Abstract
Introduction
Proximal junctional kyphosis (PJK) is an acute complication of adult spinal deformity (ASD) surgery and may require re-operation because of proximal junctional failure (PJF). PJK causes and prevention strategies remain unknown. This study aimed to investigate the differences in the backgrounds of patients with PJK, compared to those without PJK, in ASD surgery.
Methods
We included data from 86 patients who underwent ASD surgery between 2012 and 2018. There were 40 patients (46.5%) with PJK; 46 patients did not have PJK until the last follow-up. We evaluated patient demographics, clinical outcomes, and radiographic parameters, such as Cobb angle and spinopelvic parameters on standing X-ray films, in each group.
Results
There was no significant difference in patient demographics, clinical outcomes, or preoperative radiographic parameters. Postoperative pelvic incidence minus lumbar lordosis (PI-LL) and pelvic tilt (PT) were significantly lower in the PJK group, and thoracic kyphosis (TK) was higher. The cutoff values were 34.5° for TK, 0.5° for PI-LL, and 15.5° for PT. Other radiographic parameters were not significantly different. PJF developed in seven patients (17.5%) in the PJK group. PJF patients had significantly older age, higher postoperative TK, higher postoperative proximal junctional Cobb angle (PJA), more changes between pre- and postoperative PJA, and lower satisfaction scores on the Scoliosis Research Society Outcomes Questionnaire (SRS-22 satisfaction) than non-PJF patients in the PJK group.
Conclusions
One risk factor for PJK was lower postoperative PI-LL that was 0° or less. In ASD surgery, the most critical factor in a PJK prevention strategy is to obtain a postoperative LL adjusted by PI, which is >0°.
Keywords: adult spinal deformity, proximal junctional kyphosis, spinopelvic parameters, prevention strategy
Introduction
Thoracic and lumbar kyphosis and/or scoliosis are adult spinal deformities (ASD) that presented with abnormal posture, and intermittent claudication for back and leg pain leading to worsening quality of life (QOL). ASD patients receive conservative treatment at first; however, for those patients who experience QOL decline, surgical treatment is an option1).
On the other hand, ASD surgery is associated with many complications and the need for re-operations. Proximal Junctional Kyphosis (PJK) occurs at a high rate of 20% to 40% in ASD surgery and may require re-operation. Re-operation because of PJK is called proximal junctional failure (PJF), which causes serious problems, such as implant protrusion and paralysis, with a worse clinical course2,3).
In recent years, progress in surgical techniques, such as a three-column osteotomy (e.g., pedicle subtraction osteotomy or vertebral column resection) and Lateral Interbody Fusion (LIF), have led to better corrective results4,5). Still, the incidence of PJK has not improved. There are various causes of PJK, and different PJK/PJF prevention strategies, but these strategies are ineffective2,3,6). Previous reports have shown positive outcomes of ASD surgery7,8), but there are no PJK prevention guidelines. This study aimed to investigate the differences in the backgrounds of patients with PJK compared to those without PJK.
Materials and Methods
We retrospectively reviewed a database from April 2012 to March 2018 from a single institution. We included ASD patients with the following criteria: 1) aged more than 50 years at the time of surgery, 2) pelvic incidence minus lumbar lordosis (PI-LL) >10°, 3) sagittal vertical axis (SVA) >4 cm, 4) pelvic tilt (PT) >20°, 5) upper instrumented vertebra (UIV) above T10, 6) S2 alar iliac screws placed distal to the sacropelvic fixation, and 7) follow-up for at least two years. Exclusion criteria were infection, tumor, and cases that did not require spinal deformity correction. One hundred eight patients who had undergone reconstruction surgery were screened and 86 (79.6%) were finally enrolled. Through the last follow-up, we defined 40 patients (46.5%) with PJK and 46 patients without PJK through.
Patient demographics were collected, including age, sex, young adult mean of the femoral neck, operative time, operative blood loss, surgical methods with or without LIF, and fusion level (upper thoracic or lower thoracic). Clinical outcomes were assessed with the Oswestry Disability Index (ODI) and satisfaction score of the Scoliosis Research Society Outcomes Questionnaire (SRS-22 satisfaction) two years postoperatively.
