Abstract
Background:
Femoroacetabular impingement (FAI) is a well-known cause of hip pain in adolescents and young adults. However, the incidence in the general population has not been clearly defined.
Purpose:
To (1) define the population-based incidence of diagnosis of FAI in patients with hip pain, (2) report the trends in diagnosis of FAI over time, and (3) determine the changes in the rate and type of surgical management over time.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A geographic database was used to identify patients who were 14 to 50 years old with hip pain between the years 2000 and 2016. Chart and radiographic review was performed to determine which patients had FAI. To be included, patients had to have a triad of clinical symptoms, physical examination signs, and imaging findings consistent with FAI. Medical records were reviewed to obtain demographic information, clinical history, physical examination findings, imaging details, and treatment details. Statistical analysis determined the overall age- and sex-adjusted annual incidence of FAI diagnosis and trends over time.
Results:
There were 1893 patients evaluated with hip pain, and 716 (38%; 813 hips) had diagnosed FAI. The mean ± SD age was 27.2 ± 8.4 years, and 67% were female. The incidence of FAI diagnosis was 54.4 per 100,000 person-years. Female patients had a higher incidence than male patients (73.2 vs 36.1 per 100,000 person-years; P < .01). Incidence of FAI diagnosis were higher from 2010 to 2016 (72.6 per 100,000 person-years; P < .01) as compared with 2005 to 2009 (45.3) and 2000 to 2004 (40.3). Hip arthroscopy, surgical hip dislocation, and periacetabular osteotomy utilization increased from the 2000-2004 to 2010-2016 periods, respectively: 1 (1%) to 160 (20%; P = .04), 2 (1%) to 37 (5%; P = .01), and 1 (1%) to 22 (3%; P = .58).
Conclusion:
The overall incidence of FAI diagnosis was 54.4 per 100,000 person-years, and it consistently increased between 2000 and 2016. Female patients had a higher incidence than male patients. The utilization of joint preservation operations, including hip arthroscopy, surgical hip dislocation, and anteverting periacetabular osteotomy, increased over time.
Keywords: femoroacetabular impingement, hip pain, incidence
Femoroacetabular impingement (FAI) is a symptomatic clinical syndrome caused by atypical morphology of the acetabulum and/or femoral head-neck junction that leads to abnormal contact between the surfaces.9,10 It is a common cause of hip pain and is associated with the development of early osteoarthritis.6,10,26,28 Diagnostic criteria for FAI syndrome have been refined since they were first described in 1999.19 A triad of clinical symptoms, examination findings, and radiographic findings consistent with FAI is needed to reliably diagnose this condition.11,20 Strict diagnostic criteria are necessary, as radiographic findings consistent with structural impingement morphology are common in asymptomatic patients.8,12,15
Frank et al8 performed a systematic review and found the prevalence of cam and pincer deformity to be 37% and 67% in asymptomatic patients, respectively. A recent study reported the prevalence of radiographic findings consistent with FAI in patients with hip pain to be 60.5%.30 However, there is a paucity of research evaluating the true incidence of FAI utilizing a triad of clinical symptoms, examination findings, and radiographic findings for diagnostic criteria in the general population. We are aware of only 1 study that has attempted to answer this question. Roling et al24 reported an FAI incidence of 17% in 84 patients with groin pain who were seen by their general practitioner during a 1-year period. However, those data were limited by a lack of radiographic parameters used for diagnosis and a small cohort of patients presenting with groin pain.
There is a need in the literature to define the true incidence of FAI syndrome in a large cohort and to determine changes in treatment over time. This would allow clinicians to have a better understanding of the expected number of patients in their community with FAI. To answer this question, we report the findings from a geographically defined cohort of 1893 young patients presenting to the physician with hip pain. The purposes of this study were to (1) define the population-based incidence of FAI diagnosis in patients with hip pain, (2) report the trends in diagnosis of FAI over time, and (3) determine the changes in the rate and type of surgical management over time.
