Highlights
-
•
Common Hepatic Artery pseudoaneurysm after total gastrectomy is uncommon and can be devastating.
-
•
We report a case of a ruptured common hepatic artery pseudoaneurysm who presented with massive gastrointestinal bleeding.
-
•
Early assessment with CT angiography followed by early appropriate treatment is life-saving.
Keywords: Common hepatic artery, Embolization, Gastrectomy, Pseudoaneurysm
Abstract
Introduction and importance
Common Hepatic Artery (CHA) Pseudoaneurysm is a rare entity, attributed to infections, trauma, and upper abdominal surgery. Most cases occur after biliary and pancreatic surgery. CHA pseudoaneurysm after total gastrectomy is uncommon and can be devastating.
Case presentation
A 58-years male who underwent D2 total gastrectomy for gastric carcinoma ten days ago, presented with hematemesis, epigastric pain, and a history of melaena. After admission, upper gastrointestinal endoscopy showed a clot at the jejunojejunostomy site. Computed tomography with angiography was diagnostic of pseudoaneurysm of CHA located inferiorly. Coil embolization of CHA was done and the patient improved.
Clinical discussion
Pseudoaneurysm of the common hepatic artery is a serious complication after abdominal surgery. Only a few cases have been reported with similar symptoms related to gastrointestinal bleeding following various upper abdominal surgeries. Coil embolization is a gold standard technique with a high success rate.
Conclusion
CHA pseudoaneurysm is a dreadful potential complication of abdominal surgery including gastrectomy. Early recognition and emergency management of CHA pseudoaneurysm are crucial for a favorable outcome for patients with bleeding from CHA aneurysm.
1. Introduction
Visceral artery aneurysms including pseudoaneurysms are rare but potentially fatal clinical entities with an estimated prevalence of 0.1–2% [1,2]. The incidence of hepatic artery aneurysm is uncommon and is at 0.002% with approximately 50% being the hepatic artery pseudoaneurysms [3].
Infections, trauma, and surgical interventions like the upper abdominal surgeries are attributed as the cause of pseudoaneurysm. Most occur after biliary and pancreatic surgery [4]. Common hepatic artery pseudoaneurysm after total gastrectomy is rare. We report a case of a patient with a ruptured common hepatic artery pseudoaneurysm following a total gastrectomy who presented with massive gastrointestinal bleeding. This report has been written in line with SCARE guidelines [5].
2. Presentation of case
A 58-year-old male, a chronic smoker and alcoholic with hypertension presented in the emergency of Tribhuvan University Teaching Hospital with multiple episodes of hematemesis, dizziness, and pain in the epigastric region for a few hours with a history of melaena and low-grade fever for three days. There was no loss of consciousness, altered sensorium, and a decrease in urine output. Ten days before the presentation, the patient had undergone D2 total gastrectomy with Roux-en-Y esophagojejunostomy for carcinoma stomach. Also, there were multiple episodes of gastrointestinal bleed post-surgery managed at another center and then transferred to our center. There was no history of intake of anticoagulants, family history of similar illness or bleeding disorder in the past.
On examination, he was pale, cold, clammy periphery with a blood pressure of 110/60 mmHg, pulse rate of 120 beats per minute, respiratory rate of 24 breaths per minute, and oxygen saturation of 85%. The abdomen was flat, there was mild tenderness in the epigastric region without peritonitis or organomegaly. On investigations, he had a hemoglobin of 9.7 g per deciliter, platelet count was 545,000/mm3, blood sugar was 9.5 millimole per liter, total bilirubin 24 micromole per-liter, with total protein 49 g per liter, and albumin 25 g per liter. After the initial resuscitation and stabilization with fluids, Vitamin K, octreotide, and tranexamic acid, upper gastrointestinal endoscopy revealed clots at the jejunojejunostomy site with oozing as shown in Fig. 1. Ultrasonography of abdomen and pelvis showed gallbladder sludge, bilateral mild pleural effusion, and minimal ascites. The findings of the CECT abdomen with CT angiography showed patent esophagojejunostomy anastomosis and pseudoaneurysm arising from common hepatic artery inferiorly (Fig. 2, Fig. 3).
