Abstract
The COVID-19 global pandemic has disrupted the routine provision of community mental health services, which is especially concerning given that emerging data suggest a rise in mental health concerns related to the COVID-19 crisis (Xiong et al., 2020). Thus, it seems imperative to provide trauma-informed services that are tailored to clients’ coping with the pandemic and can be effectively delivered via telehealth. The goals of these important services would be to mitigate current distress, help prevent the onset of long-term mental health problems, and facilitate client safety during a public health crisis. The present article provides an overview of adoption and telehealth implementation of the Skills for Psychological Recovery (SPR) secondary prevention program within a psychology training clinic. Initial clinical outcome data supported the program’s success in reducing mental health symptoms among individuals in psychological distress due to the COVID-19 crisis; however, the results were more striking for adults than for youths. The article concludes with recommendations for broader implementation and future directions for clinicians, supervisors, organizations, and researchers.
Keywords: COVID-19, skills for psychological recovery, disaster mental health
The novel coronavirus (i.e., COVID-19) has spread globally, leading to a staggering number of cases and death toll (World Health Organization [WHO], 2020). To combat the spread of COVID-19, WHO (2020) recommended that individuals shelter in their homes as much as possible. This recommendation resulted in major disruptions to individuals, businesses, and institutions. Many businesses abruptly ordered their employees to work from home, and businesses without work-from-home capabilities were often forced to either furlough or lay off employees, with 30.3 million individuals having experienced unemployment since the start of the crisis (U.S. Bureau of Labor Statistics, 2020). Viewed together, early research showed that fear of COVID-19, social distancing practices, grief due to COVID-19-related loss, and the economic fallout has led to a surge of mental health problems worldwide (Xiong et al., 2020).
Initial Impact of COVID-19 on Mental Health
Researchers have quickly mobilized to study the effects of COVID-19 on mental health, with much of the research to date focusing on the effects of (a) lockdowns and social distancing practices, (b) contracting COVID-19 and long-term effects, and (c) working in frontline healthcare settings. For example, Rossi et al. (2020) followed Italian individuals over a 3-week period during their national lockdown in the spring of 2020 and found that over a third of the sample was experiencing symptoms of posttraumatic stress. Furthermore, a systematic review of the effect of the pandemic on the general population found that across 19 studies relatively high rates of anxiety, depression, PTSD, psychological distress, and stress were evidenced (Xiong et al., 2020). Of note, the reviewers also identified factors consistently associated with psychological distress, including unemployment, student status, and news exposure. Researchers have also identified that the mental health of frontline care workers has been especially impacted (Yuan et al., 2020), with some research indicating that factors such as social support and availability of personal protective equipment can have a mitigating effect (Muller et al., 2020). A recent meta-analysis of 21 studies examined the mental health impact on those diagnosed with COVID-19, with pooled prevalences indicating that nearly half of infected individuals suffered from depression and anxiety, and nearly a third experienced sleep disturbances (Deng et al., 2020). Viewed together, it is clear that the COVID-19 pandemic has had a far-reaching effect on mental health to date that certainly warrants intervention. However, more work is needed to better understand the long-term mental health impacts of the COVID-19 crisis and to understand the best mental health practices for facing this crisis.
COVID-19 Crisis as a Training Opportunity
In addition to the impact of COVID-19 on individuals’ mental health, the pandemic also impacted health service psychology trainees’ ability to receive training in the standard provision of mental health services. Indeed, these trainees are expected to develop certain competencies as they progress and demonstrate readiness for the next phase of training (e.g., internship, postdoctoral residency) or for entry to practice (APA, 2015). For many internships and licensing boards, readiness involves both competency evaluations and completion of a certain number of direct contact hours with clients. However, the fairly abrupt movement to remote learning and provision of telepsychology services during the COVID-19 crisis presented unique challenges for clinical training and coursework, the delivery of services, and supervision (Bell et al., 2020, Hames et al., 2020). As such, it may have been more difficult for trainees to gain the client contact hours and type of training experiences as quickly as they might have expected prior to the COVID-19 crisis.
The crisis also presented a unique training opportunity for trainees to develop competencies in several areas, including telehealth, disaster mental health, and ethics (Desai et al., 2020). The APA Ethics Code (2017), for example, implores psychologists to be cognizant of their responsibilities to both society and to the specific communities in which they live (Principle B) (Chenneville & Schwartz-Mette, 2020). Recognizing the opportunity to meet client, community, and trainee needs, leadership at a psychology training clinic, the University of Missouri Psychological Services Clinc (hereafter referred to as “the clinic”), strove to provide trauma-informed mental health services that were informed by the available research, could be tailored to address client concerns specific to COVID-19, and could be delivered effectively via telehealth.
Selection of Skills for Psychological Recovery
There is no current gold-standard prevention or intervention program for ameliorating post-disaster acute distress or for the prevention of long-term negative sequelae of surviving a global pandemic (International Society for Traumatic Stress Studies [ISTSS], 2020). In fact, programs such as Psychological Debriefing (i.e., having the victim describe the event and his or her emotional response in detail soon after the event) are no longer recommended because they have been found to impair the natural recovery process (Goldmann and Galea, 2014, International Society for Traumatic Stress Studies., 2020). However, in a review of the disaster mental health literature, Newman et al. (2014) identified that psychological interventions after a disaster can indeed be beneficial. More generally, it is recommended that disaster-related prevention and intervention efforts focus on building social support, promoting calming practices, and reestablishing normal routines (Goldmann & Galea, 2014). Consistent with this, Psychological First Aid (PFA; Brymer et al., 2006) has become one of the most widely used post-disaster interventions (Goldmann & Galea, 2014).