METHODS
Study Population and Design
A geographic population-based cohort study was performed with the Rochester Epidemiology Project (REP) database in Olmsted County, Minnesota, which had a population of 144,260 in 2010. Briefly, the REP is a medical record linkage system that provides access to the complete medical records for all residents of Olmsted County, regardless of the medical facility in which the care was delivered.23,25 After institutional review board approval was obtained (17-004959, 030-OMC-17), the REP was used to identify all patients in a geographic area who presented to a physician with International Classification of Diseases, Ninth Revision or Tenth Revision, diagnostic codes of hip pain, hip impingement, or hip joint disorders between January 2000 and December 2016. All patients were between 14 and 50 years old. The database contained complete diagnostic and procedural information from all applicable medical centers until December 1, 2019. Clinical notes, radiographic images, and operative notes related to the injury were manually reviewed in detail. Patients with a history of avascular necrosis, neuromuscular disorder, trochanteric bursitis, hip fracture, pelvic fracture, previous hip surgery, and/or hip dislocation were excluded. Patients with concomitant hip dysplasia were included.
All patients had anteroposterior and lateral (cross-table, frog-leg, or 45° Dunn view) hip radiographs at their initial physician visit. All radiographs were reviewed by attending-or senior resident–level orthopaedic surgeons (H.P.M., J.Z.). The initial 100 radiographic reviews were evaluated by each of the 2 authors to ensure agreement on the measurements. Parameters were standardized according to the parameters outlined by Clohisy et al.5 Noncompliant radiographs were not included. The radiographic findings considered consistent with FAI are shown in Table 1.
TABLE 1.
Femoroacetabular Impingement–Type Imaging Findings
FAI syndrome was ultimately diagnosed according to the 2016 Warwick Agreement based on the presence of a triad of symptoms, clinical signs, and imaging findings.11 As stated in the agreement, symptoms consistent with FAI are typically motion or position related, resulting in hip or groin pain. Pain may also be felt in the buttock, back, or thigh. In addition, mechanical symptoms such as clicking and locking may be present but are not required.11 The most commonly known clinical sign is pain with hip flexion, adduction, and internal rotation. Patients with FAI may also exhibit posterior impingement signs. The clinical sign or examination maneuver should replicate the patient’s symptoms.11 Patients not meeting the diagnostic criteria for FAI syndrome were excluded from the study.
Statistical Analysis
Age- and sex-specific rates of FAI were calculated using the incidence equation recommended by the Centers for Disease Control and Prevention: number of new FAI diagnoses during a specific period divided by the time that each person was observed, totaled for all persons. Patients who were residents of Olmsted County at the time of hip pain and who fulfilled the study criteria were included in the incidence calculations. Incidence rates were age and sex adjusted to the 2010 population of the United States. The 95% CIs for the incidence rates were constructed with the assumption that the number of incident cases per year followed a Poisson distribution. Incidence trends were examined by use of Poisson regression models with smoothing splines for age and calendar year (Figures 1 and 2). The exact Cochran-Armitage trend test was performed to determine significance of incidence over time by age and sex using the total FAI diagnoses each year as the control variable. All analysis was performed using JMP 12.0.1 software (SAS Institute Inc).
Figure 1.
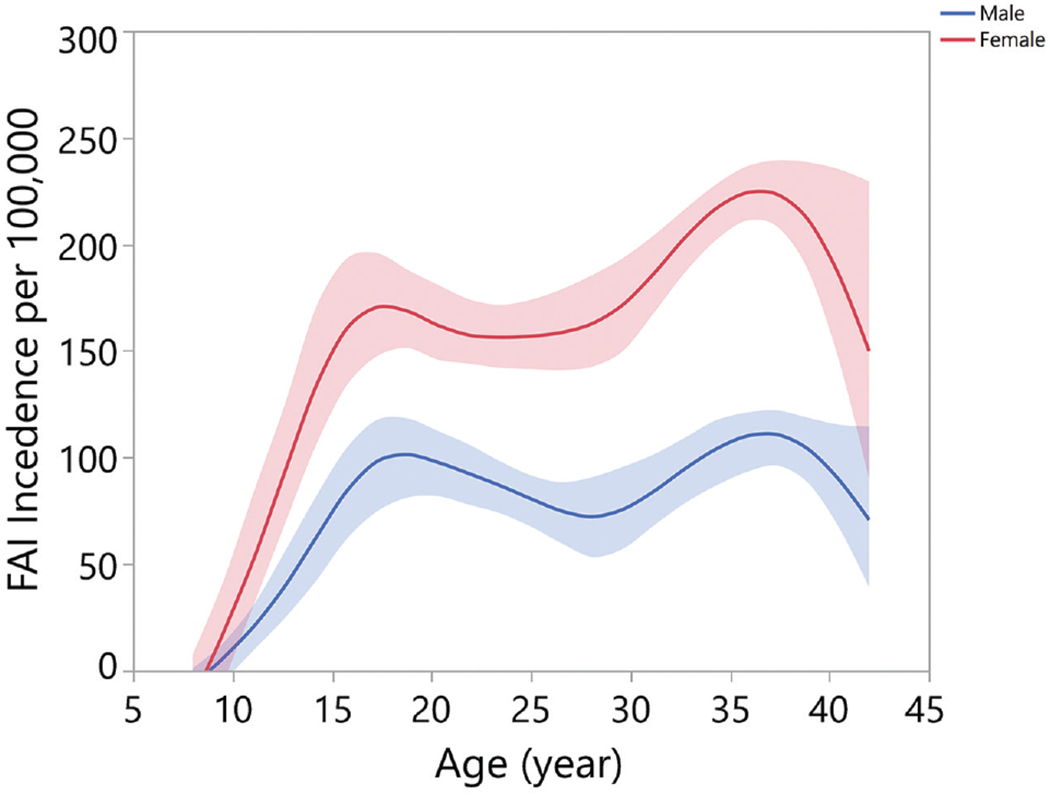
Age-specific incidence of femoroacetabular impingement diagnosis in males and females from 2000 to 2016.
