Abstract
Vascular contributions to cognitive impairment and dementia (VCID) are a common cause of cognitive decline, yet limited therapies exist. This cerebrovascular disease results in neurodegeneration via acute, chronic, local, and systemic mechanisms. The etiology of VCID is complex, with a significant impact from atherosclerosis. Risk factors including hypercholesterolemia and hypertension promote intracranial atherosclerotic disease and carotid artery stenosis (CAS), which disrupt cerebral blood flow and trigger ischemic strokes and VCID. Apolipoprotein E (APOE) is a cholesterol and phospholipid carrier present in plasma and various tissues. APOE is implicated in dyslipidemia and Alzheimer disease (AD); however, its connection with VCID is less understood. Few experimental models for VCID exist, so much of the present information has been drawn from clinical studies. Here, we review the literature with a focus on the clinical aspects of atherosclerotic cerebrovascular disease and build a working model for the pathogenesis of VCID. We describe potential intermediate steps in this model, linking cholesterol, atherosclerosis, and APOE with VCID. APOE4 is a minor isoform of APOE that promotes lipid dyshomeostasis in astrocytes and microglia, leading to chronic neuroinflammation. APOE4 disturbs lipid homeostasis in macrophages and smooth muscle cells, thus exacerbating systemic inflammation and promoting atherosclerotic plaque formation. Additionally, APOE4 may contribute to stromal activation of endothelial cells and pericytes that disturb the blood-brain barrier (BBB). These and other risk factors together lead to chronic inflammation, atherosclerosis, VCID, and neurodegeneration. Finally, we discuss potential cholesterol metabolism based approaches for future VCID treatment.
Keywords: cholesterol, atherosclerosis, APOE, vascular dementia, inflammation, glia, macrophage
Introduction
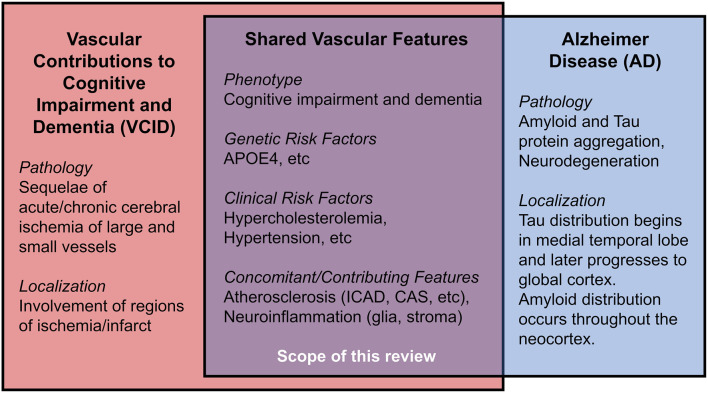
Vascular contributions to cognitive impairment and dementia (VCID) are defined by cognitive impairment secondary to acute and/or chronic cerebral ischemia and encompass the classical term, vascular dementia (Gorelick et al., 2011; Iadecola et al., 2019). VCID is the most common form of secondary neurodegeneration worldwide; one out of six people with dementia have VCID (van der Flier and Scheltens, 2005). The four subtypes of VCID are: (1) post-stroke, manifesting within 6 months after infarct; (2) subcortical ischemia, including small-vessel occlusion; (3) multi-infarct, including medium-to-large vessel disease; and (4) mixed, incorporating vascular and protein aggregate pathologies (Skrobot et al., 2018). The most common etiology of dementia is Alzheimer disease (AD), a form of cognitive impairment with amnestic-predominant phenotype and the presence of cerebral amyloid and tau protein aggregates (Jack et al., 2018). Compared to the distinct anatomical pattern of AD neurodegeneration originating within the medial temporal lobe, neurodegeneration linked to VCID occurs secondary to focal or global insufficiency of cerebral blood supply. Mixed dementia includes contributions from vascular and other pathologies (often AD) and comprises about 20% of all dementia cases (van der Flier and Scheltens, 2005; Suemoto et al., 2017). Several VCID animal models exist, though they are limited in their capacity to comprehensively recapitulate mixed pathologies/phenotypes in humans (Gooch and Wilcock, 2016). This review article focuses on the clinical aspects of certain risk factors for VCID, i.e., cholesterol, atherosclerosis, and APOE4, as well as the relationship of these risk factors for AD. We hope to offer new insight into disease mechanisms and future therapies (Figure 1).
Figure 1.
Shared features in Vascular Contributions to Cognitive Impairment and Dementia (VCID) and Alzheimer Disease (AD).
In 1894, Otto Binswanger provided the first clinicopathologic description of VCID. His patients demonstrated focal neurodegeneration where cerebral arteries displayed “extensive atherosclerotic changes,” “fatty degeneration,” and “thickening of inner and middle vascular membranes.” Strikingly, he noted a “primary proliferation of the glial parts” surrounding lipid-filled vessels (Binswanger, 1894; Blass et al., 1991). Thus, VCID is strongly associated with cerebral atherosclerosis, the chronic dysfunction of lipid homeostasis, and local inflammation caused by the accumulation of cholesterol, cholesteryl esters (CEs), other lipids, and activated stromal cells, including lipid-laden foamy macrophages, endothelial, and smooth muscle cells of vessel walls (Glass and Witztum, 2001; Hansson et al., 2006). Since perivascular astrocytes and pericytes modulate local blood vessel diameter to reflect real-time neuronal activity through “neurovascular coupling” (Attwell et al., 2010), it is reasonable to consider how activated glia and pericytes respond and contribute to intracranial atherosclerosis and ischemia (Binswanger, 1894; MacVicar and Newman, 2015; Price et al., 2018; Fernandez et al., 2019), particularly regarding lipid regulation (Koizumi et al., 2018). Atherosclerosis causes vessel stenosis and occlusion, thereby reducing cerebral blood flow. VCID is often associated with hypercholesterolemia, wherein elevated serum cholesterol promotes a cascade of cerebrovascular cholesterol deposition, inflammation, ischemia, neuronal injury, and cognitive impairment (Solomon et al., 2009; Appleton et al., 2017). We frame atherosclerosis as a condition associated with cerebrovascular lipid deposition and disease of large, medium, and small vessels, including arteriosclerosis and lipohyalinosis. While this review focuses on atherosclerotic influences on VCID, it is important to note that additional vascular etiologies contribute to VCID, including ischemia due to thromboembolism (cardiogenic sources, coagulopathy), chronic hypoperfusion, hypertension, et cetera (Qiao et al., 2017). These factors are covered in several reviews (Gorelick et al., 2011; Santos et al., 2017; Wolters and Ikram, 2019).
Apolipoprotein E (APOE) is a lipid-carrier protein tightly linked to dementia (Strittmatter et al., 1993). The APOE ε4 allele (APOE4), a minor allele of the APOE gene, is associated with a higher risk for AD (>2-fold increased risk for heterozygotes, >9-fold risk for homozygotes) and an elevated risk for VCID (2-fold increased risk for heterozygotes, 3-fold risk for homozygotes) (Rasmussen et al., 2018). Generally, APOE4 is linked to early memory impairment (Caselli et al., 2007), limbic dysfunction (Wolk and Dickerson, 2010), white matter (WM) ischemia (Koizumi et al., 2018), aberrant lipid metabolism, and neuroinflammation (Liu et al., 2013; Rasmussen, 2016; Tzioras et al., 2019). We then explore APOE4 in atherosclerosis and VCID.
Working Model of Atherosclerosis, Apoe, and Vcid
Here, we synthesize clinical data on cholesterol, atherosclerosis, APOE, and VCID into a working model; we posit that atherosclerosis and APOE4 promote reoccurring occlusion and ischemia that eventually lead to VCID. Then, we discuss potential intermediate steps involved, based on emerging research.
Atherosclerosis Is Associated With VCID and AD
Atherosclerosis can be divided into several categories: cerebral atherosclerosis that affects distal microscopic vessels, intracranial atherosclerotic disease (ICAD) that affects cerebral arteries, and large-vessel disease such as carotid artery stenosis (CAS) affecting carotid arteries supplying the brain (Box 1, Supplementary Figure 1). Myriad clinical data support the link between atherosclerosis and VCID as well as AD. For instance, cerebral autopsies (Beach et al., 2017) and Doppler ultrasound investigations of internal carotid arteries (Hofman et al., 1997) reveal vessel stenosis is more frequently observed in VCID and AD than in normal cognition, with a stronger association between VCID and atherosclerosis than AD with atherosclerosis. Additional studies support the association of atherosclerosis with dementia (Dolan et al., 2010; Dearborn et al., 2017), and with AD particularly (Roher et al., 2011; Yarchoan et al., 2012). In APOE4 carriers, ICAD/CAS is associated with greater cognitive decline (Haan et al., 1999).
Box 1. Glossary.
Carotid Artery Stenosis (CAS): Narrowing of intracranial, extracranial, and/or common carotid arteries that supply the head, neck, and Circle of Willis of the brain.
Circle of Willis (CoW): A circular network of cerebral arteries fed from carotid and vertebral arteries that deliver blood to the brain. Intracranial Atherosclerotic Disease (ICAD): Deposition of lipids, debris, and inflammatory cells in the walls of arteries in the skull that supply the brain. This condition is closely associated with VCID.
Ischemia: Loss of blood and oxygen supply to the tissue that can be chronic (atherosclerosis), or acute (sudden occlusion).
Occlusion: Blockage of a vessel leading to ischemia. In the brain, arterial occlusion causes a stroke, the occurrence of sudden neurologic deficit(s) due to inadequate vascular supply.
Stromal Activation: Proliferation and reaction of non-neuronal cells responding to and often exacerbating the neuronal injury. This includes activation of astrocytes, microglia, oligodendrocytes, vessel endothelial cells, pericytes, smooth muscle cells, macrophages, and other immune cells.
Vascular Contributions to Cognitive Impairment and Dementia (VCID): Cognitive impairment or dementia due to acute and/or chronic ischemia, secondary to a stroke, intracranial atherosclerosis, carotid artery stenosis, et cetera or a combination of vascular disease, Alzheimer neuropathologic changes (amyloid/tau), and/or other pathologies.
