Abstract
The artery of Percheron (AOP) represents a rare anatomic variant of the posterior circulation. It is a solitary trunk that provides bilateral arterial supply to the rostral midbrain and paramedian thalamus. AOP infarction presentation varies, most often presents with altered mental status, memory impairment, and supranuclear vertical gaze palsy. Diagnosis of the AOP infarct is most often missed in the initial CT scan. A majority of these diagnoses are made outside the window of thrombolytic treatment for ischemic stroke.
We report a case of a 67-year old male with a history of well-managed diabetes mellitus type 2 and hypertension, presented in the ER sudden onset severe drowsiness. On a physical exam, we found left pupil dilation and left eye deviation. Initial CT scan showed no pathological changes. The diagnosis was made on the third day of hospitalization via an MRI. Our case highlights the unusual presentation and that an absence of evidence of AOP infarction in CT scan does not exclude its diagnosis. The artery of the Percheron infarct requires a comprehensive clinical and radiological examination.
Keywords: Infarction of the Percheron artery, Paramedian arteries, Bilateral infarction, Diagnostic imaging, Ischemic stroke
Introduction
Thalami are egg-shaped, paired, symmetrical, midline structures of the diencephalon composed mainly of gray matter. Its anatomical location is between the cerebral cortex and midbrain. Thalamus consists of a series of nuclei containing excitatory and inhibitory neurons that function as a filtering hub between different subcortical structures and the cerebral cortex. The thalamus is involved in numerous functions, including processing and relaying sensory and motor signals, arousal, awareness and activity levels, pain regulation, sleep and wakefulness states, emotions, and memory. Moreover, the roles of individual nuclei of the paramedian thalamic region are yet to be explored. To date, reduced levels of consciousness, apathy, amnesia, aphasia, dysarthria, and disinhibited behaviors have been described as sequelae of bilateral infarction paramedian thalamic region [1,2].
Gérard Percheron first described the artery of Percheron (AOP) in 1973. It is a single arterial trunk originating from either proximal posterior cerebral artery and nourishes the bilateral paramedian thalamus and rostral midbrain [3]. AOP is known to exist in about 33 percent of the population, with independent hemispheric vascularization in most individuals [4]. Infarction of the Percheron artery is most often presented with a triad of symptoms, including altered consciousness, memory deficits, and supranuclear vertical gaze palsies. Infarction of the Percheron artery is most often presented with a triad of symptoms, including altered consciousness, memory deficits, and supranuclear vertical gaze palsies. Rare manifestations may include severe bradycardia, parkinsonism, and seizures. AOP infarction is an important diagnostic consideration when presented with fluctuating consciousness, especially with a normal initial CT scan. MRI is currently the gold standard to demonstrate bilateral paramedian thalamic infarction [5].
We report a case of a patient admitted for severe somnolence without apparent cause and normal early computed tomography (CT). A new brain MRI 3 days later revealed a bilateral infarction affection paramedian thalamus and midbrain. Even though AOP stroke demonstrates a characteristic pattern of bilateral paramedian thalamic infarction with or without midbrain involvement, it's vague clinical presentations, wide differentials, and poor visualization through imaging are potential barriers to timely diagnosis [6]. And patients frequently miss the window time for acute ischemic stroke management.
Case presentation
A 67-year-old man presented to the emergency department with severe drowsiness. He had a history of well-controlled type II diabetes mellitus and hypertension. Physical examination revealed a dilated left pupil and a left eye deviation. His vitals were stable without any orthostatic changes. Neurologic and other system examinations were within normal limits. An emergency head CT was obtained, it revealed no apparent pathological changes. He was admitted to the Neurology Clinic for observation.
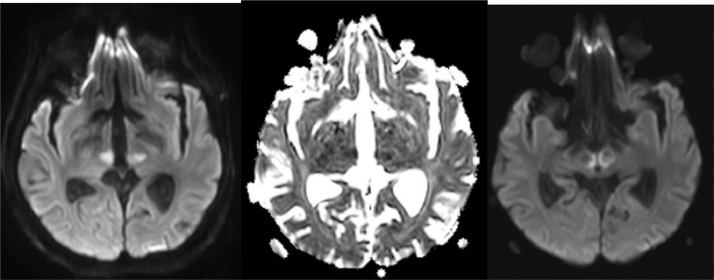
Due to a lack of typical clinical and imaging findings associated with strokes, but the persistence of the ophthalmologic signs and consciousness disturbances, a head MRI was ordered on the third day of hospitalization. It showed symmetrical lesions in the paramedian thalamus and midbrain, in the territory of the penetrating arteries. These lesions presented with hyperintensity in FLAIR and T2 sequence and an abnormal restriction of water diffusion on diffusion-weighted imaging (DWI), and a low apparent diffusion coefficient (ADC) (Fig. 2, Fig. 3, Fig. 4). The findings above confirmed the diagnosis of an acute infarction of the artery of Percheron. Late diagnosis, due to the atypical and at times bizarre clinical presentation and lack of CT anomalies, is common in this type of ischemic stroke.