Figure 2.
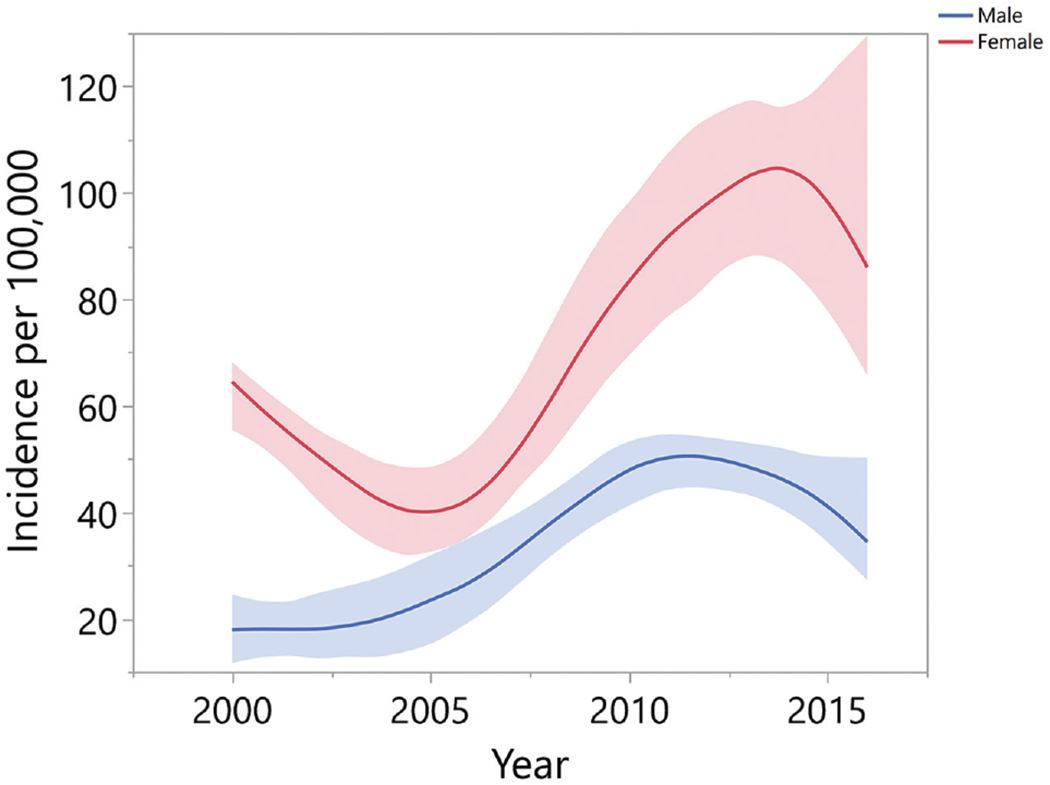
Trends in age-adjusted incidence of femoroacetabular impingement over time in males and females.