Relationships Between Atherosclerosis, Amyloid, and Tau
Amyloid and tau pathologies are the two distinct criteria for AD; they can also be present in VCID. Patients with suspected VCID and appreciable amyloid/tau biomarkers may have mixed dementia (Skrobot et al., 2018). Alterations in lipid deposition and cholesterol metabolism may modulate amyloid and/or tau pathology (Pappolla et al., 2002). Recent evidence from in vivo and ex vivo studies suggests that vascular lipid dysregulation and atherosclerosis may be independent dementia risk factors, in addition to their effects on amyloid/tau pathology. Several studies support this view: autopsies indicate ICAD does not correlate with amyloid/tau in either aging patients (Dolan et al., 2010), or in AD cohorts (Kosunen et al., 1995). ICAD severity on magnetic resonance angiography does not correlate cross-sectionally or spatially with in vivo cerebral amyloid burden based on positron emission tomography imaging (Gottesman et al., 2020). ICAD and AD elicit similar proteomic alterations in human dorsolateral prefrontal cortex glia and oligodendrocytes (Wingo et al., 2020). Interestingly, ICAD but neither amyloid nor tau pathology was associated with neurodegeneration, as measured by neurofilament light elevation (Iadecola, 2020; Wingo et al., 2020). Thus, amyloid may exert vascular changes through distinct paths from those caused by hypercholesterolemia and ICAD. Cerebral amyloid angiopathy (CAA), the deposition of amyloid aggregates in cerebral vessels, is associated with AD and VCID; moreover, both APOE4 and ICAD are associated with CAA and neurodegeneration (Premkumar et al., 1996; Tian et al., 2004; Yarchoan et al., 2012). While the APOEε2 allele (APOE2) is associated with lower AD risk, it raises CAA risk (Nelson et al., 2013), demonstrating a complex interplay between cholesterol, APOE, and parenchymal vs vascular amyloid. These data suggest vascular atherosclerosis and AD pathologies are two dissociable yet interacting contributions to neurodegeneration and cognitive decline.
APOE4 Is Associated With VCID and AD by Promoting Atherosclerosis
There is a clear association between APOE genotype and elevated VCID risk, validated through population studies (Slooter et al., 1997; Chang et al., 2010; Beach et al., 2017; Rasmussen et al., 2018; Pendlebury et al., 2020) and meta-analyses (McCarron et al., 1999). Studies investigating APOE4 in dementia after acute ischemic infarcts suggest that APOE4 impedes stroke recovery and promotes post-stroke VCID (Slooter et al., 1997; Pendlebury et al., 2020; Montagne et al., 2020b). Likewise, APOE4 carriers have an elevated risk of severe cardiac, extracranial and intracranial atherosclerosis (Mahley and Rall, 2000; Bennet et al., 2007; Granér et al., 2008). These findings are corroborated by post-mortem analyses of atherosclerosis in the Circle of Willis (CoW; Box 1; Kosunen et al., 1995; Abboud et al., 2008), and by in vivo internal carotid artery imaging studies (Terry et al., 1996; Cattin et al., 1997; Haan et al., 1999; Elosua et al., 2004; Volcik et al., 2006). A meta-analysis of 490 case-control studies also supports the impact of APOE4 on ICAD risk (Wei et al., 2017). Notably, CAS risk may be greater in middle-aged asymptomatic APOE4 carriers (Cattin et al., 1997), and ICAD may be associated more with male APOE4 carriers (Elosua et al., 2004; Abboud et al., 2008). The latter finding is distinct from AD pathology, where APOE4 is more strongly linked to AD risk in females (Neu et al., 2017). Overall, the association between APOE and cerebrovascular disease is affected by age and sex (Liu et al., 2013; Beach et al., 2017; Hohnman et al., 2018; Lamar et al., 2019). It should be noted that other studies suggest that APOE4 may not be associated with CoW ICAD severity (Premkumar et al., 1996; Yarchoan et al., 2012; Beach et al., 2017). However, on balance, a substantial plurality of studies strongly indicates a close association exists between APOE4 and ICAD.
Refining The Model: Intermediate Steps
The mechanisms leading from APOE4 to atherosclerosis to VCID are complex. Here, we consider candidate steps that may act as mediators, including serum/brain cholesterol, neurological/systemic inflammation, blood-brain permeability, and vascular aging. This requires the integration of clinical evidence with insight from animal and in vitro studies. It is important to note that additional vascular risk factors such as hypertension and smoking also influence dementia risk via multiple mechanisms to affect ICAD, stroke, and WM ischemia (Skoog et al., 1998; Kivipelto et al., 2001; Qiao et al., 2017; Koizumi et al., 2018; Nasrallah et al., 2019).
Hypercholesterolemia, APOE4, and Dementia
Hypercholesterolemia is associated with atherosclerotic cardiovascular and cerebrovascular disease (Duncan et al., 2019). Indeed, cohort studies and meta-analyses reveal that hypercholesterolemia at various times in the lifespan significantly increases the risk for ICAD (Ritz et al., 2014) and VCID (Moroney et al., 1999; Reitz et al., 2004). Elevated serum cholesterol may also promote AD, likely through mixed pathologies (Kivipelto et al., 2001; Solomon et al., 2009; Anstey et al., 2017; Wingo et al., 2019; Zhou et al., 2020). Mid-life cholesterol elevation is significantly associated with AD and trended towards elevated risk in VCID (Solomon et al., 2009). Furthermore, patients with familial hypercholesterolemia have a higher risk of mild cognitive impairment (Zambón et al., 2010). It is worth noting that most, but not all studies (Slooter et al., 1999; Mielke et al., 2010), show that hypercholesterolemia significantly raises dementia risk. Atherosclerosis risk and hypercholesterolemia are linked by mechanisms that involve APOE. APOE is present in plasma lipid particles as well as various cell types in the body and brain, as an essential lipid-carrier. It binds to low-density lipoprotein (LDL) receptors and other related receptors (Herz, 2009; Liu et al., 2013). While APOE2 is associated with elevated very-low-density lipoprotein (VLDL) and lower dementia risk (Reiman et al., 2020), APOE4 is linked to higher LDL cholesterol (Beilby et al., 2003; Saito et al., 2004; Hall et al., 2006; Bennet et al., 2007) and increased dementia risk.
Lipid Load in Astrocytes and Microglia, Neuroinflammation, and APOE4
The relationship between glia and lipid deposition traces to the original discoveries of VCID and AD, wherein Alzheimer observed that “many glial cells show adipose saccules” (Alzheimer, 1907; Stelzmann et al., 1995), and Binswanger noted the presence of rich “glial coating” of atherosclerotic vessels displaying “fatty degeneration” (Binswanger, 1894; Blass et al., 1991). Yet, only recently has local lipid deposition regained attention. Post-mortem lipidomic analyses of AD brains reveal deposits of a few selected lipid species, including cholesteryl esters (CEs), sphingomyelin, and ganglioside GM3. These species were enriched in AD-vulnerable regions (i.e., entorhinal and prefrontal cortex), but not cerebellum (Chan et al., 2012).
Astrocytes play essential roles in neuroinflammation and lipid deposition. Cumulatively, evidence indicates that astrocyte activation is linked to intracellular brain lipid accumulation, and APOE4 may exacerbate this response. For instance, human stem cell-derived APOE4 astrocytes display higher intracellular and extracellular cholesterol load, and compromised cholesterol efflux (Lin et al., 2018; Julia et al., 2019), as well as impaired endocytosis of lipids, amyloid, and other proteins, relative to astrocytes without APOE4 (Fernandez et al., 2019; Narayan et al., 2020). Similarly, cholesterol metabolism disruption was observed in human astrocytes expressing AD mutations, and these abnormalities were associated with tau hyperphosphorylation and neuronal toxicity (van der Kant et al., 2019). Lipid accumulation in AD astrocytes might be associated with aberrant acetate/acetyl-CoA metabolism, fatty-acid oxidation, and oxidative stress, which are markers for astrocyte activation (Wyss et al., 2011; Fernandez et al., 2019).
Microglia likely act as neuroinflammatory intermediaries between lipid overload and neurodegeneration. Lipid-laden microglia trigger oxidative stress and release proinflammatory cytokines (Marschallinger et al., 2020). Strikingly, numerous dementia-associated genes (i.e., APOE, ABCA1, ABCA7, CLU, PLCγ2, TREM2) are critical to lipid homeostasis and selectively expressed in microglia (Verheijen and Sleegers, 2018). Studies in mouse models demonstrate that deficiency of either APOE or TREM2 impairs phagocytosis, abrogates clearance of myelin-derived lipids, and promotes CE buildup (Nugent et al., 2020). ABCA1 is a key mediator of cellular lipid efflux. Variants in ABCA1 are implicated in cerebrovascular disease and AD (Nordestgaard et al., 2015). Further, PLCγ2 and TREM2 form a vital microglial lipid-sensing axis; genetic knockout of either gene in human stem cell-derived microglia models cause accumulation of cholesterol, CEs, and myelin-derived lipids, and perturbed inflammatory response (Andreone et al., 2020). APOE4 contributes to an inflammatory cascade of the neurovascular milieu (Lathe et al., 2014; Fernandez et al., 2019; Tzioras et al., 2019), likely in response to amyloid and lipid load. In APOE4 human microglia models, immunity/inflammation transcriptional pathways are dysregulated (Lin et al., 2018). Interestingly, in AD mouse models, Apoe expression occurs in the “late response” phase of microglial activation, possibly indicating a role for microglial APOE in chronic neuroinflammation and dementia (Keren-Shaul et al., 2017; Mathys et al., 2017).
Macrophages in Atherosclerosis and Inflammation
Macrophages are innate immune phagocytes found in both systemic and brain tissue. Macrophages display phenotypic plasticity in gene expression and cell function. In mouse models and in human atherosclerotic plaques, macrophages can be categorized into several distinct categories, including resident, proinflammatory, and foamy macrophages (Cochain et al., 2018). The cholesterol-rich, lipid-laden foamy macrophages are hallmarks of the early stages of atherosclerosis (Glass and Witztum, 2001). Surprisingly, foamy macrophages are distinct from other proinflammatory macrophages and even share transcriptional similarities to activated smooth muscle cells in atherosclerotic lesions (Winkels et al., 2018; Zernecke et al., 2020). These foamy macrophages express high levels of APOE and TREM2, suggesting crucial roles for APOE and TREM2 in maintaining macrophage cholesterol homeostasis (Zernecke et al., 2020). These studies illustrate the diversity and complexity of responses to lipid deposition in various immune and stromal cells. Foam cells in atherosclerosis may be analogous to the aging, cholesterol-rich, lipid-laden glia in the brain; APOE and TREM2 may play key roles in maintaining proper cholesterol homeostasis in the foamy microglia and astrocytes. Importantly, macrophages and glia regularly interact at key interfaces in glymphatic pathways, meningeal lymphatic vessels, and perivascular spaces (Louveau et al., 2017). Such crosstalk is integral to understanding inflammatory and vascular contributions to neurodegeneration.
