To the Editor:
Gas tamponade is commonly used at the end of vitrectomy for retinal detachment. A number of risk factors for retinal detachment surgery failure are reported; however, it is unknown whether larger gas bubbles are more effective in preventing retinal re-detachment [1].
Our aim was to explore the effect of day-1 vitreous cavity gas fill percentage on the outcomes of retinal detachment surgery. A retrospective review was performed using data from two Australian centres (The Canberra Hospital, and the Royal Victorian Eye and Ear Hospital). Only patients undergoing vitrectomy with gas tamponade for retinal detachment were included. Cases were identified from an online registry recently introduced at both institutions. Baseline features, operative details and outcome were prospectively recorded. Percentage gas fill of the vitreous cavity on postoperative day-1 (“gas fill”) was retrospectively collected from clinical notes, based on the respective surgeons’ estimate. The main outcome measure was stable retinal reattachment at 3-months postoperatively, without further need for retinal reattachment surgery. Postoperative gas fill was analysed as >=80% or <80%.
There were 445 cases of vitrectomy for rhegmatogenous retinal detachment included, a successful anatomical outcome was achieved in 399/445 (90%) and was similar at the two study sites (89.8% versus 89.6%). 364/445 (82%) eyes had a day-1 gas fill ≥80% (Fig. 1). Baseline characteristics for both fill groups are displayed in Table 1. We did not observe that expansile gas concentration (>25% SF6 or >15% C3F8) resulted in larger gas bubbles day 1 (data not shown).
Fig. 1. Graph displaying frequency.
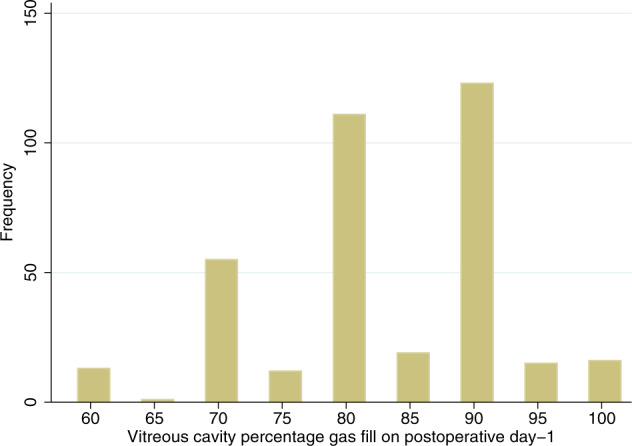
Vitreous cavity percentage gas fill on postoperative day-1.
Table 1.
Baseline characteristics and gas used, divided by each gas fill group, with outcomes.
| Baseline characteristic | Day-1 gas fill ≥80% |
Day-1 gas fill <80% |
P value |
|---|---|---|---|
| PVR ≥ grade C | 10/363 (2.8%) | 4/81 (4.9%) | 0.31 |
| Detachment >4 clock hours | 181/339 (53%) | 36/78 (46%) | 0.25 |
| Significant vitreous haemorrhage | 30/354 (8.5%) | 3/80 (3.8%) | 0.15 |
| Postoperative aphakia/pseudophakia | 121/363 (33%) | 34/81 (42%) | 0.14 |
| Macula-off detachment | 177/363 (49%) | 44/81 (54%) | 0.37 |
| Breaks in the lower third | 124/354 (35%) | 33/78 (42%) | 0.23 |
| Multiple tears | 190/294 (65%) | 36/71 (51%) | 0.03 |
| Recurrent detachment | 32/364 (8.8%) | 4/81 (4.9%) | 0.25 |
| Face-down posturing | 88/345 (25.5%) | 16/72 (22%) | 0.56 |
| Gas choice | |||
| SF6 used | 299/355 (84%) | 65/75 (87%) | |
| C3F8 used | 55/355 (15%) | 10/75 (13%) | |
| Air used | 1/355 (0.3%) | 0 | 0.80 |
| Expansile gas concentration used | 50/340 (15%) | 12/74 (16%) | 0.74 |
| Mean pre-operative acuity (letters) | 48 | 42 | 0.12 |
| Outcomes | |||
| Retinal reattachment | 325/364 (89%) | 74/81 (91%) | 0.58 |
| Adjusted Odds Ratioa | 0.81, 95% CI 0.33 to 2.03. P = 0.66 | ||
| Visual acuity (letters) | 59 | 59 | 0.99 |
| Adjusted differenceb | −0.3 letters, 95% CI −6.0 to +5.4. P = 0.92 | ||
aAdjusted odds of success for ≥80% gas fill vs. <80%. Adjusted for site of breaks (inferior vs. not), extent of detachment, gas used, PVR grade, number of previous detachment procedures, trainee surgeon, number of breaks and foveal status.