RESULTS
Of the 1893 patients presenting with hip pain, 1145 (60%) had positive FAI radiographic findings. Of those, 716 patients (813 hips) also had clinical symptoms and physical examination findings consistent with FAI (38%). We were able to definitively diagnose FAI syndrome in these 716 patients. Of these patients, 69 females and 31 males had bilateral FAI. Patients with FAI syndrome had a mean ± SD age of 27.2 ± 8.4 years, and 67% were female (Table 2). The mean BMI was 28.6 ± 4.9; 22% reported previous or current use of tobacco products; and 7% had diabetes mellitus. On radiographic analysis, 139 hips (17%), 80 hips (10%), and 590 hips (73%) had cam, pincer, and mixed morphology, respectively. Of the 716 patients with FAI, 440 underwent MRI, which indicated that 364 hips (83%) had a definitive labral tear. Of the 813 hips identified, 333 (41%) were diagnosed with FAI at initial patient presentation to the physician with hip pain.
TABLE 2.
Patient Characteristics: 2000-2016a
| 2000-2004 (n = 146) | 2005-2009 (n = 195) | 2010-2016 (n = 468) | Total (N = 813) | |
|---|---|---|---|---|
| Age at date of pain, y | 28.5 ± 8.6 | 27.9 ± 8.2 | 26.5 ± 8.4 | 27.2 ± 8.4 |
| Sex | ||||
| Male | 37 (25.3) | 72 (36.9) | 155 (33.1) | 264 (32.5) |
| Female | 109 (74.7) | 123 (63.1) | 313 (66.9) | 545 (67.0) |
| Laterality | ||||
| Left | 71 (48.6) | 97 (49.7) | 209 (44.7) | 377 (46.4) |
| Right | 75 (51.4) | 98 (50.3) | 259 (55.3) | 432 (53.1) |
| BMI | 29.5 ± 5.0 | 28.8 ± 4.9 | 28.1 ± 4.9 | 28.6 ± 4.9 |
| Comorbidities | ||||
| Smoker | 45 (30.8) | 47 (10.0) | 85 (18.2) | 177 (21.8) |
| Diabetes | 17 (11.6) | 7 (1.5) | 29 (6.2) | 53 (6.5) |
| Radiographic morphology | ||||
| Cam | 28 (19.2) | 31 (6.6) | 80 (17.1) | 139 (17.1) |
| Pincer | 9 (6.2) | 19 (4.1) | 52 (11.1) | 80 (9.8) |
| Mixed | 109 (74.7) | 145 (31.0) | 336 (71.8) | 590 (72.6) |
| FAI diagnosis at initial presentation | 26 (17.8) | 69 (14.7) | 238 (50.9) | 333 (41.0) |
Values are presented as mean ± SD or No. (%). BMI, body mass index; FAI, femoroacetabular impingement.
Population-Based Incidence of Diagnosis FAI
The overall age-and sex-adjusted annual incidence of FAI diagnosis was 54.4 (95% CI, 50.6-58.1) per 100,000 person-years. Female patients had a higher annual incidence of FAI than male patients, at 73.2 per 100,000 (95% CI, 67.0-79.4) versus 36.1 per 100,000 (95% CI, 31.7-40.5; P < .01). Table 3 and Figure 1 illustrate the incidence of all FAI diagnoses by age and sex for the years 2000 to 2016. Age-and sex-specific annual incidence in females was very similar from age 18 to 35 years (112.8-117.1 per 100,000), whereas males had a peak incidence of FAI diagnosis from age 19 to 25 years (62.0 per 100,000).
TABLE 3.
Age- and Sex-Specific Annual Incidence of Femoroacetabular Impingement Diagnosis: 2000-2016
| No. of Cases |
Incidence Rate per 100,000 Person-Years (95% CI) |
|||||
|---|---|---|---|---|---|---|
| Female | Male | Total | Female | Male | Total | |
| Age, y | ||||||
| ≤13 | 8 | 2 | 10 | 3.4 | 0.8 | 2.1 |
| 14-18 | 92 | 49 | 142 | 117.1 | 58.8 | 87.2 |
| 19-25 | 117 | 60 | 177 | 114.2 | 62.0 | 88.9 |
| 26-35 | 204 | 86 | 290 | 112.8 | 47.9 | 80.5 |
| 36-45 | 126 | 68 | 194 | 74.03 | 40.1 | 57.1 |
| Total | 548 | 265 | 813 | 73.2 (67.0-79.4)a | 36.1 (31.7-40.5)a | 54.4 (50.6-58.1)b |
Age adjusted to 2010 US population.
