Abstract
The epithelial-to-mesenchymal transition (EMT) is a dynamic epigenetic reprogramming event that occurs in a subset of tumor cells and is an initiating step towards invasion and distant metastasis. The process is reversible and gives plasticity to cancer cells to survive under variable conditions, with the acquisition of cancer stem cell-like characteristics and features such as drug resistance. Therefore, understanding survival dependencies of cells along the phenotypic spectrum of EMT will provide better strategies to target the spatial and temporal heterogeneity of tumors and prevent their ability to bypass single inhibitor treatment strategies. To address this, we integrated the data from a selective drug screen in epithelial and mesenchymal Kras/p53 (KP) mutant lung tumor cells with separate datasets including reverse phase protein array and an in vivo shRNA dropout screen. These orthogonal approaches identified AXL and MEK as potential mesenchymal and epithelial cell survival dependencies, respectively. To capture the dynamicity of EMT, incorporation of a dual fluorescence EMT sensor system into murine KP lung cancer models enabled real time analysis of the epigenetic state of tumor cells and assessment of the efficacy of single agent or combination treatment with AXL and MEK inhibitors. Both 2-D and 3-D culture systems and in vivo models revealed that this combination treatment strategy of MEK plus AXL inhibition synergistically killed lung cancer cells by specifically targeting each phenotypic subpopulation. In conclusion, these results indicate that co-targeting the specific vulnerabilities of EMT subpopulations can prevent EMT-mediated drug resistance, effectively controlling tumor cell growth and metastasis.
Statement of Significance
This study shows that a novel combination of MEK and AXL inhibitors effectively bypasses EMT-mediated drug resistance in Kras/p53 mutant NSCLC by targeting EMT subpopulations, thereby preventing tumor cell survival.
Keywords: Epithelial-to-mesenchymal transition (EMT), Tumor heterogeneity, Non-small cell lung cancer, ZEB1, microRNA-200, MEK, AXL
Introduction
The epithelial-to-mesenchymal transition (EMT) is an evolutionarily conserved, dynamic epigenetic reprogramming event that is required for normal biological processes such as embryonic development, organogenesis, and response to tissue injury (1, 2). Cells can bidirectionally shift across a spectrum, transitioning between a differentiated epithelial state and a plastic, stem-like mesenchymal state with the ability to self-renew and become motile. While a normal developmental process, numerous studies have demonstrated the role of EMT in cancer progression, contributing to the phenotypic tumor heterogeneity observed within many solid tumors. In fact, EMT markers have been correlated with tumorigenicity and metastatic propensity across several tumor types (3-7), highlighting the importance of this complex process in driving tumor progression.
EMT is tightly regulated in normal cells but becomes dysregulated in tumors by upregulation of mesenchymal transcription factors like Zeb1 and Snail (8-10). This can occur via aberrant conditions within the tumor microenvironment (TME), such as hypoxia or inflammation, which promote secretion of and tumor response to exogenous factors like TGF-β (11, 12). In non-small cell lung cancer (NSCLC) in particular, the Zeb1/miR-200 double negative feedback loop is one such tightly regulated axis that can lead to EMT via upregulation of Zeb1 and concurrent downregulation of epithelial features, including the microRNA-200 family, E-cadherin and other epithelial differentiation genes (13-17). Upon EMT, cancer cells are more motile and invasive, and this process can initiate the metastatic cascade. Besides an increase in invasiveness and metastatic propensity, mesenchymal tumor cells also gain characteristics that promote aggressiveness, including stem cell-like features and drug resistance. Thus, to improve prevention and treatment strategies, it is critical to better understand the survival dependencies of cells along the epithelial-mesenchymal spectrum.
Previous work from our lab highlighted the dependency of epithelial KrasG12D;p53R172HΔG (KP) mutant tumor cells on the MAPK pathway (18). Despite possessing identical Kras mutations, mesenchymal tumor cells were intrinsically resistant to MEK inhibition and showed no response to single agent treatment. Additionally, epithelial tumors treated over the long term with the MEK inhibitor selumetinib displayed a robust initial response, but eventually acquired resistance. The escape of epithelial tumors from MEK inhibitor-mediated cell death occurred via Zeb1-induced EMT; thus, targeting a single survival dependency delayed tumor growth, but epigenetic reprogramming by EMT allowed for tumor cell survival. In fact, despite the prevalence of KRAS mutations in many cancer types, clinical trials with MEK inhibitor therapies have demonstrated poor responses (19-21), and this is likely due to de novo tumor heterogeneity and the emergence of resistant subpopulations.
To identify potential combinations for lung cancer treatment in an EMT-centric system, we performed a selective drug targeting screen using epithelial and mesenchymal KP murine lung cancer cells. We integrated these results with two additional datasets, including an in vivo shRNA dropout screen focused on FDA approved drug targets and reverse phase protein array (RPPA) on epithelial and mesenchymal tumor cells(18, 22). These analyses revealed that AXL and PARP are selectively mesenchymal tumor cell sensitivities, whereas AKT and MEK are epithelial cell sensitivities. In vitro experiments with multiple models demonstrated that combining the MEK inhibitor selumetinib with the AXL inhibitor bemcentinib is a synergistic combination; thus, we hypothesized that this co-targeting strategy will combat drug resistance due to EMT and lead to increased tumor cell death.
We pursued this combination by utilizing the Z-cad dual fluorescent reporter sensor, which allows dynamic monitoring of EMT (23). In a highly metastatic KP mutant murine cell line, we expressed the Z-cad reporter and analyzed the impact of single agent treatments on epithelial and mesenchymal subpopulations over time in 2-D and 3-D culture model systems. We determined that the MEK inhibitor effectively killed RFP+ epithelial cells, whereas AXL inhibitor effectively killed GFP+ mesenchymal cells. The combination treatment in vivo demonstrated significantly improved efficacy in suppressing tumor growth compared to either single agent alone, thus confirming that co-inhibition of MEK and AXL targets multiple phenotypic subpopulations within a heterogeneous tumor.
Materials and Methods
Cells lines and cell culture
All cell lines used are found in Supplement Table 1. All cells were cultured at 37°C in a humidified incubator at 5% CO2 and maintained in RPMI 1640 and 10% fetal bovine serum (Gibco). Human cell lines were purchased from ATCC and murine Kras/p53 lung cancer cell lines were derived as previously described (14). Mycoplasma negative cells were used for all experiments and testing was performed using LookOut Mycoplasma PCR Detection Kit (Sigma-Aldrich).
In vitro drug screen
393P or 344P cells were plated in 96-well plates. 24 hours after seeding, drugs listed in Supplement Table 2 were added at indicated concentrations (n=8). After 72 hours, MTT (3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl-2H-tetrazolium bromide) (Sigma-Aldrich) was added and incubated at 37°C for 1-2 hours. Media was aspirated and DMSO was added to formazan crystals. Absorbance was measured at 570/630 nm and viability was normalized against cells with solvent control. IC50 values were determined using nonlinear regression function in GraphPad Prism software and are in Supplement Table 3.
shRNA screen
The 393P and 344P murine cell lines were infected with a pooled shRNA lentiviral library targeting 192 genes. Infected cells were implanted into 129sv mice as previously described (18, 22), and the genes and RSA values are in Supplement Table 4.
In vivo tumor experiments
Animal studies were approved by the Institutional Animal Care and Use Committee at The University of Texas MD Anderson Cancer Center (approved protocols #1271 & #1191). 344SQ cells or 344SQ_Z-cad cells were implanted subcutaneously into the right flank of 129sv mice of 3-7 months of age, and A549 human cells were implanted into athymic nude male mice. After palpable tumor formation, mice were treated daily with selumetinib (Selleckchem) at 25 mg/kg, p.o. and/or bemcentinib (BerGenBio) at 100 mg/kg, p.o. Additional details are found in the supplementary methods.
Results
Identification of specific survival dependencies in epithelial and mesenchymal tumor cells
Due to the heterogeneity within tumors partly driven by epigenetic reprogramming events like EMT, it is imperative to target and kill tumor cells regardless of which state the cells are in at a given time. To broach this, we integrated the results from three different datasets to highlight targets worth pursuing as EMT-centric drug targets.