Fig. 1.
Upper GI endoscopy a) shows clot at jejunojejunostomy site with oozing b) intact jejunal limb and c) intact esophagojejunostomy site.
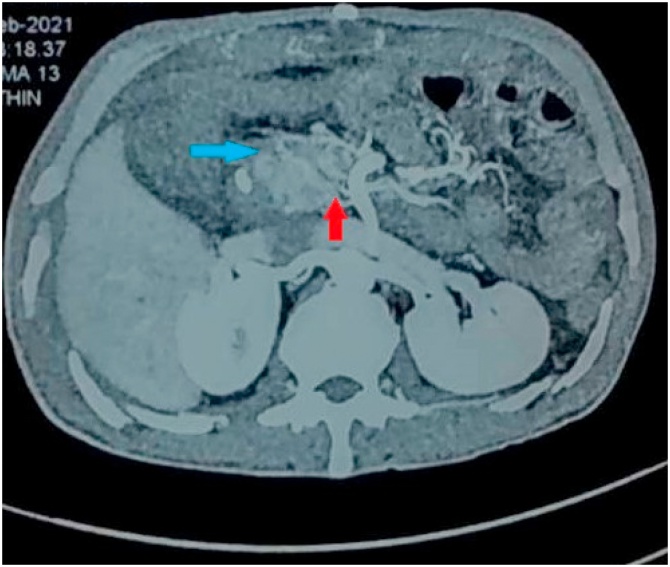
Fig. 2.
CECT abdomen and pelvis showed patent uncomplicated esophagojejunostomy anastomosis with saccular contrast filled outpouching located inferiorly of CHA (red arrow) with hyperdense contents contiguous with lesion in arterial phase (blue arrow).
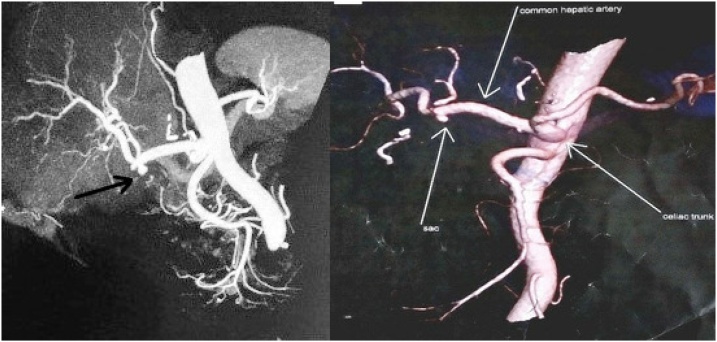
Fig. 3.
CT angiography of celiac trunk showing sac or protuberance (pseudoaneurysm) in the inferior section of CHA (arrow).
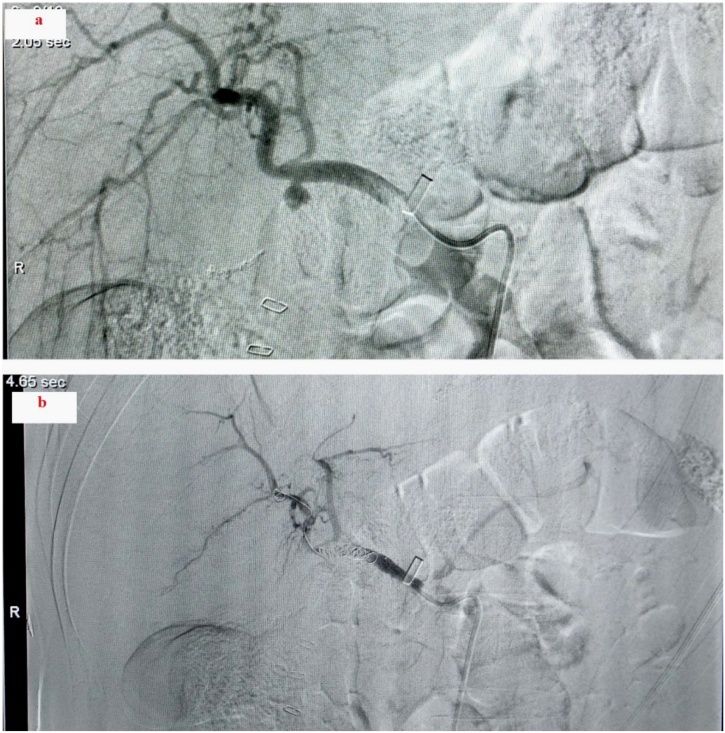
The patient was treated medically before the pre-operative procedure. The pseudoaneurysm was embolized with the coil by a team of interventional radiologists. Under aseptic conditions under fluoroscopic guidance, after accessing the celiac trunk with 5 F Simmon angiographic catheter through right common femoral access, angiogram showed pseudoaneurysm arising from the common hepatic artery. Due to the non-availability of appropriate size covered stent and falling hemoglobin, it was decided to sacrifice the hepatic artery with the known risk of hepatic ischemia. The neck of the pseudoaneurysm was crossed with a 2.1 F microcatheter and embolization of the parent artery was done distal and proximal to the pseudoaneurysm neck. Check angiogram showed complete occlusion of CHA and non-opacification of the pseudoaneurysm (Fig. 4).
Fig. 4.
Coil embolization a) before and b) after coil embolization treatment of the common hepatic pseudoaneurysm.
Hemoglobin level, blood pressure, and pulse rate improved after embolization. Though the liver enzymes were elevated for a few days following the intervention, however, normalized in seven days following the procedure. The patient is on follow-up, doing well, and satisfied with treatment.
3. Discussion
This case presents symptomatic ruptured pseudoaneurysm of common hepatic artery post gastrectomy which was successfully managed. Only about 2–4% of all cases experience postoperative bleeding after radical gastrectomy which is a serious surgical complication and can be lethal if not intervened on time [[6], [7], [8]].