Commonalities Between VCID and AD: Cholesterol, APOE4, and Inflammation
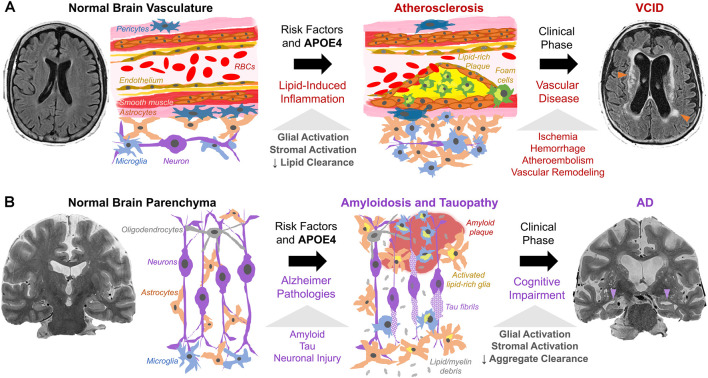
Lipid deposition (both intracellular and extracellular) and chronic inflammation are shared between atherosclerosis, VCID, and AD. In VCID, cholesterol, CEs, and other lipids accumulate in macrophages and cerebral blood vessels and impair blood flow (Figure 2A). In AD, similar lipid species accumulate mainly in glia and impede clearance of amyloid/tau aggregates (Figure 2B). In VCID and AD, crosstalk of systemic and neuroinflammatory pathways leads to stromal dysfunction (Holmes et al., 2009; Tao et al., 2018). Hence, lipid-associated inflammation alters glial, myeloid, and stromal cell interactions, hampers the turnover of accumulated lipid and protein aggregates, and promotes neurodegeneration. It is important to determine how/when proposed inflammatory cascades occur and how/when lipid overload and APOE4 spur local/systemic inflammation and worsen ICAD, VCID, and AD. Together, cholesterol accumulation, subsequent neuroinflammation, and impaired phagocytosis may be common features across the neurodegenerative spectrum.
Figure 2.
Working model of cholesterol, APOE4, and stromal activation in (A) VCID and (B) AD. (A) Risk factors (hypercholesterolemia, hypertension, smoking, APOE4) trigger atherosclerosis via cholesterol-rich plaques with local/systemic inflammation and stromal dysfunction (glia, macrophages, smooth muscle, endothelium, pericytes). Lipid-induced inflammation impairs lipid turnover and exacerbates plaque formation. This leads to ischemia (arrowheads) and dementia as detected by fluid-attenuated inversion recovery MRI. (B) Amyloid and tau pathology, with risk factors and APOE4, trigger neuronal injury. Subsequent proteinopathy-associated glial activation and lipid deposits (from glial proliferation and myelin debris) hinder amyloid/tau aggregate clearance and promote accumulation. This leads to aggregate spread and neurodegeneration (arrowheads) as seen on T2-weighted MRI.
Blood-Brain Barrier
Endothelial cells line cerebral capillaries and are linked to a vast network of pericytes and astrocyte end-feet, forming a blood-brain barrier (BBB). This structure selectively restricts the passage of substances from plasma into brain parenchyma. Dysfunction of the BBB is a potential APOE4-mediated pathway toward dementia. Indeed, loss of BBB integrity and subsequent vasogenic edema are common consequences of acute ischemia (Yang et al., 2019). Moreover, chronic activation and retraction of pericytes and endothelial cells may perpetuate pre-existing neurodegeneration in humans (Lau et al., 2020; Montagne et al., 2020a) and animal models (Bell et al., 2012). Various vascular risk factors are also associated with BBB damage (Cortes-Canteli and Iadecola, 2020). Dynamic contrast-enhanced magnetic resonance imaging (MRI) studies illustrate associations between APOE4 and limbic BBB breakdown in AD (Montagne et al., 2020a) and pericyte dysfunction in human stem cell-derived BBB models of CAA (Blanchard et al., 2020). Akin to atherosclerosis, mediation between APOE4 and dementia by the BBB may be unique to amyloid/tau response (Montagne et al., 2020a). Hence, VCID and AD likely share intermediate mechanisms, including ICAD and BBB dysfunction.
Vascular Aging
Aging may contribute to vessel disease and VCID (Ungvari et al., 2018). The relationship between age and VCID is partially attributable to age-related reduction in cholesterol metabolism/clearance, promoting hypercholesterolemia, atherosclerosis, and cognitive changes (Wang and Bennett, 2012; Zlokovic et al., 2020). Additionally, aging may promote hypertension, vessel stiffness, and disease via lipid peroxidation, oxidative stress, mitochondrial dysfunction, and senescence of stroma, vasculature, and brain parenchyma (Gustaw-Rothberg et al., 2010; Tarantini et al., 2019; Kiss et al., 2020). These metabolic changes could be exacerbated by APOE4 (Yin et al., 2019).
Potential Future Therapies
Targeting Cholesterol in Cerebral Arteries: Statins and Atherosclerosis Therapy
We now address potential therapeutic targets for both atherosclerosis and dementia. Atherosclerosis management and research have overwhelmingly been guided by stroke outcomes rather than cognition. Nevertheless, because atherosclerosis is a strong risk factor for VCID, cholesterol optimization is a current treatment strategy for cerebrovascular diseases. Statins lower LDL by inhibiting hydroxymethyl glutaryl-CoA reductase, thus increasing LDL receptor expression through sterol-mediated regulatory response in the liver (Brown and Goldstein, 1986). Though statins are an essential treatment for ICAD, CAS, and stroke, the results for VCID and AD treatments are mixed. While robust randomized controlled trials had not yet been performed for VCID and statins, cohort studies imply that statins may significantly reduce the incidence of VCID in participants with vascular risk factors such as hypercholesterolemia or diabetes (Hajjar et al., 2002; Fei et al., 2013; Giannopoulos et al., 2014). Moreover, statins may mitigate cognitive progression in adults with normal cognition and MCI (Steenland et al., 2013). APOE4 homozygotes emerged from re-analysis of statin trials with the greatest benefit, including slower cognitive decline and lower dementia incidence (Geifman et al., 2017). A meta-analysis found that statins may significantly lessen the risk of AD and MCI (Chu et al., 2018), and supporting studies trended toward benefit (Smith et al., 2017). However, numerous investigations report that statins do not prevent dementia while those studies that do support usage are often limited by smaller sample sizes (Shepardson et al., 2011a, b; McGuinness et al., 2016). Despite unclear evidence, the clinical co-occurrence of cerebrovascular disease and VCID often favors cholesterol management with statins.
To reduce infarcts that trigger/exacerbate VCID, current ICAD treatment includes cholesterol management, antiplatelet therapy (i.e., aspirin or P2Y12 inhibitors), and interventional methods (Chabriat and Bousser, 2006; Flusty et al., 2020). Yet, patients with ICAD on maximum medical therapy have non-negligible vascular risks, i.e., intracranial hemorrhage. One standard approach to treat cerebral ischemia with endovascular stenting even worsens outcomes significantly in ICAD (Chimowitz et al., 2011). Due to mixed findings, current neuro-interventional treatments are indicated for severe, symptomatic CAS only, but not for ICAD or VCID (Flusty et al., 2020). More research is required to better evaluate the possible benefit of ICAD treatment for VCID.
Targeting Cholesterol in Glia and Macrophages: LXR Agonists and ACAT1 Blockade
Statins act mainly in the liver. Beyond statins, additional strategies that act in local tissues exist to modulate cholesterol metabolism in-principle. We cite two examples. Liver X Receptors (LXRs) are essential membrane receptors that regulate cholesterol efflux in macrophages (LXRα) as well as in astrocytes and glia (LXRβ). LXRs represent possible targets for ICAD and VCID. Indeed, activation of LXRs reduces serum cholesterol and increases ABCA1-mediated cholesterol transport in humans and mouse/primate models of atherosclerosis (Calkin and Tontonoz, 2011; Muse et al., 2018), mainly by modulating lipid load in macrophages (Zhang et al., 2014). Further, LXR agonist attenuates amyloid pathology and microglial inflammation in transgenic AD models (Zelcer et al., 2007). However, current LXR agonists also adversely upregulate fatty-acid and triglyceride syntheses in mice and humans (Kirchgessner et al., 2016; Muse et al., 2018). Therefore, clinical translation may require investigation of the net impact of these opposing effects.
CEs are storage forms of cholesterol. In foamy macrophages, like those found in atherosclerotic lesions, CEs accumulate by acyl-CoA:cholesterol acyltransferase (ACAT, aka sterol O-acyltransferase, SOAT) converting cholesterol to CEs, and by cholesterol hydrolases cleaving CEs back to cholesterol (Brown et al., 1980). ACAT1 and ACAT2 enzymes are encoded by SOAT1 (Chang et al., 1993) and SOAT2 genes (Anderson et al., 1998; Cases et al., 1998; Oelkers et al., 1998). Both enzymes are integral endoplasmic reticulum membrane proteins; both are allosterically activated by cholesterol or oxysterols, and act on various sterols and long-chain fatty-acyl-CoAs as substrates (reviewed in Rogers et al., 2015). In healthy humans, ACAT1 is ubiquitously expressed across peripheral and brain tissue, whereas ACAT2 is mostly expressed in enterocytes and hepatocytes (reviewed in Chang et al., 2009). Cell models show that unlike statins (which inhibit cholesterol efflux), ACAT1 blockade promotes cholesterol efflux via ABCA1 mediated lipid efflux (Yamauchi et al., 2004). Mouse studies portray that reduction in myeloid ACAT1 alleviates diet-induced atherosclerosis (Huang et al., 2016; Melton et al., 2019). In AD studies, ACAT inhibitors significantly reduced amyloid accumulation in cell culture (Puglielli et al., 2001) and mouse models (Hutter-Paier et al., 2004). ACAT1/SOAT1 gene knockout in mice reduces amyloid (Bryleva et al., 2010) and tau burden (Shibuya et al., 2015a), by stimulating autophagy in microglia and neurons (Shibuya et al., 2014, 2015b). Additionally, ACAT1 inhibition rescues CE accumulation in human AD neurons (van der Kant et al., 2019) and human stem cell-derived microglia with TREM2 gene ablation (Nugent et al., 2020). These studies suggest that ACAT1 is a potential target to address atherosclerosis and proteinopathy in VCID or mixed dementia. Moreover, in a mouse model for the Niemann-Pick type C disease, a neurological disease caused by primary genetic defects in cholesterol homeostasis, ACAT1 blockade diverts cholesterol from storage to promote more efficient utilization in neural and peripheral tissues, suggesting that targeting ACAT1 is a potential strategy for multiple neurological diseases that involve cholesterol dyshomeostasis (Chang et al., 2020). Humans ACAT1/SOAT1 genetic variant analyses also support the role of ACAT1 in modulating dementia susceptibility (Wollmer et al., 2003; Alavez-Rubio et al., 2021).
