Abstract
Churg-Strauss syndrome (CCS) or eosinophilic granulomatosis with polyangiitis is a rare condition, which is a challenge for both diagnosis and treatment in clinical work. Occurrences of cardiac complications represent a negative predictor of treatment outcome for these patients. The aim of this article is to present the diagnostic and therapeutic modality of a 33-year-old male diagnosed with? CCS. Treatment of these patients should be multidisciplinary, with a comprehensive therapeutic modality, while early diagnosis is imperative.
Keywords: Churg-Strauss Syndrome, eosinophilia, vasculitis
Introduction
Churg-Strauss syndrome (CSS) or eosinophilic granulomatosis with polyangiitis was described by Churg and Strauss.[1,2] They have described the syndrome in patients who had asthma, eosinophilia, granulomatous inflammation, necrotizing systemic vasculitis, and necrotizing glomerulonephritis.[2] In 1990, the American Association of Rheumatologists (ACR) set 6 criteria for diagnosing CSS: asthma, eosinophilia >10%, mononeuropathy (including multiplex) or polyneuropathy, nonfixed pulmonary infiltrates on roentgenography, paranasal sinus abnormality, and biopsy containing a blood vessel with extravascular eosinophils.[3] There may also be myositis and heart failure, cardiomyopathy, coronary artery inflammation, pericardial effusion, and eosinophilic infiltration of mesenteric blood vessels leading to gastrointestinal disorders.[1,3] Incidence is 2.4–6.8/1,000,000 in the general population, and 64.4/1,000,000 in asthma patients.[4] The aim of this article is to present the diagnostic and therapeutic modality of a 33-year-old male diagnosed with CCS.
Case Report
The patient was admitted to the hospital for a gallbladder removal surgery, due to chronic problems he had with it over the years. For the last 10 years, he has been treated for asthma, and 8 years ago, he had surgery on the paranasal sinus. The cholecystectomy went well, the postoperative course was without significant problems, the wound was sutured, calm, and he was discharged for home treatment. After discharge during the coughing attack, the wound dehiscence occurred, and 10 days after the surgery, fever was noticed with developing bilateral pneumonia and wound infection in which Enterococcus Faecalis was isolated. For that reason, antibiotic therapy was included together with symptomatic and supportive therapy. He continued to have fever and after 15 days, he was hospitalized at the Clinic for Infectious Diseases, Clinical Center University of Sarajevo. During hospitalization, laboratory analyses were as follows: leukocytes 24 × 109/L, sedimentation 40 mm/h, eosinophils 63%, lactate dehydrogenase 400 U/L, C-reactive protein 69 mg/L, proteins in urine 0.5 g/L, IgE 512 UI/ml, and fibrinogen 4.6 g/L. During hospitalization, immunoassay (antinuclear antibodies negative, extractable nuclear antigen antibodies panel, anti-double-stranded DNA, perinuclear antineutrophil cytoplasmic antibodies, and cytoplasmic antineutrophil cytoplasmic antibodies were all negative. On a multidisciplinary panel and on the basis of clinical picture and laboratory test, Churg-Strauss syndrome was suspected and glucocorticoid therapy was administered. The pathohistological finding of the gallbladder indicated a mixed infiltrate in the predominance of eosinophil granulocytes with numerous congested vessels. Within the wall, there was a multifocally visible image of necrotic granules surrounded by multinuclear cells of and eosinophilic granulocytes. The hematologist performed a sternal puncture, where the finding of flow cytometry in the bone marrow proved eosinophilia up to 41%. Two days after discharge from the Clinic for Infectious Diseases, there was a worsening of the patient's condition in terms of acute heart failure. Echocardiographically reduced left ventricular ejection fraction of 18% was verified, regurgitation, and moderate pulmonary hypertension, as well as signs of pericardial and pleural effusion on both sides. [Figure 1] Glucocorticoid therapy was prescribed, with therapy for acute heart failure. The patient was presented at a cardiac surgery meeting and heart transplantation was indicated. After 7 days, the patient's condition stabilized, and after 15 days, he was discharged from the Institution. shows the X-ray findings during different stages of treatment.
Figure 1.