Radiographic parameters, including coronal Cobb angle, thoracic kyphosis (TK), lumbar lordosis (LL), PI-LL, PT, and SVA pre- and postoperatively, and at the final follow-up, were measured.
PJK is a proximal junctional Cobb angle (PJA) ≧10° and PJA at least 10° higher than the preoperative measurement9). PJK was evaluated from standing X-ray films immediately after surgery, one year postoperatively, and during the last follow-up. PJF is the requirement for a re-operation in a PJK patient.
Statistical analysis was performed using SPSS software (IBM SPSS Inc, Version 26.0; Armonk, NY: IBM Corp). The p-values were based on Student's t-tests or Mann-Whitney tests, depending upon the normal distribution of data. The p-values < 0.05 were considered significant.
Results
We analyzed patient demographics analyzed for each group, as shown in Table 1. Demographic data were not significantly different between groups. PJK occurred immediately after surgery in 27 of 40 patients (67.5%). PJK was observed in 36 patients (90.0%) one year postoperatively, and 40 patients (100%) by the final follow-up.
Table 1.
Patient Demographics of PJK and Non-PJK Groups.
| PJK (+) | PJK (−) | p-value | |
|---|---|---|---|
| Sex (M:F) | 4:36 | 3:43 | 0.860 |
| Age (year) | 67.1±7.5 | 67.9±7.4 | 0.680 |
| Follow-up (month) | 50.4±18.2 | 53.4±17.5 | 0.394 |
| Young adult mean (%) | 73.0±12.4 | 75.2±10.4 | 0.328 |
| Operative time (minute) | 589.9±150.1 | 634.8±185.6 | 0.337 |
| Operative blood loss (ml) | 1078.9±660.2 | 1227.3±793.6 | 0.489 |
| Surgical method (AP:P) | 32:8 | 34:12 | 0.508 |
| Fusion level (UT:LT) | 13:27 | 20:26 | 0.299 |
Values are mean (±standard division). PJK: proximal junctional kyphosis, AP: anterior-posterior surgery, P: posterior surgery, UT: upper thoracic, LT: lower thoracic
Table 2 presents the preoperative, postoperative, and final follow-up radiographic parameters for each group. There were no differences between groups for preoperative radiographic parameters.
Table 2.
Radiographic Parameters of PJK and Non-PJK Groups.
| PJK (+) | PJK (−) | p-value | |
|---|---|---|---|
| Preoperative | |||
| Cobb angle (°) | 49.9±13.5 | 49.3±12.9 | 0.682 |
| TK (°) | 20.6±19.4 | 15.7±16.0 | 0.443 |
| LL (°) | 6.3±24.3 | 7.8±19.6 | 0.762 |
| PI-LL (°) | 41.2±22.4 | 46.8±18.4 | 0.133 |
| PT (°) | 31.9±9.6 | 34.3±10.2 | 0.332 |
| SVA (cm) | 11.1±5.6 | 12.3±6.9 | 0.359 |