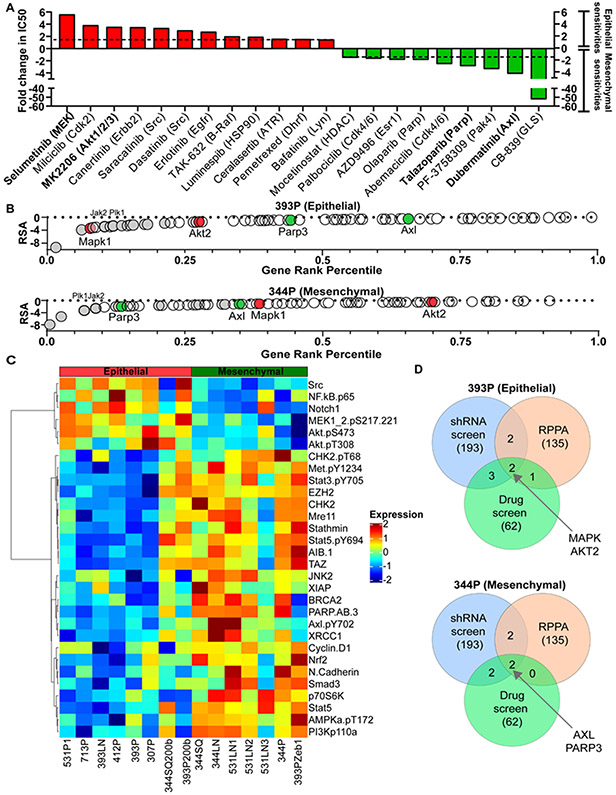
First, we performed a selective drug screen measuring cell growth of the 393P and 344P murine KP mutant lung cancer cells, which we previously described as being representative of epithelial and mesenchymal tumor cell subtypes, respectively(14) (Supplement Table 1). The screen utilized 62 compounds targeting common oncogenic pathways activated within tumor cells. The results of this screen revealed that some compounds kill equally well in both 393P and 344P cells, such as the Ras pathway inhibitor Rigosertib (Supplement Table 3). However, to identify those compounds targeting one epigenetic state or the other, we compared the fold change in IC50 for each compound between 393P and 344P cells. We implemented a cut-off in fold change value as 1.5 or greater and removed any compound with an IC50 in the sensitive cell line above 10 μM to reduce likely off-target effects. Using these criteria, we found 12 compounds that specifically targeted the epithelial 393P cells and 9 targeting the mesenchymal 344P cells (Fig 1A, Supplement Fig 1A-B, Supplement Table 3).
Figure 1. Identification of mesenchymal or epithelial cell sensitivities and selective drug targets.
(A) 393P epithelial and 344P mesenchymal cells were utilized for a selective drug screen measuring cell growth via MTT assay. The fold change in IC50 between 393P and 344P cells was calculated, and fold change values 1.5 or greater are depicted. 393P epithelial specific sensitivities are shown in red and 344P mesenchymal sensitivities are shown in green. (B) The FDAome shRNA dropout screen was performed previously in the 393P and 344P cells and tumors(18, 22). Of the ~200 total targets in the screen, only those which correspond to each drug screen target performed in A are depicted. The gene rank percentile of these hits was calculated and graphed as a function of the significance of the shRNA dropout score (redundant shRNA activity (RSA) value). Genes shown in gray are those which dropped out significantly in both 393P and 344P tumors. Mapk1 and Akt2 are depicted in red as epithelial drug screen hits, and Parp3 and Axl are depicted in green as mesenchymal drug screen hits. (C) Heatmap of RPPA profile showing statistically significant (p<0.05) differentially expressed proteins in epithelial or mesenchymal murine lung cancer cell lines. (D) Venn diagrams are shown depicting the overlap between shRNA screen, RPPA, and drug screen described in A-C. The number of hits that overlap between each respective screen are shown.
Secondly, we leveraged additional orthogonal datasets on the epithelial and mesenchymal tumor cells. We previously reported the results of a shRNA dropout screen with 393P and 344P cells to determine their survival dependencies (18, 22). Briefly, this screen included shRNAs targeting ~200 genes encoding for clinically actionable targets (termed the FDAome). FDAome-expressing cells were implanted in vivo with or without immune checkpoint blockade treatment (22), though for the purposes of this study, we focused on tumors without immune checkpoint blockade treatment. Deep sequencing for the barcoded shRNAs revealed genes necessary for cell survival, and genes were ranked upon the significance of shRNA dropout (RSA value). Because the drug screen focused on common oncogenic pathways, there was significant overlap with the FDAome screen. The RSA values from the in vivo FDAome screen for genes corresponding to the 64 drug screen targets are depicted against the overall gene rank across the entire library (Fig 1B, Supplement Table 4). We found that AXL or PARP knockdown caused dropout in the 344P mesenchymal tumors, whereas MAPK or AKT knockdown produced dropout in the 393P epithelial tumors. Thus, these in vivo data corroborate the results of the in vitro drug screen, with drug targeting of specific pathways demonstrating differential response in either cell line.
Finally, RPPA was completed on panels of human and murine epithelial and mesenchymal NSCLC cell lines to discover pathways that are differentially activated in each cell state (18). RPPA analyses revealed phospho-MEK and phospho-AKT to be more highly expressed in epithelial cells, whereas mesenchymal cells have higher expression of phospho-AXL and PARP (Fig 1C; Supplement Fig 1D). These results were confirmed via western blot on a panel of epithelial and mesenchymal murine cell lines, though total PARP did not show a significant trend in this assay (Supplement Fig 1F). We found similar pathway activation in the human cell RPPA analysis (Supplement Fig 1E, Supplement Table 1), as well as in viability assays using inhibitors against AKT, PARP, and AXL in a panel of human cell lines. Epithelial human cancer cell susceptibility to MEK inhibition was shown previously (18), and AKT inhibition specifically inhibited the viability of the epithelial cells, with only one of the mesenchymal lines having a similar IC50 value (Supplement Fig 1C, Supplement Table 5). The mesenchymal human cell lines all demonstrated a lower IC50 when treated with either the PARP or AXL inhibitor as compared to the epithelial lines, thus corroborating the murine data.
Together, the overlap of 3 independent datasets revealed AKT as a novel epithelial cell dependency and confirmed preferential MAPK pathway activation in epithelial cells. In contrast, PARP and AXL were identified as potential mesenchymal cell survival dependencies (Fig 1D).
Z-cad dual sensor detects EMT in a dynamic fashion in 344SQ murine lung cancer cells
The integration of the drug screen, shRNA screen, and RPPA datasets narrowed the potential combinations for targeting both epithelial and mesenchymal tumor cells to 2 targets each. However, bulk assays do not provide clear insight into whether these drugs are specifically targeting their respective subpopulations.
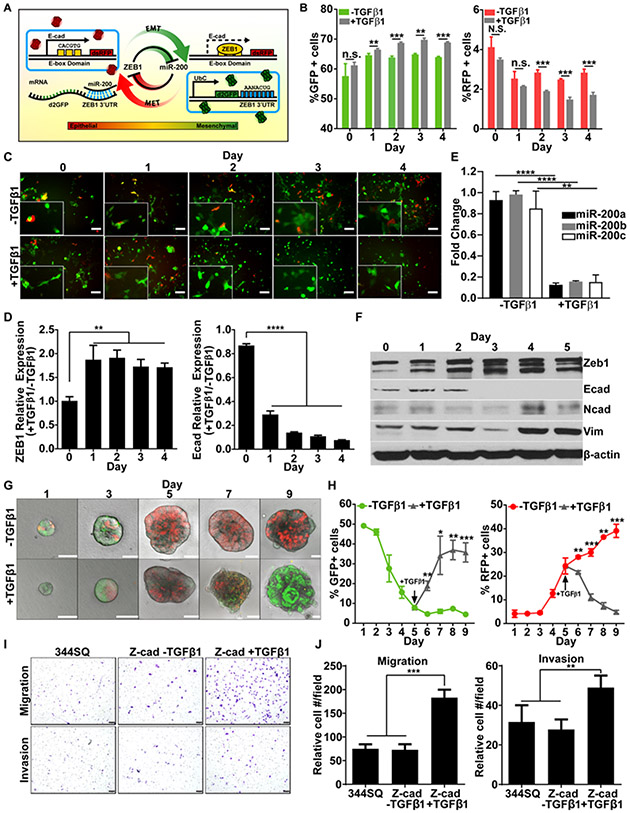
To further investigate the effects on population heterogeneity, we employed a fluorescent reporter stably transfected into our murine lung cancer cells (23). Briefly, this two-plasmid sensor system, termed the Z-cad sensor, uses one construct with a destabilized GFP linked to the 3’ UTR of Zeb1 and a separate plasmid with RFP expressed downstream of the E-cadherin promoter (Fig 2A). When cells are in a mesenchymal state, the endogenous Zeb1 protein levels are high, leading to suppression of its targets including miR-200 and E-cadherin, and thus RFP expression. In an epithelial state, high miR-200 levels downregulate Zeb1 levels post-transcriptionally via its 3’UTR, decreasing the GFP signal. The suppression of Zeb1 leads to the de-repression of the E-cadherin promotor and increased RFP expression.
Figure 2. The Z-cad dual sensor dynamically detects EMT in murine NSCLC.
