To the Editor,
We read with great interest the excellent paper by Zarifian et al. entitled: “Chest CT findings of coronavirus disease 2019 (COVID-19): A comprehensive meta-analysis of 9907 confirmed patients” published in Clinical Imaging on February 2021.1 In this article, the authors provided comprehensive and useful research on the typical and atypical chest computed tomography (CT) findings of novel coronavirus disease (COVID-19) pneumonia. In addition to the findings described in the article, we would like to contribute to the article on an important issue.
Although radiological imaging findings are not used as a criterion in the diagnosis of COVID-19, thoracic imaging methods have been used as useful examinations in practice. In critically ill patients who are suspected of worsening and causing complications, CT is frequently utilized. The literature has previously identified the most common CT findings of COVID-19 pneumonia, such as multifocal and bilateral ground-glass opacities (GGOs) and/or consolidation in the peripheral, posterior, and lower lung lobes.2 , 3 Pleural thickening, nodules, pleural effusion, lymphadenopathy, cavitation and pneumothorax were identified as atypical findings of COVID-19 pneumonia.1
Recently, we observed an increase in the incidence of cavitary lung lesions during COVID-19 pandemia in our hospital which operates as a pandemic hospital in the region. Cavitary lung lesions detected in COVID-19 cases have started to emerge as only a few case reports in the literature.4 We would like to draw attention to this issue by reporting one of our COVID-19 patients with cavitary lung lesions. The most common causes among our COVID-19 patients with cavitary lung lesions were secondary bacterial infections, mainly caused by Staphylococcus aureus. A few case reports in the literature also support our clinical experience.5 , 6
We hypothesize that the SARS-CoV-2, like the influenza virus, weakens the lung's usual defense mechanisms, allowing bacteria to settle and reproduce.7 According to our clinical observation, this is most relevant for older people, those with compromised immune systems, and patients with a long hospitalization history due to increased risk of nosocomial infection. Besides, we suggest that microvascular thrombus formation, which is detected as one of the findings of lung autopsy in COVID-19 patients, may also be effective in cavity formation.8 However, the etiology, clinical correlation, and prognostic importance of cavitary lesions in COVID-19 pneumonia require further evaluation.
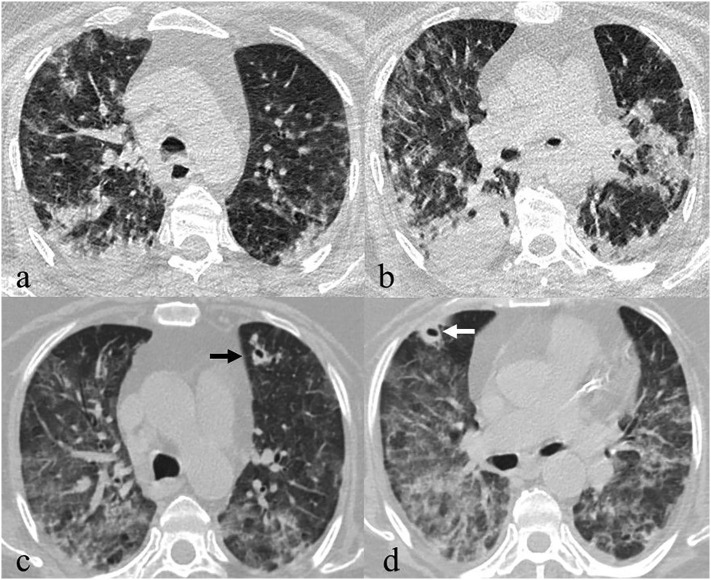
Fig. 1 demonstrates thoracic CT images of a 63-year-old male patient with cavitary lung lesions that developed after COVID-19 pneumonia. S. aureus growth was detected in the cultures taken from bronchoalveolar lavage. The patient was treated with meropenem and vancomycin for 21 days and discharged with full recovery.
Fig. 1.
63-Year-old male patient diagnosed with COVID-19 pneumonia. Axial images of non-contrast-enhanced CT obtained at the time of diagnosis show bilateral parenchymal infiltrations in the form of consolidation and ground-glass opacity, predominantly at the lower lobes and peripherally distributed (a, b). Axial images passing through the same level of non-contrast-enhanced CT obtained 10 days after the initial CT demonstrate newly formed cavitary nodules in the apicoposterior segment of the left upper lobe of the lung (black arrow) and the medial segment of the middle lobe of the right lung (white arrow) (c, d).
In conclusion, in line with our experience and case reports in the literature, newly developing cavitary lesions can be seen in patients with COVID-19 pneumonia. The secondary bacterial infection should be considered in the first place among all different causes in etiology. Thoracic CT in patients with a suspected complication is useful in the detection of cavitary lesions and patient management. Microbiological tests required for definitive diagnosis should be applied without delay.
Declaration of competing interest
The authors declare that they have no conflict of interest.
References
- 1.Zarifian A., Nour M.G., Rezayat A.A., Oskooei R.R., Abbasi B., Sadeghi R. Chest CT findings of coronavirus disease 2019 (COVID-19): a comprehensive meta-analysis of 9907 confirmed patients. Clin Imaging. 2021;70:101–110. doi: 10.1016/j.clinimag.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jiang M., Chen P., Li T., et al. Chest CT imaging features and clinical outcome of coronavirus disease 2019 (COVID-19): a single-center case study in Ningbo, China. Clin Imaging. 2021;69:27–32. doi: 10.1016/j.clinimag.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gezer N.S., Ergan B., Barış M.M., et al. Covid-19 s: a new proposal for diagnosis and structured reporting of covid-19 on computed tomography imaging. Diagn Interv Radiol. 2020;26(4):315–322. doi: 10.5152/dir.2020.20351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Afrazi A., Garcia-Rodriguez S., Maloney J.D., Morgan C.T. Cavitary lung lesions and pneumothorax in a healthy patient with active coronavirus-19 (COVID-19) viral pneumonia. Interact Cardiovasc Thorac Surg. 2021;32(1):150–152. doi: 10.1093/icvts/ivaa238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ammar A., Drapé J., Revel M. Lung cavitation in COVID-19 pneumonia. Diagn Interv Imaging. 2021;102(2):117–118. doi: 10.1016/j.diii.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marchiori E., Nobre L.F., Hochhegger B., et al. Pulmonary infarctions as the cause of bilateral cavitations in a patient with COVID-19. Diagn Interv Radiol. 2020;(16 December) doi: 10.5152/dir.2020.20865. [Epub Ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morris D.E., Cleary D.W., Clarke S.C. Secondary bacterial infections associated with influenza pandemics. Front Microbiol. 2017;8(JUN):1–17. doi: 10.3389/fmicb.2017.01041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deshpande C. Thromboembolic findings in COVID-19 autopsies: pulmonary thrombosis or embolism? Ann Intern Med. 2020;(May 6) doi: 10.7326/M20-3255. M20-2003. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]