Abstract
Background:
The distinction between within- and between-person associations with drug use disorder (DUD) has implications for intervention targets and content. We used longitudinal data from youth entering an urban emergency department (ED) to identify factors related to changes in DUD diagnosis, with particular emphasis on alcohol use.
Methods:
Research staff recruited youth age 14–24 (n=599) reporting any past six-month drug use from a Level-1 ED; participants were assessed at baseline and four biannual follow-ups. Participants self-reported validated measurements of peer/parental behaviors, violence/crime exposure, drug use self-efficacy, and alcohol use. Research staff diagnosed DUD with nine substances, post-traumatic stress disorder (PTSD), and major depressive disorder (MDD). We used repeated measures logistic regression models with person-level covariate means, and person-mean-centered covariates, as separate variables, to separate within- and between-person covariate effects.
Results:
Among 2,630 assessments, 1,128 (42.9%) were DUD diagnoses; 21.7% were co-diagnoses with multiple drugs. Positive (aOR=0.81, 95%CI:[0.70, 0.94]) and negative (aOR=1.73, 95%CI:[1.45, 2.07]) peer behaviors related to DUD, primarily through between-person effects. Parental support (aOR=0.92, 95%CI:[0.83, 0.99]), community violence/crime (aOR=1.28, 95%CI:[1.14, 1.44]), PTSD/MDD diagnosis (aOR=1.36, 95%CI:[1.04, 1.79]), and alcohol use quantity (aOR=1.06, 95%CI:[1.02, 1.11]) were associated with DUD, showing primarily within-person effects. Other factors, such as interpersonal violence involvement (aOR=1.47, 95%CI:[1.21, 1.78]), showed both within- and between-person effects.
Conclusions:
DUD is prevalent in this population, and within-person changes in DUD are predictable. Within-person effects suggest the importance of addressing escalating alcohol use, enhancing parental support, crime/violence exposure, and other mental health diagnoses as part of DUD intervention.
Keywords: drug use disorder, longitudinal, alcohol, youth, emergency department
1. INTRODUCTION
Drug use disorders (DUDs) are among the most prevalent psychiatric disorders, and often have other psychiatric comorbidities (Compton et al., 2005; Grant et al., 2016). DUD is common among adolescents and emerging adults, with estimated past 12-month and lifetime prevalence of 8.3% and 14.2%, respectively, among those age 18–29 (Grant et al., 2016), and estimated past-12-month prevalence of 3.0% among those age 12–17 (U.S. DHHS, 2019). In addition, those with DUD are at higher risk of other negative outcomes including suicide (Wilcox et al., 2004), partner violence (Chermack et al., 2008), violence (Carter et al., 2015; Chermack et al., 2010), injury (Bernstein et al., 2014), and unemployment (Henkel, 2011). Much research has focused on risk factors for increased substance use, including increased peer (Marschall-Lévesque et al., 2014) and parental (Arria et al., 2012; Yule et al., 2013) substance use, lowered parental support (Goldstick et al., 2018b), increased interpersonal violence experience (Goldstick et al., 2018c), increased community violence exposure (Löfving-Gupta et al., 2018), and increased mental health symptoms (Shrier et al., 2003), but little has focused on distinguishing within- and between-person risk factors for DUD among youth.
Longitudinal data provides the opportunity to clarify covariate effects by determining whether changes in the covariate correspond to changes in the outcome (i.e., within-person effects), and/or whether the distribution of the covariate is different in those with higher vs. lower levels of the outcome (i.e., a between-person effects) In prevention research these two effects have different implications for intervention targets and content, and the importance of this distinction is recognized in many behavioral sciences (Curran and Bauer, 2011). This work focuses on distinguishing within- and between-person effects on DUD among adolescents and emerging adults entering an urban emergency department (ED), with particular emphasis on alcohol use as a predictor.
While some risk factors are well-understood, information is lacking on the distinction between within- and between-person effects on risk of DUD development. Several existing studies that directly target within- vs. between-person effects on substance use outcomes involve the analysis of daily data (Cook et al., 2019; Stevenson et al., 2019; Walters et al., 2018), often focused on estimating circumstantial differences (e.g., mood, settings, and use motives) and how those correspond to use levels on a given day. Some work has explicitly separated both within- and between-person effects on substance use (e.g., cannabis use disorder; Defoe et al., 2019) over broader time horizons, and with more comprehensive measures than are available in daily surveys, but examples are scarce. To our knowledge no such prior work focuses on ED-based populations, which are uniquely intervenable (Cunningham et al., 2009). The within/between-person distinction may provide insights for prevention efforts; specifically, factors showing between-person associations with DUD may indicate characteristics of individuals that could benefit from interventions, while factors showing within-person associations—i.e., where within-person changes correspond to changes in DUD—may suggest intervention content/foci.
Alcohol is the most commonly used substance in the United States (U.S. DHHS, 2019), including the most commonly used substance among adolescents and emerging adults (Johnston et al., 2019). In addition, alcohol is often consumed by youth prior to initiating with substances such as tobacco or marijuana (Barry et al., 2016), which raises questions about how changes in alcohol use coalesce with changes in other substance use.. Prior work from this study showed that transitions in alcohol use were frequent and predictable (Goldstick et al., 2019), that youth with high levels of anxiety/depression symptoms and alcohol use, also had more cannabis use (Goldstick et al., 2018a), and that there was variation in cannabis use frequency over time (Walton et al., 2017). Although informative, these prior papers did not parse out within- and between-subjects effects on DUD specifically, which is the focus of this paper. Determining whether alcohol shows a within-person association with DUD would determine whether data are consistent with the hypothesis that alcohol use is a catalyst for other risk behaviors such as DUD, or whether those with higher alcohol use simply have a higher propensity for other drug use (i.e., a between-person effect), which could suggest a separate, common, causal factor.
We used data from a 2-year prospective longitudinal study of youth recruited from an urban ED to study within-person changes in DUD diagnosis, and how those coalesce with within-person changes in social exposures, violence experience, community exposure, mental health symptoms, and alcohol use quantity, while also estimating between-person effects. In addition, we conducted descriptive network analysis of DUD diagnoses to describe the joint distribution of the nine drug use disorder diagnosis, and explore which drugs are central to within-person DUD comorbidities. Optimizing intervention opportunities (e.g., an ED visit) requires identifying key intervention content (within-person effects) and at-risk populations (between-person effects), which is the purpose of this work.