APOE-Based Therapy
Investigational dementia therapies include targeting APOE directly, such as reducing APOE4 expression, with antibodies (Xiong et al., 2021), anti-sense oligonucleotides (Huynh et al., 2017), gene therapy, and gene editing (Liu et al., 2013; Yamazaki et al., 2016). In fact, an individual harboring a frameshift mutation ablating APOE expression had relatively normal cognition (Mak et al., 2014), possibly indicating treatment safety in altering APOE expression. To this end, adenoviral APOE2 knock-in approaches have already been tested in mice and in non-human primates (Williams et al., 2020). Small-molecule approaches include inhibiting deleterious APOE functions and correcting aberrant APOE structure induced by ε4 polymorphisms and associated with elevated amyloid, tau, and lipids (Mahley and Huang, 2012; Wang et al., 2018). Although it is still unclear whether APOE4 raises dementia risk by a gain of toxic function and/or loss of protective function (Kim et al., 2009; Serrano-Pozo et al., 2021), APOE-based therapies might address both mechanisms at local and systemic levels.
Conclusion
Neurodegeneration due to vascular etiologies is multifactorial and complex. Here, we describe a working model linking cholesterol load with atherosclerosis, APOE4, and VCID. At the cellular level, we posit that cholesterol load causes chronic neuroinflammation in microglia and astrocytes and triggers systemic inflammation in macrophages. Crosstalk between neuroinflammatory and systemic inflammatory signaling leads to stromal dysfunction. APOE4 may exacerbate local cellular cholesterol dyshomeostasis and stimulate glial/stromal inflammation, metabolic dysfunction, and BBB breakdown. At the macroscopic level, these changes promote atherosclerosis, ischemia, and cerebrovascular disease, ultimately contributing to VCID. Moreover, vascular changes, cholesterol accumulation, inflammation, and impaired turnover of protein and/or lipid aggregates are shared across neurodegeneration. We review potential therapies targeting cholesterol metabolism in astrocytes, microglia, and macrophages, though our understanding is far from complete. Future research may delineate VCID pathophysiology towards effective treatment.
Author Contributions
MD, T-YC, and CC conceived the project. MD wrote the initial version of the review and received inputs from IN, DW, CC, and T-YC for revisions. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Funding. This work was funded by research grant from NIA (RO1AG063544) to T-YC and CC as PI and co-I, and by an Alzheimer’s Disease Core Center grant (NIA P30-AG010124) to DW as one of the participating investigators.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2021.647990/full#supplementary-material.
Anatomy of cerebral arteries, including the (A,B) carotid arteries and (C,D) Circle of Willis (CoW), also shown on computed tomography arteriography (B,D). Illustrations adapted from Henry Gray’s Anatomy of the Human Body (1918), www.bartleby.com.
References
- Abboud S., Viiri L. E., Lütjohann D., Goebeler S., Luoto T., Friedrichs S., et al. (2008). Associations of apolipoprotein E gene with ischemic stroke and intracranial atherosclerosis. Eur. J. Hum. Genet. 16, 955–960. 10.1038/ejhg.2008.27 [DOI] [PubMed] [Google Scholar]
- Alavez-Rubio J. S., Martínez-Rodríguez N., Escobedo-de-la-Peña J., Garrido-Acosta O., Juárez-Cedillo T. (2021). Relationship between genetic variants of ACAT1 and APOE. Mol. Neurobiol. 58, 905–912. 10.1007/s12035-020-02162-3 [DOI] [PubMed] [Google Scholar]
- Alzheimer A. (1907). Über eine eigenartige Erkrankung der Hirnrinde. Allg. Z. Psychiat. 64, 146–148. [Google Scholar]
- Anderson R. A., Joyce C., Davis M., Reagan J. W., Clark M., Shelness G. S., et al. (1998). Identification of a form of acyl-CoA:cholesterol acyltransferase specific to liver and intestine in nonhuman primates. J. Biol. Chem. 273, 26747–26754. 10.1074/jbc.273.41.26747 [DOI] [PubMed] [Google Scholar]
- Andreone B. J., Przybyla L., Llapashtica C., Rana A., Davis S. S., van Lengerich B., et al. (2020). Alzheimer’s-associated PLCγ2 is a signaling node required for both TREM2 function and the inflammatory response in human microglia. Nat. Neurosci. 23, 927–938. 10.1038/s41593-020-0650-6 [DOI] [PubMed] [Google Scholar]
- Anstey K. J., Ashby-Mitchell K., Peters R. (2017). Updating the evidence on the association between serum cholesterol and risk of late-life dementia: review and meta-analysis. J. Alzheimers Dis. 56, 215–228. 10.3233/JAD-160826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleton J. P., Scutt P., Spring N., Bath P. M. (2017). Hypercholesterolaemia and vascular dementia. Clin. Sci. 131, 1561–1578. 10.1042/CS20160382 [DOI] [PubMed] [Google Scholar]
- Attwell D., Buchan A. M., Charpak S., Lauritzen M., MacVicar B. A., Newman E. A. (2010). Glial and neuronal control of brain blood flow. Nature 2468, 232–243. 10.1038/nature09613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach T. G., Wilson J. R., Sue L. I., Newell A., Poston M., Cisneros R., et al. (2017). Circle of Willis atherosclerosis association with Alzheimer’s disease, neuritic plaques and neurofibrillary tangles. Acta Neuropathol. 113, 13–21. 10.1007/s00401-006-0136-y [DOI] [PubMed] [Google Scholar]
- Beilby J. P., Hunt C. C. J., Palmer L. J., Chapman C. M. L., Burley J. P., McQuillan B. M., et al. (2003). Apolipoprotein E gene polymorphisms are associated with carotid plaque formation but not with intima-media wall thickening: results from the perth carotid ultrasound disease assessment study (CUDAS). Stroke 34, 869–874. 10.1161/01.STR.0000062901.54157.12 [DOI] [PubMed] [Google Scholar]
- Bell R. D., Winkler E. A., Singh I., Sagare A. P., Deane R., Wu Z., et al. (2012). Apolipoprotein E controls cerebrovascular integrity via cyclophilin A. Nature 485, 512–516. 10.1038/nature11087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennet A. M., Di Angelantonio E., Ye Z., Wensley F., Dahlin A., Ahlbom A., et al. (2007). Association of apolipoprotein E genotypes with lipid levels and coronary risk. JAMA 298, 1300–1311. 10.1001/jama.298.11.1300 [DOI] [PubMed] [Google Scholar]
- Binswanger O. (1894). Die abgrenzung der allgemeinen progresiven paralyse. Berl. Klin. Wochenschr. 31, 1103–1105, 1137,–1139, 1180–1186. [Google Scholar]
- Blanchard J. W., Bula M., Davila-Velderrain J., Akay L. A., Zhu L., Frank A., et al. (2020). Reconstruction of the human blood-brain barrier in vitro reveals a pathogenic mechanism of APOE4 in pericytes. Nat. Med. 26, 952–963. 10.1038/s41591-020-0886-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blass J. P., Hoyer S., Nitsch R. (1991). A translation of otto binswanger’s article, ‘the delineation of the generalized progressive paralyses’. Arch. Neurol. 48, 961–972. 10.1001/archneur.1991.00530210089029 [DOI] [PubMed] [Google Scholar]
- Brown M. S., Goldstein J. L. (1986). A receptor-mediated pathway for cholesterol homeostasis. Science 232, 34–47. 10.1126/science.3513311 [DOI] [PubMed] [Google Scholar]
- Brown M. S., Ho Y. K., Goldstein J. L. (1980). The cholesteryl ester cycle in macrophage foam cells. Continual hydrolysis and re-esterification of cytoplasmic cholesteryl esters. J. Biol. Chem. 255, 9344–9352. 10.1016/s0021-9258(19)70568-7 [DOI] [PubMed] [Google Scholar]
- Bryleva E. Y., Rogers M. A., Chang C. C., Buen F., Harris B. T., Rousselet E., et al. (2010). ACAT1 gene ablation increases 24(S)-hydroxycholesterol content in the brain and ameliorates amyloid pathology in mice with AD. Proc. Natl. Acad. Sci. U S A 107, 3081–3086. 10.1073/pnas.0913828107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkin A., Tontonoz P. (2011). LXR signaling pathways and atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 30, 1513–1518. 10.1161/ATVBAHA.109.191197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caselli R. J., Reiman E. M., Locke D. E. C., Hutton M. L., Hentz J. G., Hoffman-Snyder C., et al. (2007). Cognitive domain decline in healthy apolipoprotein E ε4 homozygotes before the diagnosis of mild cognitive impairment. Arch. Neurol. 64, 1306–1311. 10.1001/archneur.64.9.1306 [DOI] [PubMed] [Google Scholar]
- Cases S., Novak S., Zheng Y. W., Myers H. M., Lear S. R., Sande E., et al. (1998). ACAT-2, a second mammalian acyl-CoA:cholesterol acyltransferase. Its cloning, expression, and characterization. J. Biol. Chem. 273, 26755–26764. 10.1074/jbc.273.41.26755 [DOI] [PubMed] [Google Scholar]
- Cattin L., Fisicaro M., Tonizzo M., Valenti M., Danes G. M., Fonda M., et al. (1997). Polymorphism of the apolipoprotein E gene and early carotid atherosclerosis defined by ultrasonography in asymptomatic adults. Arterioscler. Thromb. Vasc. Biol. 17, 91–94. 10.1161/01.atv.17.1.91 [DOI] [PubMed] [Google Scholar]
- Chabriat H., Bousser M. G. (2006). Vascular dementia: potential of antiplatelet agents in prevention. Eur. Neurol. 55, 61–69. 10.1159/000091981 [DOI] [PubMed] [Google Scholar]
- Chan R. B., Oliveira T. G., Cortes E. P., Honig L. S., Duff K. E., Small S. A., et al. (2012). Comparative lipidomic analysis of mouse and human brain with Alzheimer disease. J. Biol. Chem. 287, 2678–2688. 10.1074/jbc.M111.274142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Y.-F., Hayden K. M., Norton M. C., Tschanz J., Breitner J. C. S., Welsh-Bohmer K. A., et al. (2010). Association between APOE ε4 allele and vascular dementia: the cache county study. Dement. Geriatr. Cogn. Disord. 29, 248–253. 10.1159/000285166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C. C., Huh H. Y., Cadigan K. M., Chang T. Y. (1993). Molecular cloning and functional expression of human acyl-coenzyme A:cholesterol acyltransferase cDNA in mutant Chinese hamster ovary cells. J. Biol. Chem. 268, 20747–20755. 10.1016/s0021-9258(19)36846-2 [DOI] [PubMed] [Google Scholar]