| Postoperative | |||
| Cobb angle (°) | 15.7±6.4 | 17.0±11.0 | 0.938 |
| TK (°) | 35.0±11.0 | 28.0±9.4 | 0.004* |
| LL (°) | 50.6±10.5 | 47.9±10.6 | 0.290 |
| PI-LL (°) | −2.5±11.2 | 5.7±11.2 | 0.002* |
| PT (°) | 17.0±8.5 | 21.2±7.5 | 0.020* |
| SVA (cm) | 3.2±2.4 | 3.0±3.9 | 0.260 |
| Changes | |||
| Cobb angle (°) | −34.2±10.0 | −32.3±11.0 | 0.548 |
| TK (°) | 14.7±18.7 | 12.3±13.1 | 0.248 |
| LL (°) | 44.3±21.7 | 40.2±16.6 | 0.307 |
| PI-LL (°) | −43.7±20.5 | −41.1±16.1 | 0.579 |
| PT (°) | −15.0±7.2 | −12.0±14.3 | 0.356 |
| SVA (cm) | −8.0±4.4 | −7.5±12.2 | 0.581 |
| Final follow up | |||
| Cobb angle (°) | 15.4±6.9 | 15.8±9.3 | 0.960 |
| TK (°) | 42.7±14.3 | 30.5±9.4 | 0.001* |
| LL (°) | 45.1±12.4 | 45.3±9.7 | 0.958 |
| PI-LL (°) | 2.8±12.8 | 8.3±12.4 | 0.038* |
| PT (°) | 22.1±8.0 | 24.3±9.7 | 0.296 |
| SVA (cm) | 4.7±3.8 | 3.8±4.8 | 0.136 |
Values are mean (±standard division). * indicates a significant difference between groups. PJK: proximal junctional kyphosis, °: degree, TK: thoracic kyphosis, LL: lumbar lordosis, PI: pelvic incidence, PT: pelvic tilt, SVA: sagittal vertical axis
Postoperatively, TK was significantly higher in the PJK group (35.0° vs. 28.0°, p=0.004), PI-LL was significantly lower in the PJK group (−2.5° vs. 5.7°, p=0.002), and PT was significantly lower (17.0° vs. 21.2°, p=0.020) in the PJK group. Other postoperative radiographic parameters were not significantly different. Receiver operating characteristic (ROC) curves obtained postoperatively (Fig. 1) were used to determine cutoff values for TK (34.5°), PI-LL (0.5°), and PT (15.5°). The area under the ROC curve (AUC) of PI-LL (0.697) was larger than for TK (0.678) and PT (0.646).
Figure 1.
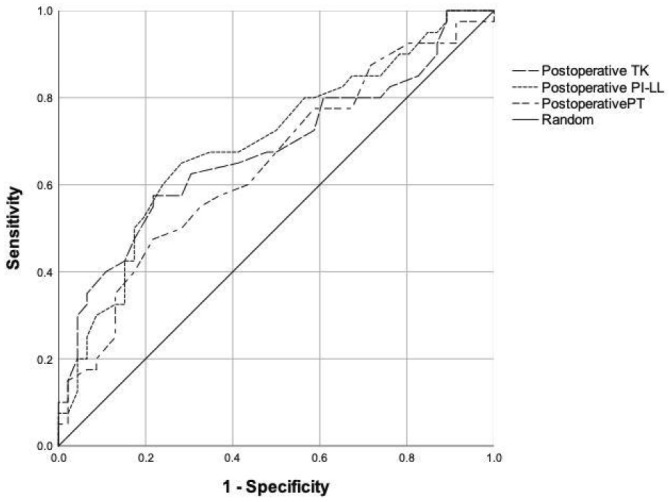
Figure 1 shows the ROC curves for postoperative PI-LL, TK, and PT. The cutoff values for TK (34.5°), PI-LL (0.5°), and PT (15.5°) were determined by the largest angle of “sensitivity - (1 - specificity) ”. The AUC of PI-LL (0.697±0.057) was larger than for TK (0.678±0.059) and PT (0.646±0.060).
The changes between pre- and postoperative radiographic parameters were not significantly different within the groups.
At the last follow-up, TK was significantly higher (42.7° vs. 30.5°, p=0.001), and PI-LL (2.8° vs. 8.3°, p=0.038) was significantly lower, in the PJK group. Other parameters were not significantly different (Fig. 2, 3).
