Abstract
Objective
To analyse the epidemiological characteristics and clinical features of children under the age of 16 years with ocular trauma at the Eye and Ear, Nose and Throat Hospital of Fudan University (Shanghai, China) and to investigate the preventive measurements taken to avoid vision-threatening eye trauma.
Methods
The inpatient medical records of children <16 years old treated for ocular trauma between January 2007 and December 2015 were collected. The age, sex, type of trauma, cause of injury, complications and visual acuity on admission and discharge were analysed statistically.
Results
A total of 2211 patients (2231 eyes) were enroled. Of these, 73.7% were male, and 61.2% were children aged 0–6 years. Mechanical ocular trauma was present in 75.3% of eyes, and penetrating injuries in 59.8%. The top three offending objects were scissors (16.3%), firecrackers (8%) and pencils (4.9%). Iris prolapse (odds ratio [OR] = 2.27), retinal detachment (OR = 2.91), endophthalmitis (OR = 2.25) or an intraocular foreign body (OR = 2.80) was associated with the same or worse visual prognosis among all the subjects. Traumatic cataract (OR = 0.37) was associated with final visual improvement.
Conclusions
An efficient strategy for preventing eye injury should focus on male children during preschool years. Our root cause analysis showed specific environmental patterns of vision-devastating objects. Specific preventive measures are proposed to reduce the incidence of paediatric eye injuries.
Subject terms: Risk factors, Eye diseases
Introduction
Ocular trauma is an important cause of blindness and visual impairment throughout the world, imposing a great socioeconomic burden [1]. Global estimates suggest that ocular trauma causes 3.9 million people to live with bilateral vision loss, and over 18 million to live with unilateral vision loss [2].
Apart from the permanent impairment of visual function [3], paediatric ocular trauma can cause psychological problems [4, 5], which are considered to be a form of post-traumatic stress disorder, arising after an ocular injury [6].
The incidence of severe paediatric ocular trauma varies from 8.85 to 15.21 per 100,000 per year [7, 8]. Even after emergency surgery, many children are left with permanent visual impairment or blindness, varying according to the severity of the trauma. Most paediatric ocular trauma is preventable [9]. Although there have been several studies of paediatric ocular trauma in developed countries, such as New Zealand [10], Canada [11] and the USA [12], reports of large samples in developing countries are limited.
Here, we report a 9-year retrospective study of paediatric eye trauma patients admitted to the Eye and Ear, Nose and Throat (EENT) Hospital (Shanghai, China), a tertiary referral centre servicing multiple provinces in Eastern China. We analysed the demographic, aetiological and clinical characteristics of children with ocular trauma. After studying the factors affecting their prognoses, we proposed targeted prevention strategies for paediatric ocular trauma.
Subjects and methods
Database
We created a database platform for ophthalmic research at the EENT Hospital of Fudan University, based on big databases in other countries and regions. It was constructed with Microsoft SQL Server 2008 (Microsoft, Redmond, WA, USA) using the rules for targeted research projects. By integrating different kinds of data from different medical record systems, we obtained structuralized texts and medical records. The veracity of the data in the database was tested, and data on paediatric eye trauma research projects were extracted. All the projects conformed to the tenets of the Declaration of Helsinki and were approved by the Institutional Review Board of the EENT Hospital of Fudan University.
General information
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of the EENT Hospital of Fudan University.
This study used the big data platform described above to review and analyse data on children aged 0–16 years with eye trauma who were admitted to our hospital between January 2007 and December 2015. Patients with congenital eye diseases were excluded. For patients with multiple hospital admissions, the first hospitalisation data relating to ocular trauma were included. The information accessed from the database included the age, sex, eye involved, mechanism and agent of injury, injury diagnosis, complications, visual acuity at the time of injury and at hospital discharge, classification and distribution of ocular trauma and the time that elapsed between injury and presentation. For the univariate analysis, the patients were divided into two groups: those with visual acuity when leaving hospital that was the same or worse than their visual acuity at presentation, and those with better visual acuity when leaving hospital. For the multivariate analysis, visual acuity that was better than the visual acuity at presentation was used as the reference. The median visual acuity in each group is shown. For the convenience of statistical analysis, visual acuity is expressed as the logarithm of the minimum angle of resolution (logMAR). Low vision category conversion was adapted from a previous publication [13]. The conversion chart is shown in the Supplementary Material (Table S1).