PFA (Brymer et al., 2006) was developed in conjunction with the National Center for PTSD and the National Child Traumatic Stress Network (NCTSN) and is based on expert consensus and research on traumatic stress. Given the widespread use of PFA, the training clinic initially planned to deliver services using this model. However, consultation with the NCTSN revealed that there was also another option: Skills for Psychological Recovery (SPR; Berkowitz et al., 2010). Like PFA, SPR is evidence-informed, was developed in conjunction with the National Center for PTSD and the NCTSN, and can be delivered in flexible settings (including by phone or video) by both mental health professionals and those outside of the profession. However, SPR is intended to be delivered over multiple meetings whereas PFA is intended for a single meeting, which may not be sufficient or appropriate due to the ongoing nature of the COVID-19 pandemic. Furthermore, SPR covers more post-disaster skill building from cognitive-behavioral therapy (CBT) than PFA. Although the pandemic shares many characteristics with other disasters (e.g., earthquakes, tornadoes, terrorist attacks), the prolonged length of the pandemic would indicate that having more skills to draw from could be essential.
Ultimately, SPR was not developed to ameliorate preexisting or more serious ongoing mental health concerns, but rather to target the acute distress and possible poor long-term mental health outcomes related to experiencing a discrete disaster. Thus, it would not be appropriate for other nondisaster-related mental health concerns exacerbated by the COVID-19 crisis or a disaster such as chronic suicidal ideation. Although no prior research on the efficacy of SPR in treating acute distress and long-term mental health outcomes has been published to date, researchers have evaluated its use by practitioners. Two studies of practitioners in Australia who were trained in SPR after several natural disasters indicated that providers found SPR to be useful and that they continued to use it months after the disaster (Forbes et al., 2010, Wade et al., 2014).
The clinic leadership team decided that trainees could ultimately benefit the community most by providing SPR, especially given that many of the skills seemed very timely and that trainees had the time and resources to appropriately deliver the content in SPR. To that end, the present article provides an overview of clinical and research procedures and initial clinical outcomes for the clinic’s implementation of SPR. In addition, adaptations made to SPR in light of the unique circumstances of the COVID-19 pandemic (e.g., the duration) are also detailed. This paper also represents the first reporting of mental health outcomes for individuals who have participated in SPR.
Method
Procedures
For all interested potential clients, the clinic’s assistant director completed a semistructured eligibility screening for the SPR program that included questions regarding presenting concerns, history of mental health concerns and treatment, and suicidal ideation and self-harm. To be eligible for the program, potential clients had to have risk that was manageable on an outpatient basis and to report concerns that were deemed appropriate for SPR (e.g., worries about self or others getting COVID, feelings of social isolation due to stay-at-home orders and social distancing guidelines, and financial difficulties related to the COVID-19 crisis such as paying rent or losing a job). Potential clients seeking services for more chronic issues not directly pertaining to the COVID-19 crisis (e.g., chronic depression or anxiety, Borderline Personality Disorder, ongoing self-harm) were referred to more appropriate services (n = 2). After individuals initiated services, clinicians reported in their session notes information regarding treatment engagement (e.g., number of sessions, modules covered) and clinical outcomes. As part of the informed consent process at the clinic, clients agreed to have their treatment and chart data used for research purposes. The present evaluation of the SPR program is considered exempt by the Univerity of Missouri’s Institutional Review Board.
Participants
Recruitment and Eligibility Criteria
Standard SPR was developed for adults and youths who had experienced a wide-scale trauma or a natural disaster (e.g., earthquake, fire). In the case of the COVID-19 crisis, there was no single discrete event that any particular potential client may have endured. Thus, clinic leadership elected to cast a wide net and include anyone who was experiencing acute distress related to the crisis. The clinic disseminated information about SPR throughout the community, reaching out to local mental health practitioners, health providers, schools, and local media outlets, and the larger university community. In advertising the program, it was made clear that the program was not intended to treat more longstanding mental health concerns; therefore, some individuals may have self-screened out. To maximize access to services regardless of clients’ ability to pay, the clinic made SPR services available at no cost to clients. This allowance was possible with the support of existing and new county-funded service contracts and scholarship subsidies from the University of Missouri’s Department of Psychological Sciences. Finally, although the majority of services were provided to clients residing locally, the flexibility of telehealth and emergency easing of interstate practice regulations allowed the clinic to serve University of Missouri students and other clients who had been displaced due to the pandemic.
Participant Description
Between April and August 2020, a total of 58 individuals were screened and accepted into the clinic’s SPR program, with 2 not meeting inclusion criteria. Of these individuals, 36 (10 youths and 26 adults) had completed SPR services by the time of this writing, with the remaining cases in progress or on a waitlist for SPR. Clients who participated in SPR identified with the following racial/ethnic group memberships: White/Caucasian (58%), Black/African American (13%), Hispanic/Latinx (19%), Native American (3%), Asian (3%), and mixed race (3%). The racial/ethnic makeup of this client group was more diverse than the surrounding community, which is 81% White, 10% Black/African American, 3.5% Hispanic/Latinx, 0.5% Native American, 5% Asian, and 3% two or more races (United States Census Bureau, 2019). Participants ranged in age from 9 to 60 years (M = 27.13) old and were predominantly female (84%).
Measures
Treatment Engagement
Clinicians reported on the number of sessions a client completed, whether the client completed treatment, whether treatment termination was planned, and what the outcome was (i.e., discharge to community, referral to other services) in their session notes. Further, clinicians were also asked to report which modules were covered during the course of treatment.