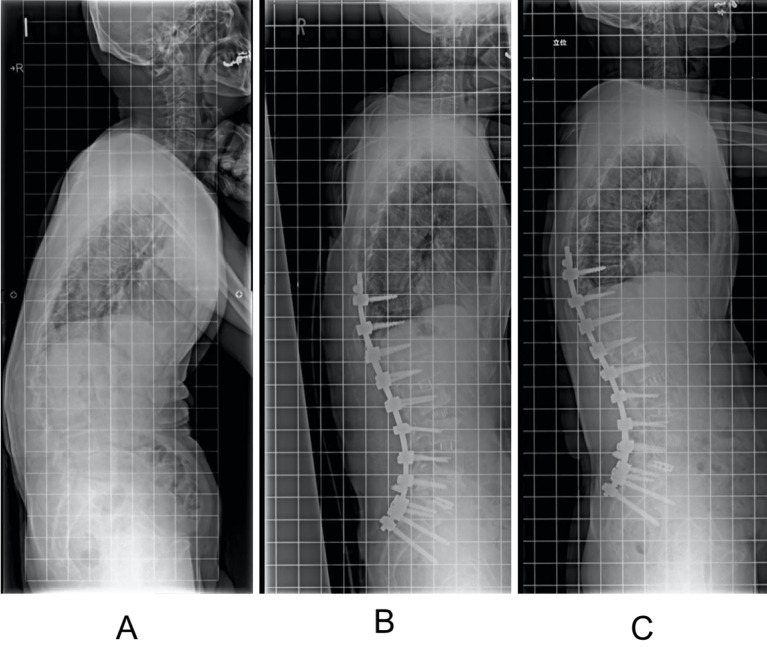
Figure 2.
A 62-year-old man presented with ASD (PJK group). (A) Preoperative X-rays revealed severe spinopelvic imbalance with PI-LL=40°, PT=31°, and SVA=14.2 cm. (B) Although spinopelvic parameters had been corrected to PI-LL of −9°, PT of 17° and SVA=2.4 cm 2 weeks after surgery. PJK developed with PJA=17° and a postoperative increase of 12° after surgery. (C) At the most recent observation (4 years postoperatively), although there was no complaint, PJA had mildly progressed to 22°.
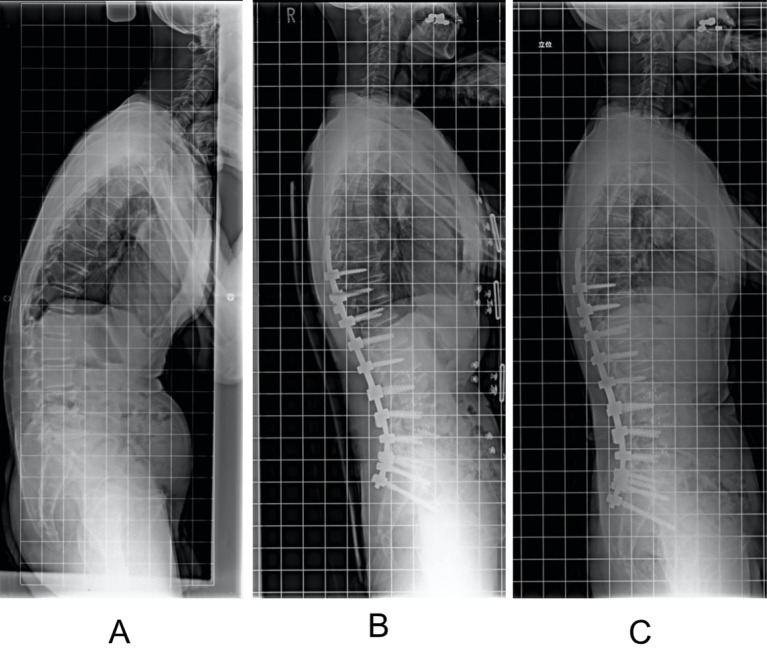
Figure 3.
A 74-year-old man presented with ASD (non-PJK group). (A) Preoperative X-rays revealed severe spinopelvic imbalance with PI-LL=48°, PT=33°, and SVA=17.6 cm. (B) Spinopelvic parameters had been corrected to PI-LL of 2°, PT of 26°, and SVA=−3.6 cm 2 weeks after surgery. PJA was 14° but increased postoperatively by 7°. (C) At the most recent observation (3 years postoperatively), PJA had increased only 3° compared with preoperative values.
ODI and SRS-22 satisfaction were used to evaluate clinical outcomes at the final follow-up. ODI (1.5±0.9 vs. 1.2±0.9, p=0.252) and SRS-22 satisfaction (3.7±0.5 vs. 3.7±0.7, p=0.403) were similar in both groups.