- Chang T.-Y., Li B.-L., Chang C. C., Urano Y. (2009). Acyl-coenzyme A:cholesterol acyltransferases. Am. J. Physiol. Endocrinol. Metab. 297, E1–E9. 10.1152/ajpendo.90926.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C. C. Y., Rogers M. A., Maue R. A., Melton E. M., Peden A. A., Garver W. S., et al. (2020). Acat1 gene KO restores TGN cholesterol deficiency in mutant NPC1 cells and expands mutant Npc1 mouse lifespan. bioRxiv [Preprint]. 10.1101/2020.08.07.241471 [DOI] [Google Scholar]
- Chimowitz M. I., Lynn M. J., Derdeyn C. P., Turan T. N., Fiorella D., Lane B. F., et al. (2011). Stenting versus aggressive medical therapy for intracranial arterial stenosis. N. Engl. J. Med. 365, 993–1003. 10.1056/NEJMoa1105335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu C.-S., Tseng P.-T., Stubbs B., Chen T.-Y., Tang C.-H., Li D.-J., et al. (2018). Use of statins and the risk of dementia and mild cognitive impairment: a systematic review and meta-analysis. Sci. Rep. 8:5804. 10.1038/s41598-018-24248-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochain C., Vafadarnejad E., Arampatzi P., Pelisek J., Winkels H., Ley K., et al. (2018). Single-cell RNA-Seq reveals the transcriptional landscape and heterogeneity of aortic macrophages in murine atherosclerosis. Circ. Res. 122, 1661–1674. 10.1161/CIRCRESAHA.117.312509 [DOI] [PubMed] [Google Scholar]
- Cortes-Canteli M., Iadecola C. (2020). Alzheimer’s disease and vascular aging: JACC focus seminar. J. Am. Coll. Cardiol. 75, 942–951. 10.1016/j.jacc.2019.10.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearborn J. L., Zhang Y., Qiao Y., Suri M. F. K., Liu L., Gottesman R. F., et al. (2017). Intracranial atherosclerosis and dementia the atherosclerosis risk in communities (ARIC) study. Neurology 88, 1556–1563. 10.1212/WNL.0000000000003837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan H., Crain B., Troncoso J., Resnick S. M., Zonderman A. B., Obrien R. J. (2010). Atherosclerosis, dementia, and Alzheimer disease in the baltimore longitudinal study of aging cohort. Ann. Neurol. 68, 231–240. 10.1002/ana.22055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan M. S., Vasan R. S., Xanthakis V. (2019). Trajectories of blood lipid concentrations over the adult life course and risk of cardiovascular disease and all-cause mortality: observations from the framingham study over 35 years. J. Am. Heart Assoc. 8:e011433. 10.1161/JAHA.118.011433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elosua R., Ordovas J. M., Cupples L. A., Fox C. S., Polak J. F., Wolf P. A., et al. (2004). Association of APOE genotype with carotid atherosclerosis in men and women: the framingham heart study. J. Lipid Res. 45, 1868–1875. 10.1194/jlr.M400114-JLR200 [DOI] [PubMed] [Google Scholar]
- Fei M., Yan Ping Z., Ru Juan M., NingNing L., Lin G. (2013). Risk factors for dementia with type 2 diabetes mellitus among elderly people in China. Age Ageing 42, 398–400. 10.1093/ageing/afs188 [DOI] [PubMed] [Google Scholar]
- Fernandez C. G., Hamby M. E., McReynolds M. L., Ray W. J. (2019). The role of APOE4 in disrupting the homeostatic functions of astrocytes and microglia in aging and Alzheimer’s disease. Front. Aging Neurosci. 11:14. 10.3389/fnagi.2019.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flusty B., de Havenon A., Prabhakaran S., Liebeskind D. S., Yaghi S. (2020). Intracranial atherosclerosis treatment past, present, and future. Stroke 51, e49–e53. 10.1161/STROKEAHA.119.028528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geifman N., Brinton R. D., Kennedy R. E., Schneider L. S., Butte A. J. (2017). Evidence for benefit of statins to modify cognitive decline and risk in Alzheimer’s disease. Alzheimers Res. Ther. 9:10. 10.1186/s13195-017-0237-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannopoulos S., Katsanos A. H., Kosmidou M., Tsivgoulis G. (2014). Statins and vascular dementia: a review. J. Alzheimers Dis. 42, S315–320. 10.3233/JAD-132366 [DOI] [PubMed] [Google Scholar]
- Glass C. K., Witztum J. L. (2001). Atherosclerosis: the road ahead. Cell 104, 503–516. 10.1016/s0092-8674(01)00238-0 [DOI] [PubMed] [Google Scholar]
- Gooch J., Wilcock D. M. (2016). Animal models of vascular cognitive impairment and dementia (VCID). Cell. Mol. Neurobiol. 36, 233–239. 10.1007/s10571-015-0286-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorelick P. B., Scuteri A., Black S. E., DeCarli C., Greenberg S. M., Iadecola C., et al. (2011). Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42, 2672–2713. 10.1161/STR.0b013e3182299496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottesman R. F., Mosley T. H., Knopman D. S., Hao Q., Wong D., Wagenknecht L. E., et al. (2020). Association of intracranial atherosclerotic disease with brain β-amyloid deposition: secondary analysis of the ARIC study. JAMA Neurol. 77, 350–357. 10.1001/jamaneurol.2019.4339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granér M., Kahri J., Varpula M., Salomon R. M., Nyyssönen K., Jauhianinen M., et al. (2008). Apolipoprotein E polymorphism is associated with both carotid and coronary atherosclerosis in patients with coronary artery disease. Nutr. Metab. Cardiovasc. Dis. 18, 271–277. 10.1016/j.numecd.2007.01.003 [DOI] [PubMed] [Google Scholar]
- Gustaw-Rothberg K., Kowalczuk K., Stryjecka-Zimmer M. (2010). Lipids’ peroxidation markers in Alzheimer’s disease and vascular dementia. Geriatr. Geront. Int. 10, 161–166. 10.1111/j.1447-0594.2009.00571.x [DOI] [PubMed] [Google Scholar]
- Haan M. N., Shemanski L., Jaguar W. J., Manolis T. A., Kuller L. (1999). The role of APOE ε4 in modulating effects of other risk factors for cognitive decline in elderly persons. JAMA 282, 40–46. 10.1001/jama.282.1.40 [DOI] [PubMed] [Google Scholar]
- Hajjar I., Schumpert J., Hirth V., Wieland D., Eleazer G. P. (2002). The impact of the use of statins on the prevalence of dementia and the progression of cognitive impairment. J. Gerontol. A Biol. Sci. Med. Sci. 57, M414–M418. 10.1093/gerona/57.7.m414 [DOI] [PubMed] [Google Scholar]
- Hall K., Murrell J., Ogunniyi A., Deeg M., Baiyewu O., Gao S., et al. (2006). Cholesterol, APOE genotype, and Alzheimer disease: an epidemiologic study of Nigerian Yoruba. Neurology 66, 223–227. 10.1212/01.wnl.0000194507.39504.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansson G. K., Robertson A.-K. L., Söderberg-Nauclér C. (2006). Inflammation and atherosclerosis. Annu. Rev. Pathol. 1, 297–329. 10.1146/annurev.pathol.1.110304.100100 [DOI] [PubMed] [Google Scholar]
- Herz J. (2009). Apolipoprotein E receptors in the nervous system. Curr. Opin. Lipidol. 20, 190–196. 10.1097/MOL.0b013e32832d3a10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofman A., Ott A., Breteler M. M. B., Bots M. L., Slooter A. J. C., van Karskamp F., et al. (1997). Atherosclerosis, apolipoprotein E, and the prevalence of dementia and Alzheimer’s disease in the Rotterdam study. Lancet 349, 151–154. 10.1016/S0140-6736(96)09328-2 [DOI] [PubMed] [Google Scholar]
- Hohnman T. J., Dumitrescu L., Barnes L. L., Thambisetty M., Beecham G., Kunkle B., et al. (2018). Sex-specific association of apolipoprotein E with cerebrospinal fluid levels of tau. JAMA Neurol. 75, 989–998. 10.1001/jamaneurol.2018.0821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes C., Cunningham C., Zotova E., Woolford J., Dean C., Culliford D., et al. (2009). Systemic inflammation and disease progression in Alzheimer disease. Neurology 73, 768–774. 10.1212/WNL.0b013e3181b6bb95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L.-H., Melton E. M., Li H., Sohn P., Rogers M. A., Mulligan-Kehoe M. J., et al. (2016). Myeloid Acyl-CoA:Cholesterol acyltransferase 1 deficiency reduces lesion macrophage content and suppresses atherosclerosis progression. J. Biol. Chem. 291, 6232–6244. 10.1074/jbc.M116.713818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutter-Paier B., Huttunen H. J., Puglielli L., Echman C. B., Kim D. Y., Hofmeister A., et al. (2004). The ACAT inhibitor CP-113,818 markedly reduces amyloid pathology in a mouse model of Alzheimer’s disease. Neuron 44, 227–238. 10.1016/j.neuron.2004.08.043 [DOI] [PubMed] [Google Scholar]
- Huynh T.-P. V., Liao E., Francis C. M., Robinson G. O., Serrano J. R., Jiang H., et al. (2017). Age-dependent effects of apoE reduction using antisense oligonucleotides in a model of β-amyloidosis. Neuron 96, 1013–1023. 10.1016/j.neuron.2017.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iadecola C. (2020). Revisiting atherosclerosis and dementia. Nat. Neurosci. 23, 691–692. 10.1038/s41593-020-0626-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iadecola C., Duering M., Hachinski V., Joutel A., Pendlebury S. T., Schneider J. A., et al. (2019). Vascular cognitive impairment and dementia JACC scientific expert panel. J. Am. Coll. Cardiol. 73, 3326–3344. 10.1016/j.jacc.2019.04.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jack C. R., Jr., Bennett D. A., Blennow K., Carrillo M. C., Dunn B., Haeberlein S. B., et al. (2018). NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 14, 535–562. 10.1016/j.jalz.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julia T. C. W., Liang S. A., Qian L., Pipalia N. H., Chao M. J., Shi Y., et al. (2019). Cholesterol and matrisome pathways dysregulated in human APOEε4 glia. bioRxiv [Preprint]. 10.1101/713362 [DOI] [Google Scholar]