Adult Mental Health Symptoms
Adult clients completed the Patient Health Questionnaire-9 (PHQ-9; Kroenke et al., 2001) and Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006) to evaluate symptoms of depression and anxiety at each session throughout treatment. The PHQ-9, a 9-item screening and diagnostic tool for depression, has well-documented reliability and validity (Beidas et al., 2015). The GAD-7 is a 7-item measure intended to assess for anxiety and can be used as both a screening and diagnostic tool (Spitzer et al., 2006). The GAD-7 has well-demonstrated internal consistency, test-retest reliability, and concurrent validity (Beidas et al., 2015). Both the PHQ-9 and GAD-7 are freely available to clinicians online (http://www.phqscreeners.com/).
Youth Mental Health Symptoms
As part of routine assessment of youth treatment progress and outcomes, caregivers completed the Youth Outcome Questionnaire (Y-OQ; Burlingame et al., 2004) and youths ages 12 (n = 6) and older completed the Youth Outcome Questionnaire-Self Report (Y-OQ-SR; Burlingame et al., 2004) at each session. The Y-OQ is a well-validated routine outcome monitoring measure that provides an index of overall mental health distress for youths (Dunn et al., 2005, Ridge et al., 2009). For the current evaluation, first-session and last-session Y-OQ and Y-OQ-SR scores for the youths who completed SPR were used. In particular, clinicians reported on (a) the total score, an index of a youth’s current total distress; and (b) the depression/anxiety subscale score, an index of a youth’s current experience of sadness and worries.
Treatment Delivery
Intended as a multi-session brief intervention, SPR typically lasts one to several sessions focusing on whichever of the five skills (i.e., Promoting Helpful Thinking, Building Problem-Solving Skills, Managing Reactions, Promoting Positive Activities, and Rebuilding Healthy Social Connections) are most relevant to the client. Further, SPR can be delivered flexibly, allowing treatment providers to tailor the intervention to the specific circumstances of a disaster or widescale trauma. Due to the nature of the pandemic and the flexibility of the model, the training clinic faced two initial choice points regarding treatment delivery. First, given the potential for contagion during the COVID-19 crisis, an SPR program development team made the decision to deliver all SPR services via telehealth. The second decision involved the number of sessions to be provided as part of the clinic’s standard “free to clients” SPR services. To balance the treatment’s focus on five skills with available funding, the SPR program development team set five sessions after the initial screening as the maximum a client could receive at no cost, which was approved by clinic leadership. This maximum was also intended to ensure that clinicians would have sufficiently frequent case openings so that potential clients would not have to wait for long periods of time for services. However, clinic leadership recognized that clients would sometimes need more than five sessions, even in this focused, brief treatment model, and so allowed occasional extensions to a sixth no-cost session. Following SPR, clients were discharged to the community or referred to further appropriate services within the clinic or in the community.
Clinician Training and Supervision
SPR sessions were provided by 16 doctoral student trainees who had completed at least 1 year in a Ph.D. program in clinical psychology and who had prior CBT training. As the clinic transitioned to telesupervision, supervisors continued to meet with trainees for weekly individual and group supervision. However, the content of supervision changed to include issues relevant to telehealth skills and SPR implementation (e.g., building rapport remotely). Trainees and supervisors alike required training in telepsychology and SPR. Regarding the former, trainees had all received training in the ethics of telepsychology through their advanced ethics coursework. To extend this training, trainees reread the Association (2013) Guidelines for the Practice of Telepsychology and attended at least one webinar on telepsychology. Supervisors also attended at least one (and frequently more) webinar or training relevant to telepsychology and telesupervision.
To prepare for delivering SPR, trainees read the treatment manual, or Field Guide, and completed interactive online SPR training through NCTSN’s website (https://learn.nctsn.org/enrol/index.php?id=535). The SPR online training and Field Guide are freely available online, which removed cost barriers for graduate student clinicians. Training in both telepsychology and SPR began in mid-March 2020, concurrent with the campus closure and onset of local stay-home orders, lasted for 2 weeks, and resulted in clinicians being able to offer SPR by April 1, 2020. Trainee clinicians had weekly individual and group telesupervision to discuss ongoing SPR cases. Supervisors provided guidance and feedback on potential material to cover and appropriateness of referrals for more intensive treatment either prior to, during, or after treatment. Further, scores on measures administered weekly throughout treatment (i.e., PHQ-9, GAD-7, Y-OQ) were used to help make such decisions.
Treatment Protocol and Procedures
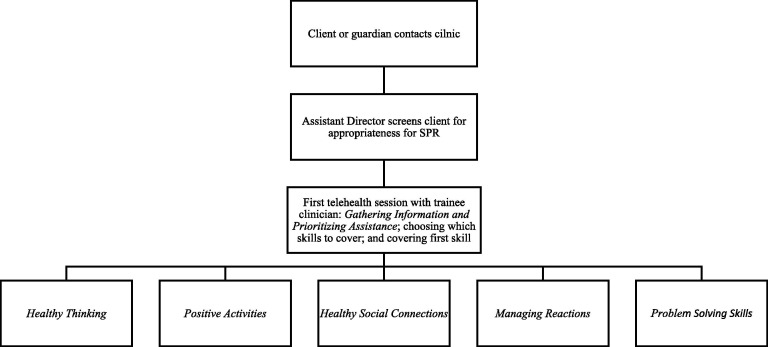
Standard clinical procedures for SPR are described in the Field Guide (Berkowitz et al., 2010), which is freely available online through the NCTSN (https://www.nctsn.org/sites/default/files/resources/special-resource/spr_complete_english.pdf). The flow of SPR services at the clinic is further illustrated in Figure 1 . Every individual receiving SPR completed an initial needs assessment (i.e., Gathering Information and Prioritizing Assistance), and covered up to five skill modules during the initial and subsequent sessions (i.e., Promoting Helpful Thinking, Building Problem Solving Skills, Managing Reactions, Promoting Positive Activities, and Rebuilding Healthy Social Connections). The SPR Field Guide contains worksheets for adults, youths, and caregivers completing SPR. Details regarding how treatment components were implemented and adapted to COVID-19 concerns are described in more detail below.