The right hepatic artery is the most frequently involved artery for the development of pseudoaneurysm (87% of the cases) while the cystic artery involves few (7.9% of cases) [9]. The pseudoaneurysm in the CHA as seen in this case is rare. The etiology of pseudoaneurysm is mainly iatrogenic. Surgical procedure causing mechanical vascular injuries during the surgical procedure of mostly malignancy and pancreatic enzymes, biliary spillage or enteric fistula with intra-abdominal abscess and sepsis causing digestion of arterial vessels may be possible explanations. Most of the pseudoaneurysm occurs after hepatobiliary and pancreatic surgery and occurrence after gastric surgery is uncommon [10,11]. Our patient had undergone a total radical gastrectomy for a carcinoma stomach.
Nonspecific abdominal pain with or without symptoms of gastrointestinal bleeding like hematemesis, melaena, hematochezia is the common presentation while some maybe even asymptomatic [12]. Other subtle signs like fatigue, nausea, and back pain are often ignored but can conceal this alarming entity [13].
Patients can present with complications like intraperitoneal or retroperitoneal hemorrhage, rupture into GI tract, venous, portal, or biliary system, and hemorrhagic shock depending on the location of the pseudoaneurysm [14,15]. A gradual fall in hemoglobin or low-grade fever lasting for weeks after abdominal surgery should raise a suspicion of sepsis and pseudoaneurysm formation [16]. Our patient had gastrointestinal bleeding, features of hemorrhagic shock on presentation alongside low hemoglobin in the background of low-grade fever following total gastrectomy. The absence of apparent anastomotic leakage, pancreatic enzymes, and bile spillage with no intra-abdominal abscess raised the suspicion of sepsis or mechanical injury during surgery in our case.
Upper GI endoscopy is a useful diagnostic tool to detect clots, hemorrhages indicated after post-operative intraluminal bleeds, which in our case showed clots at the jejunojejunostomy site [17]. Imaging is often needed to find the exact pathology and diagnosis of the pseudoaneurysm, usually, a CT angiography which shows focal arterial disruption and inflammation bordering irregular aneurysmal walls suggest pseudoaneurysm [1,18,19]. In our case, various diagnostic modalities lead to the diagnosis of the pseudoaneurysm.