(A) Schematic diagram illustrating the Z-cad dual sensor constructs. The d2GFP-Zeb1 3’UTR construct constitutively expresses destabilized GFP under the control of a ubiquitin promoter. The Zeb1 3’ UTR, which contains 8 miR-200 binding sites, is expressed downstream of d2GFP. The E-cad-RFP construct contains the E-cadherin promoter, with 3 E-box domains. This promoter regulates the expression of RFP. (B) The Z-cad dual sensor system was expressed in the 344SQ murine cancer cells (344SQ_Z-cad cells). Flow cytometry for the percentage of GFP+ (left) and RFP+ (right) cells was performed over 4 days with and without TGF-β (5 ng/ml). Data was analyzed using unpaired Students t-test. N.S.= not significant, ** p< 0.01, *** p< 0.001. (C) The 344SQ_Z-cad cells were grown over 4 days with and without TGF-β (5 ng/ml) and fluorescent microscopy was performed. Representative images are shown. Scale bar=100 μM. (D) Real-time PCR (qPCR) analysis for relative expression of Zeb1 and E-cadherin in 344SQ_Z-cads over 4 days with and without TGF-β (5 ng/ml). Expression values are normalized against L32 reference gene. Statistical difference compared to day 0 for all samples. ** p< 0.01, **** p< 0.0001. (E) qPCR analysis of miR-200a/b/c in 344SQ_Z-cad cells with or without TGF-β treatment. Values were normalized to miR-16. (F) Western blot was performed on the 344SQ_Z-cad cells treated with TGF-β (5 ng/ml) over 5 days. Zeb1, E-cadherin, N-cadherin, and vimentin were probed as markers of EMT, and β-actin was used as a loading control. (G) Fluorescent confocal images were acquired of 344SQ_Z-cad cells plated on a Matrigel matrix. On day 5, TGF-β (5 ng/ml) was added. Confocal images acquired over 9 days and representative images are shown on each day. Scale bar = 50 μM. (H) Flow cytometry of the percentage of GFP+ and RFP+ cells was performed on the 344SQ_Z-cad 3D spheres grown over 9 days as described in F. TGF-β (5 ng/ml) added on Day 5 shown in gray line. Data was analyzed using unpaired Students t-test. * p< 0.05, ** p< 0.01, *** p< 0.001. (I) 344SQ wildtype and 344SQ_Z-cad cells −/+ TGF-β (5 ng/ml) were plated in Transwell migration and invasion assays. Representative images of chambers in each condition are shown. Scale bar = 1mm. (J) The relative cell number per field in migration and invasion chambers from (H) were analyzed. n= 3 chambers per condition. Data was analyzed using an unpaired Students t-test. ** p< 0.01, *** p< 0.001.
We co-expressed the Z-cad sensor plasmids in the mesenchymal 344SQ murine cell line (344SQ_Z-cad). We utilized the 344SQ instead of the 344P cells as an additional validation of the findings and because while both are mesenchymal in 2-D culture, the 344SQ cells display even greater plasticity and readily undergo MET under different conditions (14, 24); thus, they were an ideal cell line to test the dynamic readout of the Z-cad reporter. We confirmed the functionality of the sensor in detecting each phenotypic state. In 2-D culture, the 344SQ_Z-cad cell line is ~58% GFP+ at baseline by flow cytometry and fluorescent imaging, whereas only ~4% of the population is RFP+ (Fig 2B, C). To determine that the sensor responds in a dynamic manner to EMT-promoting conditions, the 344SQ_Z-cad cells were stimulated with TGF-β1 to further induce a mesenchymal state. As expected, the addition of TGF-β1 significantly increased the percentage of GFP+ cells within 24 hours, with a significant decrease in the RFP+ epithelial cells occurring within 2 days and continuing throughout the experiment (Fig 2B, C). We confirmed that TGF-β1 induced a molecular EMT by measuring Zeb1, vimentin, N-cadherin, E-cadherin and the miR-200 family expression (Fig 2D-F).
The phenotypically plastic 344SQ cells can shift their EMT status based on external stimuli. When cultured in a 3-D laminin-rich Matrigel matrix, the cells form polarized epithelial spheres (14). Thus, we tested whether these epithelial structures were also RFP+ by plating the 344SQ_Z-cad cells in a Matrigel matrix. Fluorescent imaging and flow cytometry confirmed that while 50% GFP+ after initial plating, each day in Matrigel caused a reduction in the GFP+ subpopulation with a steady increase in the RFP+ population (Fig 2G, H). After 9 days in culture, the 3-D structures were roughly 40% RFP+ and <10% of cells maintained GFP expression. Again, addition of TGF-β1 at day 5 of 3-D culture stimulated EMT and produced GFP+ expression within 24 hours (Fig 2G, H), overcoming the influence of the Matrigel matrix. Lastly, we confirmed that the 344SQ_Z-cad cell lines mirror the parental 344SQ cells in their migratory and invasive phenotype and that TGF-β1 increased their invasive capability in Transwell assays, again correlating with a mesenchymal phenotype (Fig 2I, J).
Detecting RFP+ epithelial cells in 393P cells with inducible GFP-Zeb1 as a half sensor of EMT
As the 344SQ_Z-cad cells are mainly mesenchymal but plastic at baseline, we sought to create a converse model of an epithelial cell line that can effectively sense induction of EMT. Thus, we created a half sensor in the epithelial 393P cells expressing a doxycycline inducible GFP-tagged Zeb1 (18). In these cells, we introduced a single plasmid, the construct expressing RFP downstream of the E-cadherin promoter (393P_pTG-Zeb1-ER). As measured by flow cytometry and confirmed qualitatively by fluorescent microscopy, these cells are ~80% RFP+ at baseline with no detectable GFP without doxycycline (Supplement Fig 2A, B). However, GFP-Zeb1 expression increased 4 hours after doxycycline, with a robust increase observed after 48 hours (Supplement Fig 2A, B). Similar results were observed when the 393P_pTG-Zeb1-ER cells were cultured within a 3-D Matrigel matrix, with structures converting from RFP+ to GFP+ within 5 days of GFP-Zeb1 induction (Supplement Fig 2C). We confirmed a molecular EMT by analyzing the mRNA and protein levels of E-cadherin and Zeb1 (Supplement Fig 2D, E), and the miR-200 family expression (Supplement Fig 2H). Additionally, we confirmed that GFP-Zeb1 expression significantly promoted both migration and invasion as compared to the no doxycycline control and wildtype 393P cells (Supplement Fig 2F, G). Lastly, we compared the Zeb1-induced EMT with a TGF-β1-stimulated EMT and found that both GFP-tagged Zeb1 and TGF-β1 stimulation were able to significantly repress the RFP+ population in the 393P_pTG-Zeb1-ER cells (Supplement Fig 2I-K). Taken together, we confirmed that these cells can dynamically detect an EMT.
Utilizing the sensor cells to confirm the EMT-centric drug screen results
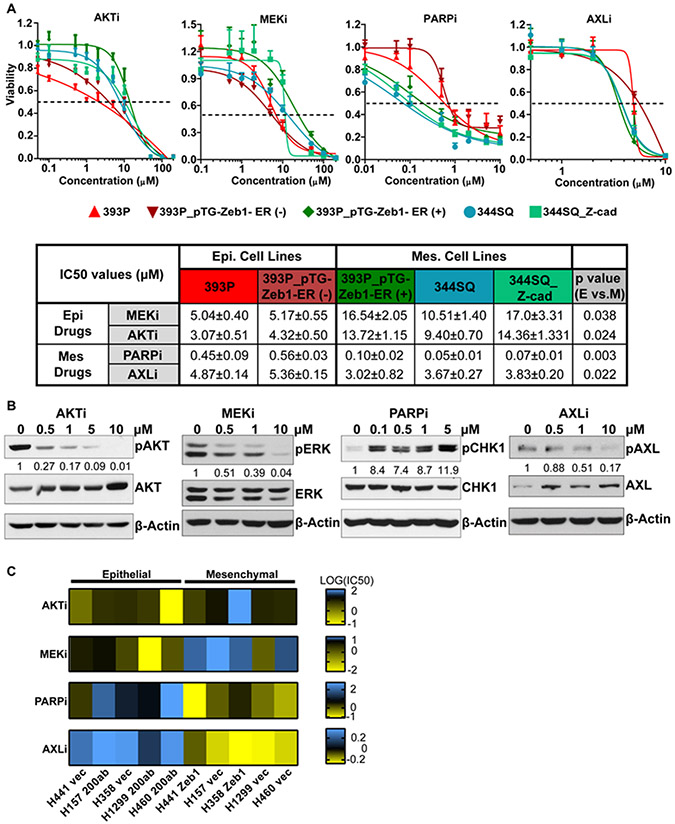
Utilizing the 344SQ_Z-cad and 393P_pTG-Zeb1-ER cell lines as sensors for EMT, we confirmed that the manipulated cell lines responded similarly to their corresponding parental cell lines upon treatment with the drugs indicated in Figure 1, and further assessed whether EMT directly alters the sensitivity of the cells to each drug.
Specifically, we compared the viability of the 344SQ_Z-cad and parental 344SQ cells, and the 393P_pTG-Zeb1-ER cells to the parental 393P cells when treated with inhibitors of AKT, MEK, PARP, and AXL. We found that each sensor cell line responded similarly as the corresponding parental cell line (Fig 3A), providing confidence that the manipulated cell lines can be used for future analyses. We confirmed that each drug hit its respective target by western blotting after treatment with escalating doses of each agent in the 344SQ_Z-cad cells for 48 hours (Fig 3B). We also induced the expression of GFP-Zeb1 in the 393P_pTG-Zeb1-ER cell line with doxycycline, pushing these cells into a mesenchymal state (Supplement Fig 2). Taking all cell lines together and comparing the epithelial to the mesenchymal groups, we found a significant difference in the sensitivities to each of the drugs. The epithelial lines (red shades) were significantly less viable in the face of the AKT inhibitor MK2206 or the MEK inhibitor selumetinib, whereas the mesenchymal cell lines (blue-green shades) were significantly less viable when treated with either the PARP inhibitor talazoparib or the AXL inhibitor bemcentinib (Fig 3A). We also found that longer term treatments with single agent selumetinib or MK2206 (~4 weeks) produced a partial resistance to the drug (Supplement Fig 3A) and induced an EMT in the 344SQ_Z-cad cell lines, as shown by immunofluorescence images demonstrating a downregulation of membranous E-cadherin and upregulation of Zeb1 (Supplement Fig 3B, C). Conversely, long term treatment with and subsequent resistance to bemcentinib or talazoparib induced an MET, with a robust increase in membranous E-cadherin and downregulation of Zeb1 (Supplement Fig 3A-C).