Figure 1.
Flow of Assessment and Skills for Psychological Recovery at the University of Missouri’s Psychological Services Clinic.
Gathering Information and Prioritizing Assistance
The first phase of SPR was dedicated to assessing the client’s current needs (e.g., medical, physical, psychological). The purpose of this initial, brief assessment was to determine the ultimate appropriateness of SPR and whether facilitating access to other providers was more appropriate. For example, a client might have stated that their presenting concern was anxiety related to their health regarding COVID. A clinician may have then discovered that this client was experiencing anxiety about having potentially contracted COVID due to interacting with a COVID-positive individual and now displayed a cough and fever. In cases like this, the clinician shifted to helping the client access appropriate medical testing and care. However, if the client had this anxiety without the medical symptomatic concerns, then the client and clinician moved on to selecting which skills modules they felt best met current needs. At this stage, the clinician provided the client with details about the skills that could be covered and what types of problems those skills might fit best. Clinicians and clients collaboratively and flexibly decided whether all five skills would be covered or whether it would be better to cover fewer skills in more depth. The clinician and client also determined the order in which the skills would be covered. Then, the clinician introduced the first skill that fit with the client’s needs.
Promoting Helpful Thinking
It is typical for individuals who have lived through a disaster to have cognitive distortions about themselves and the world around them. As such, the Promoting Helpful Thinking module seeks to address these distortions by promoting more adaptive thought processes. Clinicians are instructed to review “Common Unhelpful Thoughts” with clients and teach them cognitive-behavioral strategies to come up with “Alternative Helpful Thoughts.” Pertaining to COVID-19, distortions often revolved around a thought such as, “I will definitely get the virus.” Helpful replacements for this distortion included thoughts such as, “If I continue to wear my mask and observe social distancing guidelines, I can reduce my risk of becoming sick.” As available information regarding the virus changed frequently over the first several months of the pandemic, the resulting lack of clarity contributed to uncertainty and anxiety. Thoughts related to not knowing what the future would hold, such as “I’ll never be able to return to school again,” were replaced with more helpful alternatives such as: “Even if school does not look the way it used to, I am still able to continue learning at home.” In these ways, clinicians encouraged clients to recognize and challenge maladaptive thoughts and, consequently, more effectively manage negative emotions related to the COVID-19 crisis.
Building Problem-Solving Skills
The Building Problem-Solving Skills module covers classical CBT-based problem solving, such that clients were taught to (1) define the problem, (2) set a goal, (3) brainstorm ideas, (4) choose a possible solution, and (5) try out the solution. Clients completing SPR through the clinic identified many different problems to work on, including employment seeking following job loss and managing COVID risk. Youths in particular also identified problems such as not being able to spend time with friends due to a local stay-at-home order. When choosing a possible solution, clients were asked to identify what barriers related to the pandemic or otherwise might impede their proposed solution. Clinicians therefore helped clients anticipate challenges (e.g., travel restrictions due the COVID-19), and prepare to more effectively address problems they had identified as causing stress in their daily lives.
Managing Reactions
The Managing Reactions module is perhaps the most wide-ranging module in the SPR Field Guide, such that the number of possible skills covered in this module exceeds those of the other modules. This variety is due, in part, to the number of possible emotional reactions that a client may experience due to a traumatic stressor. Skills covered in this module related to handling anger and irritability, sleep difficulties, depression, and substance use, and included approaches such as sleep hygiene and relaxation. For youths, caregivers were also provided information on how to respond to child acting-out behaviors. In typically delivered SPR, the Writing Exercise in this module resembles a trauma narrative where the client is asked to recount a singular traumatic event and also process the emotions and thoughts related to this event. For the COVID-19 crisis, clinicians presented this exercise as an ongoing journal prompt that clients could return to over time to continue reflecting on their experience of the developing pandemic.
Promoting Positive Activities
The Promoting Positive Activities module covers skills pertaining to engaging in activities intended to boost the client’s mood. Activities fall under four categories: indoor activities, outdoor activities, social activities, and rebuilding activities. This module required significant adaptation to the COVID-19 crisis to ensure that clients chose activities that elicited a positive mood while promoting appropriate social distancing. For example, one of the suggested social activities in the standard SPR Field Guide, “hanging out with friends,” could not likely be done safely in person. Thus, therapists helped clients identify ways they could spend time with their friends virtually, such as video chatting and playing online games together. The closure of many venues for socializing (e.g., restaurants, bars, gyms, etc.) also limited clients’ options. As an adaptation of SPR, clinicians also encouraged clients to engage in mastery activities to provide opportunities for clients to feel proud of themselves while participating in safe activities at home, such as drawing, home improvement projects, or playing an instrument. Furthermore, clinicians worked with clients to encourage engagement in outdoor activities that could be done while social distancing (e.g., going for walks).
Rebuilding Healthy Social Connections
For Rebuilding Healthy Social Connections, clients were asked to think about their current social circles, evaluate who might be available to provide support, learn skills to ask for support, and consider how they might best support others. Similar to Promoting Positive Activities, adaptations for this module often pertained to implementing coping skills in ways consistent with social distancing that was part of local mandates or personal efforts to prevent the spread of COVID-19. In particular, clients and clinicians had to problem-solve around getting and giving support virtually, such as planning online celebrations for important milestones and scheduling times to meet with friends when all would have access to a reliable internet connection.
