To the Editor: Since the arrival of COVID-19, cases of telogen effluvium (TE) have substantially increased.1 In this study, we assess the influence of race, ethnicity, and comorbidities on the incidence of TE during the pandemic.
To analyze the occurrence of TE, the number of patients with this diagnosis were extracted from the combined patient volume evaluated by the dermatology departments of 8 safety-net hospitals in New York City. The incidence of TE between August 1, 2019, and February 29, 2020, (pre-pandemic) was compared with the incidence of this disorder between March 1, 2020, and October 1, 2020 (pandemic). Cases were filtered by COVID-19 positivity, demographics, and comorbidities. This study was exempted from IRB approval as only unidentifiable data was utilized (Slicer/Dicer, EPIC, WI).
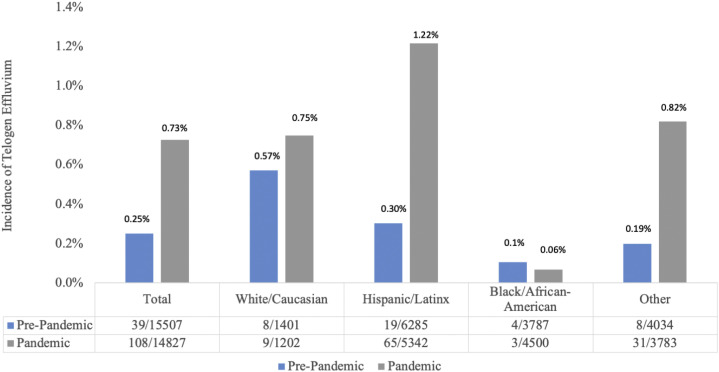
From March 1, 2020, to October 1, 2020, 108 patients were diagnosed with TE (10 positive and 98 negative or untested for COVID-19) compared with 39 patients from before the pandemic, corresponding to a nearly 3-fold increased incidence during the pandemic (Fig 1 ). Although the extent of illness among our COVID+ cohort is unknown, it is notable that all but 1 (9/10) had underlying medical conditions that portend a more serious presentation of SARS-CoV-22 (Table I ). A prior case series of 10 individuals with TE subsequent to COVID-19 similarly identified that a majority (8/10) had prior medical issues, suggesting that the presence of comorbidities in conjunction with COVID-19 positivity may increase one's risk of developing TE.1 A larger sample size is needed to confirm this association.
Fig 1.
Demographic distribution of the incidence of telogen effluvium (TE). Pre-pandemic is measured from August 1, 2019 to February 29, 2020. Pandemic is measured from March 1, 2020 to October 1, 2020. Total patients evaluated by the dermatology departments at Woodhull, Cumberland, Kings County, Elmhurst, Lincoln, Jacobi, Coney Island & Metropolitan Hospital Sites. Cases of TE/total patients evaluated by dermatology in each demographic.
Table I.
Characteristics of COVID-19+ patients diagnosed with telogen effluvium. COVID-19 infection confirmed by either PCR or serology, March 1, 2020, to October 1, 2020
 |
During the pandemic, the number of cases of TE in Caucasians (n = 9) was similar to that identified before the pandemic (n = 8) (Fig 1). However, cases of TE increased significantly in Hispanic (65 pandemic >19 pre-pandemic) and other non-White individuals (31 pandemic > 8 pre-pandemic) in line with the disproportionate effect of COVID-19 on minority populations. Unexpectedly, there were only 3 diagnoses of TE in Blacks, a demographic also severely impacted by the pandemic. A paucity of cases of TE in Blacks (n = 4) was similarly noted before the pandemic compared with all other groups. Limitations include the possibility of coding errors and potential for inconsistencies in the diagnostic criteria of TE among hospital sites.
Although TE is one of the most common types of nonscarring hair loss, there is remarkably limited data on the epidemiology of this disorder. Notably, telogen percentage, density, and growth rate of normal hair show substantial variability among ethnicities.3 The microstructural appearance differs as well. In Whites and Asians, hair lost in grooming tends to be full-length with an attached root, whereas in Blacks, the root is more commonly lacking and there is longitudinal fissuring in the shaft suggestive of breakage.4 Hair loss disorders can also demonstrate ethnic and racial disparities. Blacks, for instance, are at increased risk for cicatricial alopecia,5 a trend we have similarly observed in our population (Supplemental Fig 1 available via Mendeley at 10.17632/gpjzxt7f2f.1). This demographic may have a decreased risk for other types of hair loss, such as TE, which may contribute to the paucity of cases noted in this group. A larger sample size is needed to investigate this hypothesis. Further research exploring the development and diagnosis of TE in diverse populations is also warranted.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Exempt.
Reprints not available from the authors.
References
- 1.Mieczkowska K., Deutsch A., Borok J. Telogen effluvium: a sequela of COVID-19. Int J Dermatol. 2021;60(1):122–124. doi: 10.1111/ijd.15313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williamson E.J., Walker A.J., Bhaskaran K. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loussouarn G., Lozano I., Panhard S., Collaudin C., El Rawadi C., Genain G. Diversity in human hair growth, diameter, colour and shape. An in vivo study on young adults from 24 different ethnic groups observed in the five continents. Eur J Dermatol. 2016;26(2):144–154. doi: 10.1684/ejd.2015.2726. [DOI] [PubMed] [Google Scholar]
- 4.Khumalo N.P., Doe P.T., Dawber R.P., Ferguson D.J. What is normal black African hair? A light and scanning electron-microscopic study. J Am Acad Dermatol. 2000;43(5 Pt 1):814–820. doi: 10.1067/mjd.2000.107958. [DOI] [PubMed] [Google Scholar]
- 5.Malki L., Sarig O., Romano M.T. Variant PADI3 in central centrifugal cicatricial alopecia. N Engl J Med. 2019;380(9):833–841. doi: 10.1056/NEJMoa1816614. [DOI] [PubMed] [Google Scholar]