Figure 3. EMT alters sensitivity of cells to AKT, MEK, PARP, and AXL inhibitors in mouse and human lung cancer cell lines.
(A) In vitro cell viability was measured via MTT assay in epithelial cell lines (393P (red), 393P_pTG-Zeb1-ER (−) doxycycline (dark red)), and in mesenchymal cell lines (393P_pTG-Zeb1-ER (+) doxycycline (dark green), 344SQ (teal), and 344SQ_Z-cads (light green)) treated with MK2206 (AKTi), selumetinib (MEKi), talazoparib (PARPi), or bemcentinib (AXLi) for 72 hours. N = 8 per each drug concentration. The curve was generated using a nonlinear regression fit model. IC50 values are listed in the table below the graphs ± standard deviation. Statistical analysis was performed using an unpaired Students t-test comparing epithelial cells lines (reds) to mesenchymal cell lines (greens). (B) 344SQ_Z-cad cells were treated with each of the drugs from (A) for 48 hours, and western blot was utilized to demonstrate drug efficacy over a dose range. For AKT inhibitor treatment, phospho-AKT was used to demonstrate efficacy. Phosphorylated ERK was used as a marker for MEK inhibitor efficacy. With treatment with PARP inhibitor, increased expression of phospho-CHK1 was used to demonstrate drug efficacy. Phospho-AXL was used to demonstrate efficacy of AXL inhibitor treatment. Total levels of proteins and β-actin were used as controls across all drug treatments. Concentrations of drugs utilized are depicted above each lane. Densitometry calculations were performed using ImageJ software. The phosphorylated protein of interest was measured and normalized to the loading control for each sample, and then normalized to the control (first lane) for each drug. (C) Human NSCLC cell lines were also tested for sensitivity to the drugs described in (A) as a function of EMT. Epithelial cell lines used were H358 and H441 and mesenchymal cell lines used were H460, H157, and H1299. The epithelial cells were driven to undergo EMT via doxycycline inducible Zeb1 and mesenchymal cells were driven to undergo MET via doxycycline inducible miR-200ab. The vector only cell lines were used as controls. IC50 values were obtained for each cell line with each drug treatment, log transformed, and graphed on a heatmap with blue indicating high IC50 values and yellow indicating low IC50 values.
Lastly, we tested the impact of EMT on drug sensitivity in human NSCLC cell lines. Specifically, we used H358 and H441 epithelial cells and H1299, H157, and H460 mesenchymal cell lines. To induce EMT in the epithelial lines, we introduced the doxycycline-inducible GFP-Zeb1 vector, and in the mesenchymal cells, we introduced a doxycycline-inducible miR-200a/b vector to induce MET, as previously described (18). Using these cell lines, we performed viability assays with AKT, MEK, AXL, and PARP inhibitors and determined the IC50 values. We found that cells in a mesenchymal state are more sensitive to bemcentinib and talazoparib than when in an epithelial state, and conversely, epithelial cells are more sensitive to selumetinib and MK2206 than the mesenchymal cells (Fig 3C, Supplement Table 5).
Overall, these data indicate that the EMT sensor cell lines are representative of the parental cell lines in terms of drug response and that EMT significantly alters the sensitivity of cells to inhibitors targeting AXL, PARP, MEK, or AKT in murine and human lung cancer cells.
MEK and AXL inhibitors synergistically decrease the viability of 344SQ Z-cad cells
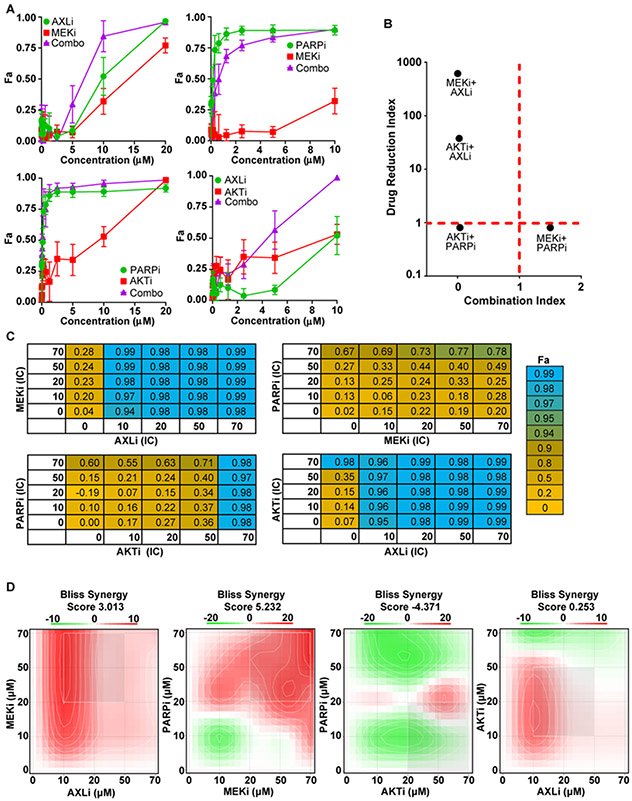
Our data indicate that selumetinib and MK2206 target epithelial cells and bemcentinib and talazoparib target mesenchymal cells. However, our goal was to identify a drug combination(s) efficacious against heterogeneity by killing subpopulations in either phenotypic cell state. Therefore, we performed synergy analyses with combinations of one epithelial drug and one mesenchymal drug.
We treated the 344SQ_Z-cad cells with an epithelial cell targeting drug or a mesenchymal cell targeting drug for 72 hours. We applied two different tools to assess synergy, the Chou-Talalay method based on Loewe additivity (25) and SynergyFinder 2.0 using Bliss analysis (26) . Inhibitors were combined and the fraction affected (Fa) values were obtained after exposure to a series of fixed concentrations (Fig 4A). The combination index (CI) and drug reduction index (DRI) were calculated for each dose using the Chou-Talalay method (Supplement Fig 4A, B). We relied on favorable DRI, shown in yellow (Supplement Fig 4B) to confirm the CI data. The drug combinations of selumetinib + bemcentinib and bemcentinib + MK2206 showed favorable DRI (DRI>1) and evidence of synergy (CI<1) (Fig 4B, Supplement Table 6). Additionally, we evaluated the drug combinations using a non-constant ratio (Fig 4C; drug concentrations listed in Supplement Table 7). Utilizing SynergyFinder, we found the combination of selumetinib + bemcentinib and talazoparib + selumetinib had the highest bliss synergy scores, indicating synergism (Fig 4D).
Figure 4. MEK and AXL inhibition is a synergistic combination in the murine 344SQ_Zcad sensor cell line and human lung cancer cell lines.
(A) 344SQ_Z-cad cells were treated with bemcentinib (AXLi), selumetinib (MEKi), talazoparib (PARPi), or MK2206 (AKTi) single agents or the indicated combinations for 72 hours, and cell growth was measured using MTT assays. A constant drug ratio was used for each combination and ratios are listed in Supplement Fig 4C. The fraction affected (Fa) versus drug concentration is shown for each individual drug and the combination (purple). Values were normalized to DMSO control wells. (B) The 4 drug combinations from (A) were used to determine the Drug Reduction Index (DRI) and Combination Index (CI) using the Chou-Talalay method. (C) Fa tables are shown for four drug combinations of MEKi, AXLi, PARPi, and AKTi. Combinations used are listed on each table over five concentrations of 0, IC10, IC20, IC50, and IC70 of each drug. Exact concentrations used for each drug are listed in Supplement Table 5. (D) Synergy scores were calculated for all independent combinations from C, using the Bliss independence model. Mean synergy scores are shown. Red sections indicate areas of synergism, green areas of antagonism, and white areas of additive interactions.
We also tested the efficacy of combining MEK and AXL inhibitors in the human NSCLC lines, A549 and H358. Using the Chou-Talalay method, we found that MEK plus AXL inhibition was a synergistic combination in both lines (Supplement Fig 4C-D). Interestingly, when cells are “locked” into one phenotypic state by expression of Zeb1 or miR-200, synergy is diminished. Specifically, in the epithelial H441 cells expressing the control vector, we found very strong synergism with selumetinib + bemcentinib (Supplement Fig 4E). However, with Zeb1 induction, there was only slight synergism observed at the highest concentrations of the combination (Supplement Fig 4F). Similarly, the combination was strongly synergistic in the mesenchymal H1299 cells (Supplement Fig 4G), but with forced miR-200 expression, synergism is only observed at the highest concentrations, but with unfavorable DRI (Supplement Fig 4H, Supplement Table 6). Thus, these data suggest that a heterogeneous population is required for the observed drug synergism with the combination of MEK and AXL inhibitors.