Attention to Issues of Diversity and Racism
The sample was diverse in terms of reported client backgrounds and identities. Notably, some of these clients identified issues regarding racism related to the pandemic (e.g., xenophobia) or unique challenges related to their background (e.g., difficulties with visas expiring). In addition, SPR was being provided during what APA (2020b) has coined the “racism pandemic,” in which multiple instances of police brutality and racial injustice towards Black individuals have merited significant national attention. The SPR Field Guide stresses the importance of cultural sensitivity in appropriate delivery of the treatment for clients of various backgrounds. Indeed, the manual emphasizes that the principles and techniques of SPR meet culturally informed standards. The manual also provides multiple “Culture Alert” prompts to guide clinician decision-making when working with different cultural groups. For example, in the Building Problem Solving Skills module, the “Culture Alert” suggests that the clinician consider the role of collective decision making in potentially choosing a solution to a client’s problem. Further, for Promoting Positive Activities, the “Culture Alert” reminds clinicians that in some cultures it may be disrespectful for the client to engage in pleasurable activities soon after a traumatic event. Given that SPR is designed to be tailored to meet individual client’s needs, it is the provider’s responsibility to both sufficiently assess the effects of the heightened attention to ongoing racial injustice on client’s functioning and adapt how they teach SPR skills. For example, in the Promoting Helpful Thinking module, a Black client may identify the following negative thought: “law enforcement will always judge me based on my skin color.” Although it is important that this thought not be treated as factually untrue or unrealistic, the clinician can work with the client to develop more helpful thoughts, such as “Although the police may be biased against people who look like me, their judgment is not a reflection of my character.” Clinic clinicians’ culturally informed clinical training served as a useful foundation for being able to incorporate these values into their work with SPR clients.
Analytic Strategy
Descriptive statistics (i.e., means, standard deviations, percentages) were calculated in SPSS to describe pre- and posttreatment scores on measures and changes on outcomes. Furthermore, paired samples t-tests were conducted in IBM SPSS Statistics (Version 27) on the clinical outcomes for adults to evaluate changes from pre to posttreatment. The same analyses were not conducted for the youth outcomes due to only nine youths having completed treatment.
Results
Treatment Engagement for Adults
Of the 26 adults who completed SPR treatment, 21 (81%) completed their intended number of sessions. Over half (58%) of clients completed five intervention sessions (M = 4.15 sessions). Two clients were approved for a sixth SPR session. After completing SPR, clients were discharged to the community (78%), referred within the clinic for further services (13%), or referred to an outside provider (9%).
Session notes documented which modules clients completed. All 26 adult clients covered the introductory Gathering Information and Prioritizing Assistance module. Because clients and clinicians determined whether and which skills would be covered in depth, there was variability in the number of skills covered and the frequency with which they were covered. Twenty-five clients covered skills beyond the introductory module (M = 2.84 skills covered, SD = 1.18). The most frequently addressed skills included Promoting Helpful Thinking (covered by 80% of adult clients), followed by Building Problem Solving Skills (60%), Managing Reactions (60%), Promoting Positive Activities (48%), and Rebuilding Healthy Social Connections (36%). Only one client chose to cover all five skills.
Clinical Outcomes for Adults
PHQ-9 scores indicated that clients’ self-reported symptoms of depression were in the moderately depressed range at pretreatment (M = 11.83, SD = 6.60), but the minimally depressed range at posttreatment (M = 4.91, SD = 3.83). As an indicator of clinical change, clients’ self-reported anxiety symptoms on the GAD-7 moved from the moderate anxiety range at pretreatment (M = 11.74, SD = 4.44) to the mild anxiety range at posttreatment (M = 4.68, SD = 4.24). At posttreatment, 81% and 71% of adult clients moved down at least one severity level (e.g., from moderate to mild) of depression and anxiety, respectively.
A paired samples t-test was conducted to evaluate the differences between pre- and posttreatment scores on the PHQ-9 and GAD-7 for the 21 individuals who completed treatment. The t-test for the PHQ-9 was statistically significant (t [20] = 5.35, p < .001), with an effect size of Cohen’s d = 1.17 (95% CI = 0.60–1.72). The difference in pre- and posttreatment means for the GAD-7 was also statistically significant, t (20) = 5.94, p < .001. The effect size for this difference was Cohen’s d = 1.30 (95% CI = 0.70–1.87).
Treatment Engagement for Youths
Of the 10 youths who have completed treatment to date, 9 (90%) had planned terminations. Fifty percent of all youths completed the five offered sessions, with 40% completing fewer than five. One youth was approved to have an additional sixth session. Youths who completed SPR were either discharged to the community (80%) or referred to other providers in the community (20%). For all youth clients, a caregiver attended at least a portion of each session. Every youth and clinician covered the Gathering Information and Prioritizing Assistance module. Youth covered an average of 3.60 skills (SD = 1.51), with three youths covering all 5 skills. Skills were covered with the following frequency: Promoting Helpful Thinking (90%), Managing Reactions (80%), Promoting Positive Activities (80%), Building Problem Solving Skills (70%), and Rebuilding Healthy Social Connections (40%).
Clinical Outcomes for Youths
At first session, youths’ Y-OQ and Y-OQ-SR mean total scores fell below the clinical severity cutoff of 29 for parent report and 30 for self-report and were consistent with community normative scores (Y-OQ: M = 28.44, SD = 7.68; Y-OQ-SR: M = 26.17, SD = 11.82). Of note, 44% of youths were above the clinical cutoff at baseline. Both caregiver and youth report scores were lower at last session (Y-OQ: M = 23.44, SD = 11.82; Y-OQ-SR: M = 16.50, SD = 10.07), but neither change met nor exceeded the Reliable Change Index of 10 points or higher (Burlingame et al., 2004). However, only one youth was above the clinical cutoff per caregivers’ reports and none were above the clinical cutoff per youths’ reports at termination. The depression/anxiety subscale of the Y-OQ does not have a cutoff score or Reliable Change Index, but scores can range from 0 to 24, with higher scores indicating greater levels of internalizing symptoms. Both caregiver and youth report indicated a decrease from pre- (Y-OQ: M = 10.00, SD = 4.07; Y-OQ-SR: M = 14.00, SD = 5.15) to posttreatment (Y-OQ: M = 8.38, SD = 3.89; Y-OQ-SR: M = 8.80; SD = 5.97).
