Abstract
To promote rational drug use in developing countries, it is important to assess drug use pattern, using the World Health Organisation (WHO) drug indicators. The aim of this study was to assess the prescription patterns at the primary healthcare centres in Khartoum locality, compare prescription habits between consultants and medical officers and identify polypharmacy and its effect on prescription quality using WHO drug indicators. The study was descriptive and cross-sectional. The sample was selected using systematic random sampling. Five hundred and four patient prescriptions were reviewed. The study showed that the average number of drugs prescribed per encounter was 2.4%, the percentage of drugs’ generic name was 49.8% the percentage of encounter with antibiotic was 34.1%. Other important components for completeness of prescription including prescribers name were mentioned in almost all encounters, whereas the patient’s age was stated in 38.3%. Drug strength, quality and doses frequency were stated in 64.1%, 69.4% and 70.4%, respectively. Consultant tendency towards polypharmacy prescription was in 14.9% compared to medical officers (85.1%). The quality of prescriptions was classified as complete, incomplete or deficient with 29.4%, 60.7% and 9.9%, respectively.
Keywords: Prescription pattern, Primary health centres, Khartoum, Sudan
INTRODUCTION
A robust healthcare system needs to be able to support the responsible use of medicines by assuring that essential medicines are procured efficiently through centralised caring, delivered effectively to healthcare providers and patients without stock-outs and routinely checked to assure quality [1]. The World Health Organisation (WHO) encourages governments to facilitate the implementation of evidence-based treatment guidelines to avoid unnecessary adverse consequences on health outcomes and expenditure [1]. Medicine plays an essential role in protecting, maintaining and restoring health. The rationale drug use requires medicine and dosages to satisfy patients’ clinical status over the entire period of treatment and with the lowest cost burden [2]. Prescribing is a complexity of medical knowledge that is used to carefully judge the risks and benefits of treatment [3]. An order from a physician to the dispenser is considered as a legal document. So it must be clearly, accurately and completely written to avoid potentially preventable, but serious, prescription errors. The WHO estimates that more than half of all medicines are prescribed, dispensed or sold inappropriately [2]. The irrational prescribing practices have unintended consequences on patient health and treatment costs [4,5]. Studies have found that prescribing is the most challenging area for new graduates, and that errors are common, among both trainees and professionals [6]. The physicians should adhere to the guidelines for the prescriptions’ writing to ensure patient safety, as there is a high incidence of documentation errors in the traditional handwritten prescription process. The irrational practice of medicine is influenced by numerous factors which include self-prescribing medication, polypharmacy prescriptions, unjustified prescribed antibiotics, injections misuse and prescribing outside the clinical guidelines [2,4,5]. This is besides patients, practitioners, working environment, drug supply systems, laws and drug regulations, information and misinformation related to drugs and influence of drug companies’ intentions [7]. The quality of basic training in pharmacotherapy for undergraduate medical and paramedical students has a significant influence on future prescribing [8]. Rational pharmacotherapy training should adopt clinical guidelines and essential medicines lists for effective prescribing practices [8]. In this issue, the British Pharmacological Society, in partnership with the Medical Schools Council, developed the Prescribing Safety Assessment, which is an online tool, aiming to sustain the relationship between pharmacology education and the application of knowledge [9]. Regular auditing for the prescribing and dispensing process using the standard treatment guidelines should be ensured. To achieve this, a set of drug indicators were developed to measure healthcare facilities’ performance concerning drug utility by the WHO in partnership with the International Network of Rational Use of Drugs in the 1990s [10]. These indicators are facility-based measures meant to describe practices representative of a sample of health facilities. They are classified into prescribing, patient care and facility-specific ones [6,10]. The prescribing indicators measure the performance of healthcare providers in several key dimensions related to the appropriate use of the drug. These indicators and (optimal values) are:
The average number of medicines per encounter (1.6-1.8)
Percentage of drugs prescribed by generic name (100%)
Percentage of encounters with an antibiotic prescribed (20.0-26.8)
Percentage of encounters with an injection prescribed (13.4-24.1)
Percentage of medicines prescribed from essential medicines list or formulary (100%).