- Keren-Shaul H., Spinrad A., Weiner A., Matcovitch-Natan O., Dvir-Szternfeld R., Ulland T. K. (2017). A unique microglia type associated with restricting development of Alzheimer’s disease. Cell 169, 1276–1290. 10.1016/j.cell.2017.05.018 [DOI] [PubMed] [Google Scholar]
- Kim J., Basak J. M., Holtzman D. M. (2009). The role of apolipoprotein E in Alzheimer’s disease. Neuron 63, 287–303. 10.1016/j.neuron.2009.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchgessner T. G., Sleph P., Ostrowski J., Lupisella J., Ryan C. S., Liu X., et al. (2016). Beneficial and adverse effects of an lxr agonist on human lipid and lipoprotein metabolism and circulating neutrophils. Cell Metab. 9, 223–233. 10.1016/j.cmet.2016.07.016 [DOI] [PubMed] [Google Scholar]
- Kiss T., Nyúl-Tóth A., Balasubramanian P., Tarantini S., Ahire C., Yabluchanskiy A., et al. (2020). Nicotinamide mononucleotide (NMN) supplementation promotes neurovascular rejuvenation in aged mice: transcriptional footprint of SIRT1 activation, mitochondrial protection, anti-inflammatory, and anti-apoptotic effects. Geroscience 42, 527–546. 10.1007/s11357-020-00165-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivipelto M., Helkala E.-L., Laakso M. P., Hänninen T., Hallikainen M., Alhainen K., et al. (2001). Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ 322, 1447–1451. 10.1136/bmj.322.7300.1447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koizumi K., Hattori Y., Ahn S. J., Buendia I., Ciacciarelli A., Uekawa K., et al. (2018). Apoε4 disrupts neurovascular regulation and undermines white matter integrity and cognitive function. Nat. Commun. 9:3816. 10.1038/s41467-018-06301-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosunen O., Talasniemi S., Lehtovirta M., Heinonen O., Helisalmi S., Mannermaa A., et al. (1995). Relation of coronary atherosclerosis and apolipoprotein E genotypes in Alzheimer patients. Stroke 26, 743–748. 10.1161/01.str.26.5.743 [DOI] [PubMed] [Google Scholar]
- Lamar M., Yu L., Rubin L. H., James B. D., Barnes L. L., Marcelo Farfel J., et al. (2019). APOE genotypes as a risk factor for age-dependent accumulation of cerebrovascular disease in older adults. Alzheimers Dement. 15, 258–266. 10.1016/j.jalz.2018.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lathe R., Sapronova A., Kotelevtsev Y. (2014). Atherosclerosis and Alzheimer-diseases with a common cause? Inflammation, oxysterols, vasculature. BMC Geriatr. 14:36. 10.1186/1471-2318-14-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau S.-F., Cao H., Fu A. K. Y., Ip N. Y. (2020). Single-nucleus transcriptome analysis reveals dysregulation of angiogenic endothelial cells and neuroprotective glia in Alzheimer’s disease. Proc. Natl. Acad. Sci. U S A 117, 25800–25809. 10.1073/pnas.2008762117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.-T., Seo J., Gao F., Feldman H. M., Wen H.-L., Penney J., et al. (2018). APOE4 causes widespread molecular and cellular alterations associated with Alzheimer’s disease phenotypes in human iPSC-derived brain cell types. Neuron 98, 1141–1154. 10.1016/j.neuron.2018.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.-C., Kanekiyo T., Xu H., Bu G. (2013). Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy. Nat. Rev. Neurol. 9, 106–118. 10.1038/nrneurol.2012.263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louveau A., Plog B. A., Antila S., Alitalo K., Nedergaard M., Kipnis J. (2017). Understanding the functions and relationships of the glymphatic system and meningeal lymphatics. J. Clin. Invest. 127, 3210–3219. 10.1172/JCI90603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacVicar B. A., Newman E. A. (2015). Astrocyte regulation of blood flow in the brain. Cold Spring Harb. Perspect. Biol. 7:a020388. 10.1101/cshperspect.a020388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahley R. W., Huang Y. (2012). Small-molecule structure correctors target abnormal protein structure and function: the structure corrector rescue of apolipoprotein E4- associated neuropathology. J. Med. Chem. 55, 8997–9008. 10.1021/jm3008618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahley R. W., Rall S. C., Jr. (2000). Apolipoprotein E: far more than a lipid transport protein. Annu. Rev. Genomics Hum. Genet. 1, 507–537. 10.1146/annurev.genom.1.1.507 [DOI] [PubMed] [Google Scholar]
- Mak A. C. Y., Pullinger C. R., Tang L. F., Wong J. S., Deo R. C., Schwarz J.-M., et al. (2014). Effects of the absence of apolipoprotein e on lipoproteins, neurocognitive function, and retinal function. JAMA Neurol. 71, 1228–1236. 10.1001/jamaneurol.2014.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschallinger J., Iram T., Zardeneta M., Lee S. E., Lehallier B., Haney M. S., et al. (2020). Lipid-droplet-accumulating microglia represent a dysfunctional and proinflammatory state in the aging brain. Nat. Neurosci. 23, 194–208. 10.1038/s41593-019-0566-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathys H., Adaikkan C., Gao F., Young J. Z., Manet E., Hemberg M., et al. (2017). Temporal tracking of microglia activation in neurodegeneration at single-cell resolution. Cell Rep. 21, 366–380. 10.1016/j.celrep.2017.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarron M. O., Delong D., Alberts M. J. (1999). APOE genotype as a risk factor for ischemic cerebrovascular disease A meta-analysis. Neurology 53, 1308–1311. 10.1212/wnl.53.6.1308 [DOI] [PubMed] [Google Scholar]
- McGuinness B., Craig D., Bullock R., Passmore P. (2016). Statins for the prevention of dementia. Cochrane Database Syst. Rev. 1:CD003160. 10.1002/14651858.CD003160.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melton E. M., Li H., Benson J., Sohn P., Huang L.-H., Song B.-L., et al. (2019). Myeloid Acat1/Soat1 KO attenuates pro-inflammatory responses in macrophages and protects against atherosclerosis in a model of advanced lesions. J. Biol. Chem. 294, 15836–15849. 10.1074/jbc.RA119.010564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielke M. M., Zandi P. P., Shao H., Waern M., Östling S., Guo X., et al. (2010). The 32-year relationship between cholesterol and dementia from midlife to late life. Neurology 75, 1888–1895. 10.1212/WNL.0b013e3181feb2bf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagne A., Nation D. A., Sagare A. P., Barisano G., Sweeney M. D., Chakhoyan A., et al. (2020a). APOE4 leads to blood-brain barrier dysfunction predicting cognitive decline. Nature 581, 71–76. 10.1038/s41586-020-f2247-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagne A., Nation D. S., Zlokovic B. V. (2020b). APOE4 accelerates development of dementia after stroke is there a role for cerebrovascular dysfunction? Stroke 51, 699–700. 10.1161/STROKEAHA.119.028814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moroney J. T., Tang M. X., Berglund L., Small S., Merchant C., Bell K., et al. (1999). Low-density lipoprotein cholesterol and the risk of dementia with stroke. JAMA 282, 254–260. 10.1001/jama.282.3.254 [DOI] [PubMed] [Google Scholar]
- Muse E. D., Yu S., Edillor C. R., Tao J., Spann N. J., Troutman T. D., et al. (2018). Cell-specific discrimination of desmosterol and desmosterol mimetics confers selective regulation of LXR and SREBP in macrophages. Proc. Natl. Acad. Sci. U S A 115, E4680–E4689. 10.1073/pnas.1714518115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan P., Sienski G., Bonner J. M., Lin Y.-T., Seo J., Baru V., et al. (2020). PICALM rescues endocytic defects caused by the Alzheimer’s disease risk factor APOE4. Cell Rep. 33:108224. 10.1016/j.celrep.2020.108224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasrallah I. M., Pajewski N. M., Auchus A. P., Chelune G., Cheung A. K., Cleveland M. L., et al. (2019). Association of intensive vs standard blood pressure control with cerebral white matter lesions. JAMA 322, 524–534. 10.1001/jama.2019.10551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson P. T., Pious N. M., Jicha G. A., Wilcock D. M., Fardo D. A., Estus S., et al. (2013). APOE-ε2 and APOE-ε4 correlate with increased amyloid accumulation in cerebral vasculature. J. Neuropathol. Exp. Neurol. 72, 708–715. 10.1097/NEN.0b013e31829a25b9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neu S. C., Pa J., Kukull W., Beekly D., Kuzma A., Gangadharan P., et al. (2017). Apolipoprotein E genotype and sex risk factors for Alzheimer disease: a meta-analysis. JAMA Neurol. 74, 1178–1189. 10.1001/jamaneurol.2017.2188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordestgaard L. T., Tybjaerg-Hansen A., Nordestgaard B. G., Frikke-Schmidt R. (2015). Loss of- function mutation in ABCA1 and risk of Alzheimer’s disease and cerebrovascular disease. Alzheimers Dement. 11, 1430–1438. 10.1016/j.jalz.2015.04.006 [DOI] [PubMed] [Google Scholar]
- Nugent A. A., Lin K., van Lengerich B., Lianoglou S., Przybyla L., Davis S. S., et al. (2020). TREM2 regulates microglial cholesterol metabolism upon chronic phagocytic challenge. Neuron 105, 837–854. 10.1016/j.neuron.2019.12.007 [DOI] [PubMed] [Google Scholar]