PJF developed in seven patients (17.5%) in the PJK group. One patient required hook removal and cutting of the rods. Six patients required upper thoracic spine extension caused by a burst fracture at the UIV. The UIV of all six patients who required extension was in the thoracolumbar region in the initial surgery. Table 3 presents patient demographics analyzed for PJF and non-PJF patients in the PJK group. PJF patients had a significantly older age (72.9 years vs. 65.9 years, p=0.016) than non-PJF patients in the PJK group. Table 4 presents preoperative, postoperative, and postoperative changes radiographic parameters analyzed for each group. PJF patients had significantly higher postoperative TK (44.0°vs. 33.1°, p=0.019), higher postoperative PJA (22.6°vs. 13.8°, p=0.004), and greater changes between pre- and postoperative PJA (19.7°vs. 11.0°, p=0.002) than non-PJF patients in the PJK group. Clinical outcomes at the final follow-up analyzed for each group. PJF patients had significantly lower SRS-22 satisfaction (2.9±0.3 vs. 3.8±0.7, p=0.018) than non-PJF patients in the PJK group. The ROC curves (Fig. 4) indicated cutoff values for age (70.5 years), postoperative TK (38.5°), postoperative PJA (15.5°), and postoperative PJA changes (14.5°). The AUC of postoperative PJA changes (0.870) was larger than for postoperative PJA (0.851), age (0.792), and postoperative TK (0.786).
Table 3.
Patient Demographics of PJF and Non-PJF Patients in the PJK Group.
| PJF (+) | PJF (−) | p-value | |
|---|---|---|---|
| Sex (M:F) | 1:6 | 3:30 | 0.459 |
| Age (year) | 72.9±3.6 | 65.9±7.5 | 0.016* |
| Follow-up (month) | 42.9±15.2 | 52.0±18.4 | 0.206 |
| Young adult mean (%) | 75.2±17.2 | 72.5±11.1 | 0.856 |
| Operative time (minute) | 529.4±116.0 | 602.7±153.3 | 0.463 |
| Operative blood loss (ml) | 817.3±542.8 | 1134.4±669.5 | 0.180 |
| Surgical method (AP:P) | 7:0 | 25:8 | 0.326 |
| Fusion level (UT:LT) | 1:6 | 12:21 | 0.382 |
Values are mean (±standard division). * indicates a significant difference between groups. PJF: proximal junctional failure, PJK: proximal junctional kyphosis, AP: anterior-posterior surgery, P: posterior surgery, UT: upper thoracic, LT: lower thoracic
Table 4.
Radiographic Parameters of PJF and Non-PJF Patients in the PJK Group.
| PJF (+) | PJF (−) | p-value | |
|---|---|---|---|
| Preoperative | |||
| Cobb angle (°) | 47.5±12.8 | 50.2±13.6 | 0.681 |
| TK (°) | 19.7±9.1 | 20.8±20.9 | 0.640 |
| LL (°) | −0.6±8.4 | 7.8±26.2 | 0.364 |
| PI-LL (°) | 39.0±6.9 | 41.7±24.5 | 0.789 |
| PT (°) | 31.3±9.2 | 32.1±9.7 | 0.783 |
| SVA (cm) | 9.6±2.7 | 11.4±6.0 | 0.498 |
| PJA (°) | 2.9±4.6 | 2.8±5.0 | 0.680 |
| Postoperative | |||
| Cobb angle (°) | 10.8±4.7 | 16.4±6.3 | 0.153 |
| TK (°) | 44.0±11.5 | 33.1±9.8 | 0.019* |
| LL (°) | 46.4±10.3 | 51.5±10.4 | 0.363 |
| PI-LL (°) | −5.3±12.6 | −1.8±10.8 | 0.569 |
| PT (°) | 16.7±7.5 | 17.1±8.7 | 0.831 |
| SVA (cm) | 2.8±2.3 | 3.3±2.4 | 0.735 |
| PJA (°) | 22.6±6.1 | 13.8±6.4 | 0.004* |
| Changes | |||
| Cobb angle (°) | −23.8±12.4 | −33.8±9.5 | 0.612 |
| TK (°) | 24.3±8.4 | 12.3±19.3 | 0.067 |
| LL (°) | 47.0±10.4 | 43.7±23.3 | 0.618 |
| PI-LL (°) | −44.3±10.6 | −43.5±22.0 | 0.972 |
| PT (°) | −14.6±8.0 | −15.1±7.0 | 0.769 |
| SVA (cm) | −6.8±3.3 | −8.2±4.6 | 0.510 |
| PJA (°) | 17.5±2.4 | 11.3±7.9 | 0.002* |
Values are mean (±standard division). * indicates a significant difference between groups. PJF: proximal junctional failure, PJK: proximal junctional kyphosis, °: degree, TK: thoracic kyphosis, LL: lumbar lordosis, PI: pelvic incidence, PT: pelvic tilt, SVA: sagittal vertical axis, PJA: proximal junctional angle
Figure 4.