The patient care indicators are:
Average consultation time ≥10 minutes
An average dispensing time ≥90 seconds
Percentage of drugs dispensed (100%)
Percentage of drugs adequately labelled (100%)
Patients’ knowledge of correct dosage (100%)
The healthcare facility indicators are:
Availability of copy of essential drug list or formulary (100%)
Availability of key drug (100%)
Medicine prescribing process at health facilities does not follow standardised guidelines for prescribing; this was observed during our fieldwork and supported by a study conducted in Sudan in 2006 [11]. The main objective of this study is to assess the quality of prescription at primary healthcare centres in Khartoum locality, Khartoum State, Sudan.
MATERIALS AND METHODS
The study design was a descriptive, cross-sectional study. It was conducted in Khartoum locality within Khartoum State. The locality is one of the three largest localities in the state, and contains 15 healthcare centres. Out of these, Alsahafa, Samir and Alshagara Health Centres were randomly selected. These are public healthcare centres, serving areas of high intensity of population in South Khartoum. They work for 24 hours per day, including Friday, and are run by consultants and general practitioners. The data were collected during the period from June to July 2014, by three well-trained pharmacist assistants who utilised a checklist. It included all medical prescriptions, irrespective of age and gender that were received and kept in the healthcare centres’ pharmacies. Those for other healthcare centres were excluded.
The sample size was calculated by a statistician to be:
where:
n is the required sample size, z = confidence level at 95% (standard value of 1.96).
p is the probability (0.5), q = 1-p, d = margin of error at 5% (standard value of 0.05)
Non-response rate (30%) =115.2
Sample size was estimated to be = 384+115.2 =499.2 ~ 500.
The sampling technique was a systemic randomised one. The prescriptions were evaluated for the presence of the WHO prescribing indicators (standard indicators). These include the average of drugs per encounter, the percentage of the drug in generic name and the percentage of encounters comprised an antibiotic. It was also analysed for complementary elements that involve the presence of demographic data, the diagnosis, drug dosages, strength, quantity and instruction for patients. These were independent variables. The dependent variable was the quality of the prescription which was classified into complete, incomplete and deficient ones.
The data were analysed by using the Statistical Package for Social Science version 21. Based on the objectives of the study, descriptive statistics in the form of frequency, percentage and mean were used to quantify the prescription elements. A chi-square test was applied for the qualitative variables. In this study, p-value < 0.05 was considered as statistically significant, and CI of 95% was used to test the association between variables.
RESULTS
A total of 504 prescriptions were assessed. Out of these, 380 were prescribed by general practitioners (75.4%), while 124 were prescribed by consultants (24.6%). The elements of the prescription are shown in Table 1.
Table 1.
Details of the prescription elements
| Percent | Number | Element |
|---|---|---|
| 94.6 5.4 0 100 0 100 |
477 27 0 504 0 504 |
Prescriber information Name Mentioned Not Address Mentioned Not Telephone number Mentioned Not |
| 100 38.3 61.7 6 94 5 95 0 100 0 100 |
504 191 311 30 474 25 479 0 504 0 504 |
Patient information Name Mentioned Age Mentioned Not Gender Mentioned Not Weight Mentioned Not Address Mentioned Not Telephone number Mentioned Not |
| 1.4 98.6 |
7 497 |
Pharmacist name Mentioned Not |
Other essential complementary elements for completeness of prescription are summarised in Table 2.
Table 2.
Other essential complementary elements of the prescription
| Percentage | Number | Element |
|---|---|---|
| 97 3 |
489 15 |
Prescription date Mentioned Not |
| 49.8 39.7 10.5 |
251 200 53 |
Drug name Generic Trade Mixed |
| 64.1 3 32.9 |
323 15 166 |
Drug strength Mentioned for all drugs Some None |
| 69.4 3.2 27.4 |
350 16 138 |
Drug quantity Mentioned for all drugs Some None |
| 70.4 4.8 24.8 |
355 24 125 |
Instruction to patient Full instruction Partial None |
| 49.6 50.4 |
250 254 |
Diagnosis Mentioned Not |
| 88.5 8.1 3.4 |
446 41 17 |
Prescription handwriting Readable Partially Unreadable |
The average number of drugs per prescription was 2.5 (maximum 10, Minimum 1). Less than one-fifth (18.7%) of the encounters contained polypharmacy drugs, as shown in Table 3,4.
Table 3.