Age and sex adjusted to 2010 US population.
Trends in Diagnosis of FAI
Table 4 illustrates the age-and sex-specific annual incidence of FAI over a 17-year period grouped into 5-year intervals (2000-2016). Incidence of FAI was significantly higher from 2010 to 2016 (72.6 per 100,000 person-years; 95% CI, 65.979.2) when compared with 2000 to 2004 (40.3 per 100,000 person-years; 95% CI, 34.2-46.3) and 2005 to 2009 (45.3 per 100,000 person-years; 95% CI, 38.9-51.7). In all time brackets, female patients had a significantly higher incidence of FAI as compared with male patients (2000-2004, 50.6 vs 29.2; 2005-2009, 55.6 vs 32.3; 2010-2016, 93.9 vs 46.3; P < .001) (Figure 2). Total incidence in male patients significantly increased over time (P < .002). Incidence of male patients with FAI between the ages of 26 and 35 years significantly increased from 2000 to 2016 (10.5 to 77.4 per 100,000 person-years; P < .003). Incidence of FAI in male patients between the ages of 35 and 45 years significantly decreased over time (77.9 to 46.9 per 100,000 person-years; P < .001). Total incidence of FAI in female patients increased over time (P < .001). Incidence in female patients between 14 and 18 years significantly increased from 2000 to 2016 (52.5 to 213.1 per 100,000 person-years; P < .001).
TABLE 4.
Trends in Age- and Sex-Specific Incidence of Femoroacetabular Impingement Diagnosis Over Time: 2000-2016a
| 2000-2004 |
2005-2009 |
2010-2016 |
|||||
|---|---|---|---|---|---|---|---|
| Sex: Age, y | No. | Incidence Rate | No. | Incidence Rate | No. | Incidence Rate | P Value |
| Male | |||||||
| ≤13 | 1 | 1.5 | 0 | 0.0 | 1 | 0.9 | .785 |
| 14-18 | 7 | 28.9 | 13 | 54.3 | 29 | 82.4 | .135 |
| 19-25 | 10 | 37.4 | 18 | 64.7 | 31 | 73.5 | .790 |
| 26-35 | 5 | 10.5 | 19 | 36.8 | 62 | 77.4 | .003 |
| 36-45 | 41 | 77.9 | 22 | 45.3 | 32 | 46.9 | .001 |
| Total | 64 | 29.2 | 72 | 32.3 | 155 | 46.3 | .002 |
| Female | |||||||
| ≤13 | 2 | 3.1 | 4 | 5.9 | 2 | 1.9 | .189 |
| 14-18 | 12 | 52.5 | 8 | 35.1 | 72 | 213.1 | .001 |
| 19-25 | 19 | 69.5 | 27 | 91.6 | 70 | 153.4 | .533 |
| 26-35 | 40 | 83.8 | 56 | 107.6 | 108 | 133.3 | .341 |
| 36-45 | 36 | 67.9 | 28 | 57.4 | 61 | 89.2 | .179 |
| Total | 109 | 50.6 | 123 | 55.6 | 313 | 93.9 | .001 |
| Totalb | 40.3 (34.25-46.3) | 45.3 (38.9-51.7) | 72.6 (65.9-79.2) | ||||
Bold indicates P < .05.
Incidence (95% CI) is age and sex adjusted to 2010 US population.
FAI Management Trends Over Time
In total, 220 (27%) hips went on to surgical management. Table 5 describes the trends in management of FAI over time. For patients with FAI, nonoperative treatment with physical therapy was common (81%). Overall, 274 hips had an intra-articular steroid injection, and the rate significantly increased over time (36 to 168 hips, P < .02). Hip arthroscopy was the primary method of operative management, totaling 160 hips (26 bilateral hips) over the 16 years. The number of hip arthroscopy procedures significantly increased over time (P < .04). Surgical hip dislocation (SHD) also significantly increased over time (P < .01), although the majority of SHDs were performed in the early 2010s. The number of combined cases of hip arthroscopy–periacetabular osteotomy (PAO) did not significantly increase over time. In all cases, anteverting PAO was performed only for patients with acetabular retroversion and limited internal rotation. The decision to perform SHD versus hip arthroscopy was primarily surgeon dependent and unrelated to patient factors.
TABLE 5.