- Oelkers P., Behari A., Cromley D., Billheimer J. T., Sturley S. L. (1998). Characterization of two human genes encoding acyl coenzyme A:cholesterol acyltransferase-related enzymes. J. Biol. Chem. 273, 26765–26771. 10.1074/jbc.273.41.26765 [DOI] [PubMed] [Google Scholar]
- Pappolla M. A., Smith M. A., Bryant-Thomas T., Bazan N., Petanceska S., Perry G., et al. (2002). Cholesterol, oxidative, stress and Alzheimer’s disease: expanding the horizons of pathogenesis. Free Radic. Biol. Med. 33, 173–181. 10.1016/s0891-5849(02)00841-9 [DOI] [PubMed] [Google Scholar]
- Pendlebury S. T., Poole D., Burgess A., Duerden J., Rothwell P. M., Oxford Vascular Study (2020). APOE-ε4 genotype and dementia before and after transient ischemic attack and stroke. Stroke 51, 751–758. 10.1161/STROKEAHA.119.026927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Premkumar D. R., Cohen D. L., Hedera P., Friedland R. P., Kalaria R. N. (1996). Apolipoprotein E-epsilon4 alleles in cerebral amyloid angiopathy and cerebrovascular pathology associated with Alzheimer’s disease. Am. J. Pathol. 148, 2083–2095. [PMC free article] [PubMed] [Google Scholar]
- Price B. R., Norris C. M., Sompol P., Wilcock D. M. (2018). An emerging role of astrocytes in vascular contributions to cognitive impairment and dementia. J. Neurochem. 144, 644–650. 10.1111/jnc.14273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puglielli L., Konopka G., Pack-Chung E., Ingano L. A., Berezovska O., Hyman B. T., et al. (2001). Acyl-coenzyme A: cholesterol acyltransferase modulates the generation of the amyloid beta-peptide. Nat. Cell Biol. 3, 905–912. 10.1038/ncb1001-905 [DOI] [PubMed] [Google Scholar]
- Qiao Y., Suri F. S., Zhang Y., Liu L., Gottesman R., Alonso A., et al. (2017). Racial differences in prevalence and risk for intracranial atherosclerosis in a US community-based population. JAMA 2, 1341–1348. 10.1001/jamacardio.2017.4041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen K. L. (2016). Plasma levels of apolipoprotein E, APOE genotype and risk of dementia and ischemic heart disease. Atherosclerosis 255, 145–155. 10.1016/j.atherosclerosis.2016.10.037 [DOI] [PubMed] [Google Scholar]
- Rasmussen K. L., Tybjærg-Hansen A., Nordestgaard B. G., Frikke-Schmidt R. (2018). Absolute 10-year risk of dementia by age, sex and APOE genotype. CMAJ 190, E1033–E1041. 10.1503/cmaj.180066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman E. M., Arboleda-Velasquez J. F., Quiroz Y. T., Huentelman M. J., Beach T. G., Caselli R. J., et al. (2020). Exceptionally low likelihood of Alzheimer’s dementia in APOE2 homozygotes from a 5,000-person neuropathological study. Nat. Commum. 11:667. 10.1038/s41467-019-14279-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitz C., Tang M.-X., Luchsinger J., Mayeux R. (2004). Relation of plasma lipids to Alzheimer disease and vascular dementia. Arch. Neurol. 61, 705–714. 10.1001/archneur.61.5.705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritz K., Denswil N. P., Stam O. C. G., van Lieshout J. J., Daemen M. J. A. P. (2014). Cause and mechanisms of intracranial atherosclerosis. Circulation 130, 1407–1414. 10.1161/CIRCULATIONAHA.114.011147 [DOI] [PubMed] [Google Scholar]
- Rogers M. A., Liu J., Song B.-L., Li B.-L., Chang C. C., Chang T.-Y. (2015). Acyl-CoA:cholesterol acyltransferases (ACATs/SOATs): enzymes with multiple sterols as substrates and as activators. J. Steroid Biochem. Mol. Biol. 151, 102–107. 10.1016/j.jsbmb.2014.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roher A. E., Tyas S. L., Maarouf C. L., Daugs I. D., Kokjohn T. A., Emmerling M. R., et al. (2011). Intracranial atherosclerosis as a contributing factor to Alzheimer’s disease dementia. Alzheimers Dement. 7, 436–444. 10.1016/j.jalz.2010.08.228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito M., Eto M., Nitta H., Kanda Y., Shigeto M., Nakayama K., et al. (2004). Effect of apolipoprotein E4 allele on plasma LDL cholesterol response to diet therapy in type 2 diabetic patients. Diabetes Care 27, 1276–1280. 10.2337/diacare.27.6.1276 [DOI] [PubMed] [Google Scholar]
- Santos C. Y., Snyder P. J., Wu W.-C., Zhang M., Echeverria A., Alber J. (2017). Pathophysiologic relationship between Alzheimer’s disease, cerebrovascular disease and cardiovascular risk: a review and synthesis. Alzheimers Dement. 7, 69–87. 10.1016/j.dadm.2017.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Pozo A., Das S., Hyman B. T. (2021). APOE and Alzheimer’s disease: advances in genetics, pathophysiology and therapeutic approaches. Lancet Neurol. 20, 68–80. 10.1016/S1474-4422(20)30412-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepardson N. E., Shankar B. M., Selkoe D. J. (2011a). Cholesterol level and statin use in Alzheimer disease I. Review of epidemiological and preclinical studies. JAMA Neurol. 68, 1239–1244. 10.1001/archneurol.2011.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepardson N. E., Shankar B. M., Selkoe D. J. (2011b). Cholesterol level and statin use in Alzheimer disease II. Review of human trials and recommendations. JAMA Neurol. 68, 1385–1392. 10.1001/archneurol.2011.242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibuya Y., Chang C. C. Y., Chang T.-Y. (2015a). ACAT1/SOAT1 as a therapeutic target for Alzheimer’s disease. Future Med. Chem. 7, 2451–2467. 10.4155/fmc.15.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibuya Y., Niu Z., Bryleva E. Y., Harris B. T., Murphy S. R., Kheirollah A., et al. (2015b). Acyl-coenzyme A:cholesterol acyltransferase 1 blockage enhances autophagy in the neurons of triple transgenic Alzheimer’s disease mouse and reduces human P301L-tau content at the presymptomatic stage. Neurobiol. Aging 36, 2248–2259. 10.1016/j.neurobiolaging.2015.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibuya Y., Chang C. C., Huang L. H., Bryleva E. Y., Chang T. Y. (2014). Inhibiting ACAT1/SOAT1 in microglia stimulates autophagy-mediated lysosomal proteolysis and increases Aβ1- 42 clearance. J. Neurosci. 34, 14484–14501. 10.1523/JNEUROSCI.2567-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoog I., Hesse C., Aevarsson O., Landahl S., Wahlström J., Friedman P., et al. (1998). A population study of apoE genotype at the age of 85, relation to dementia, cerebrovascular disease and mortality. J. Neurol. Neurosurg. Psychiatry 64, 37–43. 10.1136/jnnp.64.1.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skrobot O. A., Black S. E., Chen C., DeCarli C., Erkinjuntti T., Ford G. A., et al. (2018). Progress toward standardized diagnosis of vascular cognitive impairment: guidelines from the Vascular Impairment of Cognition Classification Consensus Study. Alzheimers Dement. 14, 280–292. 10.1016/j.jalz.2017.09.007 [DOI] [PubMed] [Google Scholar]
- Slooter A. J. C., Cruts M., Ott A., Bots M. L., Witteman J. C. M., Hofman A., et al. (1999). The effect of APOE on dementia is not through atherosclerosis: the Rotterdam study. Neurology 53, 1593–1595. 10.1212/wnl.53.7.1593 [DOI] [PubMed] [Google Scholar]
- Slooter A. J., Tang M. X., van Duijn C. M., Stern Y., Ott A., Bell K., et al. (1997). Apolipoprotein E epsilon4 and the risk of dementia with stroke. A population-based investigation. JAMA 277, 818–821. 10.1001/jama.277.10.818 [DOI] [PubMed] [Google Scholar]
- Smith K. B., Kang P., Sabbagh M. N., Alzheimer’s Disease Neuroimaging Initiative . (2017). The effect of statins on rate of cognitive decline in mild cognitive impairment. Alzheimers Dement. 3, 149–156. 10.1016/j.trci.2017.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon A., Kivipelto M., Wolozin B., Zhou J., Witmer R. A. (2009). Midlife serum cholesterol and increased risk of Alzheimer’s and vascular dementia three decades later. Dement. Geriatr. Cogn. Disord. 28, 75–80. 10.1159/000231980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steenland K., Zhao L., Goldstein G. C., Levey A. I. (2013). Statins and cognitive decline in older adults with normal cognition or mild cognitive impairment. J. Am. Geriatr. Soc. 61, 1449–1455. 10.1111/jgs.12414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stelzmann R. A., Schnitzlein H. N., Murtagh F. R. (1995). An english translation of Alzheimer’s 1907 paper, “Über eine eigenartige Erkankung der Hirnrinde”. Clin. Anat. 8, 429–431. 10.1002/ca.980080612 [DOI] [PubMed] [Google Scholar]
- Strittmatter W. J., Saunders A. M., Schmechel D., Pericak-Vance M., Enghild J., Salvesen G. S., et al. (1993). Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc. Natl. Acad. Sci. U S A 90, 1977–1981. 10.1073/pnas.90.5.1977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suemoto C. K., Ferretti-Rebustini R. E. L., Rodriguez R. D., Leite R. E. P., Soterio L., Brucki S. M. D., et al. (2017). Neuropathological diagnoses and clinical correlates in older adults in Brazil: a cross-sectional study. PLoS Med. 14:e1002267. 10.1371/journal.pmed.1002267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao Q., Ang T. F. A., DeCarli C., Auerbach S. H., Devine S., Stein T. D., et al. (2018). Association of chronic low-grade inflammation with risk of Alzheimer disease in ApoE4 carriers. JAMA Netw. Open 1:e183597. 10.1001/jamanetworkopen.2018.3597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarantini S., Yabluchanskiy A., Csipo T., Fulop G., Kiss T., Balasubramanian P., et al. (2019). Treatment with the poly(ADP-ribose) polymerase inhibitor PJ-34 improves cerebromicrovascular endothelial function, neurovascular coupling responses and cognitive performance in aged mice, supporting the NAD+ depletion hypothesis of neurovascular aging. Geroscience 41, 533–542. 10.1007/s11357-019-00101-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry J. G., Howard G., Mercuri M., Bond M. G., Crouse 3rd J. R. (1996). Apolipoprotein E polymorphism is associated with segment-specific extracranial carotid artery intima-media thickening. Stroke 27, 1755–1759. 10.1161/01.str.27.10.1755 [DOI] [PubMed] [Google Scholar]