Definitions and classifications
The term ‘ocular trauma’ included compromised structures of the eyeball and the ocular adnexa. Ocular injuries were classified according to the Ocular Trauma Classification Group guidelines and mechanical eye trauma was described based on the Birmingham Eye Trauma Terminology [14, 15]. Mechanical injuries were further dichotomised into open-globe injuries and closed-globe injuries [16]. Penetrating injuries, perforating injuries, intraocular foreign bodies and rupture were categorised as open-globe injuries. Closed-globe injuries were subdivided into lamellar lacerations and contusions. The types of non-mechanical ocular injuries observed in this study included chemical injuries, thermal burns and electrical injuries [17]. Associated ocular damage, such as iris prolapse, vitreous haemorrhage, retinal detachment, lens damage and endophthalmitis, was also evaluated.
Statistical analyses
Statistical analyses were performed with SAS 9.4 (SAS, Cary, NC, USA). Continuous variables are reported as means and standard deviations and categorical variables are described as percentages of each group. Two groups of categorical variables were tested with the χ2 or Fisher’s exact test. Ordinal categorical variables were analysed with the Wilcoxon rank sum test. Differences in continuous variables between groups were compared with the Kruskal–Wallis test. Correlations were determined with Spearman’s correlation analysis. A logistic regression analysis was used to evaluate the relationships between presenting variables and the final visual outcome, and the odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Differences were considered statistically significant at p ≤ 0.05.
Results
Demographic data
A total of 2211 patients (2231 eyes) are enroled. Of these, 1629 (73.7%) were males and 582 (26.3%) were females, with a male-to-female ratio of 2.8:1. Twenty (0.9%) patients have bilateral involvement and 2191 (99.1%) have unilateral injuries (1141 right eyes, 1050 left eyes) (Table 1). The mean age of onset was 6.06 ± 3.93 years. The peak occurrence of ocular trauma was in children aged 4 years (n = 250), followed by those aged 3 years (n = 240) and those aged 2 years (n = 235; Fig. 1a). The patients were further divided into age brackets: 0–3 years old (with a male-to-female ratio of 1.94), 4–6 years old (2.71), 7–12 years old (3.63) and 13–16 years old (6.96) (Fig. 1b).
Table 1.
Demographic features of patients.
| n | % | |
|---|---|---|
| Gender | ||
| Male | 1629 | 73.7 |
| Female | 582 | 26.3 |
| Laterality | ||
| Right | 1141 | 51.6 |
| Left | 1050 | 47.5 |
| Bilateral | 20 | 0.9 |
Fig. 1. The frequency distribution of each age and each age group.
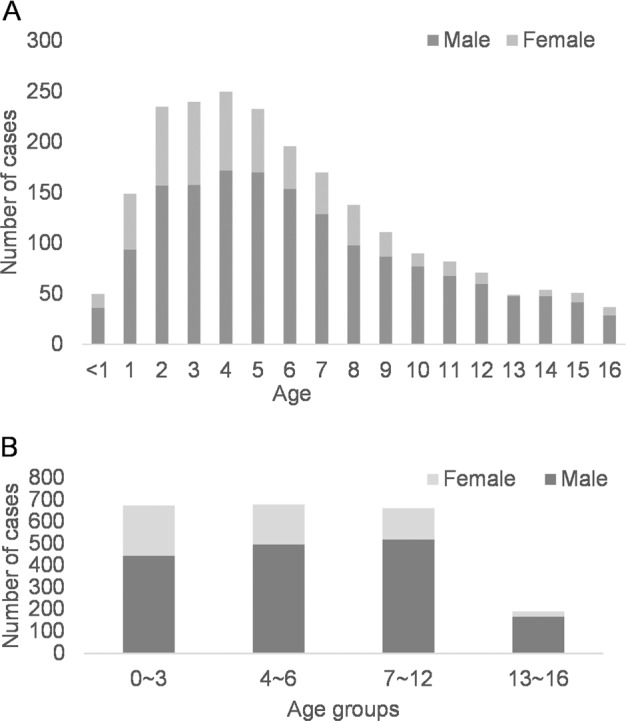
a Frequency distribution of injury in each age group. The peak occurrence of ocular trauma was in children aged 4 years (n = 250) and the least frequent occurrence was in children aged 16 years (n = 37). b Frequency distribution in each age group. Ratio of males to females gradually increased with increasing age: 0–3 years old, 1.94; 4–6 years old, 2.71; 7–12 years old, 3.63; and 13–16 years old, 6.96.