Percentages of polypharmacy drugs per prescription
| Drugs per prescriptions | Frequency | Percentage |
|---|---|---|
| Poly pharmacy | 94 | 18.7 |
| No | 410 | 81.3 |
| Total | 504 | 100 |
Table 4.
The World Health Organisation’s core (standard) prescribing indicators
| Percent | Core indicators |
|---|---|
| 2.5 | Average number of drugs prescribed per encounter |
| 34.1 | Percentage of encounter with antibiotic |
| 49.8 | Percentage of drugs generic name |
| Not available | Percentage of medicines prescribed from essential medicines list or formulary |
More frequently prescribed drugs were antibiotics (208, 34.1%), analgesics (172, 41.3%) and antihypertensive (119, 23.6%).
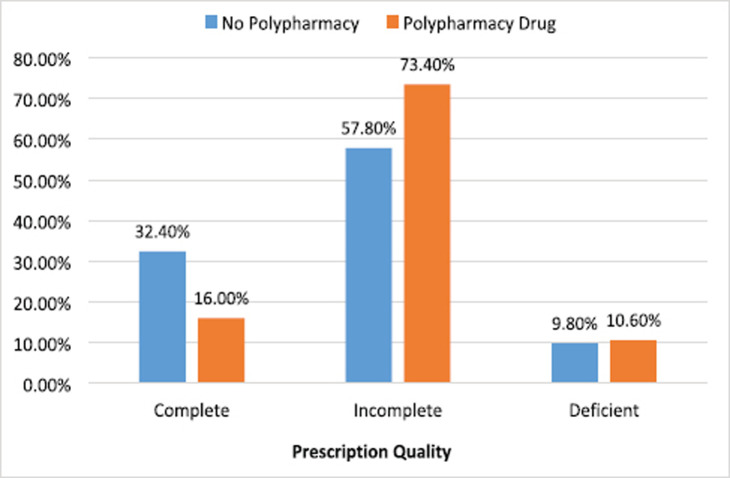
The quality of prescription was classified as complete (148, 29.4%), incomplete (306, 60.7%) and deficient (50, 9.9%). There was no significant correlation between the quality of prescription and prescribers’ qualifications (p = 0.25). The correlation between the prescriber’s qualification and polypharmacy was statistically significant (p = 0.015). A total of 410 prescriptions contained no polypharmacy drugs, of which 300 (73.2%) were prescribed by medical officers and 110 (26.8%) by consultants. Of 94 prescriptions which contained polypharmacy, 80 (85.1%) were prescribed by medical officers and 14 (14.9%) by consultants. The association between polypharmacy and quality of prescription (Figure 1) was found to be significant (p value = 0.006).
Figure 1.
Association between polypharmacy and prescription quality.
DISCUSSION
A prescription reflects the healthcare professional’s attitude towards the disease being treated and the type of healthcare system in the country. The current study reveals that the mean number of drugs per encounter was 2.5. The value was above the permissible one (1.6-1.8) and better than those reported elsewhere [12,13]. Moreover, less than one-quarter (18.7%) of the encounters contained four or more drugs suggesting a trend of polypharmacy. This trend of prescribing might harm patients’ health by increasing the drug’s adverse reactions and interactions, reducing patients’ compliance or increase the risk of drug resistance. There are several reasons for that including poor adherence to guidelines and lack of continuous medical education for healthcare professionals.
The generic name prescribing is a safe measure for patients and an easing tool for communication between healthcare professionals [14]. In the present study, only 49.8% of the medicine was prescribed in generic name. This is far from the permissible value (100%), but similar to values from most of the developing countries (<40%) [15]. It could be attributed to the influence of healthcare professional’s faith on branded products, intentions of pharmaceutical companies or lack of adherence to guidelines.
The percentage of encounters which comprised an antibiotic represented 41.6%, which was higher than the permissible ranges (20.0%-26.8%), and in a line with the majority of those reported from developing countries (24%-50%) [15]. Irrationality in prescribing an antibiotic is a universal problem that ultimately leads to an increased chance of adverse drug reactions and the frequency of hospitalisation.
In the present study, complementary parameters involving the patient’s name, age and gender, the healthcare professional’s name and the prescribing date represented 66.1%, 38.3%, 6%, 94.6% and 97%, respectively. These results are better than those reported previously from Sudan: name = 18.8%, prescriber’s name = 6.5%, gender = 5.7% and date = 88.8%, respectively [11]. These differences in results between hospitals and healthcare centres in Sudan could represent a base for further studies.