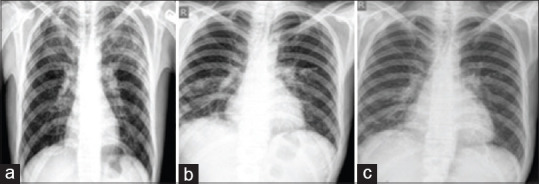
X-ray during 2 months - (a) before the cholecystectomy; (b) after verifying heart failure and administering glucocorticoid and heart failure therapy; (c) 1 month after discharge from hospital
Discussion
The exact pathogenesis of CSS is unknown. Antineutrophil cytoplasmic antibodies (ANCA) were detected in about 40%–60% of patients and CSS was classified among ANCA-positive vasculitis. However, ANCAs are not known to have a pathogenic role in CSS or they merely reflect one end of the spectrum of CCS manifestations. The events leading to the initiation of granulomatosis with polyangiitis are unclear. Possible causes are infectious, genetic, and environmental factors (and combinations of all three).[1] Cardiovascular complications are among the most severe complications of CCS, accounting for about half of the fatalities attributable to CCS.[5,6] Clinical manifestations include clinical signs of heart failure or pericarditis and heart rhythm disorders.[6] Comarmond et al. in their study in 108 ANCA-positive patients had reported significantly more ear, nose, and throat manifestations, peripheral neuropathy, and/or renal involvement, but less frequent cardiac manifestations, than the ANCA-negative patients.[7] The presented patient fulfilled five criteria for the diagnosis of CSS, according to the ACR criteria. The clinical picture and the course of the disease in this case were typical with the onset of paranasal sinusitis, corticosteroid-dependent bronchial asthma. During the last hospitalization, weight loss was noted along with eosinophilia, transient pulmonary infiltrates, and heart failure with pleural and pericardial effusion, together with pathohistological diagnosis of eosinophilic granulomas. Birmingham Vasculitis score (BVAS) and Five Factors Score were developed to evaluate vascular disease activity in patients with eosinophilic granulomatosis with polyangiitis and other vasculitis.[8] Most CSS patients achieve remission with glucocorticoid therapy alone, and when the symptoms of the disease are brought under control, the glucocorticoid dose is gradually reduced over approximately 12–18 months.[9] The use of immunosuppressants is indicated in severe forms (along with immunoglobulins).[10] Antibodies against interleukin-5 (mepolizumab and reslizumab) and an antibody against the interleukin-5-receptor-alpha-chain (benralizumab) are also therapeutic options.[11] Most deaths result from complications of the vasculitic phase of the disease, most commonly resulting from cardiac failure and/or myocardial infarction, cerebral hemorrhage, kidney disorders, gastrointestinal bleeding, asthmaticus status, opportunistic infections, and other less-avoidable, immunosuppressive complications medication.[1,5,10]
Conclusion
The treatment of these patients should be multidisciplinary, with a comprehensive therapeutic modality, while early diagnosis is imperative. Churg-Strauss syndrome pose diagnostic as well as therapeutic challenge. The treatment of these patients should be multidisciplinary, with a comprehensive therapeutic modality, while early diagnosis is imperative.
Declaration of patient consent
The authors certify that they have obtained a patient inform consent form. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial would not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mukamal LV, Sodré CT, Prata LB, Nakasato F, Cuzzi T, Ramos-E-Silva M, et al. Churg-Strauss syndrome or eosinophilic granulomatosis with polyangiitis: Exuberant classic clinical picture of a rare disease. Case Rep Dermatol. 2018;10:175–81. doi: 10.1159/000489162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol. 1951;27:277–301. [PMC free article] [PubMed] [Google Scholar]
- 3.Masi AT, Hunder GG, Lie JT, Michel BA, Bloch AD, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis) Arthritis Rheum. 1990;33:1094–100. doi: 10.1002/art.1780330806. [DOI] [PubMed] [Google Scholar]
- 4.Watts RA, Lane SE, Bentham G, Scott DG. Epidemiology of systemic vasculitis: A ten-year study in the United Kingdom. Arthritis Rheum. 2000;43:414–9. doi: 10.1002/1529-0131(200002)43:2<414::AID-ANR23>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 5.Neumann T, Manger B, Schmid M, Kroegel C, Hansch A, Kaiser WA, et al. Cardiac involvement in Churg-Strauss syndrome: Impact of endomyocarditis. Medicine (Baltimore) 2009;88:236–43. doi: 10.1097/MD.0b013e3181af35a5. [DOI] [PubMed] [Google Scholar]
- 6.Corradi D, Maestri R, Facchetti F. Postpartum Churg-Strauss syndrome with severe cardiac involvement: Description of a case and review of the literature. Clin Rheumatol. 2009;28:739–43. doi: 10.1007/s10067-009-1143-x. [DOI] [PubMed] [Google Scholar]
- 7.Comarmond C, Pagnoux C, Khellaf M, Cordier JF, Hamidou M, Viallard JF, et al. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss): Clinical characteristics and long-term follow-up of the 383 patients enrolled in the French Vasculitis Study Group cohort. Arthritis Rheum. 2013;65:270–81. doi: 10.1002/art.37721. [DOI] [PubMed] [Google Scholar]
- 8.French Vasculitis Study Group (FVSG) Guillevin L, Pagnoux C, Seror R, et al. The Five-Factor Score revisited: Assessment of prognoses of systemic necrotizing vasculitis based on the French Vasculitis Study Group (FVSG) cohort. Medicine (Baltimore) 2011;90:19–27. doi: 10.1097/MD.0b013e318205a4c6. [DOI] [PubMed] [Google Scholar]
- 9.Ribi C, Cohen P, Pagnoux C, Mahr A, Arène JP, Lauque D, et al. Treatment of Churg-Strauss syndrome without poor-prognosis factors: A multicenter, prospective, randomized, open-label study of seventy-two patients. Arthritis Rheum. 2008;58:586–94. doi: 10.1002/art.23198. [DOI] [PubMed] [Google Scholar]
- 10.Samson M, Puéchal X, Devilliers H, Ribi C, Cohen P, Stern M, et al. Long-term outcomes of 118 patients with eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) enrolled in two prospective trials. J Autoimmun. 2013;43:60. doi: 10.1016/j.jaut.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Roufosse F. Targeting the interleukin-5 pathway for treatment of eosinophilic conditions other than asthma. Front Med (Lausanne) 2018;5:49. doi: 10.3389/fmed.2018.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]