Trends in Management of Femoroacetabular Impingement: 2000-2016a
| 2000-2004 (n = 146) | 2005-2009 (n = 195) | 2010-2016 (n = 468) | Total (N = 813) | P Value | |
|---|---|---|---|---|---|
| Nonoperative | |||||
| Participation in physical therapy | 113 (77) | 154 (79) | 389 (83) | 656 (81) | .091 |
| Intra-articular steroid injection | 36 (25) | 70 (36) | 168 (36) | 274 (34) | .021 |
| Operative | |||||
| Hip arthroscopy only | 1(1) | 7 (4) | 152 (32) | 160 (20) | .040 |
| Hip arthroscopy + anteverting PAO | 0 (0) | 0 (0) | 15 (3) | 15 (2) | .097 |
| Anteverting PAO only | 1(1) | 0 (0) | 7(1) | 8(1) | .581 |
| Surgical hip dislocation | 2 (1) | 13 (7) | 22 (5) | 37 (5) | .010 |
Values are presented as No. (%). Bold indicates P < .05. PAO, periacetabular osteotomy.
DISCUSSION
The radiographic findings associated with FAI are well-defined.5 Multiple studies have reported the prevalence of radiographic structural deformity in asymptomatic individuals.8,12,15 One study reported the prevalence of radiographic parameters of structural deformity in patients with hip pain.30 However, the clinical diagnosis of FAI syndrome requires the presence of a triad of clinical symptoms, physical examination signs, and imaging findings.11 We are aware of 1 study that reported the incidence of true FAI syndrome, although this was in a small cohort and the radiographic parameters were not well-defined.24 To our knowledge, the present study is the first to define the population-based incidence of FAI diagnosis in a large cohort of patients with hip pain. We found that the overall annual incidence of FAI diagnosis was 54.4 per 100,000 person-years. Female patients had a higher incidence than male patients, and the rate of diagnosis and surgical management increased over time.
The present study represents a large cohort of young patients (>1800) presenting to a physician with hip pain. Strict diagnostic criteria were used to define the incidence of FAI diagnosis, which had yet to be defined in a large cohort. Roling et al24 reported the incidence of FAI in patients presenting to a general practitioner in the Netherlands during a 1-year period. Of the 84 patients presenting with groin pain, 17% received a diagnosis of FAI via the triad of clinical, physical examination, and radiographic findings. Unfortunately, the radiographic diagnostic criteria were not defined, and not all patients had radiographs. The authors estimated that an additional 30% had FAI based on symptoms for a total of 47%, but no radiographs were performed. Additionally, their study included slightly older patients (15-60 years). Our study had a similar percentage of patients (38%) presenting with hip pain to receive a diagnosis of FAI. The prevalence of radiographic findings consistent with FAI has been evaluated more often.8,12,15,30 A systematic review evaluated the prevalence of cam-and pincer-type FAI on radiographs in asymptomatic patients. It revealed that 37% of asymptomatic patients had cam-type findings and 67% had pincer-type findings.8 The prevalence of radiographic findings consistent with FAI in a large cohort of patients presenting with hip pain was recently found to be 60.5%.30 The percentage of patients with FAI syndrome in the present study was less than that in the studies evaluating radiographs only. This is an expected finding since it is known that many asymptomatic patients have findings consistent with FAI on radiographs alone.8
Female patients consistently had a higher incidence of FAI during each period between 2000 and 2016. Roling et al24 found the same to be true, but other studies have yielded varied results. Multiple studies have reported radiographic findings consistent with FAI to be more common in asymptomatic males than asymptomatic females.13,14,17 In contrast, Clohisy et al4 noted an increased incidence in female patients when evaluating symptomatic patients who ended up having surgery. These data suggest that symptomatic FAI is more commonly found in females, as suggested in our study. Another interesting finding was that for patients aged >35 years, the incidence of FAI decreased for both male and female patients. We suspect that patients who are not symptomatic before 35 years of age are less likely to become symptomatic later on. The incidence of FAI consistently increased over time in the present study. This is an expected finding, as awareness and understanding of the pathology have increased since first being described in 1999.19 We believe that, although it may be multifactorial, the primary reason for the increased incidence over time is related to clinician education on the diagnosis of FAI. Overall, 41% of patients with FAI had the condition correctly diagnosed at initial physician presentation. As expected, this consistently increased over time, and between 2010 and 2016, 52% of patients received the correct diagnosis. Many of the patients were evaluated initially by a general practitioner before referral to a specialist. Although increased clinician understanding is still needed, these data suggest that the recognition of FAI syndrome is improving.