As pseudoaneurysm are lethal, early diagnosis and management form the cornerstone for improving a patient's prognosis [16]. Embolization of the pseudoaneurysm is considered a gold standard technique with a very high success rate (approximating 94.5%) and with no major complications, though various treatment modalities have been suggested. Blocking the sac or vessel with emboli agents or coils or embolizing the proximal and distal part of the vessel forming pseudoaneurysm, if blocking is ineffective are techniques used to perform embolization of the pseudoaneurysm [9]. Possible complications of embolization include hepatic necrosis, liver rupture, abscess formation, sepsis, jaundice, hematoma formation, ascites, and gallbladder necrosis [20]. However, owing to the fact that the portal system is the major vascular supply to the liver, occlusion of the hepatic artery is less likely to cause significant hepatic ischemia [13]. Successful coil embolization of the CHA was done by an interventional radiologist with no complications in this case.
4. Conclusions
Common hepatic artery pseudoaneurysm is rare but a possible postoperative complication after abdominal surgery including gastrectomy which needs to be considered. As it represents an emergency, early recognition of symptoms should prompt the clinicians to suspicion of the entity. CT angiography followed by early appropriate treatment is life-saving.
Declaration of Competing Interest
The authors report no declarations of interest.
Sources of funding
None.
Ethical approval
Nothing to declare.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Sanjeev Kharel (SK), Paleswan Joshi Lakhey (PJL) and Ajit Thapa (AT) = Study concept, Data collection, surgical therapy for the patient and operating radiologist.
Sanjeev Kharel (SK) and Suraj Shrestha (SS) = Writing - original draft preparation.
NG (Nitin Gyawali), Narendra Maharjan (NM) and Bishnu Prasad Kandel (BPK) = Editing and writing.
Paleswan Joshi Lakhey (PJL) = Senior author and manuscript reviewer.
All the authors read and approved the final manuscript.
Registration of research studies
Not applicable.
Guarantor
Sanjeev Kharel accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Note
No patient or author details are included in the figures.
Acknowledgment
None.
Contributor Information
Sanjeev Kharel, Email: Kharel_sanjeev@iom.edu.np.
Suraj Shrestha, Email: multisurazz@gmail.com.
Nitin Gyawali, Email: nitin.gyawali@gmail.com.
Narendra Maharjan, Email: narendramaharjancms@gmail.com.
Ajit Thapa, Email: drajitthapa@gmail.com.
Bishnu Prasad Kandel, Email: drkandel@hotmail.com.
Paleswan Joshi Lakhey, Email: lakheypj@gmail.com.
References
- 1.Tulsyan N., Kashyap V.S., Greenberg R.K. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J. Vasc. Surg. 2007;45(2):276–283. doi: 10.1016/j.jvs.2006.10.049. [DOI] [PubMed] [Google Scholar]
- 2.Berceli S.A. Hepatic and splenic artery aneurysms. Semin. Vasc. Surg. 2005;18(4):196–201. doi: 10.1053/j.semvascsurg.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 3.Abbas M.A., Fowl R.J., Stone W.M. Hepatic artery aneurysm: factors that predict complications. J. Vasc. Surg. 2003;38(1):41–45. doi: 10.1016/s0741-5214(03)00090-9. [DOI] [PubMed] [Google Scholar]
- 4.Clark E.T., Gewertz B.L. Intermittent ischemia potentiates intestinal reperfusion injury. J. Vasc. Surg. 1991;13(5):601–606. doi: 10.1016/0741-5214(91)90342-r. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;(84):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Kim M.C., Kim W., Kim H.H. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale Korean multicenter study. Ann. Surg. Oncol. 2008;15(10):2692–2700. doi: 10.1245/s10434-008-0075-z. [DOI] [PubMed] [Google Scholar]