Further evidence for the combination of MEK and AXL inhibitors was explored by analyzing a previously described selumetinib-resistant cell line, derived from 393P tumors that have undergone EMT after long term in vivo treatment (393P_AZDR1) (18). Unlike the 393P control line, the resistant cells are no longer receptive to selumetinib (Supplement Fig 5A), but demonstrate a shift in sensitivity to bemcentinib, with ~2.5-fold decrease in IC50 as compared to the control cells. Additionally, protein analyses demonstrate that MEK is shut off in the AZDR1 cells, as expected, but they have a robust increase in AXL (Supplement Fig 5B). Lastly, we analyzed signaling cascades in the face of each single agent in both cell lines and tumors and found a robust increase in phospho-AXL with selumetinib treatment (Supplement Fig 5C,D), whereas treatment with the AXL inhibitor caused an increase in phospho-ERK levels. Together, these data suggest that treatment with one compound sensitizes the remaining viable cells to the other, further supporting that the combination of selumetinib and bemcentinib synergistically impacts the growth of lung cancer cells.
MEK and AXL inhibition targets epithelial and mesenchymal cells, respectively
We identified the combination of the MEK inhibitor selumetinib and the AXL inhibitor bemcentinib as a synergistic combination in bulk assays analyzing cell viability. However, we next wanted to utilize the EMT-sensing cells to determine whether each drug specifically targets its respective subpopulation, as well as analyze the impact of the drug combination.
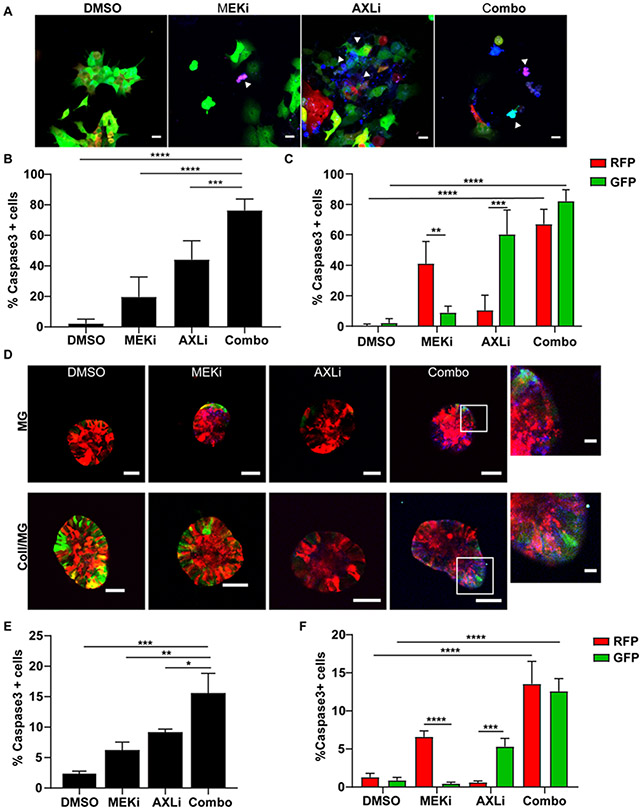
To accomplish this, we performed confocal microscopy of 344SQ_Z-cad cells treated with single agent or the selumetinib/bemcentinib combination, and cells were stained with a caspase-3/7 substrate dye as a readout for apoptosis. In 2-D culture, DMSO control showed little caspase-3 activity (Fig 5A-C). In the selumetinib treatment, there was a significant increase in caspase-3+/RFP+ cells, with ~40% of the RFP+ cells undergoing cell death, whereas less than 10% of the GFP+ cell population underwent apoptosis with selumetinib treatment (Fig 5C). Conversely, bemcentinib treatment specifically killed 60% of the GFP+ subpopulation with a slight increase in death in the RFP+ cells. Combination treatment demonstrated a significant increase in the total amount of cell death as measured by total caspase-3+ cells (Fig 5B), and interestingly, the combination killed both subpopulations to a greater degree than either single agent (Fig 5C). These data were supported by flow cytometry analysis from 344SQ_Z-cad cells treated with single agent or combination, which found that selumetinib treatment significantly decreased the RFP+ viable population, whereas bemcentinib treatment significantly decreased the GFP+ viable population (Supplement Fig 6A).
Figure 5. MEK and AXL inhibitors target epithelial and mesenchymal cells, respectively, decreasing tumor cell viability in 3D.
(A-C) 344SQ_Z-cad cells were treated with DMSO, selumetinib (MEKi) (5 μM), bemcentinib (AXLi) (2 μM) or the combination. NucView® 405 Caspase 3 substrate was added to each condition as a readout for apoptosis. Representative fluorescence microscopy images are shown in (A) which were acquired 72 hours after addition of drugs. Scale bar = 20 μM. Red; epithelial cells, Green; mesenchymal cells, blue; NucView® 405 Caspase-3 substrate. (B) Images from (A) were quantified for total caspase-3+ cells as a percentage of total cells in each FOV. n = 4-7 FOV. (C) Images from (A) were also quantified for the percentage of RFP+ or GFP+ cells that were also caspase-3+ in each FOV within each treatment condition. (D-F) 344SQ_Z-cad cells were plated in a Matrigel (MG) or a Collagen/Matrigel (Coll/MG) matrix. After 24 hours, spheroids were treated with DMSO, MEKi (5 μM), AXLi (2 μM) or the combination. After three days of treatment, NucView® 405 Caspase 3 substrate was added to each condition as a readout for apoptosis and confocal images were acquired. Representative images are shown in (D). Scale bar = 50 μM. (E) 344SQ_Z-cad spheroids from (D) were disassociated from the 3-D Coll/MG matrix environment and processed into single cells. These cells were then analyzed by flow cytometry for the percentage of caspase-3+ cells (E) as well as the percentage of RFP+ or GFP+ cells that were also positive for caspase-3 (F).
We also tested the effect of each drug on epithelial and mesenchymal subpopulations when cultured in 3-D matrices. We embedded the 344SQ_Z-cad cell lines within a 3-D matrix and treated with single agent or combination of selumetinib and bemcentinib. As shown previously, the 344SQ_Z-cad cells shift towards RFP+ epithelial phenotype when embedded within a Matrigel (MG) matrix (Supplement Fig 6B). To quantify, we calculated the percentage of the colored pixels that are either GFP or RFP per field of view (Supplement Fig 6C). Selumetinib treatment caused an enrichment in GFP+ structures (Supplement Fig 6B, C), whereas bemcentinib had little effect, likely due to the lower percentage of GFP+ cells at baseline. Therefore, we also utilized a collagen type I and Matrigel (Coll/MG) matrix, which promotes a mesenchymal phenotype (24, 27). In a Coll/MG matrix, 344SQ_Z-cad structures were 68% GFP+ at baseline (Supplement Fig 6B, C). Treatment with selumetinib had little impact in this matrix; however, bemcentinib significantly enriched the epithelial RFP+ population. In both matrices, the combination of selumetinib and bemcentinib returned the RFP and GFP percentages to about 50:50, suggesting that both tumor cell subpopulations are being targeted equally. We also analyzed the viability of these 3-D structures in single agent and combination treatments. In MG, selumetinib significantly decreased cell viability, whereas bemcentinib had no significant effect. Combining selumetinib and bemcentinib significantly decreased viability compared to single agent MEK inhibition. In Coll/MG, both single agents decreased viability to about 50%, whereas the combination had a greater impact than either single agent (Supplement Fig 6D).
Lastly, we tested the specific cytotoxicity of each drug on their respective EMT subpopulation within a 3-D microenvironment. Using the caspase-3/7 substrate dye described above, we found a robust increase in total cell death in the combination of selumetinib and bemcentinib in both MG and Coll/MG conditions (Fig 5D, E; Supplement Fig 6E). Analyzing the caspase-3+ cells within EMT subpopulations, we determined that selumetinib is specifically cytotoxic towards the RFP+ epithelial cells in both Coll/MG (Fig 5F) and MG (Supplement Fig 6E) matrices, whereas bemcentinib specifically targets the GFP+ mesenchymal population. Combining these inhibitors caused a significant increase in death in both subpopulations to a greater degree than single agent treatments.
Using the Z-cad EMT reporter system, we determined that the MEK inhibitor selumetinib specifically targets and kills RFP+ epithelial cells, whereas the AXL inhibitor bemcentinib specifically targets GFP+ mesenchymal tumor cells. Together, the combination targets both subpopulations effectively, significantly decreasing overall tumor cell viability in 2-D and 3-D cultures.
Co-targeting MEK and AXL significantly repressed tumor growth in vivo
To determine the translational relevance of the combination of selumetinib and bemcentinib inhibitors, we tested the in vivo efficacy of this treatment strategy.