Figure 4 shows the ROC curves for age, postoperative TK, postoperative PJA, and postoperative PJA changes. The cutoff values for age (70.5 years), postoperative TK (38.5°), postoperative PJA (15.5°), and postoperative PJA changes (14.5°) were determined by the largest angle of “sensitivity - (1 - specificity) ”. The AUC of postoperative PJA changes (0.870±0.058) was larger than for postoperative PJA (0.851±0.066), age (0.792±0.081), and postoperative TK (0.786±0.107).
Discussion
PJK is one of the most common complications of adult spinal deformity surgery, with an incidence of 20% to 40%; 13% to 66% of those require re-operation because of PJF2,3). PJF requiring re-operation may cause fracture or paralysis. Our results were similar to those reported by others. Both patient and operative factors account for this, but PJK is a multifactorial complication, and effective prevention strategies are unproven.
The major risk factors for PJK are older age, severe deformities, higher correction, anterior-posterior spinal fusion, and fusion to the sacrum2,3,6). Minor risk factors are low bone density, high BMI, and the presence of comorbidities2,3,6).
Our results indicated that lower postoperative PI-LL was the highest risk factor for PJK. To emphasize, the number of PJK patients with PI-LL≦0° increased postoperatively. These results indicate that it is important to obtain postoperative LL that matches the PI. It reduces the mechanical stress on the proximal junction and thus the risk of PJK. Of the seven patients with PJF, five patients had postoperative PI-LL≦0°. At one time, it was difficult to achieve a large LL for severe deformities through surgery. In recent years, a large LL could be obtained by three-column osteotomy and LIF, but excessive LL causes PJK as an overcorrection. Other PJK prevention strategies were to achieve a postoperative TK≦34.5°, and postoperative PT≧15.5°. However, TK was not included in the fixation area in the case with UIV in the lower thoracic spine, and PT could not be confirmed intraoperatively. LL could be confirmed intraoperatively. If the appropriate postoperative PI-LL was obtained, postoperative PT also had an appropriate value in many cases. It is important to obtain the postoperative LL adjusted by PI (the postoperative PI-LL) greater than 0°.
PJK occurred immediately after surgery in 27 of 40 patients (67.5%) and increased to 36 patients (90.0%) one year after the operation. Yagi et al. showed that 66% of PJK patients could be identified within three months after surgery10). Our results are consistent with this. The overload at the UIV level causes PJK earlier.
PJF was caused by a vertebral fracture and/or the posterior ligament complex at UIV level2,3). Patients with PJF may require re-operation because of pain, skin troubles, neurological deficits, or ambulatory difficulties2,3). The PJA was increased by 20° or more with PJF3). A standing X-ray in patients with PJF showed that PJA increased about 20° in the immediate postoperative period and then progressed to PJF. In our sample population, seven patients with PJF had significantly older age, higher postoperative TK, higher postoperative PJA, and greater changes in pre- and postoperative PJA than non-PJF patients in the PJK group. In addition to these, excessive correction of postoperative PI-LL≦0° may increase the risk of PJF. Of the seven patients with PJF, PI-LL was 0° or less in five patients and PI-LL was −10° or less in three patients. The UIV of six of the seven patients with PJF who required extension because of a burst fracture was in the lower thoracic spine in the initial surgery. Although there was no significant difference in the selection of the UIV, the risk of PJF was greater if postoperative TK was 38.5° or more. Therefore, extending the UIV to the upper thoracic spine to lower postoperative TK at the initial surgery is a desirable goal to prevent PJF.