- 7.Park D.J., Lee H.-J., Kim H.-H., Yang H.-K., Lee K.U., Choe K.J. Predictors of operative morbidity and mortality in gastric cancer surgery. Br. J. Surg. 2005;92(9):1099–1102. doi: 10.1002/bjs.4952. [DOI] [PubMed] [Google Scholar]
- 8.Jeong O., Park Y.K., Ryu S.Y., Kim D.Y., Kim H.K., Jeong M.R. Predisposing factors and management of postoperative bleeding after radical gastrectomy for gastric carcinoma. Surg. Today. 2011;41(3):363–368. doi: 10.1007/s00595-010-4284-2. [DOI] [PubMed] [Google Scholar]
- 9.Machado N., Al-Zadjali A., Kakaria A., Younus S., Rahim M., Al-Sukaiti R. Hepatic or cystic artery pseudoaneurysms following a laparoscopic cholecystectomy: literature review of aetiopathogenesis, presentation, diagnosis and management. Sultan Qaboos Univ. Med. J. 2017;17(2):e135–e146. doi: 10.18295/squmj.2016.17.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Z., Jie Z., Liu Y., Xie X. Management of delayed hemorrhage following radical gastrectomy for gastric carcinoma patients. Hepatogastroenterology. 2012;59(September (118)):2016–2019. doi: 10.5754/hge11825. [DOI] [PubMed] [Google Scholar]
- 11.Song W., Yuan Y., Peng J. The delayed massive hemorrhage after gastrectomy in patients with gastric cancer: characteristics, management opinions and risk factors. Eur. J. Surg. Oncol. (EJSO) 2014;40(10):1299–1306. doi: 10.1016/j.ejso.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Zhao J.-C., Lu S.-C., Yan L.-N. Incidence and treatment of hepatic artery complications after orthotopic liver transplantation. World J. Gastroenterol. 2003;9(12):2853–2855. doi: 10.3748/wjg.v9.i12.2853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mohanty S., Mukhopadhyay S., Yusuf J., Tyagi S. Emergency hepatic artery embolization in a patient with post-traumatic ruptured hepatic artery pseudoaneurysm. J. Emerg. Trauma Shock. 2014;7(3):246–247. doi: 10.4103/0974-2700.136878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volpi M.A., Voliovici E., Pinato F. Pseudoaneurysm of the gastroduodenal artery secondary to chronic pancreatitis. Ann. Vasc. Surg. 2010;24(8) doi: 10.1016/j.avsg.2010.03.034. 1136.e7-e1136.e11. [DOI] [PubMed] [Google Scholar]
- 15.Shawky M.S., Tan J., French R. Gastroduodenal artery aneurysm: a case report and concise review of literature. Ann. Vasc. Dis. 2015;8(4):331–333. doi: 10.3400/avd.cr.15-00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung H.Y.S., Tang C.N., Fung K.H., Li M.K.W. Bleeding pseudoaneurysms complicating upper abdominal surgery. Hong Kong Med. J. 2007;13(6):449–452. https://www.ncbi.nlm.nih.gov/pubmed/18057433 [PubMed] [Google Scholar]
- 17.Park J.Y., Kim Y.-W., Eom B.W. Unique patterns and proper management of postgastrectomy bleeding in patients with gastric cancer. Surgery. 2014;155(6):1023–1029. doi: 10.1016/j.surg.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Laganà D., Carrafiello G., Mangini M. Multimodal approach to endovascular treatment of visceral artery aneurysms and pseudoaneurysms. Eur. J. Radiol. 2006;59(1):104–111. doi: 10.1016/j.ejrad.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 19.Múnera F., Soto J.A., Palacio D., Velez S.M., Medina E. Diagnosis of arterial injuries caused by penetrating trauma to the neck: comparison of helical CT angiography and conventional angiography. Radiology. 2000;216(2):356–362. doi: 10.1148/radiology.216.2.r00jl25356. [DOI] [PubMed] [Google Scholar]
- 20.Riesenman P.J., Bower T.C., Oderich G.S., Bjarnason H. Multiple hepatic artery aneurysms: use of transcatheter embolization for rupture. Ann. Vasc. Surg. 2006;20(3):399–404. doi: 10.1007/s10016-006-9025-z. [DOI] [PubMed] [Google Scholar]