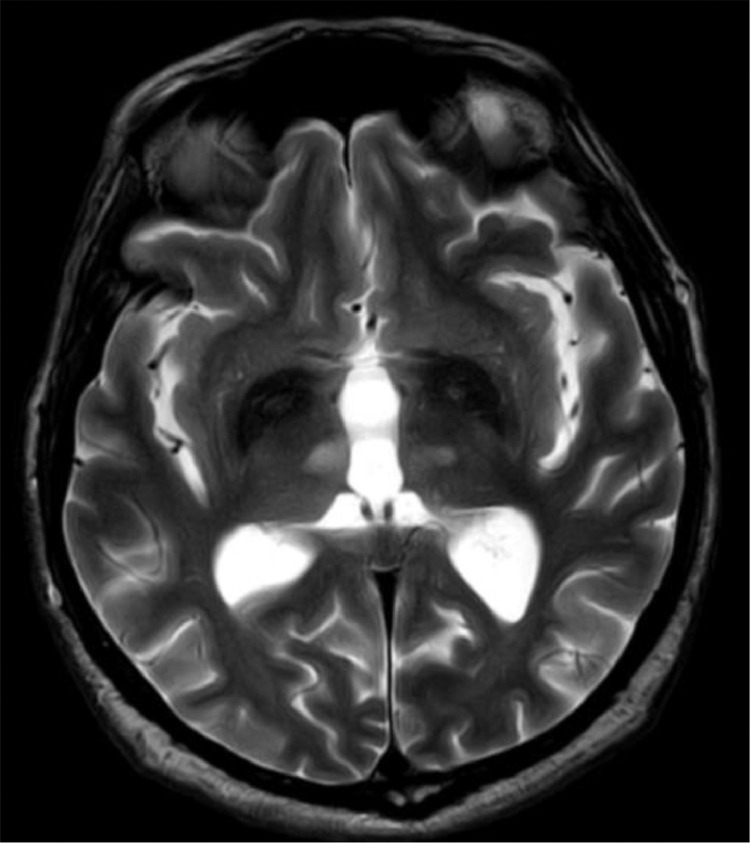
Fig. 2.
Axial T2-weighted image shows symmetrical hyperintense lesions presented in the paramedial thalamus.
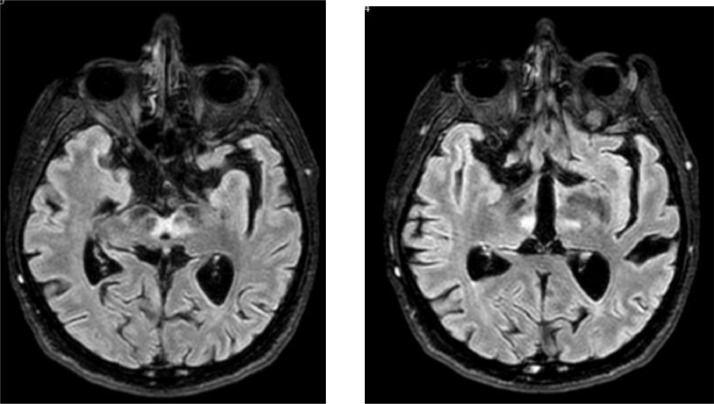
Fig. 3.
FLAIR hyperintense signals demonstrate bilateral paramedian thalami and paramedial mesencephalon—in the territory of the penetrating arteries.