Types of injury
Of all the patients, 90.2% (n = 1995) had mechanical ocular injuries. Among these injuries, 1664 were open-globe injuries and 331 were closed-globe injuries. Non-mechanical causes were responsible for 2.3% of injuries. Ocular adnexa injuries occurred in 4.3% of the patients (Table 2).
Table 2.
Distributions of injury types in hospitalised patients.
| Type of ocular trauma | Number of cases (%) |
|---|---|
| Mechanical ocular injuries | |
| Open-globe injuries | |
| Penetrating | 1321 (59.8%) |
| Rupture | 225 (10.2%) |
| Perforating | 12 (0.5%) |
| Intraocular foreign body | 106 (4.8%) |
| Closed-globe injuries | |
| Contusion | 312 (14.1%) |
| Lamellar laceration | 19 (0.9%) |
| Non-Mechanical ocular injuries | |
| Chemical injury | 28 (1.3%) |
| Thermal injury | 21 (0.9%) |
| electrical injury | 1 (0.0%) |
| Ocular adnexa injuriesa | 94 (4.2%) |
| Othersb and unknown | 72 (3.3%) |
| Total | 2211 (100.00%) |
aOcular adnexal injuries included eyelid injury in 20 patients, lacrimal injury in 16 patients, orbital injury 34 patients and conjunctival injury 24 patients.
bOther injuries included corneal foreign bodies in 63 patients.
The causes of the mechanical injuries are shown in Table S2. The most frequent causes was sharp instruments (52.8%), followed by blunt trauma (26.6%), explosive injury (9.0%), fall (2.5%), traffic accident (2.0%), thermal or chemical injury (1.5%) and animal-related injury (1.0%), whereas 4.7% has unknown or undocumented causes. The three commonest offending objects were scissors (16.3%), firecrackers (8%) and pencils (4.9%; Table S3). Other minor causes of mechanical injury are listed in Table S3. Interestingly, the injuries caused by scissors mainly occurred in July–September (Fig. S1), the time of the summer vacation.
The offending objects involved in the injuries differed across different age groups and between males and females (Table S4). In the 0–3-year-age group, the commonest agents of injury in both the male and female was scissors, followed by glass in males and metal wire in females. Scissors were again the commonest offending object in the 4–6-year-group, whereas firecrackers and pencils were the second commonest cause. Among 7–12-year-old children, the top two objects of injury in boys were firecrackers and scissors, respectively, but this was reversed in girls. Among teenage boys, although sports equipment was the second commonest agent of injury, firecrackers were still the first. In contrast, chemicals and plants were the top two offending agents among teenage girls. Firework injuries accounted for the largest proportion of injuries in February (35.6%), around the Chinese Spring Festival (Fig. S1).
Prognoses and related factors
In the current series, the commonest complication after injury was traumatic cataract, which was found in 52.9% of subjects. This was followed by iris prolapse (21.9%) and endophthalmitis (17.3). Other complications included hyphemia (17.0%), retinal detachment (12.7%) and vitreous haemorrhage (12.4%; Table S5).
Excluding those patients with pneumatic retinopexy, the visual acuity of 830 patients were recorded at presentation and discharge. The distributions of visual acuity at presentation and the final visual acuity are listed in Table S6. These children were classified into two groups: those with vision improvement and those without (same or worse). In a univariate analysis, iris prolapse, traumatic cataract, retinal detachment, choroidal detachment, endophthalmitis and intraocular foreign were identified as statistically significant prognostic factors (Table 3, p ≤ 0.05). A further logistic regression analysis showed that iris prolapse, retinal detachment, endophthalmitis and intraocular foreign body were risk factors for a lack of visual improvement (Table 4). Traumatic cataract was associated with better visual prognosis (OR = 0.37).
Table 3.