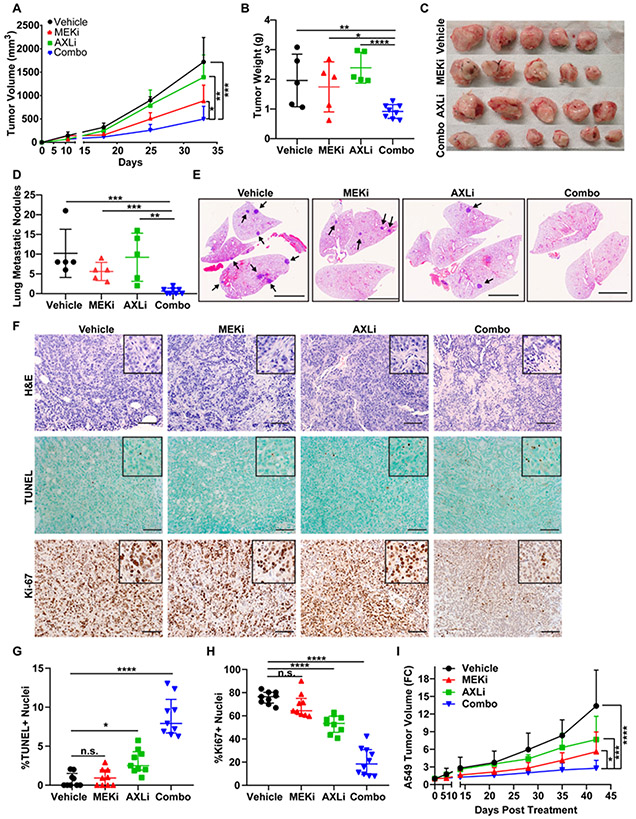
We implanted the 344SQ_Z-cad cells subcutaneously in immunocompetent wildtype mice. In two independent studies, we treated mice with selumetinib, bemcentinib, or the combination for 3-4 weeks after tumor formation. Using caliper measurements over time, we found that single agents did delay tumor growth (Fig 6A, Supplement Fig 7A-D); however, this effect was largely lost by the end of treatment as shown by tumor weights and images taken at necropsy (Fig 6B, C; Supplement Fig 7D). Additionally, single agent treatment with bemcentinib in wildtype 344SQ tumors also demonstrated no significant difference in primary tumor size or in lung metastatic nodule formation (Supplement Fig 7E), suggesting single agent resistance develops rapidly. In contrast, the co-targeting treatment strategy had a significant impact on tumor growth throughout the duration of treatment (Fig 6A; Supplement Fig 7C). Additionally, we analyzed the impact of treatment on the metastatic ability of the tumor cells by macroscopic lung metastatic nodule counts and lung H&Es and found a significant repression in lung metastases with the combination treatment compared to either single agent or vehicle (Fig 6D, E). We observed no change in body weight over time (Supplement Fig 7B), suggesting no overt toxicities with the treatments. These data were corroborated by histopathological (Supplement Fig 8A, B) and serum (Supplement Fig 8C) analyses to analyze the impact of single agent or combination treatment on kidney and liver functions (Supplement Table 8). Both methods revealed no aberrant changes in liver and kidney morphology or function, suggesting no chronic toxicity from treatment.
Figure 6. Co-targeting MEK and AXL significantly decreases tumor growth and viability in vivo.
(A) In vivo tumor volume measurements at the indicated time points (days) for 344SQ_Z-cad subcutaneous tumors in syngeneic 129/Sv mice after daily treatment with selumetinib (MEKi) (25 mg/kg), bemcentinib (AXLi) (100 mg/kg), combination (MEKi (25 mg/kg) + AXLi (100 mg/kg)), or vehicle control. Treatment start time was day 10 and endpoint was day 32. Treatment performed on 5-8 mice per group. Tumor volume data plotted as mean and SD. (B) Tumor weight was recorded at endpoint per group on day 32. * p< 0.05, ** p< 0.01, **** p< 0.0001. (C) Gross images of tumors from (B). (D) At necropsy, mouse lungs from the experiment described in (A) were analyzed for macroscopic metastatic lung nodules in each treatment group. ** p<0.01, *** p<0.001. (E) Representative H&E images of mouse lungs from the experiment described in (A). Arrows denote single metastatic lung nodules. (F) Tumors from the treatment efficacy experiment described in (A) were formalin-fixed and paraffin embedded for H&E and immunohistochemical analyses. TUNEL was used to measure cell death and Ki67 was used to measure cell proliferation in vehicle, MEKi, AXLi, or combination treated mice. (G) TUNEL and (H) Ki67 IHC images were quantified in each treatment group. N = 3 mice per group, 3 FOV per mouse for a total of 9 images per group. (I) A549 human NSCLC cells were implanted subcutaneously into athymic nude mice. After tumor formation (~4 weeks), mice were treated with single agent selumetinib (MEKi), bemcentinib (AXLi), the combination, or vehicle control. Mice were treated daily, and tumor growth was monitered using weekly caliper measurements. Graph represents tumor volume as a fold change (FC) normalized to the tumor volume measurement taken 1 day prior to the start of treatment.
We confirmed that each drug was targeting its respective pathway by performing immunohistochemical analyses on tumors from each treatment group. As expected, treatment with the MEK inhibitor caused a reduction in phospho-ERK, whereas bemcentinib reduced phospho-AXL staining (Supplement Fig 9A). Interestingly, treatment with bemcentinib increased phospho-ERK levels and selumetinib increased phospho-AXL levels, supporting the in vitro findings of reciprocal pathway activation with single agent treatments.
While the combination significantly repressed tumor growth, the efficacy seemed less impressive than our in vitro studies would have suggested. To better understand the TME with single agent and combination treatments, we performed histological analyses (Fig 6F). H&E sections from these tumors revealed that significant portions of the combination treated tumors encompassed non-nucleated regions as measured by area of eosin staining per FOV (Fig 6F; Supplement Fig 9B). This suggests that the impact of combination treatment cannot be wholly measured by the tumor size alone. Additionally, we found a significant increase in apoptotic cells as measured by TUNEL staining (~2-3-fold), and conversely, a significant repression in proliferation as measured by Ki67 in combination treated tumors (~4-fold; Fig 6F-H). Together, our data indicate that inhibiting MEK and AXL together significantly reduced tumor cell viability as well as likely influenced other factors within the TME.
Additionally, we tested the efficacy of combining MEK and AXL inhibitors in a human xenograft model. Human A549 cells were implanted subcutaneously into athymic nude mice. Once tumors were palpable (~4 weeks), we treated with single agents or the combination of selumetinib and bemcentinib. Similar to the 344SQ_Z-cad study, we found that the combination treatment was more efficacious in controlling tumor growth (Fig 6I, Supplement Fig 9C). Specifically, these tumors demonstrated only 2.7-fold increase in growth over the 6 weeks of treatment, as compared to ~13-fold in vehicle control mice. Single agent treatments were partially effective, with 7.6-fold and 5.6-fold increase in tumor growth with bemcentinib and selumetinib treatment, respectively. These data confirm that co-targeting MEK and AXL in a representative human xenograft model has a significant effect in controlling tumor cell growth.
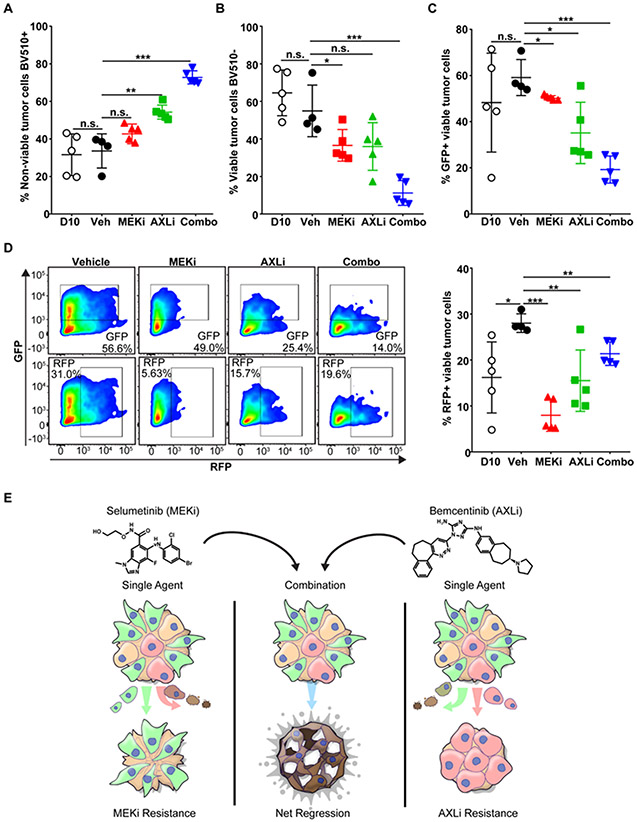
MEK and AXL inhibitors are efficacious in combination by targeting epithelial and mesenchymal subpopulations in tumors
To analyze the impact of treatment on EMT subpopulations, we collected the 344SQ_Z-cad tumors at day 10 (prior to receiving any treatment; D10) as well as at necropsy for flow cytometry analysis of tumor cell viability, and RFP or GFP signals from the subpopulations (Supplement Fig 9D). Consistent with the tumor growth patterns and the in vitro data, we found total viable cells as measured by Ghost 510 live/dead marker to be significantly reduced in the combination treatment arm with a corresponding significant increase in non-viable tumor cells (Fig 7A, B; Supplement Fig 9E). In fact, combination treatment tumors had only ~10% viable cells after the 3 weeks of treatment compared to ~40% viable tumor cells in either single agent treatment or ~60% in controls. From the remaining viable cells, we analyzed the percentage of GFP+ and RFP+ cells. As expected, the majority of cells within the vehicle treated tumors were GFP+ (roughly 60%) (Fig 7C, D), and this was not statistically different from the day 10 tumors. There was a marginal yet statistically significant decrease in viable GFP+ cells with the treatment of selumetinib, whereas bemcentinib caused a more robust and significant decrease in this population to <40%. The combination of selumetinib and bemcentinib demonstrated the greatest reduction in the GFP+ mesenchymal population, significantly lower than the D10 early tumors and the time matched vehicle treated mice. Conversely, we found a significant increase in the RFP+ population between early (D10) and late tumors (Veh), suggesting the epithelial population increases over time. Selumetinib treatment significantly decreased the RFP+ to less than 10% (Fig 7D). Interestingly, we also observed a significant decrease in RFP+ cells with bemcentinib treatment, which returned the RFP+ population back to the baseline levels observed in the early D10 tumors, although this effect was not as strong as that seen with selumetinib. Combination treatment also significantly decreased the RFP+ subpopulation, though the decrease in RFP+ cells was less robust than that observed with single agent treatments, with ~20% of RFP+ epithelial cells still viable in the combination treatment group. Overall, the in vivo data revealed that the combination therapy was superior in controlling mesenchymal tumor cell growth than either single agent, whereas the effect on the epithelial population is slightly more ambiguous.