Discussion
Given the widespread mental health effects of the COVID-19 crisis (Deng et al., 2020), brief, flexibly delivered prevention programs that mitigate current distress while promoting long-term resilience may provide a unique opportunity to efficiently benefit our struggling communities while also allowing for a substantive training opportunity for rising clinicians. One such brief prevention program, SPR, represents a highly accessible option for practitioners, supervisors, and organizations looking to meet the mental health needs of their communities. To that end, the current article provided an overview and initial evaluation of the University of Missouri Psychological Services Clinic’s successful implemenation of SPR. For clinicians with a foundation in cognitive-behavioral interventions, implementing SPR was a feasible way to respond quickly to client needs during the COVID-19 pandemic. The results indicated that SPR clinicians and clients most often decided to cover fewer skills in more depth instead of broadly covering all five skills, with Promoting Helpful Thinking being the most frequently covered skill for both youth and adults. Futher, both adults and youths in the present study saw improvements in their mental health symptoms from pre- to posttreatment. However, improvement was more modest for youth clients than for adults, and only the results for adults indicated clinically significant change. Overall, these results provide useful information regarding whether and how SPR can be implemented in the face of a pandemic.
Implications for Providers, Supervisors, and Organizations
It is the intention of this article to help provide a useful framework for clinicians, supervisors, clinics, and organizations hoping to implement SPR as the COVID-19 pandemic continues to unfold. Therefore, there are several implications for clinical practice worth noting (see Table 1 for a list of condensed recommendations for organizations, supervisors, and clinicians). First, our client engagement data supported the feasibility of implementing SPR across both youths and adults. Interestingly, most participants tended to use the maximum number of sessions without necessarily covering all five available skills. This suggests that clients and clinicians prioritized more in-depth coverage of selected skills over the breadth of covering all five skills. Second, the skill the clients and clinicians chose to cover the least (i.e., Rebuilding Healthy Social Connections) pertained to social support. This could be due to overlap with other modules (e.g., Positive Activities, Problem Solving Skills) that were covered more frequently. It could also be the case that many participants were already receiving information on maintaining social support during the COVID-19 crisis due to the extensive coverage of this issue on news and social media outlets. Thus, it is important for clinicians providing SPR to attend to issues for which individuals are not already getting support and education. Finally, it is worth noting that some clients required referrals to more standard therapy after completing SPR. This would suggest that it is vital for providers to collaboratively work with clients to figure out an appropriate discharge plan and to be continuously assessing for the appropriateness of SPR. Given the unprecedented length and duration of the COVID-19 pandemic, and the emerging data on long-term impacts of the virus, it seems reasonable that some individuals will require more intensive services.
Table 1.
Recommendations for Providers, Supervisors, and Organizations Implementing COVID-19-Relevant Services
| Recommendations for Providers |
|
| Recommendations for Supervisors |
|
| Recommendations for Organizations |
|
There are also several noteworthy considerations for supervisors hoping to implement SPR with their supervisees. As noted, our clinic found it helpful for supervisors to have ongoing discussions with their supervisees regarding a client’s initial and ongoing appropriateness for the brief SPR model. Because there will be clients for whom more intensive services will be appropriate in lieu of SPR or for whom treatment needs will extend beyond SPR’s brief treatment model, supervisors should help trainees identify the factors that increase or decrease “fit” for SPR services and evaluate these factors throughout their contact with clients. Second, our experience suggests that supervision of SPR can facilitate trainees’ ability to implement flexible, individually tailored treatment. Adapting SPR modules to specific issues relevant to the client’s specific circumstances during COVID-19 (e.g., social distancing in the context of a high-contact job, balancing work with protection of an immune-compromised family member) was an integral part of our SPR implementation, and thus was an important focus of supervision. Beyond the direct benefit to the trainees’ current cases, however, SPR supervision can provide a framework for focusing on the more general process of deciding when and how to tailor interventions to specific clients. Third, the targeted and short-term nature of SPR provided our supervisors with an excellent opportunity to support their trainees’ active use of frequent progress monitoring to evaluate client response to SPR treatment. Given the short-term nature of SPR, weekly use of brief symptom/adjustment measures that are sensitive to rapid change would seem to be important in helping clinicians and supervisors evaluate the appropriateness and effectiveness of SPR for individual clients and to guide treatment adjustments. Fourth, supervisors are encouraged to help their supervisees to remain informed of the most recent literature relevant to their use of SPR. In the context of the current study, it was important to stay abreast of emerging literature on the effects of the pandemic on mental health, as well as on promising options for intervention and progress/outcomes monitoring. Together, these supervision foci—on identifying an appropriate intervention based on the available literature and client circumstances, tailoring the intervention to fit the client’s values and needs, and using routine outcomes monitoring to evaluate the intervention and client response—may facilitate important benefits to both client outcomes and supervisees’ development of competencies in evidence-based practice.
At a broader organizational level, it is important to note that the freely available interactive online training and Field Guide allowed for the quick training of clinicians in SPR. In fact, our telehealth SPR services were available to clients just 2 weeks after training began in March. It is possible that this timeline could have been even quicker if clinicians had had prior experience delivering telehealth and were not also managing the upheaval COVID-19 created across all aspects of their own lives, ranging from closure of campus and community functions, the need to pause or transition to remote work in all aspects of their research, teaching, coursework, and other training activities, and the impact on their personal lives. Professionals with greater experience or those involved in full-time clinical work may be able to move even more quickly to using SPR. Nevertheless, our clinic’s swift transition to offering an evidence-informed, remotely delivered, trauma-informed service to address acute mental health concerns related to COVID-19 provides an important demonstration of the feasibility of launching such a program.