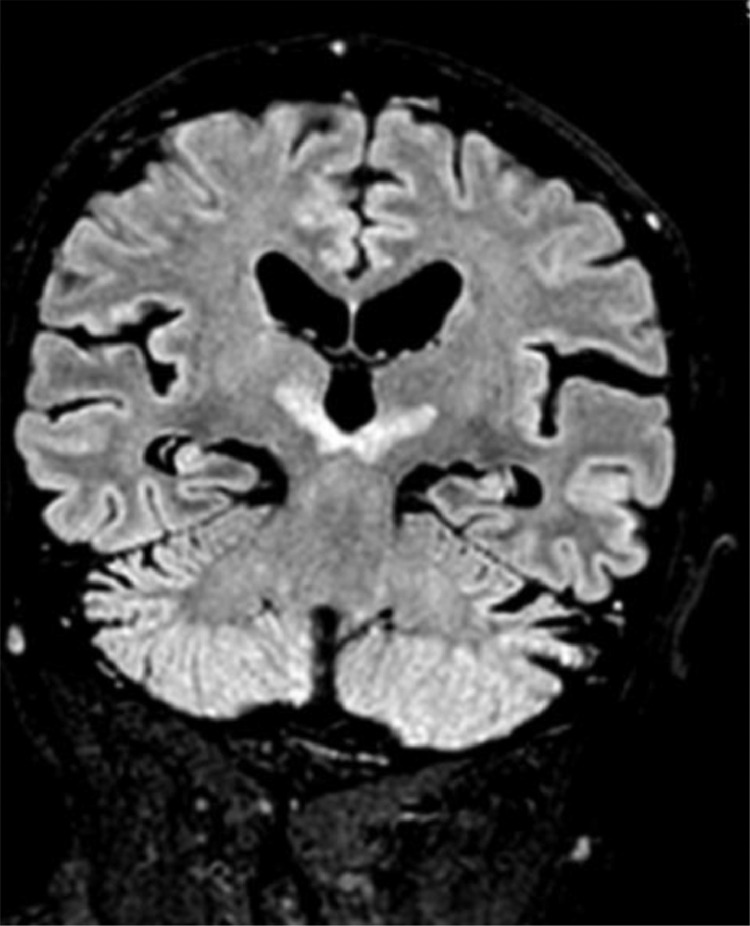
Fig. 4.
Coronal FLAIR sequence presenting hyperintense symmetrical lesions presented in the paramedial thalamus.
Discussion
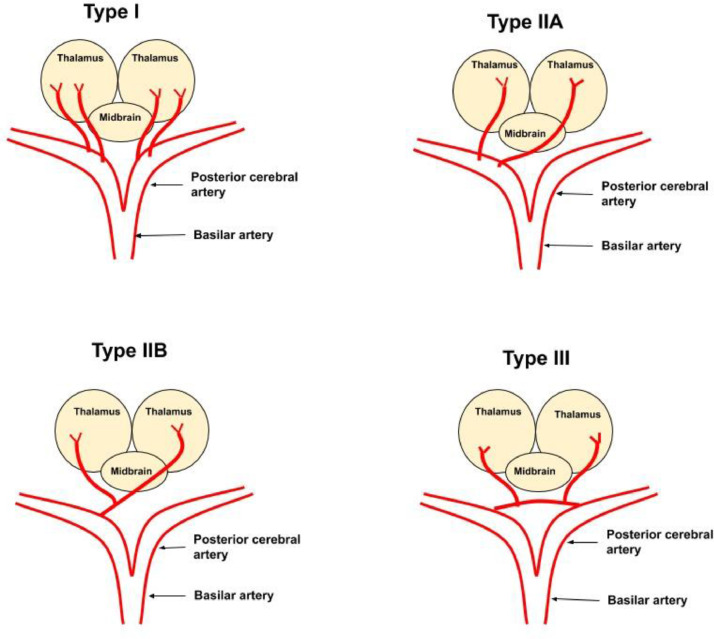
Artery of Percheron (AOP) is a solitary arterial trunk from one of either proximal segments of the posterior cerebral artery [7], [8], [9]. It perfuses the bilateral paramedian thalami and, most often, the rostral midbrain [7], [8], [9]. The artery of Percheron is one of the several anatomic variants of thalamic artery supply. Artery of Percheron infarction is one of the uncommon variants of ischemic stroke. Identifying AOP infarction is essential to detect early to initiate an ischemic stroke management algorithm (Fig. 1).
Fig. 1.
Four neurovascular anatomical variants have been described for the thalamus and midbrain [7], [8], [9]. Type I is the most frequent, where 2 paramedian arteries arise from the proximal, that is, P1 segment of each posterior cerebral artery. In type IIa both paramedian arteries arising from the (P1 segment) of either the left or the right posterior cerebral artery. Type IIb refers to the Artery of Percheron, a single trunk originating unilaterally from one of the (P1 segment) posterior cerebral arteries and bifurcating to supply the paramedian thalamus and bilateral rostral midbrain. In contrast, type III refers to the existence of a communicating artery between the proximal aspect (P1 segments) of both the left and right posterior cerebral arteries, from which the paramedian arteries originate [2,10].