Figure 7. MEK and AXL inhibitors work synergistically to target phenotypic heterogeneity within tumors.
(A-D) Flow cytometry analysis was performed on 344SQ_Z-cad tumors treated with selumetinib (MEKi), bemcentinib (AXLi), the combination, or vehicle control (described in Figure 6A). Tumors were collected at day 10 (D10), indicative of an early timepoint prior to treatment start, and at endpoint (day 32). Tumors were then processed for flow cytometry analysis of live/dead cells. Non-viable (A) and viable (B) tumor cells were quantitated in each treatment group. N.S. not significant, ** p< 0.01, *** p< 0.001. (C) Flow cytometry analysis of GFP+ or RFP+ cells from tumors in each treatment group. Tumors were collected and processed for flow cytometry analysis of live/dead, and viable cells were further gated with RFP vs GFP. * p< 0.05, ** p< 0.01, *** p< 0.001. (D) Representative dot plot of the percentage of GFP+ and RFP+ cells from a single tumor for each treatment group from (C). (E) Model representing MEK and AXL inhibitors killing epithelial or mesenchymal cells within a tumor, respectively. In combination, MEK and AXL inhibitors are able to synergistically kill both epithelial and mesenchymal cells within a tumor.
Together, our data provides a rational drug combination that co-targets MEK and AXL signaling pathways. This combination works effectively to target cells in an epithelial or mesenchymal phenotypic state, leading to significant repression of tumor growth and prevention of resistant outgrowth by targeting EMT-related tumor heterogeneity (Fig 7E).
Discussion
EMT is a well-studied but complex and dynamic epigenetic reprogramming event that promotes tumor progression, metastasis, and drug resistance, facilitating cancer cell adaption to conditions within the TME to ensure survival and thereby producing considerable cellular heterogeneity. The goal of this study was to identify novel combination treatment strategies that can inhibit cells in either phenotypic state to prevent EMT-mediated escape. We performed a selective drug screen on representative epithelial and mesenchymal murine lung cancer cell lines and overlapped those select targets with unbiased datasets analyzing genes necessary for in vivo cell survival and protein signaling cascades activated in epithelial and mesenchymal cells. We identified AKT and MAPK as epithelial cell dependencies and AXL and PARP as mesenchymal cell dependencies. Previous data from our lab highlighted that epithelial cancer cells are dependent on MAPK signaling for survival whereas mesenchymal cells are not, even when harboring identical KRAS mutations(18). Additionally, the expression and activity of AXL in mesenchymal cancer cells has been established in the literature. In patients with esophageal squamous cell carcinoma, AXL mRNA expression was significantly correlated with several EMT markers including vimentin and Zeb1(28). AXL is expressed in HER2+ breast cancers with a positive EMT signature and essential for metastasis(29), upregulated in drug resistant models of prostate cancer(30), found in mesenchymal subsets of lung cancer(31-33), and is an upstream regulator of EMT to promote cancer stem cell initiation and chemoresistance in breast cancer(34). Together, these data provide confidence that the targets identified in our screens were likely EMT-centric hits and worthy of additional study in a dynamic system.
Methodologies assaying the process of EMT lack the ability to capture dynamic changes in real-time and/or in a heterogeneous population. The dual Z-cad reporter system was designed to address these issues by simultaneously reporting the activity of the miR-200 family on the GFP-Zeb1-3’UTR, and conversely, Zeb1 activity on E-cadherin-driven RFP(23). As the miR-200/Zeb1 axis is critical for EMT(13-16), this was an ideal model to evaluate EMT shifts in the face of targeted agent treatments. By expressing the Z-cad sensor in the murine 344SQ cells, we determined that the MEK inhibitor selumetinib and the AXL inhibitor bemcentinib specifically target RFP+ epithelial and GFP+ mesenchymal populations, respectively, and when combined, significantly inhibit tumor cell growth in 2-D and 3-D in vitro systems. While mathematical models generated from 2-D assays revealed synergy with this combination, in some cases the impact appears more additive, such as within a 3-D matrix, though the combination outperforms single agent treatment in promoting tumor cell death. Interestingly, additional data revealed that synergy with bemcentinib and selumetinib in inhibiting tumor cell growth requires a heterogeneous cell population. When locked into either an epithelial or mesenchymal state by induction of miR-200 or Zeb1, respectively, the combination loses favorable DRI and synergism across multiple doses; thus, the combination is likely most efficacious in tumors that present with EMT-mediated heterogeneity or have the capacity to shift along the EMT spectrum as a mechanism of resistance.
In vivo murine and human cancer cell growth was significantly inhibited with selumetinib and bemcentinib compared to either single agent. In fact, the combination had marked efficacy on 344SQ_Z-cad tumor cell proliferation and death and may even influence the TME as shown by histology. Similarly, FACS analysis on treated tumors revealed that bemcentinib treatment reduced both GFP+ mesenchymal and RFP+ epithelial cells in vivo. This result may be due to effects beyond direct tumor cell killing in these syngeneic tumors. For example, treatment with AXL inhibitor has been shown to impact the tumor-infiltrating CD8+ and CD4+ T cells(35) and alters the immune cytokine and myeloid cell landscape(36); therefore, further analyses will be required to determine if either of these drugs alone or in combination are having non-cell-autonomous effects on controlling tumor growth.
The compounds utilized in the drug screen were largely selected for their clinical status; thus, any combination discovered may be readily translatable to clinical practice. Selumetinib has been and is currently being tested in clinical trials for treatment of various cancers driven by oncogenic RAS, including NSCLC. However, most of these trials did not improve progression free survival. Our group determined that one avenue of intrinsic and acquired resistance to MEK inhibition is EMT(18), indicating a need for combinatorial treatment strategies that either prevent this epigenetic shift or independently target mesenchymal cells. The AXL inhibitor bemcentinib was the first AXL-specific tyrosine kinase inhibitor to enter clinical trials and is currently in several phase I/II trials for glioblastoma, AML, TNBC, and NSCLC, either alone or in combination with chemotherapy agents or immunotherapies like pembrolizumab. Our data suggest that combining bemcentinib with an epithelial targeting drug like selumetinib may work effectively to target phenotypic heterogeneity and EMT plasticity within tumors, ultimately improving the anti-tumor efficacy of these targeted agents.
Supplementary Material
Acknowledgements:
We would like to thank BergenBio (Norway) for providing bemcentinib. We thank Dr. Sendurai Mani (MD Anderson Cancer Center, Houston TX) and Dr. Jeffrey Rosen (Baylor College of Medicine, Houston TX) for the E-cad RFP and GFP Zeb1 3’UTR expression constructs. We thank Dr. John Heymach (MD Anderson Cancer Center, Houston TX) for providing the GLS inhibitor for our drug screen. We thank the Institute for Applied Cancer Science (IACS at MD Anderson Cancer, Houston TX) for providing compounds for our drug screen. We thank the Flow Cytometry Lab South Campus Core facility at MDACC for the use of their facilities.
Funding: This work was supported in part by National Institutes of Health grants R37CA214609 (D.L.G.), R01CA207295 and U01CA213273 (L.A.B.), and F32CA239292 (J.M.K.). This work was also supported in part by the Cancer Prevention and Research Institute of Texas (CPRIT) grant RP160652 (D.L.G.), the University of Texas Lung Cancer SPORE grant P5CA070907, the LUNGevity foundation award (L.A.B. and D.L.G.), Rexanna’s Foundation (D.L.G. and L.A.B.), and through generous philanthropic contributions to The University of Texas MD Anderson Lung Cancer Moonshot Program. The Flow Cytometry Lab South Campus Core facility at MDACC is supported by CCSG NCI P30CA16672.
Footnotes
Conflict of Interest: D.L.G. has served on scientific advisory committees for AstraZeneca, GlaxoSmithKline, Sanofi and Janssen and has received research support from Janssen, Takeda, Ribon Therapeutics, Astellas and AstraZeneca. L.A.B. serves on advisory committees for AstraZeneca, AbbVie, GenMab, BergenBio, Pharma Mar SA, Sierra Oncology, Merck, Bristol Myers Squibb, Genentech, and Pfizer and has research support from AbbVie, AstraZeneca, GenMab, Sierra Oncology, Tolero Pharmaceuticals.