2. METHODS
2.1. Study Setting
Data for this study was collected during the Flint Youth Injury (FYI) Study (Cunningham et al., 2015) a prospective longitudinal study of the service needs of youth age 14–24 entering an urban ED and also report past-six-month drug use. Baseline enrollment for the FYI study was conducted in the Hurley Medical Center in Flint, Michigan from 12/2009 through 09/2011.
2.2. Study Procedures
Study recruitment occurred 7 days/week from 5am-2am. Study staff approached ED entrants age 14–24 presenting with assault injuries for screening and sequentially approached the next non-assault-injured arrival with the same gender and age group (14–17, 18–20, 21–24). Youth responding with any past-six-month illicit drug use or non-medical prescription drug use were eligible for the longitudinal study. Exclusion criteria were: presenting with sexual assault, suicidal ideation, child abuse, or inability to consent (e.g., due to medical incapacitation). In total, n=599 participants enrolled for the longitudinal study (349 assault injured at baseline), and were followed up at 6-, 12-, 18-, and 24-months post baseline (follow-up rates ranged from 83.7%−85.3%). Further details on study methods are available in prior publications (Roche et al., 2018). All study procedures were approved by IRBs at the University of Michigan and Hurley Medical Center.
2.3. Measures
At each biannual survey assessment, participants were measured on the primary outcome for this analysis—drug use disorder (DUD) diagnosis. With the exception of gender, race, and reason for ED visit, all measures listed below are time-varying.
2.3.1. Drug use disorder
At each assessment, staff made current DSM-IV diagnosis of dependence and/or abuse on nine substances—cannabis, cocaine, prescription stimulants, methamphetamine, inhalants, sedatives, hallucinogens, street opioids, and prescription opioids—using the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al., 2010). Participants diagnosed with abuse or dependence on any of the listed substances were coded as “Yes” for drug use disorder, and “No” otherwise. The outcome variable was current DUD diagnosis, measured at each of the five assessments.
2.3.2. Alcohol use and other mental health diagnoses
We measured alcohol use quantity using the Alcohol Use Disorder Identification Test (AUDIT-C) (Babor and Robaina, 2016), a three-item set of questions, which are summed to produce a 12 point scale. The MINI neuropsychiatric interview (Sheehan et al., 2010) provided DSM-IV diagnoses for current post traumatic stress disorder (PTSD) and current major depression disorder (MDD).
2.3.3. Peer behaviors
We used items from the Flint Adolescent Study (Zimmerman et al., 2002) to measure number of friends (1–5 scale; 1: None, 5: All) engaging in four positive behaviors (e.g., taking part in community activities; intend to attend college), and seven negative behaviors (e.g., friend substance use, fighting). We averaged each group of variables to produce two summary scores.
2.3.4. Parental and familial exposures
Scales from the Flint Adolescent Study measure family conflict (5 items, 1–4 scale; e.g., frequency of fighting within the family), and parental drug and alcohol use (4 items; 1–5 scale) (Zimmerman et al., 2000), with higher values indicating greater frequency. We measured parental support using the social support scale of Procidano & Heller, which measures six aspects of parental support (e.g., “I rely on my parents for moral support”) on a 1–5 scale. Each of the three scales was averaged separately to produce summary scores.
2.3.5. Peer, partner, and community violence
The modified conflict tactics scale (Straus et al., 1996) measured partner violence (13 items each for victimization and perpetration) and non-partner violence (13 items each for victimization and perpetration), which were each reduced to binary indicators (Yes/No) for both partner and non-partner violence. Due to substantial content overlap (resulting in collinearity), in the adjusted models, we combined all interpersonal violence (victim/aggressor, peer/partner) into a single binary measurement. We measured community violence and crime exposure using the five item “Things I’ve Seen and Heard” survey (Richters and Saltzman, 1990), which were averaged to produce one score.
2.3.6. Substance use self-efficacy
An adapted form of the Specific Event Drug and Alcohol Refusal Efficacy scale (Belgrave et al., 2004) measured substance use likelihood on a 5-point (1: “Not at all”, 5: “Extremely”) scale in eight circumstances. We summarized those measurements into two scales comprised of the average of three questions related to social pressure (e.g., “If someone made fun of me for not using”), and the average of five questions related to internal reasons (e.g., “If there were problems with my family”).
2.3.7. Demographics
Participants self-reported age, sex, and race based on items from the National Survey of Adolescent Health (Harris and Florey, 2003). Self-reported race was predominantly White or Black (>90%); thus we reduced it to a binary indicator of Black race.
2.4. Statistical Analysis
We began with descriptive analyses of the within-person DUD diagnoses comorbidity networks. We displayed frequencies of specific DUD diagnoses for each of the nine substances comprising the DUD outcome, and frequencies of joint diagnoses. To estimate dependencies between diagnoses we used an Ising network model (Van Borkulo et al., 2014), which has been used in prior literature to analyze clustering of substance use disorder symptoms (Rhemtulla et al., 2016). We used the Ising model to estimate associations between each binary diagnosis indicator, adjusted for each other node. To ensure network parsimony, network edges were penalized using an adaptation of the lasso penalty, which has the property of automatically shrinking small or overly variable (e.g., due to small cell sizes) associations to zero. We also reported centrality measures of the estimated association network including node strength, betweenness centrality, and local clustering coefficient.
We quantified within-person variability in both specific DUD diagnoses and in the covariates of interest. Specifically, we a) displayed changes over time in the rates of DUD, and the rates of new and persistent DUD diagnoses; and b) showed levels of within-person variation in each time-varying covariate, confirming their viability for establishing both within- and between-person effects. Next, we estimated unadjusted associations between each covariate and DUD with two sample comparisons and unadjusted odds ratios; we adjusted all confidence intervals for repeated measures using Huber-White standard errors.