Univariate analysis of prognoses and related factors.
| Factors | Unimproved (n = 420) | Improved (n = 410) | P |
|---|---|---|---|
| Gender | 0.858 | ||
| Female | 87 (50.0%) | 87 (50.0%) | |
| Male | 333 (50.8%) | 323 (49.2%) | |
| Age | 0.371 | ||
| 13–16 | 62 (56.9%) | 47 (43.1%) | |
| 7–12 | 217 (49.8%) | 219 (50.2%) | |
| 0–6 | 141 (49.5%) | 144 (50.5%) | |
| Time between injury and the first evaluation | <0.001 | ||
| >48 h | 247 (45.3%) | 298 (54.7%) | |
| ≤48 h | 172 (60.8%) | 111 (39.2%) | |
| Leukoma | 23 (47.9%) | 25 (52.1%) | 0.701 |
| RAPD* | 113 (52.3%) | 103 (47.7%) | 0.558 |
| Iridodialysis | 19 (40.4%) | 28 (59.6%) | 0.151 |
| Iris prolapse | 113 (68.1%) | 53 (31.9%) | <0.001 |
| Hypopyon | 8 (57.1%) | 6 (42.9%) | 0.622 |
| Hyphema | 74 (54.8%) | 61 (45.2%) | 0.285 |
| Trauma cataract | 232 (43.3%) | 304 (56.7%) | <0.001 |
| Glaucoma | 21 (39.6%) | 32 (60.4%) | 0.098 |
| Vitreous haemorrhage | 62 (58.5%) | 44 (41.5%) | 0.082 |
| Retinal detachment | 95 (69.3%) | 42 (30.7%) | <0.001 |
| Choroidal detachment | 34 (70.8%) | 14 (29.2%) | 0.004 |
| Endophthalmia | 101 (64.7%) | 55 (35.3%) | <0.001 |
| Intraocular foreign body | 42 (79.2%) | 11 (20.8%) | <0.001 |
| Open globe | 341 (54.9%) | 280 (45.1%) | <0.001 |
| Hypotony | 6 (66.7%) | 3 (33.3%) | 0.328 |
RAPD* related afferent pupillary defect.
Table 4.
Logistic regression analysis of prognosis and related factors, and the median visual acuity.
| Factors | OR (95% CI) | P | Initial VA | Discharge VA |
|---|---|---|---|---|
| Open globe | 0.94 (0.66, 1.34) | 0.733 | 1.90 ± 0.90 | 1.60 ± 0.48 |
| Iris prolapse | 2.27 (1.51, 3.42) | <0.001 | 1.00 ± 0.48 | 0.95 ± 0.40 |
| Trauma cataract | 0.37 (0.27, 0.50) | <0.001 | 2.30 ± 1.90 | 0.80 ± 0.40 |
| Retinal detachment | 2.91 (1.38, 3.20) | 0.001 | 2.30 ± 1.90 | 2.30 ± 1.90 |
| Endophthalmitis | 2.25 (1.50, 3.37) | <0.001 | 2.30 ± 1.90 | 2.30 ± 1.00 |
| Intraocular foreign body | 2.80 (1.33, 5.88) | 0.007 | 1.40 ± 0.48 | 0.95 ± 0.48 |
For the multivariate analysis, visual acuity on leaving hospital that was better than the visual acuity at first presentation at hospital was used as the reference. Differences were considered statistically significant at p ≤ 0.05. The VA was shown as logarithm of the minimum angle of resolution (logMAR).
Discussion
Ocular trauma is an important public-health concern worldwide, especially in children and adolescents, because it significantly affects both vision and psychological health. In addition to the challenges encountered in its diagnosis and treatment, preoperative examinations in this population are hindered by a lack of cooperation [5]. However, most eye injuries can be prevented with better supervision and education, as proposed by Podbielski [18]. Previous studies have reported the prevalence and types of paediatric eye injuries, but studies evaluating the risk factors for final visual acuity are limited. The EENT Hospital of Fudan University is one of the largest eye hospitals in Eastern China, with a high volume of trauma cases admitted. In this retrospective study, we used the big data platform of the EENT Hospital to study the clinical characteristics and mechanism of eye injuries, the associated ocular pathologies, and the risk factors for visual acuity at the final review after paediatric ocular trauma. To our knowledge, this study involves a larger sample size than previous studies and highlights some significant risk factors for the visual prognosis. Our study offers important new strategies for the prevention, diagnosis and treatment of paediatric ocular trauma.
Our data show that a high proportion of boys were affected by eye trauma. The male-to-female ratio was 2.8 to 1, consistent with other reports (1.9:1 to 5.1:1 [19]). Many studies show that school-aged children are more vulnerable to ocular trauma than younger children, and the average age at onset is 8.4–10.7 years old [20, 21]. The average age at onset in our study was 6.06 ± 3.93 years, with a peak age at 4 years, which is younger than those in other regions. The male-to-female ratio increases with age, probably attributable to the tendency for boys to engage in more risky and vigorous activities than girls. In China, parents and teachers should take more care of infants and preschool-aged children, and understand the safety of school age (especially boys) in order to reduce the number of eye trauma.