References:
- 1.Tam WL & Weinberg RA The epigenetics of epithelial-mesenchymal plasticity in cancer. Nature Medicine 19, 1438–1449 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thiery JP, Acloque H, Huang RY & Nieto MA Epithelial-mesenchymal transitions in development and disease. Cell 139, 871–890 (2009). [DOI] [PubMed] [Google Scholar]
- 3.Aktas B, Tewes M, Fehm T, Hauch S, Kimmig R & Kasimir-Bauer S Stem cell and epithelial-mesenchymal transition markers are frequently overexpressed in circulating tumor cells of metastatic breast cancer patients. Breast Cancer Res 11, R46 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gravdal K, Halvorsen OJ, Haukaas SA & Akslen LA A Switch from E-Cadherin to N-Cadherin Expression Indicates Epithelial to Mesenchymal Transition and Is of Strong and Independent Importance for the Progress of Prostate Cancer. Clinical Cancer Research 13, 7003–7011 (2007). [DOI] [PubMed] [Google Scholar]
- 5.Loboda A, Nebozhyn MV, Watters JW, Buser CA, Shaw PM, Huang PS et al. EMT is the dominant program in human colon cancer. BMC Medical Genomics 4, 9 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teschendorff AE, Journée M, Absil PA, Sepulchre R & Caldas C Elucidating the Altered Transcriptional Programs in Breast Cancer using Independent Component Analysis. PLOS Computational Biology 3, e161 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wellner U, Schubert J, Burk UC, Schmalhofer O, Zhu F, Sonntag A et al. The EMT-activator ZEB1 promotes tumorigenicity by repressing stemness-inhibiting microRNAs. Nat Cell Biol 11, 1487–1495 (2009). [DOI] [PubMed] [Google Scholar]
- 8.Aigner K, Dampier B, Descovich L, Mikula M, Sultan A, Schreiber M et al. The transcription factor ZEB1 (deltaEF1) promotes tumour cell dedifferentiation by repressing master regulators of epithelial polarity. Oncogene 26, 6979–6988 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Barrallo-Gimeno A & Nieto MA The Snail genes as inducers of cell movement and survival: implications in development and cancer. Development 132, 3151–3161 (2005). [DOI] [PubMed] [Google Scholar]
- 10.Eger A, Aigner K, Sonderegger S, Dampier B, Oehler S, Schreiber M et al. DeltaEF1 is a transcriptional repressor of E-cadherin and regulates epithelial plasticity in breast cancer cells. Oncogene 24, 2375–2385 (2005). [DOI] [PubMed] [Google Scholar]
- 11.Dumitriu IE, Dunbar DR, Howie SE, Sethi T & Gregory CD Human dendritic cells produce TGF-beta 1 under the influence of lung carcinoma cells and prime the differentiation of CD4+CD25+Foxp3+ regulatory T cells. J Immunol 182, 2795–2807 (2009). [DOI] [PubMed] [Google Scholar]
- 12.Massague J TGFbeta in Cancer. Cell 134, 215–230 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burk U, Schubert J, Wellner U, Schmalhofer O, Vincan E, Spaderna S et al. A reciprocal repression between ZEB1 and members of the miR-200 family promotes EMT and invasion in cancer cells. EMBO Rep 9, 582–589 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gibbons DL, Lin W, Creighton CJ, Rizvi ZH, Gregory PA, Goodall GJ et al. Contextual extracellular cues promote tumor cell EMT and metastasis by regulating miR-200 family expression. Genes Dev 23, 2140–2151 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol 10, 593–601 (2008). [DOI] [PubMed] [Google Scholar]
- 16.Korpal M, Lee ES, Hu G & Kang Y The miR-200 family inhibits epithelial-mesenchymal transition and cancer cell migration by direct targeting of E-cadherin transcriptional repressors ZEB1 and ZEB2. J Biol Chem 283, 14910–14914 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manshouri R, Coyaud E, Kundu ST, Peng DH, Stratton SA, Alton K et al. ZEB1/NuRD complex suppresses TBC1D2b to stimulate E-cadherin internalization and promote metastasis in lung cancer. Nature Communications 10, 5125 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peng DH, Kundu ST, Fradette JJ, Diao L, Tong P, Byers LA et al. ZEB1 suppression sensitizes KRAS mutant cancers to MEK inhibition by an IL17RD-dependent mechanism. Science Translational Medicine 11, eaaq1238 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blumenschein GR Jr., Smit EF, Planchard D, Kim DW, Cadranel J, De Pas T et al. A randomized phase II study of the MEK1/MEK2 inhibitor trametinib (GSK1120212) compared with docetaxel in KRAS-mutant advanced non-small-cell lung cancer (NSCLC)dagger. Ann Oncol 26, 894–901 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Janne PA, van den Heuvel MM, Barlesi F, Cobo M, Mazieres J, Crino L et al. Selumetinib Plus Docetaxel Compared With Docetaxel Alone and Progression-Free Survival in Patients With KRAS-Mutant Advanced Non-Small Cell Lung Cancer: The SELECT-1 Randomized Clinical Trial. Jama 317, 1844–1853 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun C, Hobor S, Bertotti A, Zecchin D, Huang S, Galimi F et al. Intrinsic resistance to MEK inhibition in KRAS mutant lung and colon cancer through transcriptional induction of ERBB3. Cell Rep 7, 86–93 (2014). [DOI] [PubMed] [Google Scholar]
- 22.Konen JM, Rodriguez BL, Fradette JJ, Gibson L, Davis D, Minelli R et al. Ntrk1 Promotes Resistance to PD-1 Checkpoint Blockade in Mesenchymal Kras/p53 Mutant Lung Cancer. Cancers (Basel) 11 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toneff MJ, Sreekumar A, Tinnirello A, Hollander PD, Habib S, Li S et al. The Z-cad dual fluorescent sensor detects dynamic changes between the epithelial and mesenchymal cellular states. BMC Biology 14, 47 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ungewiss C, Rizvi ZH, Roybal JD, Peng DH, Gold KA, Shin D-H et al. The microRNA-200/Zeb1 axis regulates ECM-dependent β1-integrin/FAK signaling, cancer cell invasion and metastasis through CRKL. Scientific Reports 6, 18652 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chou T-C Theoretical Basis, Experimental Design, and Computerized Simulation of Synergism and Antagonism in Drug Combination Studies. Pharmacological Reviews 58, 621–681 (2006). [DOI] [PubMed] [Google Scholar]
- 26.Ianevski A, Giri AK & Aittokallio T SynergyFinder 2.0: visual analytics of multi-drug combination synergies. Nucleic Acids Res (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Padhye A, Ungewiss C, Fradette JJ, Rodriguez BL, Albritton JL, Miller JS et al. A novel ex vivo tumor system identifies Src-mediated invasion and metastasis in mesenchymal tumor cells in non-small cell lung cancer. Scientific Reports 9, 4819 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang G, Kong X, Wang M, Zhao H, Han S, Hu R et al. AXL is a marker for epithelial-mesenchymal transition in esophageal squamous cell carcinoma. Oncol Lett 15, 1900–1906 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goyette M-A, Duhamel S, Aubert L, Pelletier A, Savage P, Thibault M-P et al. The Receptor Tyrosine Kinase AXL Is Required at Multiple Steps of the Metastatic Cascade during HER2-Positive Breast Cancer Progression. Cell Reports 23, 1476–1490 (2018). [DOI] [PubMed] [Google Scholar]
- 30.Lin J-Z, Wang Z-J, De W, Zheng M, Xu W-Z, Wu H-F et al. Targeting AXL overcomes resistance to docetaxel therapy in advanced prostate cancer. Oncotarget 8, 41064–41077 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taverna JA, Hung C-N, DeArmond DT, Chen M, Lin C-L, Osmulski PA et al. Single-cell Proteomic Profiling Identifies Combined AXL and JAK1 Inhibition as a Novel Therapeutic Strategy for Lung Cancer. Cancer Research, canres.3183.2019 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Byers LA, Diao L, Wang J, Saintigny P, Girard L, Peyton M et al. An epithelial-mesenchymal transition gene signature predicts resistance to EGFR and PI3K inhibitors and identifies Axl as a therapeutic target for overcoming EGFR inhibitor resistance. Clin Cancer Res 19, 279–290 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mak MP, Tong P, Diao L, Cardnell RJ, Gibbons DL, William WN et al. A Patient-Derived, Pan-Cancer EMT Signature Identifies Global Molecular Alterations and Immune Target Enrichment Following Epithelial-to-Mesenchymal Transition. Clinical Cancer Research 22, 609–620 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Asiedu MK, Beauchamp-Perez FD, Ingle JN, Behrens MD, Radisky DC & Knutson KL AXL induces epithelial-to-mesenchymal transition and regulates the function of breast cancer stem cells. Oncogene 33, 1316–1324 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo Z, Li Y, Zhang D & Ma J Axl inhibition induces the antitumor immune response which can be further potentiated by PD-1 blockade in the mouse cancer models. Oncotarget 8, 89761–89774 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ludwig KF, Du W, Sorrelle NB, Wnuk-Lipinska K, Topalovski M, Toombs JE et al. Small-Molecule Inhibition of Axl Targets Tumor Immune Suppression and Enhances Chemotherapy in Pancreatic Cancer. Cancer Research 78, 246–255 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.