Besides missing the healthcare professional’s address, telephone number and pharmacist’s names, the weight was recorded in only 5%. These data are essential in case further clarification and contact is needed. Also, the age and weight parameters facilitate the choice of proper dosage and help dispense the proper form of the drug, especially in the paediatric age group.
The diagnosis was present in 49.6% of the prescriptions, which is lower than that reported from India (64.66%) [16]. It influences the drug-dispensing process, especially when similarly sound drugs are prescribed, and might be of help in case of illegible handwritten prescriptions.
More than half (64.1%) of the prescriptions comprised the drug’s strength, similar to a study conducted in Pakistan (65.82%) [15]. The drug quantity was mentioned in 69.4%, while only 24.8% of the prescriptions contained instructions to patients. These parameters are important for dispensing different paediatric formulae and have great significance when prescribing dangerous narcotic drugs.
The proportion of prescriptions with illegible handwriting (11.5%) is better than that reported from India (68%) [17]. Illegible handwriting is distressing to the pharmacist and can lead to serious errors. The overall quality of prescription was poor as the completed ones comprised only 29.4%. This result is comparable to a previous study conducted in Sudan [18] where 96% of the prescriptions did not include one or more necessary elements. Cost-effective multifaceted interventions to improve prescribing and dispensing practice were thereafter recommended [19].
The study showed no significant association between prescription quality and healthcare professional’s qualification (p = 0.05). This might be attributed to a deficiency in continuous medical education. There was a significant correlation between the quality of prescription and polypharmacy drugs (p = 0.006), which indicates a negative impact of polypharmacy on prescription quality. Also, a statistically significant association between polypharmacy prescribing and healthcare professional’s qualification (p = 0.015) was documented. This justifies fewer propensities of consultants for polypharmacy, which might be clarified if more indicators were analysed.
The study was limited in that it was not designed to assess other WHO indicators, such as patient care and health facility indicators, and further studies are needed to explore these areas. However, the study had strengths by investigating at the first level of contact of individual, family and community with the national healthcare systems, and by looking at complementary prescription parameters.
CONCLUSION AND RECOMMENDATIONS
In conclusion, the WHO indicators represented in the mean number of drugs per encounter was 2.5, the percentage of drug prescribed in generic name was 49.8% and the percentage of encounters with an antibiotic was 41.6%. All observed values for prescribing indicators have deviated from the established norm.
Essential parameters for completeness of prescription showed deficiencies. Overall, there was legible handwriting, but the quality of the prescription was poor.
The authors would, therefore, recommend:
Problem-based teaching of pharmacotherapy for undergraduates to improve the prescribing process.
Adoption of the WHO guidelines for drug prescription in Khartoum healthcare centres.
Auditing of the prescriptions quality.
Updating the prescription form to include all items recommended by the WHO.
Utilising computerised prescription at primary healthcare centres in Khartoum.
Enforce pharmacists to play their role in drug utilisation.
Further studies using WHO indicators in all three areas: prescribing, patient care and health facility.
ACKNOWLEDGEMENTS
The authors would like to thank all pharmacists and pharmacist assistants in the health centres for their great and valuable help.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this article.
FUNDING
None.
ETHICAL APPROVAL
Ethical approval was obtained from the Ministry of Health, Sudan, and University of Medical Science and Technology, Khartoum, Sudan. Informed consent was obtained from the participants and confidentiality was ensured at all stages.
REFERENCES
- 1.World Health Organization. The pursuit of responsible use of medicines: sharing and learning from country experiences. WHO/EMP/MAR/2012.3. Available from: www.who.int .
- 2.World Health Organization. Policy perspectives on medicines-promoting rational use of medicines: core components. [2020 Aug 10];2002 Sep; Available from: www.who.int .