bDifference adjusted for pre-operative macular status and for post-operative lens status.
Eyes with gas fill ≥80% were not observed to have better outcomes than eyes with lesser gas fill. In eyes with ≥80% gas fill a successful outcome was achieved in 325/364 (89%), compared with 74/81 (91%) in eyes with <80% (P = 0.58). Eyes with inferior breaks were more likely to fail (15.3 vs. 7.6%, P = 0.012), however, we did not observe better gas fill to improve outcome in these eyes with inferior breaks (19/124 (15.3%) failure vs. 5/33 (15.2%), P = 0.98). After adjustment for site of breaks (inferior vs. not), extent of detachment, gas used, PVR grade, number of previous detachment procedures, trainee surgeon, number of breaks, and foveal status (attached vs. not), the adjusted odds ratio of success in eyes with ≥80% day-1 gas fill was 0.81 (95% CI 0.33 to 2.03, P = 0.66). The mean 3-month Snellen visual acuity was 59 letters in both groups (approximately 6/19, P = 0.99). After adjustment for pre-operative macular status and for postoperative lens status, better gas fill was not observed to have any effect on visual acuity outcome at 3 months (−0.3 LogMAR letter effect, 95% CI −6.0 to +5.4 letters, P = 0.92), nor visual acuity change (−4.3 LogMAR letter effect, 95% CI −11.4 to +2.8, P = 0.23).
We did not observe a difference in anatomical nor visual outcomes at 3 months between eyes with ≥80% fill compared with those with <80% vitreous gas fill day-1 postoperatively. The mechanism of action of gas tamponade in retinal detachment repair appears not to be related to bubble size, and may indeed be it’s effect on changing intraocular fluid currents [2]. It may not be necessary to use deliberately expansile bubbles with their attendant risk of elevated intraocular pressure [3]. Retinal reattachment with vitrectomy has in fact been performed without the use of tamponade by others [4, 5].
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/1/2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
- 1.Williamson TH, Lee EJ, Shunmugam M. Characteristics of rhegmatogenous retinal detachment and their relationship to success rates of surgery. Retin (Phila, Pa) 2014;34:1421–7. doi: 10.1097/IAE.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 2.Kuhn F, Aylward B. Rhegmatogenous retinal detachment: a reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014;51:15–31. doi: 10.1159/000355077. [DOI] [PubMed] [Google Scholar]
- 3.Williamson TH, Guillemaut JY, Hall SK, Hutter JC, Goddard T. Theoretical gas concentrations achieving 100% fill of the vitreous cavity in the postoperative period: a gas eye model study. Retin (Phila, Pa) 2018;38(Suppl 1):S60–4. doi: 10.1097/IAE.0000000000001963. [DOI] [PubMed] [Google Scholar]
- 4.Martinez-Castillo V, Zapata MA, Boixadera A, Fonollosa A, Garcia-Arumi J. Pars plana vitrectomy, laser retinopexy, and aqueous tamponade for pseudophakic rhegmatogenous retinal detachment. Ophthalmology. 2007;114:297–302. doi: 10.1016/j.ophtha.2006.07.037. [DOI] [PubMed] [Google Scholar]
- 5.Heriot WJ. Thermofusion of the retina with the RPE to seal tears during retinal detachment repair. Graefe’s Arch Clin Exp Ophthalmol. 2016;254:691–6. doi: 10.1007/s00417-016-3295-0. [DOI] [PubMed] [Google Scholar]