Our key inferential target in this analysis was to de-couple within- and between-person covariate of DUD diagnosis. At a basic level, between-person effects suggest characteristics of individuals at highest risk for DUD, while within-person effects suggest potential targets for behavior change. Specifically—in linear models, the effect of a time-varying covariate on the response is a weighted average of the between- and within-group (person, in this case) effect, with the weight equal to the intra-class correlation (ICC) of the covariate, with analogous logic applying in logistic models; our goal was to estimate each effect separately. To accomplish that goal, we calculated both the person-level means for each time-varying-covariate and the within-person difference from that mean, and entered those as separate covariates; the coefficient for the former estimates the between-person effect, and the coefficient for the latter estimates the within-person effect (Curran and Bauer, 2011). This approach was used previously to study within-person changes in firearm carrying using these data (Sokol et al., 2020). While multi-level models are frequently used for such analysis, the same logic applies using other methods for adjusting for residual within-person correlation, such as GEE (Harter et al., 2019; Schunck, 2013); given the choice, we prefer GEE due to simpler interpretation and fewer unverifiable assumptions, as noted elsewhere (Hubbard et al., 2010). Person/time points where any covariates or the outcome were missing were excluded.
3. RESULTS
3.1. DUD Frequencies and Partial Correlation Networks
In total, 2,630 assessments were completed and 1,128 (42.9%) resulted in DUD diagnosis; 443 participants (74.0%) were diagnosed with DUD at ≥1 assessment. Table 1 shows the frequency of each individual DUD diagnosis, and frequencies of co-diagnosis with every pair of drugs. The most frequent diagnosis was cannabis use disorder (n=1,050) and the least frequent was inhalant use disorder (n=2); the most common co-diagnosis was cannabis and sedatives (n=112). Over three quarters of diagnoses (n=883; 78.3%) were with a single substance; among those, cannabis (n=838), was the most common. Among those with multiple DUDs, 161 (14.3%) had two diagnoses, and 84 (7.4%) had three; the most common triplicate was cannabis/sedatives/prescription opioids (n=29).
Table 1:
Drug use disorder diagnosis and co-diagnosis counts in the FYI study, aggregated across follow-ups
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1 Cannabis | 1050 | ||||||||
| 2 Cocaine | 39 | 58 | |||||||
| 3 Rx Stimulant | 18 | 1 | 25 | ||||||
| 4 Methamphetimine | 1 | 0 | 0 | 4 | |||||
| 5 Inhalant | 1 | 0 | 0 | 0 | 2 | ||||
| 6 Sedatives | 112 | 11 | 6 | 1 | 1 | 142 | |||
| 7 Hallucinogen | 14 | 5 | 4 | 0 | 0 | 8 | 27 | ||
| 8 Illicit Opioids | 10 | 8 | 0 | 3 | 0 | 4 | 3 | 28 | |
| 9 Rx Opioids | 83 | 13 | 11 | 0 | 0 | 42 | 8 | 6 | 121 |
Note 1: Diagonal entries are the total number of abuse or dependence diagnoses with each substance
Note 2: Out of 2,630 MINI diagnostic interviews, 84 (3.2%) resulted in abuse/dependence diagnoses on three substances. Among those 84, the most common combination was Cannabis/Sedative/Rx Opioid (29; 34.5%), followed by Cannabis/Cocaine/Sedative (8; 9.5%), Cannabis/Rx Stimulants (7; 8.3%), and Cannabis/Cocaine/Rx Opioids (5; 6.0%); all others occurred <5 times.
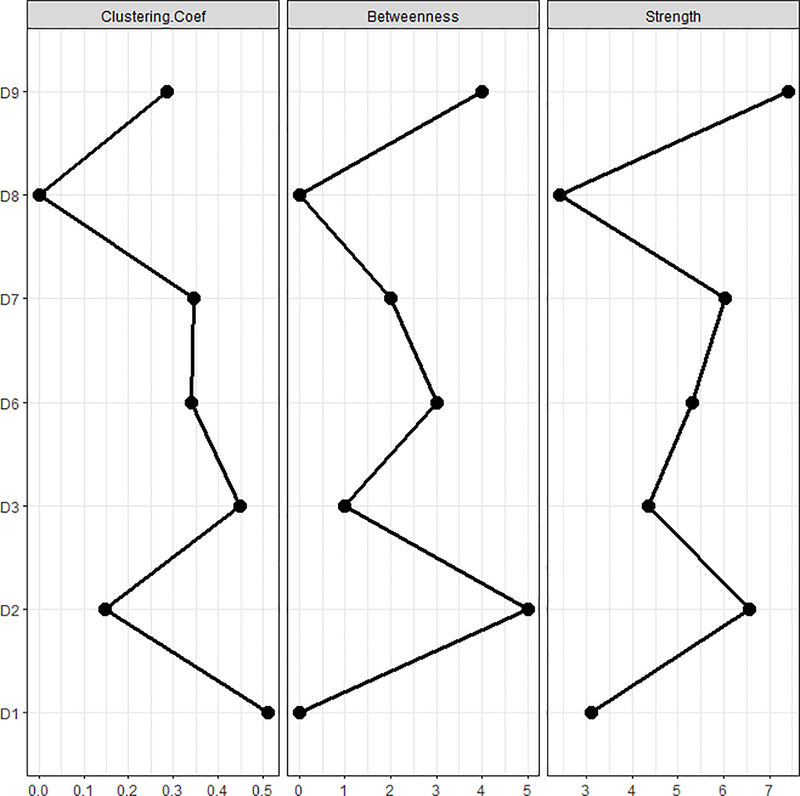
Figure 1 shows the network of partial correlations between diagnoses. Cannabis showed the largest weighted clustering coefficient, meaning that its connections are often connected to one another. Thus, although Cannabis use disorder often occurs in isolation, when it co-occurs with another DUD, there are often >1. Cocaine and prescription opioids both showed the largest node strength (the sum of the edge weights) suggesting those two substances collectively show the largest associations with the other nodes. Betweenness centrality, which measures the tendency of a node to bridge other pairs of nodes, showed similar results, suggesting that cocaine and prescription opioids are key to connecting nodes within the DUD comorbidity network. The lack of edge between street opioid use disorder and prescription opioid use disorder is an illustration of the lasso regularization; though the two are associated, the small cell size (n=6) corresponded to high uncertainty. Inhalants and methamphetamine were excluded from this analysis due to low frequencies (<5).