- 3.WHO Drug Information. 2018;32(2):194–220. Available from: https://www.who.int/medicines/publications/druginformation/issues/DrugInformation2018_Vol32-2/en/ [Google Scholar]
- 4.Desalegn AA. Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, South Ethiopia: a cross-sectional study. BMC Health Serv Res. 2013;13(1):170. doi: 10.1186/1472-6963-13-170. https://doi.org/10.1186/1472-6963-13-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Atif M, Sarwar MR, Azeem M, Umer D, Rauf A, Rasool A, et al. Assessment of WHO/INRUD core drug use indicators in two tertiary care hospitals of Bahawalpur, Punjab, Pakistan. J Pharm Policy Pract. 2016;9(1):27. doi: 10.1186/s40545-016-0076-4. https://doi.org/10.1186/s40545-016-0076-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ross S, Bond C, Rothnie H, Thomas S, Macleod MJ, et al. What is the scale of prescribing errors committed by junior doctors? A systematic review. Br J Clin Pharmacol. 2009;67(6):629–40. doi: 10.1111/j.1365-2125.2008.03330.x. https://doi.org/10.1111/j.1365-2125.2008.03330.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. The use of essential drugs: sixth report of the WHO Expert Committee. [2015 Oct 18];1995 Available from: http://apps.who.int/iris/handle/10665/37340 . [PubMed]
- 8.Chapter-3, Rationality of Drugs. 2018;10(2):48–54. Available from: http://www.locostindia.com/CHAPTER_3/Rationality%20of%20Drugs.htm . [Cited] Pharmaspire. [Google Scholar]
- 9.Maxwell SRJ, Cameron IT, Webb DJ. Prescribing safety: ensuring that new graduates are prepared. Lancet. 2015;385:579–81. doi: 10.1016/S0140-6736(14)62339-4. https://doi.org/10.1016/S0140-6736(14)62339-4. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Geneva, Switzerland: WHO; 1993. [2020 Aug]. How to investigate drug use in health facilities. Selected drug use indicators. Available from: https://apps.who.int/iris/handle/10665/60519 . [Google Scholar]
- 11.Yousif E, Ahmed A.M, Abdalla ME, Abdelgadir MA. Short communication: Deficiencies in medical prescriptions in a Sudanese hospital. Easter. Mediterr Health J. 2006;12(6):915–918. [PubMed] [Google Scholar]
- 12.Ragam AS, Acharya S, Holla R. Assessment of drug use pattern using World Health Organization prescribing indicators in a tertiary care hospital in Mangalore: a cross-sectional study. Natl J Physiol Pharm Pharmacol. 2017;7(10):1026–30. [Google Scholar]
- 13.Tripathy R, Lenka B, Pradhan MR. Prescribing activities at district health care centres of Western Odisha. Int J Basic Clin Pharmacol. 2015;4:419–21. https://doi.org/10.18203/2319-2003.ijbcp20150005. [Google Scholar]
- 14.Akl OA, El Mahalli AA, Elkahky AA, Salem AM. WHO/INRUD drug use indicators at primary healthcare centers in Alexandria, Egypt. J Taibah Univ Med Sci. 2014;9(1):54–64. https://doi.org/10.1016/j.jtumed.2013.06.002. [Google Scholar]
- 15.Atif M, Sawar M, Azeem M, Naz M, Amir S, Nazir K. Assessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, Pakistan. BMC Health Serv Res. 2016;16:684. doi: 10.1186/s12913-016-1932-2. https://doi.org/10.1186/s12913-016-1932-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shipra J, Zafar YK, Prerna U, Kumar A. Assessment of prescription pattern in a private teaching hospital in India. Int J Pharm Sci. 2013;3(3):219–22. [Google Scholar]
- 17.Bachewar NP, Choudhari S R, Dudhgaonkar S. Assessment of prescription pattern using WHO drug prescribing indicators in medicine wards of a tertiary care teaching hospital. Int J Basic Clin Pharmacol. 2017;6(8):2070–7. https://doi.org/10.18203/2319-2003.ijbcp20173298. [Google Scholar]
- 18.Awad All, Himad HA. Drug-use practices in teaching hospitals of Khartoum state, Sudan. Eur J Clin Pharmacol. 2006;62(12):1087–93. doi: 10.1007/s00228-006-0216-x. https://doi.org/10.1007/s00228-006-0216-x. [DOI] [PubMed] [Google Scholar]
- 19.Holloway K, Dijk VL. 3rd. Geneva, Switzerland: World Health Organization; 2011. The world medicines situation 2011, rational use of medicines; pp. 1–34. [Google Scholar]