Occlusion of the artery of Percheron causes a bilateral paramedian thalamic infarction with or without anterior thalamic and/or midbrain involvement [8]. These patterns correlate with the clinical presentation. The classic triad of a bilateral paramedian thalamic infarction consists of altered mental status ranging from drowsiness and confusion to coma, vertical gaze palsy, and memory impairment [7], [8], [9]. Other manifestations such as severe cognitive impairment, amnesia, inappropriate social conduct, and apathy have also been reported [9]. Involvement of the anterior thalamus is associated with severe memory deficits [8]. In contrast, rostral midbrain involvement may be accompanied by signs frequently encountered in strokes, including aphasia, dysarthria, oculomotor disturbance, hemiplegia, cerebellar ataxia, and movement disorders [7], [8], [9]. Patients may present with seizures or Korsakoff-like psychosis and confabulation [11].
Four patterns of AOP infarction in neuroimaging have been described so far, and bilateral paramedian thalamic region involvement is common for each pattern [8]. Involvement of bilateral paramedian thalami with midbrain is the commonest affecting up to 43% of cases. In comparison, bilateral paramedian thalamic infarction without midbrain is the second commonest and has been reported in 38% of cases. The third pattern has been reported in 14% of cases and describes the infarction anterior thalamus and midbrain along with bilateral paramedian thalami. Infarction involving the anterior thalamus without the midbrain is the rarest and has been reported in only 5% of cases. Several studies report MRI to be the most sensitive diagnostic technique. Lazzaro et al. described the midbrain "V sign," a hypertensive signal observed on FLAIR and DWI, a pathognomonic sign of 67% sensitivity, to detect AOP infarction [12]. Conventional angiography does not yield Percheron arterial variant visualization as of its small size. However, digital subtraction angiography can be an effective and alternative angiographic technique for detecting AOP [6,13].
As with any ischemic stroke, the most effective treatment for AOP infarction is thrombolytic therapy, when possible to administer within the therapeutic window (4.5-hour). This signifies the necessity of prompt diagnosis to maximize therapeutic efficacy. The first known case treated with thrombolytic therapy via catheterization demonstrated complete recovery with no gaze palsy or eye deviation [14]. Likewise, thrombolytic treatment should be maintained at a strategic distance from patients with cerebral hemorrhage found on CT or MRI. Cassourret et al. has reported a case where a patient received intravenous heparin 2 days following onset of unconsciousness, dysarthria. The patient demonstrated significant cognitive and motor improvement with partial memory deficit [10]. However, many nonemergent cases have been reported to manage conservatively and were monitored clinically and radiologically following being placed for rehabilitation therapy [13].
Artery of Percheron infarction poses a potential diagnostic challenge due to its elusive clinical presentation and the typical lack of CT imaging anomalies. The small size of the AOP may render the visualization of the vessel and possible occlusions difficult, in conventional imaging modalities such as CT and MRI, [Fig. 2, Fig. 3] further contributing to delays in the diagnosis of AOP infarction [15]. Delays in performing an MRI result in a late diagnosis, significantly impacting the management and prognosis of these patients, as was the case of our patient. His hypertension and type II diabetes mellitus may have contributed as predisposing factors.
This case report emphasizes the necessity of recognizing these clinical patterns and considering AOP infarction in the diagnostic consideration of patients presenting with acute neuropsychological and ophthalmological signs, disturbances of consciousness, or other atypical and otherwise inexplicable neurological symptoms Fig. 5.
Fig. 5.
In the sequences mentioned above lesions have hyperintensity in FLAIR and T2-weighted images while presenting water diffusion restriction in DWI- ADC hereby findings indicate—confirm diagnosis of Percheron artery infarction.
Conclusion
Patient consent
This is to state that I give my full permission for the publication, reproduction, broadcast and other use of photographs, recordings and other audio-visual material of myself (including of my face) and textual material (case histories) in all editions of the above-named product and in any other publication (including books, journals, CD-ROMs, online and internet), as well as in any advertising or promotional material for such product or publications.
I declare, in consequence of granting this permission, that I have no claim on ground of breach of confidence or any other ground in any legal system against—Juna Musa—and its agents, publishers, successors, and assigns in respect of such use of the photograph(s) and textual material (case histories).