In our results, ODI and SRS-22 satisfaction were similar in both groups. Because the PJK was evaluated radiographically, even if the PJK was positive, no symptoms were recognized. The correlation between QOL and radiographic parameters emphasizes the importance of global sagittal balance and spinopelvic parameters7). One of these parameters is the LL proportional to the PI, and the LL should be increased to PI±9. Our strict standard for PJK prevention was that the postoperative LL adjusted by PI should be greater than 0°. PJF patients in the PJK group had significantly lower SRS-22 satisfaction so it is important not to create PJK in order not to cause PJF secondary to PJK, especially in cases with 70 years old or older.
Preoperative planning and intraoperative evaluation are necessary to obtain the ideal postoperative PI-LL as a preventive strategy for PJK and PJF. Preoperative full spine X-rays in the prone position and fulcrum backward bending are useful to evaluate the required correction angle. If two-stage surgery is possible, further evaluation can be made after the first operation. In some cases, it is possible to change the surgical plan to extend the fixation level to prevent the PJK and PJF before the second operation. The use of an intraoperative computer-assisted device is effective in preventing under- or overcorrection and can reduce the operative time. Intraoperative X-rays are most important to determine whether the ideal postoperative PI-LL has been obtained.
There are some limitations of this study. First, this is a retrospective study with small sample size. Other factors may be identified as the number of cases increases. Second, there may be other risk factors than those investigated here. Further prospective studies are needed to validate our results.
Conclusion
Our results showed that 40 of 86 patients (46.5%) who underwent ASD surgery had PJK. Of those 40, 27 patients (67.5%) had PJK immediately after surgery, and 36 patients (90.0%) had PJK within one year postoperatively. PJF required re-operation in 7 of 40 patients (17.5%). The risk factors for PJK were higher postoperative TK and lower postoperative PI-LL and PT. In ASD surgery, the most important factor for a PJK prevention strategy was to maintain a postoperative PI-LL >0°.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Ethical Approval: No. 2020007, Institutional review board of Seirei Sakura Citizen Hospital.
Author Contributions: Tsuyoshi Sakuma wrote and prepared the manuscript, and all of the authors participated in the study design. All authors have read, reviewed, and approved the article.
Informed Consent: Informed consent was obtained by all participants in this study.
References
- 1.Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30(18):2024-9. [DOI] [PubMed] [Google Scholar]
- 2.Lau D, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine. 2014;39(25):2093-102. [DOI] [PubMed] [Google Scholar]
- 3.Scheer JK, Fakurnejad S, Lau D, et al. Results of the 2014 SRS survey on PJK/PJF: a report on variation of select SRS member practice patterns, treatment indications, and opinions on classification development. Spine. 2015;40(11):829-40. [DOI] [PubMed] [Google Scholar]
- 4.Kim YJ, Bridwell KH, Lenke LG, et al. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine. 2007;32(20):2189-97. [DOI] [PubMed] [Google Scholar]
- 5.Park HY, Ha KY, Kim YH, et al. Minimally invasive lateral lumbar interbody fusion for adult spinal deformity: clinical and radiological efficacy with minimum two years follow-up. Spine. 2018;43(14):E813-21. [DOI] [PubMed] [Google Scholar]
- 6.Kim HJ, Lenke LG, Shaffrey CI, et al. Proximal junctional kyphosis as a distinct form of adjacent pathology after spinal deformity surgery: a systematic review. Spine. 2012;37(22):S144-64. [DOI] [PubMed] [Google Scholar]
- 7.Schwab F, Patel A, Ungar B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine. 2010;35(25):2224-31. [DOI] [PubMed] [Google Scholar]
- 8.Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine. 2012;37(12):1077-82. [DOI] [PubMed] [Google Scholar]
- 9.Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcome, and risk factor analysis. Spine. 2005;30(14):1643-9. [DOI] [PubMed] [Google Scholar]
- 10.Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine. 2011;36(1):E60-8. [DOI] [PubMed] [Google Scholar]