Figure 1:

Network of drug use disorder diagnoses
D1: Cannabis
D2: Cocaine
D3: Stimulant (Rx)
D4: Methamphetimine
D5: Inhalants
D6: Sedatives
D7: Hallucinogens
D8: Illicit Opioids
D9: Opioids (Rx)
Note 1: line thickness indicates the strength of relationship between co-occurring diagnoses
Note 2: Inhalants and methamphetimines were excluded from this analysis due to very low frequencies (<5 total diagnoses)
3.2. Descriptive Analysis of within-person changes in DUD diagnoses and covariates
Figure 2 shows changes over time in the prevalence of DUD diagnoses, and the rates of new and persistent DUD diagnoses. Diagnosis rates were highest at baseline (57.1%), but remained above 34% across assessments. Among those diagnosed, between 22.6%−31.1% had no DUD diagnosis at the prior assessment, showing within-person variability in diagnoses. Table 2 shows total, within-, and between-person variation in each time-varying covariate. All time-varying-covariates show ICCs between 0.32 and 0.67, suggesting both within- and between-person variability are substantial.
Figure 2:
Drug use disorder diagnosis counts across time points.
Note: “Persistent DUD” refers to diagnoses at consecutive time points; “New DUD” refers to a transition from No DUD to DUD at two consecutive time points.
a: Percentages are out of the total number of MINI interviews
b: Percentages are out of the number of DUD diagnoses
Table 2:
Within- and between-person variation in time-varying predictors
| Range | σ2 (total) | σ2 (between) | σ2 (within) | ICC | |
|---|---|---|---|---|---|
| Peer Behaviors | |||||
| Positive Behaviors | 1–5 | 0.52 | 0.29 | 0.23 | 0.55 |
| Negative Behaviors | 1–5 | 0.45 | 0.29 | 0.16 | 0.63 |
| Parental/Familial | |||||
| Parental Drug/Alc Use | 1–5 | 0.56 | 0.36 | 0.19 | 0.65 |
| Parental Support | 1–5 | 1.72 | 1.15 | 0.57 | 0.67 |
| Family Conflicta | 1–5 | 0.60 | 0.35 | 0.25 | 0.59 |
| Violence/Crime Exposure | |||||
| Partner Victimizationb | 0–1 | 0.24 | 0.11 | 0.14 | 0.44 |
| Partner Aggressionb | 0–1 | 0.22 | 0.10 | 0.12 | 0.47 |
| Non-Partner Victimizationb | 0–1 | 0.23 | 0.07 | 0.16 | 0.32 |
| Non-Partner Aggressionb | 0–1 | 0.23 | 0.09 | 0.14 | 0.38 |
| Community Violence/Crime | 1–5 | 0.83 | 0.36 | 0.47 | 0.43 |
| Alcohol, Mental Health, Self-Efficacy | |||||
| Alcohol Use (AUDIT-C) | 0–12 | 6.82 | 4.01 | 2.81 | 0.59 |
| MDE Diagnosisb | 0–1 | 0.10 | 0.04 | 0.06 | 0.43 |
| PTSD Diagnosisb | 0–1 | 0.05 | 0.02 | 0.04 | 0.36 |
| Social Self-Efficacy | 0–5 | 0.22 | 0.10 | 0.12 | 0.47 |
| Internal Self-Efficacy | 0–5 | 0.62 | 0.36 | 0.26 | 0.58 |
14 missing values
These measures are binary (Yes/No; although, correlation is not an ideal measure for binary measurements, the ICC is reported to a rough quantification of the within- and between-person variability in these measures across the study period.
ICC: Intra-class correlation (within-person correlation, in this case)
3.3. Unadjusted covariate effects on DUD
Unadjusted covariate effects on DUD are shown in Table 3. DUD was more common among males, and negatively associated with age, and was not associated with race or reason for baseline ED visit. Fewer positive peer affiliations, and more negative peer affiliations, both corresponded to higher rates of DUD. Greater parent substance use, family conflict, and less parental support, were risk factors for DUD. Peer and partner violence, as victim or aggressor, was associated with DUD, as was greater community violence/crime rates. Greater alcohol consumption, and other mental health diagnoses (PTSD, MDD) were positively associated with DUD. Tendency to cope with social pressures, and with other internal pressures, by using substances were both associated with higher risk of DUD.
Table 3:
Unadjusted odds ratios—total, between-, and within-person—quantifying the association between each predictor and DUD diagnosis.
| Total (N=2,630) | DUD (N=1,128) | No DUD (N=1,502) | OR (95% CI) (Combined) | |
|---|---|---|---|---|
| Demographics | ||||
| Age | 21.0 (2.5) | 20.8 (2.6) | 21.1 (2.5) | 0.9 (0.9, 1.0) |
| Male Gender | 1500 (57.0%) | 726 (64.4%) | 774 (51.5%) | 1.7 (1.4, 2.0) |
| Black race | 1588 (60.4%) | 648 (57.4%) | 940 (62.6%) | 0.8 (0.6, 1.0) |
| Violent Injury At Baseline | 1532 (58.3%) | 681 (60.4%) | 851 (56.7%) | 1.2 (0.9, 1.5) |
| Peer Behaviors | ||||
| Positive Behaviors | 2.1 (0.7) | 2.1 (0.7) | 2.2 (0.7) | 0.8 (0.7, 0.9) |
| Negative Behaviors | 2.0 (0.7) | 2.2 (0.7) | 1.8 (0.6) | 3.5 (2.9, 4.2) |
| Parental/Familial | ||||
| Parental Drug/Alcohol Use | 1.5 (0.7) | 1.6 (0.9) | 1.4 (0.6) | 1.5 (1.3, 1.7) |
| Parental Support | 3.1 (1.3) | 3.0 (1.3) | 3.2 (1.3) | 0.9 (0.8, 1.0) |
| Family Conflicta | 1.8 (0.8) | 1.9 (0.8) | 1.6 (0.7) | 1.6 (1.4, 1.9) |
| Violence/Crime Exposure | ||||
| Partner Victimizationb | 10–8 (40.6%) | 587 (52.0%) | 481 (32.0%) | 2.3 (1.9, 2.8) |
| Partner Aggressionb | 880 (3 3.5%) | 497 (44.1%) | 383 (25.5%) | 2.3 (1.9, 2.8) |
| Non-Partner Victimizationb | 967 (36.8%) | 560 (49.6%) | 407 (27.1%) | 2.7 (2.2, 3.2) |
| Non-Partner Aggressionb | 962 (36.6%) | 577 (51.2%) | 385 (25.6%) | 3.0 (2.5, 3.7) |
| Community Violence/Crime | 1.4 (0.9) | 1.7 (0.9) | 1.2 (0.9) | 1.8 (1.6, 2.0) |
| Alcohol, Mental Health, Self-Efficacy | ||||
| Alcohol Use (aUDIT-C) | 1.8 (2.6) | 2.5 (3.0) | 1.3 (2.1) | 1.2 (1.2, 1.2) |
| PTSD Diagnosisb | 153 (5.8%) | 101 (9.0%) | 52 (3.5%) | 2.7 (1.9, 4.0) |
| MDE Diagnosisb | 288 (11.0%) | 176 (15.6%) | 112 (7.5%) | 2.3 (1.7, 3.1) |
| Social Self-Efficacy | 1.1 (0.5) | 1.3 (0.6) | 1.1 (0.3) | 3.3 (2.3, 4.7) |
| Internal Self-Efficacy | 1.5 (0.8) | 1.8 (0.9) | 1.3 (0.5) | 3.3 (2.7, 3.9) |
14 missing values
These are binary measurements, and so the entries are total “Yes”s with percent out of the total
DUD: Drug use disorder
For numeric variables, the entries are means with standard deviations in parentheses; for Yes/No variables, the entries are the number reporting “Yes”, with the percent out of the total in parentheses.