Nonoperative treatment was consistently utilized throughout this study, but hip arthroscopy increased significantly during each 5-year period. This is expected, as hip arthroscopy techniques and understanding have improved. The majority of patients engaged in physical therapy in all periods, and consistently around one-third of patients received an intra-articular steroid injection. It is widely accepted that nonoperative management should be the first-line treatment of FAI.7 This was the case in the present study. Some patients ultimately had failure of nonoperative management and proceeded to operative management. The consistent increase in hip arthroscopy in our study aligns with what has been shown in the literature.7,22 As noted by Zhang and Feeley,29 the utilization of hip arthroscopy has risen meteorically. Montgomery et al18 reported a 365% increase in hip arthroscopy utilization since 2004. Furthermore, Bonazza et al3 analyzed a database of >30,000 hip arthroscopy surger and found that the number of procedures performed between 2008 and 2013 tripled. The number of SHD procedures increased during each time frame. The majority of SHD cases were performed in the early 2010s but relatively decreased thereafter as hip arthroscopy was more commonly utilized. The increase was likely due to increased understanding and diagnosis of FAI as initially described by Dr Ganz.9 A small percentage of patients underwent anteverting PAO in this study, but its utilization consistently also increased over time. This is likely related to the increased understanding of acetabular retroversion and the need for open correction in some cases.21 Combined hip arthroscopy and PAO increased over time but not significantly. This finding was likely not significant, owing to the low sample size.
The present study is the first to define the population-based incidence of FAI syndrome diagnosis in a large cohort of patients, but there are limitations to consider. This was a retrospective study, which has inherent limitations. Additionally, there was no control group. Clinician understanding of FAI and appropriate documentation of diagnostic physical examination signs in the early years of this study were limited in some cases. We maintained strict diagnostic criteria. Because of this, it is possible that patients with FAI syndrome were excluded owing to a lack of documented positive physical examination findings. This may have contributed to the increased diagnosis over time, as clinician understanding and documentation of FAI syndrome have improved. Additionally, only 1 lateral radiographic view was required for inclusion. As such, it is possible that a cam lesion may have been underestimated in some circumstances. Finally, as with any geographic cohort, this study was limited by the demographics of the studied area and may not be generalizable to all geographic areas.
CONCLUSION
The overall incidence of FAI diagnosis was 54.4 per 100,000 person-years, and it consistently increased between 2000 and 2016. Female patients had a higher incidence than male patients. The utilization of joint preservation operations, including hip arthroscopy, SHD, and anteverting PAO, increased over time.
Acknowledgments
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was partially funded by the National Institutes of Health under grant T32AR056950 as well as Jiangsu Health International Exchange Program (JSH-2018-004) and grant UL1 TR002377 from the National Center for Advancing Translational Sciences. H.P.M. has received hospitality payments from DePuy Synthes Sales. M.D.L. has a family member with the following disclosures: intellectual property royalties and consulting fees from Arthrex Inc, Ossur, and Smith & Nephew. B.A.L. has received consulting fees from Arthrex Inc and Smith & Nephew; research support from Biomet, Stryker, and Smith & Nephew; speaking fees from Linvatec; and royalties from Arthrex Inc. A.J.K. has received research support from Aesculap/B. Braun, Arthritis Foundation, Ceterix, Exactech, Gemini Medical, Histogenics; consulting fees from Arthrex, JRF Ortho, DePuy, Vericel; and intellectual property royalties from Arthrex. A.J.K. is also a shareowner in Responsive Arthroscopy. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
REFERENCES
- 1.Beall DP, Sweet CF, Martin HD, et al. Imaging findings of femoroacetabular impingement syndrome. Skeletal Radiol. 2005;34(11):691–701. [DOI] [PubMed] [Google Scholar]
- 2.Blankenbaker DG, Tuite MJ. The painful hip: new concepts. Skeletal Radiol. 2006;35(6):352–370. [DOI] [PubMed] [Google Scholar]
- 3.Bonazza NA, Homcha B, Liu G, Leslie DL, Dhawan A. Surgical trends in arthroscopic hip surgery using a large national database. Arthroscopy. 2018;34(6):1825–1830. [DOI] [PubMed] [Google Scholar]