I hereby agree to release and discharge Juna Musa and any editors or other contributors and their agents, publishers, successors and assigns from any and all claims, demands or causes of action that I may now have or may hereafter have for libel, defamation, invasion of privacy, copyright or moral rights or violation of any other rights arising out of or relating to any use of my image or case history.
References
- 1.Carrera E, Bogousslavsky J. The thalamus and behavior: effects of anatomically distinct strokes. Neurology. 2006;66(12):1817–1823. doi: 10.1212/01.wnl.0000219679.95223.4c. [DOI] [PubMed] [Google Scholar]
- 2.Khanni JL, Casale JA, Koek AY, Del Pozo PHE, Espinosa PS. Artery of percheron infarct: an acute diagnostic challenge with a spectrum of clinical presentations. Cureus. 2018;10(9):e3276. doi: 10.7759/cureus.3276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Percheron G. The anatomy of the arterial supply of the human thalamus and its use for the interpretation of the thalamic vascular pathology. Z Neurol. 1973;205(1):1–13. doi: 10.1007/BF00315956. [DOI] [PubMed] [Google Scholar]
- 4.Aysun U. Variations in the origin of the thalamoperforating arteries. J Clin Neurosci. 2007;(2):134–137. doi: 10.1016/j.jocn.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 5.Snyder HE, Ali S, Sue J, Unsal A, Fong C, Deng Z. Artery of Percheron infarction with persistent amnesia: a case report of bilateral paramedian thalamic syndrome. BMC Neurol. 2020;20(1):370. doi: 10.1186/s12883-020-01949-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kheiralla O, Alghamdi S, Aljondi R, Tajaldeen A, Bakheet AO. Artery of Percheron infarction: a characteristic pattern of ischemia and variable clinical presentation: a literature review. Curr Med Imaging. 2020 doi: 10.2174/1573405616666201130095801. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Khanni JL, Casale JA, Koek AY, Espinosa PS. Artery of Percheron infarct: an acute diagnostic challenge with a spectrum of clinical presentations. Cureus. 2018;10(9):e3276. doi: 10.7759/cureus.3276759/cureus.3276. 10 Sep. 2018, doi:10. Khanni, Javed L et al. “Artery of Percheron Infarct: An Acute Diagnostic Challenge with a Spectrum of Clinical Presentations.” Cureus vol. 10,9 e3276. 10 Sep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lazzaro NA, Wright B, Castillo M, Fischbein N.J, Glastonbury C.M, Hildenbrand P.G. Artery of Percheron infarction: imaging patterns and clinical spectrum. AJNR Am J Neuroradiol. 2010;31(7):1283–1289. doi: 10.3174/ajnr.a2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turner J, Richardson T, Kane I, Vundavalli S. Decreased consciousness: bilateral thalamic infarction and its relation to the artery of Percheron. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-201848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cassourret G, Prunet B, Sbardella F, Bordes J, Maurin O, Boret H. Ischemic stroke of the artery of Percheron with normal initial MRI: a case report. Case Rep Med. 2010 doi: 10.1155/2010/425734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou Y, Fox D, Anand A, Elhaj A, Kapoor A, Najibi F. Artery of Percheron infarction as an unusual cause of Korsakoff’s syndrome. Case reports in neurological medicine. 2015;((2015): 927809.) doi: 10.1055/2015/927809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lazzaro NA, Wright B, Castillo M, Fischbein NJ, Glastonbury CM, Hildenbrand PG. Artery of Percheron infarction: imaging patterns and clinical spectrum. AJNR Am J Neuroradiol. 2010;31(7):1283–1289. doi: 10.3174/ajnr.A2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li X, Agarwal N, Hansberry DR, Prestigiacomo CJ, Gandhi CD. Contemporary therapeutic strategies for occlusion of the artery of Percheron: a review of the literature. J Neurointerv Surg. 2015;7(2):95–98. doi: 10.1136/neurintsurg-2013-010913. [DOI] [PubMed] [Google Scholar]
- 14.Kostanian V, Cramer SC. Artery of Percheron thrombolysis. AJNR Am J Neuroradiol. 2007;28(5):870–871. [PMC free article] [PubMed] [Google Scholar]
- 15.Kheiralla OAM. Artery of Percheron infarction a rare anatomical variant and a diagnostic challenge: case report. Radiol Case Rep. 2020;16(1):22–29. doi: 10.1016/j.radcr.2020.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]