3.4. Adjusted covariate effects on DUD
The models showing covariate effects on DUD risk, adjusted for demographics, peer/parental behaviors, violence exposure, mental health, substance use self-efficacy, and alcohol use are shown in Table 4. Due to content overlap and collinearity, all partner/peer violence, both as aggressor or victim, was collapsed into a single indicator, as were the indicators for PTSD and MDD diagnosis. The final model had an area of the ROC curve of 0.81, suggesting good discriminatory power. Model calibration was verified graphically in Supplemental Figure 1, which shows good agreement between observed and expected DUD prevalence at each decile of the model-predicted risks.
Table 4:
Adjusted estimates of person-level and time-varying covariate effects on drug use disorder
| Model 1 |
Model 2 |
||
|---|---|---|---|
| AOR (Combined) | AOR (Between) | AOR (Within) | |
| Demographics | |||
| Age | 0.95 (0.91, 0.99) | 0.96 (0.91, 1.01) | 0.89 (0.78, 1.01) |
| Gender (ref=Female) | 1.87 (1.48, 2.37) | 1.80 (1.40, 2.32) | n/a |
| Black race (ref=Other) | 0.97 (0.76, 1.24) | 1.02 (0.78, 1.33) | n/a |
| Violent Injury At Baseline | 1.01 (0.79, 1.27) | 0.92 (0.72, 1.17) | n/a |
| Peer Behaviors | |||
| Positive Behaviors | 0.81 (0.70, 0.94) | 0.64 (0.48, 0.82) | 1.00 (0.82, 1.23) |
| Negative Behaviors | 1.73 (1.45, 2.07) | 3.14 (2.25, 4.38) | 1.13 (0.90, 1.43) |
| Parental/Familial | |||
| Parental Drug/Alcohol Use | 1.10 (0.95, 1.28) | 1.02 (0.81, 1.27) | 1.21 (0.96, 1.52) |
| Parental Support | 0.92 (0.83, 0.99) | 0.98 (0.86, 1.12) | 0.87 (0.77, 0.98) |
| Family Conflicta | 0.94 (0.81, 1.10) | 0.90 (0.67, 1.21) | 1.02 (0.82, 1.26) |
| Violence/Crime Exposure | |||
| Any Interpersonal Violenceb | 1.47 (1.21, 1.78) | 1.94 (1.22, 3.10) | 1.35 (1.07, 1.70) |
| Community Violence/Crime | 1.28 (1.14, 1.44) | 1.07 (0.83, 1.37) | 1.35 (1.16, 1.59) |
| Alcohol Use, Mental Health, Self-Effiicacy | |||
| Alcohol Use (AUDIT-C) | 1.06 (1.02, 1.11) | 0.99 (0.92, 1.06) | 1.07 (1.01, 1.13) |
| PTSD/MDE Diagnosisb | 1.36 (1.04, 1.79) | 0.82 (0.44, 1.54) | 1.41 (1.00, 1.99) |
| Social Drug Use Self-Efficacy | 1.25 (0.90, 1.74) | 1.59 (1.00, 2.51) | 1.17 (0.75, 1.83) |
| Internal Drug Use Self-Efficacy | 1.90 (1.60, 2.25) | 3.34 (2.45, 4.54) | 1.40 (1.14, 1.73) |
14 missing values
Combines aggression and victimization, and both peer and partner violence
AOR: Adjusted odds ratio; MDE: Major depressive episode; PTSD: Post-traumatic stress disorder
The effects of peer behaviors—both positive and negative—on DUD both appear to be attributable to between-person effects. Specifically, those with DUD have higher average levels of negative peer affiliations, and lower average levels of positive peer affiliations, but within-person changes in those factors are not associated with within-person changes in DUD. Within-person changes in parental support corresponded to changes in DUD, but average levels of parental support were not different between those with and without DUD. Parental substance use and family conflict were unassociated with DUD in adjusted analyses. As in the unadjusted models, younger age, and male gender, were associated with DUD.
Violence experience showed both within- and between-person effects, meaning both that those with higher overall violence tendency have higher risk of DUD, and when an individual’s violence involvement changes, their DUD risk changes (within person effect). The risk-enhancing effect of community violence/crime was primarily attributable to within-person changes in community violence/crime exposure, and not between-person differences.
The effects of alcohol use quantity and comorbid mental health diagnosis were primarily attributable to within-person changes in those factors, not between-person differences. Effects of substance use self-efficacy related to social pressures (e.g., ability to abstain in the face of peer pressure) were due to between-person differences, while those related to internal reasons (e.g., abstaining when worried about a personal problem) showed both within- and between-person effects.