- Tian J., Shi J., Bailey K., Mann D. M. A. (2004). Relationships between arteriosclerosis, cerebral amyloid angiopathy and myelin loss from cerebral cortical white matter in Alzheimer’s disease. Neuropathol. Appl. Neurobiol. 30, 46–56. 10.1046/j.0305-1846.2003.00510.x [DOI] [PubMed] [Google Scholar]
- Tzioras M., Davies C., Newman A., Jackson R., Spires-Jones T. (2019). Invited review: APOE at the interface of inflammation, neurodegeneration and pathological protein spread in Alzheimer’s disease. Neuropathol. Appl. Neurobiol. 45, 327–346. 10.1111/nan.12529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ungvari Z., Tarantini S., Donato A. J., Galvan V., Csiszar A. (2018). Mechanisms of vascular aging. Circ. Res. 123, 849–867. 10.1161/CIRCRESAHA.118.311378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Flier W. W., Scheltens P. (2005). Epidemiology and risk factors of dementia. J. Neurol. Neurosurg. Psychiatry 76, v2–v7. 10.1136/jnnp.2005.082867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Kant R., Langness V. F., Herrera C. M., Williams D. A., Fong L. K., Leestemaker Y., et al. (2019). Cholesterol metabolism is a druggable axis that independently regulates tau and amyloid-β in iPSC-derived Alzheimer’s disease neurons. Cell Stem Cell 24, 363–375. 10.1016/j.stem.2018.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verheijen J., Sleegers K. (2018). Understanding Alzheimer disease at the interface between genetics and transcriptomics. Trends Genet. 34, 434–437. 10.1016/j.tig.2018.02.007 [DOI] [PubMed] [Google Scholar]
- Volcik K. A., Barkley R. A., Hutchinson R. G., Mosley T. H., Heiss G., Sharrett A. R., et al. (2006). Apolipoprotein E polymorphisms predict low density lipoprotein cholesterol levels and carotid artery wall thickness but not incident coronary heart disease in 12,491 ARIC study participants. Am. J. Epidemiol. 164, 342–348. 10.1093/aje/kwj202 [DOI] [PubMed] [Google Scholar]
- Wang J. C., Bennett M. (2012). Aging and atherosclerosis mechanisms, functional consequences, and potential therapeutics for cellular senescence. Circ. Res. 111, 245–259. 10.1161/CIRCRESAHA.111.261388 [DOI] [PubMed] [Google Scholar]
- Wang C., Najm R., Xu Q., Jeong D.-E., Walker D., Balestra M. E., et al. (2018). Gain of toxic apolipoprotein E4 effects in human iPSC-derived neurons is ameliorated by a small-molecule structure corrector. Nat. Med. 24, 647–657. 10.1038/s41591-018-0004-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei L. K., Au A., Menon S., Griffiths L. R., Kooi C. W., Irene L., et al. (2017). Polymorphisms of MTHFR, eNOS, ACE, AGT, ApoE, PON1, PDE4D, and ischemic stroke. J. Stroke Cerebrovasc. Dis. 26, 2482–2493. 10.1016/j.jstrokecerebrovasdis.2017.05.048 [DOI] [PubMed] [Google Scholar]
- Williams T., Borchelt D. R., Chakrabarty P. (2020). Therapeutic approaches targeting Apolipoprotein E function in Alzheimer’s disease. Mol. Neurodegen. 15:8. 10.1186/s13024-020-0358-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo T. S., Cutler D. J., Wingo A. P., Le N.-A., Rabinovici G. D., Miller B. L., et al. (2019). Association of early-onset Alzheimer disease with elevated low-density lipoprotein cholesterol levels and rare genetic coding variants of APOB. JAMA Neurol. 76, 809–817. 10.1001/jamaneurol.2019.0648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo A. P., Fan W., Duong D. M., Gerasimov E. S., Dammer E. B., Liu Y. (2020). Shared proteomic effects of cerebral atherosclerosis and Alzheimer’s disease on the human brain. Nat. Neurosci. 23, 696–700. 10.1038/s41593-020-0635-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkels H., Ehinger E., Vassallo M., Buscher K., Dinh H., Kobiyama K., et al. (2018). Atlas of the immune cell repertoire in mouse atherosclerosis defined by single-cell RNA-sequencing and mass cytometry. Circ. Res. 122, 1675–1688. 10.1161/CIRCRESAHA.117.312513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolk D. A., Dickerson B. C., Alzheimer’s Disease Neuroimaging Initiative . (2010). Apolipoprotein, E. (APOE) genotype has dissociable effects on memory and attentional-executive network function in Alzheimer’s disease. Proc. Natl. Acad. Sci. U S A 107, 10256–10261. 10.1073/pnas.1001412107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wollmer M. A., Streffer J. R., Tsolaki M., Grimaldi L. M. E., Lütjohann D., Thal D., et al. (2003). Genetic association of acyl-coenzyme A: cholesterol acyltransferase with cerebrospinal fluid cholesterol levels, brain amyloid load, and risk for Alzheimer’s disease. Mol. Psychiatry 8, 635–638. 10.1038/sj.mp.4001296 [DOI] [PubMed] [Google Scholar]
- Wolters F. J., Ikram M. A. (2019). Epidemiology of vascular dementia: nosology in a time of epiomics. Arterioscler. Thromb. Vasc. Biol. 39, 1542–1549. 10.1161/ATVBAHA.119.311908 [DOI] [PubMed] [Google Scholar]
- Wyss M. T., Magistretti P. J., Buck A., Weber B. (2011). Labeled acetate as a marker of astrocytic metabolism. J. Cereb. Blood Flow Metab. 31, 1668–1674. 10.1038/jcbfm.2011.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong M., Jiang H., Serrano J. R., Gonzales E. R., Wang C., Gratuze M., et al. (2021). APOE immunotherapy reduces cerebral amyloid angiopathy and amyloid plaques while improving cerebrovascular function. Sci. Transl. Med. 17:eabd7522. 10.1126/scitranslmed.abd7522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamauchi Y., Chang C. C., Hayashi M., Abe-Dohmae S., Reid P. C., Chang T. Y., et al. (2004). Intracellular cholesterol mobilization involved in the ABCA1/apolipoprotein mediated assembly of high-density lipoprotein in fibroblasts. J. Lipid Res. 45, 1943–1951. 10.1194/jlr.M400264-JLR200 [DOI] [PubMed] [Google Scholar]
- Yamazaki Y., Painter M. M., Bu G., Kanekiyo T. (2016). Apolipoprotein E as a therapeutic target in Alzheimer’s disease: a review of basic research and clinical evidence. CNS Drugs 30, 773–789. 10.1007/s40263-016-0361-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C., Hawkins K. E., Doré S., Candelario-Jalil E. (2019). Neuroinflammatory mechanisms of blood-brain barrier damage in ischemic stroke. Am. J. Physiol. Cell Physiol. 316, C135–C153. 10.1152/ajpcell.00136.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarchoan M., Xie S. X., Kling M. A., Toledo J. B., Wolk D. A., Lee E. B., et al. (2012). Cerebrovascular atherosclerosis correlates with Alzheimer pathology in neurodegenerative dementias. Brain 135, 3749–3756. 10.1093/brain/aws271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin J., Nielsen M., Carcione T., Li S., Shi J. (2019). Apolipoprotein E regulates mitochondrial function through the PGC-1α-sirtuin 3 pathway. Aging 11, 11148–11156. 10.18632/aging.102516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zambón D., Quintana M., Mata P., Alonso R., Benavent J., Cruz-Sánchez F., et al. (2010). Higher incidence of mild cognitive impairment in familial hypercholesterolemia. Am. J. Med. 123, 267–274. 10.1016/j.amjmed.2009.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zelcer N., Khanlou N., Clare R., Jiang Q., Reed-Geaghan E. G., Landreth G. E., et al. (2007). Attenuation of neuroinflammation and Alzheimer’s disease pathology by liver x receptors. Proc. Natl. Acad. Sci. U S A 104, 10601–10606. 10.1073/pnas.0701096104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zernecke A., Winkels H., Cochain C., Williams J. W., Wolf D., Soehnlein O., et al. (2020). Meta-analysis of leukocyte diversity in atherosclerotic mouse aortas. Circ. Res. 127, 402–426. 10.1161/CIRCRESAHA.120.316903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X.-Q., Even-Or O., Xu X., van Rosmalen M., Lim L., Gadde S., et al. (2014). Nanoparticles containing a liver X receptor agonist inhibit inflammation and atherosclerosis. Adv. Healthc. Mater. 4, 228–236. 10.1002/adhm.201400337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Z., Liang Y., Zhang X., Xu J., Lin J., Zhang R., et al. (2020). Low-density lipoprotein cholesterol and Alzheimer’s disease: a systematic review and meta-analysis. Front. Aging Neurosci. 12:5. 10.3389/fnagi.2020.00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlokovic B. V., Gottesman R. F., Bernstein K. E., Seshadri S., McKee A., Snyder H., et al. (2020). Vascular contributions to cognitive impairment and dementia (VCID): a report from the 2018 National Heart, Lung and Blood Institute and National Institute of Neurological Disorders and Stroke Workshop. Alzheimers Dement. 16, 1714–1733. 10.1002/alz.12157 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anatomy of cerebral arteries, including the (A,B) carotid arteries and (C,D) Circle of Willis (CoW), also shown on computed tomography arteriography (B,D). Illustrations adapted from Henry Gray’s Anatomy of the Human Body (1918), www.bartleby.com.