Open-globe injury is associated with a worse visual prognosis. Penetrating injuries and perforating injuries are the most and least common types of open-eye trauma in hospitalised children, respectively, accounting for 54.0–83.0% and 2.4–4.0% of injuries, respectively [20–22]. The proportions of penetrating injuries and perforating injuries in our hospital are consistent with those reported in other studies.
In our hospital, mechanical ocular trauma accounted for 93.0% of all paediatric ocular trauma, and 75.3% of these cases were open-globe trauma. Of this trauma, penetration injuries of the eyeball were the most frequent (59.8%), followed by rupture injuries (10.2%), intraocular foreign bodies (4.8%) and perforating injuries (0.5%). The incidence of penetration injuries was lower in our study than in Batur’s study [23], but the incidence of rupture injuries and perforating injuries was higher in our study.
The causative objects of trauma differ among regions. In the present study, scissors were the most frequent objects causing ocular trauma. However, in North India, stones and thorns are the top causes of blunt and penetrating injuries [24]. Adlina et al. reported that organic foreign bodies are the most frequent cause of injury in suburban Malaysia [25]. Our study also demonstrates that the causative agent changes with age. The top offending agent changed from scissors (0–6 years) to fireworks (7–16 years) in males and from scissors (0–12 years) to chemicals (13–16 years) in females. Firework injuries peaked during February, around Chinese New Year, which is consistent with another report of eye trauma in China [26].
Traumatic cataract was the commonest complication in the current study, accounting for 52.9% of all cases. This is higher than in previous studies, in which the incidence of traumatic cataract ranged from 36.7 to 49.2% [27, 28]. In open-globe trauma, uveal prolapse occurs in up to 72% of cases [29], and the posterior extent of the injury is a risk factor for retinal detachment [22]. The incidences of iris prolapse and retinal detachment in our study was lower than in other studies [22, 29]. Patients with closed-eye trauma had a higher rate of improvement in visual acuity after discharge than patients with open-globe trauma.
The incidence of endophthalmitis in children after trauma ranges from 10 to 54.2% [29, 30], which is higher than in adult patients’ (4.2%) [31]. The delayed expression of visual complaints in children may explain this discrepancy. Therefore, close follow-up is required to reduce vision-threatening complications in paediatric patients with eye trauma. The risk factors for endophthalmitis include intraocular foreign bodies, wound contamination with organic matter, open wounds that are not closed within 24 h, and ocular trauma involving the lens capsule [29, 30]. In this study, the objects associated with endophthalmitis were mainly contaminated metal sharps, such as scissors (18.8%), discarded needles (8.4%) and metal wire (6.8%).
We found that children with traumatic cataract showed ultimate visual improvement. This is consistent with Du’s study, which showed that early cataract extraction was associated with a better visual prognosis after trauma [32]. This can be explained by the imminent relief of the media opacity from the visual axis. However, further study is required to examine the long-term visual prognosis in such cases.
The lack of long-term follow-up was a major limitation of our study. Most patients were lost to follow-up because most of them underwent follow-up with ophthalmologists in their home provinces. We hope to obtain their medical records from outside the hospital to assess their long-term visual outcomes.
Our results suggest that scissors are the commonest cause of paediatric ocular trauma. Preventing children’s exposure to scissors should substantially prevent open-eye injuries. To avoid firework-related eye trauma, local authorities must pass stricter regulations controlling the times and places at which fireworks are used during the Spring Festival. The awareness of eye protection among both teachers and parents must also improve. Finally, a fast track for paediatric eye trauma should be available in tertiary eye centres to facilitate its timely evaluation and treatment.
Summary
What was known before
Previous studies were mainly concern demographic and aetiologic in paediatric eye trauma, but less in prognostic factors.
Large sample reports in developing countries are very limited.
What this study adds
The work analysed clinical characteristics and prognostic factors of children with ocular trauma.
The work suggested eye injury prevention work for male children and preschool children should be emphasised.