4. DISCUSSION
We showed DUD was prevalent in this population, there was substantial within-person variability in DUD over the course of 24-months following an ED visit among, and that those changes were associated with between- and within-person differences. Our analysis confirms much of what is known about the importance of peer behaviors, parental/family environment, violence exposure, alcohol use, and mental health symptoms in the epidemiology of DUD, but adds further nuance in terms of sources of those effects. Between-person effects suggesting sub-populations in greatest need of DUD treatment include those with peer exposures and trouble handling social pressure to using substances. Within-person effects suggest key content to integrate into interventions include increasing parental support, addressing community violence exposure, reducing alcohol use, and providing support for those with mental health disorders.
DUD profiles in this population were varied and involved several substances. Cannabis use disorder was the most common diagnosis, and was the only diagnosis in a large majority of positive DUD cases, but when it did co-occur with other DUDs, it was often multiple substances. DUD diagnoses occurred for all nine substances examined, and cocaine, sedative, hallucinogen, non-prescription opioid, and prescription opioid use disorders were each diagnosed in over 1% of interviews. In addition, drug use disorder co-diagnosis occurred in over 1 in 5 interviews. Cocaine and prescription opioids were the lynchpins of the co-diagnosis network, showing the largest collective associations with other DUD diagnoses, and most often acting as the intermediary between other connections; this finding heightens concern given the risk for overdose (Gladden et al., 2019).
We found that the association between alcohol use quantity and DUD was attributable to a within-, and not between-person, effect. This finding is consistent with other work suggesting that alcohol use catalyzes changes in other substance use behaviors (Kirby and Barry, 2012). One implication is that changes in drinking quantity—which may be more easily observed and measured outside of a research study, due to its legality among ages 21 and older, and acceptability in everyday culture—may effectively proxy changes in DUD risk. Another is that intervening and reducing drinking rates may correspond to reduced risk of DUD and its accompanying risks. Previous findings showing that transitions in alcohol use are also frequent and predictable(Goldstick et al., 2019) enhance its practicality as a time-varying gage of DUD risk.
Our results show that both peer delinquency, peer positive behaviors, and substance use self-efficacy in the face of social pressure are associated with the development of DUD. Associations between substance use and that of peers is likely explained by a combination of peer influences (Tucker et al., 2014) and selecting peers with similar substance use behavior (De La Haye et al., 2015; Knecht et al., 2010). Relatedly, evidence suggests youth social networks are assortative with regard to drinking (Goodreau et al., 2009), drug use (Poulin et al., 2011), and general delinquency (Knecht et al., 2010). Within-person changes in exposure to positive and negative peer behaviors did not correspond to changes in DUD in this population, though the person-level average exposure to each did, suggesting a between-person effect. The fact that peer-related social factors produced a between-person, and not a within-person, effect supports the idea of peer selection rather than peer influence in this population, and highlights affiliates of delinquent peers as a high-need population.
Protective effects of parental support and lower community violence/crime being primarily attributable to within-person effects gives support to DUD intervention content centered on enhancing promotive factors. In addition to community-level interventions such as neighborhood greening to reduce youth violence (Heinze et al., 2018), resiliency theory posits that youth can reduce poor outcomes following risk exposure by promoting coping skills and self-efficacy, such as through cultivating parental social support and community involvement (Zimmerman, 2013). This is especially important because self-efficacy for avoiding drug use in response to internalizing symptoms was also identified as both a within- and between-person risk factor, suggesting both that those who use drugs to cope are a particularly high need population, and that such a resiliency-based approach may be beneficial for them. Combining multi-level approaches (individual, family, community) may be particularly beneficial in this regard (Heinze et al., 2016).
Our results showed that interpersonal violence involvement was both a within- and between-person risk factor for DUD. The between-person effect here highlights those experiencing interpersonal violence as a high need population, and is consistent with DUD and violence involvement having shared causes in this population. Dual interventions have been successful at jointly reducing violence and substance use consequences in similar populations (Cunningham et al., 2012; Walton et al., 2010), which is consistent with our finding. The presence of a within-person effect is also consistent with notions of the stress and mental health symptoms resulting from interpersonal violence (Beydoun et al., 2012; Krause et al., 2008) contributing to substance use, which is also consistent with the PTSD/MDD co-diagnosis findings. Thus, it is reasonable to expect that interventions focusing on concomitant violence exposure and involvement, other diagnoses such as PTSD, could produce downstream effects on DUD incidence.
Our work carries some limitations. This was a single-site study of youth who report drug use in Flint, MI. Flint has comparable demographics to other rust belt cities, but our findings should be taken in the context of this as a high-risk sample. This is a critical study population, but studies of DUD transitions in the general population would complement our findings. Second, substance use had already been initiated by study baseline and data on substance use prior to baseline would enhance the argument that between-person factors are akin to person-level traits, while within-person factors are modifiable intervention targets. Our study features high follow-up rates and comprehensive drug use measures, but data from pre-initiation would improve our inference. Third, collapsing all DUD outcomes into a single outcome, which was for parsimony and to avoid further complication of an already complex analysis, does limit some implications. For example, different substances have different onset ages, which may complicate interpretation of certain covariate effects, like the finding that younger age was associated with lower DUD risk, which may relate to a majority of diagnoses involving cannabis. Future studies with specificity to particular substances will further clarify the relationships found here.
Notwithstanding study limitations, we have presented characteristics of DUD diagnoses, as well as rates and factors associated with within-person changes in a critical study population. We found that DUD was common in this population, is most frequently involving cannabis, and that cocaine and prescription opioids are central to the polysubstance use disorder network, raising concerns about overdose risk in this population. Youth with more delinquent peer affiliations, more interpersonal violence, and lower substance use avoidance self-efficacy are important candidates for prevention. Changing levels of interpersonal violence involvement, depression/PTSD symptoms, community violence exposure, and internalizing strategies for substance use avoidance—or promoting resiliency in those factors when changing exposure is not possible—could improve prevention programs. In addition, interrupting increasing trajectories of alcohol use may help optimize the opportunity for DUD prevention afforded by an ED visit.
Supplementary Material
Highlights.
