analyses, and, in that way, an adaption to the official population structure was accomplished. Differences were calculated using chi-square statistic.
A p-value <0.05 was regarded as statistically significant; no correction for multiple testing was performed. The myopia prevalence trend analysis and the regression analysis were defined as primary analyses. All further analyses are sensitivity analyses. The statistical analyses were performed using the statistical software package SPSS version 24.0.