Supplementary information
Table S1: Low vision category conversion chart
Table S4: The main objects of injury different age groups between males and females
Table S6: The distribution of presenting VA and final VA
Acknowledgments
Funding
This study was supported by the Shanghai Committee of Science and Technology (grant no. 16411953700, China; grant no. 16401932500, China; grant no. 14401932700, China).
Author contributions
YG and YL performed the study and wrote the paper; HX performed the data analysis; ZZ designed the study and revised the paper; DG designed and performed the study.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Yue Guo, Yiwen Liu
Contributor Information
Zhenyang Zhao, Email: Zhezhao@utmb.edu.
Dekang Gan, Email: dekang.gan@fdeent.org.
Supplementary information
The online version of this article (10.1038/s41433-020-1002-1) contains supplementary material, which is available to authorised users.
References
- 1.Schein OD, Hibberd PL, Shingleton BJ, Kunzweiler T, Frambach DA, Seddon JM, et al. The spectrum and burden of ocular injury. Ophthalmology. 1988;95:300–5. doi: 10.1016/S0161-6420(88)33183-0. [DOI] [PubMed] [Google Scholar]
- 2.Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–69. doi: 10.1076/opep.5.3.143.8364. [DOI] [PubMed] [Google Scholar]
- 3.Abbott J, Shah P. The epidemiology and etiology of pediatric ocular trauma. Surv Ophthalmol. 2013;58:476–85. doi: 10.1016/j.survophthal.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Serrano JC, Chalela P, Arias JD. Epidemiology of childhood ocular trauma in a northeastern Colombian region. Arch Ophthalmol. 2003;121:1439–45. doi: 10.1001/archopht.121.10.1439. [DOI] [PubMed] [Google Scholar]
- 5.Al-Mahdi HS, Bener A, Hashim SP. Clinical pattern of pediatric ocular trauma in fast developing country. Int Emerg Nurs. 2011;19:186–91. doi: 10.1016/j.ienj.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 6.Charak R, Ford JD, Modrowski CA, Kerig PK. Polyvictimization, emotion dysregulation, symptoms of posttraumatic stress disorder, and behavioral health problems among justice-involved youth: a latent class analysis. J Abnorm Child Psych. 2019;47:287–98. doi: 10.1007/s10802-018-0431-9. [DOI] [PubMed] [Google Scholar]
- 7.Strahlman E, Elman M, Daub E, Baker S. Causes of pediatric eye injuries. A population-based study. Arch Ophthalmol. 1990;108:603–6. doi: 10.1001/archopht.1990.01070060151066. [DOI] [PubMed] [Google Scholar]
- 8.Desai P, MacEwen CJ, Baines P, Minassian DC. Incidence of cases of ocular trauma admitted to hospital and incidence of blinding outcome. Br J Ophthalmol. 1996;80:592–6. doi: 10.1136/bjo.80.7.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pizzarello LD. Ocular trauma: time for action. Ophthalmic Epidemiol. 1998;5:115–6. doi: 10.1076/opep.5.3.115.8366. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson RA, Sung J, McKelvie J. New Zealand childhood ocular trauma study: analysis of 75,601 cases of ocular injury from 2007 to 2016. Clin Exp Ophthalmol. 2019;47:718–25. doi: 10.1111/ceo.13489. [DOI] [PubMed] [Google Scholar]
- 11.Archambault C, Gabias C, Fallaha N, Belanger C, Superstein R. Pediatric ocular injuries: a 3-year review of patients presenting to an emergency department in Canada. Can J Ophthalmol. 2019;54:83–6. doi: 10.1016/j.jcjo.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Gise R, Truong T, Parsikia A, Mbekeani JN. Visual pathway injuries in pediatric ocular trauma-a survey of the National Trauma Data Bank from 2008 to 2014. Pediatr Neurol. 2018;85:43–50. doi: 10.1016/j.pediatrneurol.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 13.Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the freiburg visual acuity test. Investig Ophthalmol Vis Sci. 2006;47:1236–40. doi: 10.1167/iovs.05-0981. [DOI] [PubMed] [Google Scholar]
- 14.Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin N Am. 2002;15:139–43. doi: 10.1016/S0896-1549(02)00004-4. [DOI] [PubMed] [Google Scholar]
- 15.Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol. 1996;234:399–403. doi: 10.1007/BF00190717. [DOI] [PubMed] [Google Scholar]