- 4.Clohisy JC, Baca G, Beaule PE, et al. Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. Am J Sports Med. 2013;41(6):1348–1356. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, Carlisle JC, Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(suppl 4):47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ecker TM, Tannast M, Puls M, Siebenrock KA, Murphy SB. Pathomorphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res. 2007;465:46–52. [DOI] [PubMed] [Google Scholar]
- 7.Fairley J, Wang Y, Teichtahl AJ, et al. Management options for femoroacetabular impingement: a systematic review of symptom and structural outcomes. Osteoarthritis Cartilage. 2016;24(10):1682–1696. [DOI] [PubMed] [Google Scholar]
- 8.Frank JM, Harris JD, Erickson BJ, et al. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015;31(6):1199–1204. [DOI] [PubMed] [Google Scholar]
- 9.Ganz R, Gill TJ, Gautier E, et al. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001; 83(8):1119–1124. [DOI] [PubMed] [Google Scholar]
- 10.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003; 417:112–120. [DOI] [PubMed] [Google Scholar]
- 11.Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19): 1169–1176. [DOI] [PubMed] [Google Scholar]
- 12.Hack K, Di Primio G, Rakhra K, Beaule PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2444. [DOI] [PubMed] [Google Scholar]
- 13.Jung KA, Restrepo C, Hellman M, et al. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93(10):1303–1307. [DOI] [PubMed] [Google Scholar]
- 14.Kapron AL, Anderson AE, Aoki SK, et al. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS exhibit selection. J Bone Joint Surg Am. 2011;93(19):e111(1–10). [DOI] [PubMed] [Google Scholar]
- 15.Kapron AL, Peters CL, Aoki SK, et al. The prevalence of radiographic findings of structural hip deformities in female collegiate athletes. Am J Sports Med. 2015;43(6):1324–1330. [DOI] [PubMed] [Google Scholar]
- 16.Kutty S, Schneider P, Faris P, et al. Reliability and predictability of the centre-edge angle in the assessment of pincer femoroacetabular impingement. Int Orthop. 2012;36(3):505–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leunig M, Juni P, Werlen S, et al. Prevalence of cam and pincer-type deformities on hip MRI in an asymptomatic young Swiss female population: a cross-sectional study. Osteoarthritis Cartilage. 2013;21(4):544–550. [DOI] [PubMed] [Google Scholar]
- 18.Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013;29(4):661–665. [DOI] [PubMed] [Google Scholar]
- 19.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363: 93–99. [PubMed] [Google Scholar]
- 20.Nepple JJ, Prather H, Trousdale RT, et al. Clinical diagnosis of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(suppl 1):S16–S19. [DOI] [PubMed] [Google Scholar]
- 21.Parry JA, Swann RP, Erickson JA, et al. Midterm outcomes of reverse (anteverting) periacetabular osteotomy in patients with hip impingement secondary to acetabular retroversion. Am J Sports Med. 2016; 44(3):672–676. [DOI] [PubMed] [Google Scholar]
- 22.Reiman MP, Thorborg K. Femoroacetabular impingement surgery: are we moving too fast and too far beyond the evidence? Br J Sports Med 2015;49(12):782–784. [DOI] [PubMed] [Google Scholar]
- 23.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87(12):1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roling MA, Mathijssen NM, Bloem RM. Incidence of symptomatic femoroacetabular impingement in the general population: a prospective registration study. J Hip Preserv Surg. 2016;3(3):203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanders TL, Pareek A, Desai VS, et al. Low accuracy of diagnostic codes to identify anterior cruciate ligament tear in orthopaedic database research. Am J Sports Med. 2018;46(12):2894–2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sankar WN, Nevitt M, Parvizi J, et al. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. 2013;21(suppl 1):S7–S15. [DOI] [PubMed] [Google Scholar]
- 27.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188(6):1540–1552. [DOI] [PubMed] [Google Scholar]
- 28.Wyles CC, Heidenreich MJ, Jeng J, et al. The John Charnley Award: redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res. 2017;475(2):336–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang AL, Feeley BT. Editorial commentary: the rise of hip arthroscopy—temporary trend or here to stay? Arthroscopy. 2018; 34(6):1831–1832. [DOI] [PubMed] [Google Scholar]
- 30.Zhou J, Melugin HP, Hale RF, et al. The prevalence of radiographic findings of structural hip deformities for femoroacetabular impingement in patients with hip pain. Am J Sports Med. 2020;48(3):647–653. [DOI] [PubMed] [Google Scholar]