Drug use disorder (DUD) is common in this population, many involving >1 drugs (22%)
Several factors explained differences in DUD—some within- and some between-person
Within-person changes in alcohol use quantity correspond to changes in DUD
Peer behaviors and related factors affect DUD through between-person effects
Parent support, violence exposure, and mental health show within-person effects
Acknowledgements:
This work was funded by R03 AA025449 and R01 DA024646. We thank the FYI study staff at the University of Michigan and the Hurley Medical Center for making this work possible.
Footnotes
Conflict of Interest
The authors have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Arria AM, Mericle AA, Meyers K, & Winters KC (2012). Parental substance use impairment, parenting and substance use disorder risk. Journal of substance abuse treatment, 43(1), 114–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, & Robaina K (2016). The Alcohol Use Disorders Identification Test (AUDIT): A review of graded severity algorithms and national adaptations. The International Journal of Alcohol and Drug Research, 5(2), 17–24. [Google Scholar]
- Barry AE, King J, Sears C, Harville C, Bondoc I, & Joseph K (2016). Prioritizing alcohol prevention: Establishing alcohol as the gateway drug and linking age of first drink with illicit drug use. Journal of school health, 86(1), 31–38. [DOI] [PubMed] [Google Scholar]
- Belgrave FZ, Reed MC, Plybon LE, & Corneille M (2004). The impact of a culturally enhanced drug prevention program on drug and alcohol refusal efficacy among urban African American girls. Journal of Drug Education, 34(3), 267–279. [DOI] [PubMed] [Google Scholar]
- Bernstein J., Bernstein E., Belanoff C., Cabral HJ., Babakhanlou Chase H., Derrington TM., … Jacobs H (2014). The association of injury with substance use disorder among women of reproductive age: an opportunity to address a major contributor to recurrent preventable emergency department visits? Academic emergency medicine, 21(12), 1459–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beydoun HA, Beydoun MA, Kaufman JS, Lo B, & Zonderman AB (2012). Intimate partner violence against adult women and its association with major depressive disorder, depressive symptoms and postpartum depression: a systematic review and meta-analysis. Social science & medicine, 75(6), 959–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter PM, Walton MA, Roehler DR, Goldstick J, Zimmerman MA, Blow FC, & Cunningham RM (2015). Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics, 135(5), 805–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chermack ST, Grogan-Kaylor A, Perron BE, Murray RL, De Chavez P, & Walton MA (2010). Violence among men and women in substance use disorder treatment: A multi-level event-based analysis. Drug and alcohol dependence, 112(3), 194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chermack ST, Murray RL, Walton MA, Booth BA, Wryobeck J, & Blow FC (2008). Partner aggression among men and women in substance use disorder treatment: correlates of psychological and physical aggression and injury. Drug and alcohol dependence, 98(1–2), 35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, & Grant BF (2005). Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry, 66(6), 677–685. [DOI] [PubMed] [Google Scholar]
- Cook MA, Newins AR, Dvorak RD, & Stevenson BL (2019). What about this time? Within-and between-person associations between drinking motives and alcohol outcomes. Experimental and clinical psychopharmacology. [DOI] [PubMed] [Google Scholar]
- Cunningham R, Knox L, Fein J, Harrison S, Frisch K, Walton M, … Hargarten SW (2009). Before and after the trauma bay: the prevention of violent injury among youth. Annals of emergency medicine, 53(4), 490–500. [DOI] [PubMed] [Google Scholar]
- Cunningham RM, Carter PM, Ranney M, Zimmerman MA, Blow FC, Booth BM, … Walton MA (2015). Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA pediatrics, 169(1), 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Chermack ST, Zimmerman MA, Shope JT, Bingham CR, Blow FC, & Walton MA (2012). Brief motivational interviewing intervention for peer violence and alcohol use in teens: one-year follow-up. Pediatrics, 129(6), 1083–1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual review of psychology, 62, 583–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De La Haye K, Green HD, Pollard MS, Kennedy DP, & Tucker JS (2015). Befriending risky peers: factors driving adolescents’ selection of friends with similar marijuana use. Journal of youth and adolescence, 44(10), 1914–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Defoe IN, Khurana A, Betancourt LM, Hurt H, & Romer D (2019). Disentangling longitudinal relations between youth cannabis use, peer cannabis use, and conduct problems: developmental cascading links to cannabis use disorder. Addiction, 114(3), 485–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gladden RM, O’Donnell J, Mattson CL, & Seth P (2019). Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine—25 states, July–December 2017 to January–June 2018. Morbidity and Mortality Weekly Report, 68(34), 737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Bohnert KM, Davis AK, Bonar EE, Carter PM, Walton MA, & Cunningham RM (2018). Dual trajectories of depression/anxiety symptoms and alcohol use, and their implications for violence outcomes among drug-using urban youth. Alcohol and alcoholism, 53(6), 659–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Heinze J, Ngo Q, Hsieh H-F, Walton MA, Cunningham RM, & Zimmerman MA (2018). Perceived peer behavior and parental support as correlates of marijuana use: The role of age and gender. Substance use & misuse, 53(3), 521–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Heinze JE, Stoddard SA, Cunningham RM, & Zimmerman MA (2018). Age-Specific Associations Between Violence Exposure and Past 30 Day Marijuana and Alcohol Use. Journal of research on adolescence, 29(2), 480–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstick JE, Walton MA, Bohnert AS, Heinze JE, & Cunningham R (2019). Predictors of alcohol use transitions among drug-using youth presenting to an urban emergency department. PloS one, 14(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodreau SM, Kitts JA, & Morris M (2009). Birds of a feather, or friend of a friend? Using exponential random graph models to investigate adolescent social networks. Demography, 46(1), 103–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, … Huang B (2016). Epidemiology of DSM-5 drug use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA psychiatry, 73(1), 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris K, & Florey F (2003). The national longitudinal study of adolescent health: Research design. Retrieved from http://www.cpc.unc.edu/projects/addhealth/design