- 16.Pieramici DJ, Sternberg PJ, Aaberg TS, Bridges WJ, Capone AJ, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123:820–31. doi: 10.1016/S0002-9394(14)71132-8. [DOI] [PubMed] [Google Scholar]
- 17.Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001;85:1379–83. doi: 10.1136/bjo.85.11.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Podbielski DW, Surkont M, Tehrani NN, Ratnapalan S. Pediatric eye injuries in a Canadian emergency department. Can J Ophthalmol. 2009;44:519–22. doi: 10.3129/i09-093. [DOI] [PubMed] [Google Scholar]
- 19.Li X, Zarbin MA, Bhagat N. Pediatric open globe injury: a review of the literature. J Emerg Trauma Shock. 2015;8:216–23. doi: 10.4103/0974-2700.166663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tok O, Tok L, Ozkaya D, Eraslan E, Ornek F, Bardak Y. Epidemiological characteristics and visual outcome after open globe injuries in children. J AAPOS. 2011;15:556–61. doi: 10.1016/j.jaapos.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 21.Puodziuviene E, Jokubauskiene G, Vieversyte M, Asselineau K. A five-year retrospective study of the epidemiological characteristics and visual outcomes of pediatric ocular trauma. BMC Ophthalmol. 2018;18:10. doi: 10.1186/s12886-018-0676-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lesniak SP, Bauza A, Son JH, Zarbin MA, Langer P, Guo S, et al. Twelve-year review of pediatric traumatic open globe injuries in an urban U.S. population. J Pediatr Ophthalmol Strabismus. 2012;49:73–9. doi: 10.3928/01913913-20110712-02. [DOI] [PubMed] [Google Scholar]
- 23.Batur M, Seven E, Akaltun MN, Tekin S, Yasar T. Epidemiology of open globe injury in children. J Craniofac Surg. 2017;28:1976–81. doi: 10.1097/SCS.0000000000004033. [DOI] [PubMed] [Google Scholar]
- 24.Sharma AK, Aslami AN, Srivastava JP, Iqbal J. Visual outcome of traumatic cataract at a tertiary eye care centre in North India: a prospective study. J Clin Diagn Res. 2016;10:C5–8. doi: 10.7860/JCDR/2016/17216.7049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adlina AR, Chong YJ, Shatriah I. Clinical profile and visual outcome of traumatic paediatric cataract in suburban Malaysia: a ten-year experience. Singap Med J. 2014;55:253–6. doi: 10.11622/smedj.2014067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in South-Central China. Acta Ophthalmol. 2017;95:e503–10. doi: 10.1111/aos.13438. [DOI] [PubMed] [Google Scholar]
- 27.Ilhan HD, Bilgin AB, Cetinkaya A, Unal M, Yucel I. Epidemiological and clinical features of paediatric open globe injuries in southwestern Turkey. Int J Ophthalmol. 2013;6:855–60. doi: 10.3980/j.issn.2222-3959.2013.06.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chakraborti C, Giri D, Choudhury KP, Mondal M, Datta J. Paediatric ocular trauma in a tertiary eye care center in Eastern India. Indian J Public Health. 2014;58:278–80. doi: 10.4103/0019-557X.146297. [DOI] [PubMed] [Google Scholar]
- 29.Hosseini H, Masoumpour M, Keshavarz-Fazl F, Razeghinejad MR, Salouti R, Nowroozzadeh MH. Clinical and epidemiologic characteristics of severe childhood ocular injuries in southern iran. Middle East Afr J Ophthalmol. 2011;18:136–40. doi: 10.4103/0974-9233.80702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Narang S, Gupta V, Simalandhi P, Gupta A, Raj S, Dogra MR. Paediatric open globe injuries. Visual outcome and risk factors for endophthalmitis. Indian J Ophthalmol. 2004;52:29–34. [PubMed] [Google Scholar]
- 31.Duch-Samper AM, Menezo JL, Hurtado-Sarrio M. Endophthalmitis following penetrating eye injuries. Acta Ophthalmol Scand. 1997;75:104–6. doi: 10.1111/j.1600-0420.1997.tb00263.x. [DOI] [PubMed] [Google Scholar]
- 32.Du Y, He W, Sun X, Lu Y, Zhu X. Traumatic cataract in children in Eastern China: Shanghai Pediatric Cataract Study. Sci Rep. 2018;8:2588. doi: 10.1038/s41598-018-20982-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Low vision category conversion chart
Table S4: The main objects of injury different age groups between males and females
Table S6: The distribution of presenting VA and final VA