Importantly, the University of Missouri Psychological Services Clinic’s COVID-relevant SPR services program serves as an example for other organizations and practitioners faced with responding to COVID-19 or a similar community need. The challenges, responses, and outcomes of our clinic’s service development and implementation suggest several considerations for future clinical work. First, advance preparation is a key facilitator of rapid response. Of course, it is not realistic to prepare for every possible scenario, particularly within the constraints of time and resource limitations that may leave little room to address possible futures after addressing current realities. However, to the extent that organizations or individual mental health providers can incorporate foundational or preparatory elements into their standard operating procedures, they may be better positioned to respond to novel and abrupt community needs. For example, our clinicians’ strong foundations in ethical and evidence-based practice, and in application of CBT principles and methods to a variety of presenting problems enabled them to translate these competencies to COVID-related stress and to novel telehealth service delivery methods. Our clinicians’ familiarity and comfort with regular and ongoing access to the current literature and training resources to guide their practice with new presenting problems or treatment methods similarly facilitated their ability to digest training materials quickly and efficiently.
Second, easy access to necessary training resources is critical. This was certainly the case for the clinic’s ability to pivot effectively to the new SPR approach as well as to telehealth service. Although some level of access may be incorporated into an organization’s standard resources (e.g., a clinic, campus, or personal library; regular grand rounds or staff training; continuing education subscriptions), other access requires a creative and opportunistic approach. For example, professional and educational organizations were extremely generous in sharing resources relevant to the COVID-19 crisis, from helping clients and providers cope with stressors to supporting providers’ effective use of telehealth. Many of our trainee clinicians and supervisors commented on the embarrassment of riches and resulting resource overload, but overall were grateful to have the guidance available. Having a way to help clinicians locate, organize, and prioritize the resources that will be most useful for their circumstances, and making sure they are able to access and absorb the information (e.g., with release time, stable internet connection for web-based training, and opportunities to consult or discuss the information), will greatly enhance providers’ effectiveness in designing and delivering context-responsive care.
Third, identifying individuals who could shift their duties to move resources to implementing SPR proved essential. Indeed, individuals at our clinic worked efficiently to identify which services we could feasibly implement via telehealth and were able to decide on the appropriateness of SPR. Then, these individuals were able to quickly organize resources and trainings for student clinicians, identify possible funds to make services free for clients (e.g., local COVID-19 related grants), and determined methods of disseminating information about SPR to the broader community. Ultimately, having this team of individuals proved vital to the swift implementation of SPR at our clinic. Thus, organizations may want to consider dedicating a rapid response team to implementing SPR or other intervention programs targeting COVID-related mental health concerns.
Finally, the importance of devoting resources to evaluation of both client progress/outcomes and the intervention program itself cannot be overstated. As noted in our introduction, despite the promise of SPR for our clinic’s ability to meet acute community needs for attention to the mental health challenges induced or exacerbated by the COVID-19 pandemic, this is, to our knowledge, the first published description and evaluation of client mental health outcomes using this treatment. Clinicians, supervisors, and clinics have the opportunity, and we would argue the responsibility, to contribute to the evidence base that supports interventions for acute and novel stressors like the pandemic. Developing and supporting the structures needed to help clinics identify and utilize client and program evaluation measures, and then to evaluate and disseminate their findings, will benefit not just the individual clients served, but the profession and public more broadly.
Limitations and Future Directions
Several limitations of the present article warrant comment. First, we were only able to report on limited client outcome data to date, which is a reflection of the recency of the pandemic and the mental health response to it. Future work is needed to collect more data and cross-agency collaboration could facilitate the compilation of larger datasets to allow for further examination of SPR and other COVID-related mental health services. Second, the improvements in youths’ mental health functioning reported on in the present article were not clinically reliable. This could be due to low levels of initial distress or insensitivity of the Y-OQ to the expected short-term changes from SPR. Third, SPR was not appropriate for some of the more severe mental health concerns that may have been triggered or exacerbated by COVID-19 (e.g., suicidality). It also may not be appropriate for addressing client distress and dysfunction as services shift from acute to more chronic stress and trauma. Thus, in future work, SPR may need to be implemented as part of a broader continuum of care. Finally, the measures chosen as part of the present study (i.e., PHQ-9, GAD-7, Y-OQ) may not be the optimal tools for assessing for COVID-19-related mental health symptoms. Future research evaluating SPR and other program outcomes could seek to use measures developed for the pandemic, such as NIH’s CRISIS.
Conclusions
In sum, the utilization of the National Child Traumatic Stress Network’s and National Center for PTSD’s Skills for Psychological Recovery program showed promise in the delivery of brief, free, and effective mental health services to members of our community during the unprecedented COVID-19 crisis. Given that the duration of the global pandemic remains unknown, it seems imperative to implement brief interventions that can be flexibly delivered outside of a clinic setting and by individuals across different experience levels (e.g., trainees) in order to mitigate the long-term mental health effects of the COVID-19 crisis. Even beyond the current health pandemic, lessons learned in this context are invaluable in future efforts to prepare professionals to be able to move rapidly and flexibly to provide evidence-informed, context-tailored care to meet unanticipated and novel community needs.
Footnotes
We have no known conflicts of interests and no funding sources to declare.
References
- American Psychological Association (2020). “We are Living in a Racism Pandemic,” Says APA President. https://www.apa.org/news/press/releases/2020/05/racism-pandemic.