- Harter M, Contzen N, & Inauen J (2019). The role of social identification for achieving an open-defecation free environment: A cluster-randomized, controlled trial of Community-Led Total Sanitation in Ghana. Journal of environmental psychology, 66, 101360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinze JE, Krusky Morey A, Vagi KJ, Reischl TM, Franzen S, Pruett NK, … Zimmerman MA (2018). Busy Streets Theory: The Effects of Community engaged Greening on Violence. American journal of community psychology, 62(1–2), 101–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinze JE, Reischl TM, Bai M, Roche JS, Morrel-Samuels S, Cunningham RM, & Zimmerman MA (2016). A Comprehensive Prevention Approach to Reducing Assault Offenses and Assault Injuries among Youth. Prevention Science, 17(2), 167–176. doi: 10.1007/s11121-015-0616-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henkel D (2011). Unemployment and substance use: a review of the literature (1990–2010). Current drug abuse reviews, 4(1), 4–27. [DOI] [PubMed] [Google Scholar]
- Hubbard AE, Ahern J, Fleischer NL, Van der Laan M, Satariano SA, Jewell N, … Satariano WA (2010). To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiology, 467–474. [DOI] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick M. E. J. I. f. S. R. (2019). Monitoring the Future National Survey Results on Drug Use, 1975–2018: Overview, Key Findings on Adolescent Drug Use. Institute for Social Research. [Google Scholar]
- Kirby T, & Barry AE (2012). Alcohol as a gateway drug: a study of US 12th graders. Journal of School Health, 82(8), 371–379. [DOI] [PubMed] [Google Scholar]
- Knecht A, Snijders TA, Baerveldt C, Steglich CE, & Raub W (2010). Friendship and delinquency: Selection and influence processes in early adolescence. Social Development, 19(3), 494–514. [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, & Dutton MA (2008). Avoidant coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. Journal of traumatic stress, 21(1), 83–90. [DOI] [PubMed] [Google Scholar]
- Löfving-Gupta S, Willebrand M, Koposov R, Blatný M, Hrdlička M, Schwab-Stone M, & Ruchkin V (2018). Community violence exposure and substance use: cross-cultural and gender perspectives. European Child & Adolescent Psychiatry, 27(4), 493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschall-Lévesque S, Castellanos-Ryan N, Vitaro F, & Séguin JR (2014). Moderators of the association between peer and target adolescent substance use. Addictive behaviors, 39(1), 48–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulin F, Kiesner J, Pedersen S, & Dishion TJ (2011). A short-term longitudinal analysis of friendship selection on early adolescent substance use. Journal of adolescence, 34(2), 249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhemtulla M, Fried EI, Aggen SH, Tuerlinckx F, Kendler KS, & Borsboom D (2016). Network analysis of substance abuse and dependence symptoms. Drug and alcohol dependence, 161, 230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richters JE, & Saltzman W (1990). Survey of exposure to community violence: Self-report version: JE Richters. [Google Scholar]
- Roche J, Clery M, Carter PM, Dora-Laskey A, Walton MA, Ngo Q, & Cunningham RM (2018). Tracking Assault injured, Drug using Youth in Longitudinal Research: Follow up Methods. Academic Emergency Medicine. doi:| 10.1111/acem.13495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schunck R (2013). Within and between estimates in random-effects models: Advantages and drawbacks of correlated random effects and hybrid models. The Stata Journal, 13(1), 65–76. [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, … Wilkinson B (2010). Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). The Journal of clinical psychiatry. [DOI] [PubMed] [Google Scholar]
- Shrier LA, Harris SK, Kurland M, & Knight JR (2003). Substance use problems and associated psychiatric symptoms among adolescents in primary care. Pediatrics, 111(6), e699–e705. [DOI] [PubMed] [Google Scholar]
- Sokol RL, Carter PM, Goldstick J, Miller AL, Walton MA, Zimmerman MA, & Cunningham RM (2020). Within-person variability in firearm carriage among high-risk youth. American journal of preventive medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson BL, Dvorak RD, Kramer MP, Peterson RS, Dunn ME, Leary AV, & Pinto D (2019). Within-and between-person associations from mood to alcohol consequences: The mediating role of enhancement and coping drinking motives. Journal of abnormal psychology, 128(8), 813. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of family issues, 17(3), 283–316. [Google Scholar]
- Tucker JS, de la Haye K, Kennedy DP, Green HD Jr, & Pollard MS (2014). Peer influence on marijuana use in different types of friendships. Journal of Adolescent Health, 54(1), 67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2019). Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19–5068, NSDUH Series H-54). Rockville, MD: Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Van Borkulo CD, Borsboom D, Epskamp S, Blanken TF, Boschloo L, Schoevers RA, & Waldorp LJ (2014). A new method for constructing networks from binary data. Scientific reports, 4(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KJ, Simons JS, & Simons RM (2018). Self-control demands and alcohol-related problems: Within-and between-person associations. Psychology of Addictive Behaviors, 32(6), 573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, & Cunningham RM (2010). Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: a randomized controlled trial. Jama, 304(5), 527–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Epstein-Ngo Q, Carter PM, Zimmerman MA, Blow FC, Buu A, … Cunningham RM (2017). Marijuana use trajectories among drug-using youth presenting to an urban emergency department: Violence and social influences. Drug Alcohol Depend, 173, 117–125. doi: 10.1016/j.drugalcdep.2016.11.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, & Caine ED (2004). Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug and alcohol dependence, 76, S11–S19. [DOI] [PubMed] [Google Scholar]
- Yule AM, Wilens TE, Martelon MK, Simon A, & Biederman J (2013). Does exposure to parental substance use disorders increase substance use disorder risk in offspring? A 5 year follow up study. The American Journal on Addictions, 22(5), 460–465. [DOI] [PubMed] [Google Scholar]
- Zimmerman MA (2013). Resiliency theory: A strengths-based approach to research and practice for adolescent health. In: Sage Publications Sage CA: Los Angeles, CA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman MA, Caldwell CH, & Bernat DH (2002). Discrepancy Between Self Report and School Record Grade Point Average: Correlates With Psychosocial Outcomes Among African American Adolescents 1. Journal of Applied Social Psychology, 32(1), 86–109. [Google Scholar]
- Zimmerman MA, Ramirez Valles J, Zapert KM, & Maton KI (2000). A longitudinal study of stress buffering effects for urban African American male adolescent problem behaviors and mental health. Journal of community psychology, 28(1), 17–33. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.