- American Psychological Association (2015). Commission on Accreditation: Implementing Regulations. https://www.apa.org/ed/accreditation/section-c-soa.pdf.
- American Psychological Association (2013). Guidelines for the Practice of Telepsychology. https://www.apa.org/practice/guidelines/telepsychology.
- Beidas R.S., Stewart R.E., Walsh L., Lucas S., Downey M.M., Jackson K., Fernandez T., Mandell D.S. Free, brief, and validated: Standardized instruments for low-resource mental health settings. Cognitive and Behavioral Practice. 2015;22:5–19. doi: 10.1016/j.cbpra.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell, D. J., Self, M. M., Davis, III, Cl, Conway, F., Washburn, J. J., & Crepeau-Hobson (2020). Health service psychology education and training in the time of COVID-19: Challenges and opportunities. American Psychologist. Advance online publication. 10.1037/amp0000673. [DOI] [PubMed]
- Berkowitz, S., Bryant, R., Brymer, M., Hamblen, J., Jacobs, A., Layne, C., & Watson, P. (2010). Skills for psychological recovery: field operations guide. The National Center for PTSD & the National Child Traumatic Stress Network.
- Brymer M., Layne C., Jacobs A., Pynoos R., Ruzek J., Steinberg A., Vernberg E., Watson P. Psychological first aid field operations guide. National Child Traumatic Stress Network. 2006 [Google Scholar]
- Burlingame, G. M., Dunn, T., Hill, M., Cox, J., Wells, M. G., Lambert, M. J., & Brown, G. S. (2004). Administration and Scoring Manual for the YOQ-30.2 (Youth Outcome Questionnaire-30 Version 2.0).
- Chenneville T., Schwartz-Mette R. Ethical considerations for psychologists in the time of COVID-19. American Psychologist. 2020;75:644–654. doi: 10.1037/amp0000661. [DOI] [PubMed] [Google Scholar]
- Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Huang E., Zuo Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Annals of the New York Academy of Sciences. 2020:1–22. doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai A., Lankford C., Schwartz J. With crisis comes opportunity: Building ethical competencies in light of COVID-19. Ethics & Behavior. 2020;30:401–413. doi: 10.1080/10508422.2020.1762603. [DOI] [Google Scholar]
- Dunn T.W., Burlingame G.M., Walbridge M., Smith J., Crum M.J. Outcome assessment for children and adolescents: Psychometric validation of the Youth Outcome Questionnaire 30.1 (Y-OQ®-30.1) Clinical Psychology & Psychotherapy. 2005;12:388–401. doi: 10.1002/cpp.461. [DOI] [Google Scholar]
- Forbes D., Fletcher S., Wolfgang B., Varker T., Creamer M., Brymer M.J., Ruzek J.I., Watson P., Bryant R.A. Practitioner perceptions of Skills for Psychological Recovery: A training programme for health practitioners in the aftermath of the Victorian bushfires. Australian & New Zealand Journal of Psychiatry. 2010;44:1105–1111. doi: 10.3109/00048674.2010.513674. [DOI] [PubMed] [Google Scholar]
- Goldmann E., Galea S. Mental health consequences of disasters. Annual Review of Public Health. 2014;35:169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- Hames J.J., Bell D.J., Perez-Lima L.M., Holm-Denoma J.M., Rooney T., Charles N.E., Charles N.E., Thompson S.M., Mehlenbeck R.S., Tawfik S.H., Fondacaro K.M., Simmons K.T., Hoersting R.C. Navigating uncharted waters: Considerations for training clinics in the rapid transition to telepsychology and telesupervision during COVID-19. Journal of Psychotherapy Integration. 2020;30:348–365. doi: 10.1037/int0000224. [DOI] [Google Scholar]
- International Society for Traumatic Stress Studies (2020). Posttraumatic Stress Disorder Prevention and Treatment Guidelines: Method and Recommendations.
- Kroenke K., Spitzer R.L., Williams J.B. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller R.A.E., Stensland R.S.Ø., van de Velde R.S. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Research. 2020;293:113441. doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman E., Pfefferbaum B., Kirlic N., Tett R., Nelson S., Liles B. Meta-analytic review of psychological interventions for children survivors of natural and man-made disasters. Current Psychiatry Reports. 2014;16(9):462. doi: 10.1007/s11920-014-0462-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridge N.W., Warren J.S., Burlingame G.M., Wells M.G., Tumblin K.M. Reliability and validity of the youth outcome questionnaire self-report. Journal of Clinical Psychology. 2009;65:1115–1126. doi: 10.1002/jclp.20620. [DOI] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry. 2020;11:1–6. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau . Boone County; Missouri: 2019. Quick Facts. https://www.census.gov/quickfacts/fact/table/boonecountymissouri/PST045219. [Google Scholar]
- U.S. Bureau of Labor Statistics (2020). Labor force statistics from the current population survey. https://data.bls.gov/timeseries/LNS11000000.
- Wade D., Crompton D., Howard A., Stevens N., Metcalf O., Brymer M., Ruzek M., Watson P., Bryant R., Forbes D. Skills for Psychological Recovery: Evaluation of a post-disaster mental health training program. Disaster Health. 2014;2:138–145. doi: 10.1080/21665044.2015.1085625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020). Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- Xiong J., Lipsitz O., Nasri F., Lui L.M., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020 doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S., Liao Z., Huang H., Jiang B., Zhang X., Wang Y., Zhao M. Comparison of the indicators of psychological stress in the population of Hubei Province and non-endemic provinces in China during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 2020;26 doi: 10.12659/MSM.923767. e923767-1–e923767-10. https://dx.doi.org/10.12659%2FMSM.923767. [DOI] [PMC free article] [PubMed] [Google Scholar]