Abstract
Background
Clopidogrel, prasugrel and ticagrelor, acting on platelet P2Y12 receptor, are commonly used for prevention of stent thrombosis (ST) among patients who underwent percutaneous coronary intervention (PCI). This study aimed to compare the effects of these drugs by a systematic review and network meta‐analysis.
Hypothesis
Efficacies of clopidogrel, prasugrel and ticagrelor on preventing ST are not the same.
Methods
PubMed, Embase and Cochrane Library were searched for randomized controlled trials (RCTs) that investigated the effect of clopidogrel, prasugrel, or ticagrelor on prevention of ST in patients who underwent PCI. The efficacies between groups were compared by a Bayesian network meta‐analysis, by which the pooled odds ratios (ORs) and 95% confidence intervals (CIs) was calculated.
Results
Fourteen studies and 46 983 participants were included in this study. The pooled results illustrated that clopidogrel, prasugrel and ticagrelor were effective on prevention of ST. Patients treated with prasugrel (OR = 0.30, 95% CI = 0.052 ~ 0.73, P < 0.05) and ticagrelor (OR = 0.25, 95% CI = 0.035 ~ 0.65, P < 0.05) had lower incidence of ST compared to those treated with clopidogrel. Patients treated with ticagrelor showed similar frequency with those in prasugrel group (OR = 0.86, 95% CI = 0.22 ~ 2.3, P > 0.05). No significant heterogeneity was observed across included studies.
Conclusions
Our findings suggest that prasugrel and ticagrelor are more effective than clopidogrel on prevention of ST among patients underwent PCI. Simultaneously, there is no significant difference in the prevention of ST between prasugrel and ticagrelor.
Keywords: clopidogrel, network meta‐analysis, percutaneous coronary intervention, prasugrel, stent thrombosis, ticagrelor
1. INTRODUCTION
The approach of percutaneous coronary intervention (PCI) with intracoronary stents has been widely used to prevent the occurrence of myocardial infarction (MI) in patients with acute coronary syndrome (ACS). 1 , 2 However, it is noteworthy that stent thrombosis (ST) is one of the severe complications following PCI, potentially leading to death. 3 Results from the ADAPT‐DES study indicates that early ST (within 30 days) attributes to about 40% of mortalities among individuals who undergo PCI. During 2 years follow‐up, all‐cause mortality in these patients is significantly higher than those without MI, ST or clinically relevant bleeding (27.2% vs. 2.7%). 4 Therefore, it is increasingly concerned to reduce the incidence of ST after PCI treatment.
As is known, the occurrence of ST is associated with patient‐, lesion‐, procedure‐, and post‐procedure‐related risk factors. 5 Platelets play an important role in the pathophysiology of ST. Implantation of stent struts initiates platelet activation and adhesion, followed by thrombus formation, which results in early ST. 5 Therefore, inhibition of platelet function is considered effective for preventing the occurrence of ST. Currently, one of the clinical approaches for inhibition of platelet aggregation is dual antiplatelet therapy (DAPT), which is based on the combination of aspirin with one of P2Y12 inhibitors (i.e., clopidogrel, prasugrel and ticagrelor). 6 Studies have focused on the differences in the efficacies of P2Y12 inhibitors. Pharmacodynamic studies have suggested that the effect of clopidogrel is weaker than prasugrel or ticagrelor. 7 Clinical trials and real‐world studies discovered that patients using clopidogrel suffered from higher incidence of ST compared to those treated with prasugrel or ticagrelor. 8 , 9 , 10 , 11 However, up to date, the difference in the incidences of ST between prasugrel and ticagrelor has not been clearly elucidated. Two studies reported that prasugrel was more effective than ticagrelor for preventing ST 12 , 13 ; however, other studies released insignificant results. 14 , 15 , 16 Here, we conducted a systematic review and network meta‐analysis to compare the efficacies of three P2Y12 inhibitors (i.e., clopidogrel, prasugrel and ticagrelor).
2. METHODS
2.1. Search strategy
PubMed, Embase and Cochrane Library were searched for randomized controlled trials (RCTs) that compared the effect of clopidogrel, prasugrel, and/or ticagrelor in patients who underwent PCI. The search terms were “ticagrelor or brilinta”, “clopidogrel or plavix”, “prasugrel or effient”, and “ST”. These databases were searched for studies published up to January 12, 2020. RCTs registered in www.clinicaltrials.gov and major international cardiology meetings (American College of Cardiology (ACC), American Heart Association (AHA), and European Society of Cardiology (ESC)) were also identified. Inclusion criteria were: (a) RCTs, (b) comparison of clopidogrel, prasugrel or ticagrelor, (c) patients underwent PCI, (d) patients with follow‐up at least 6 months.
The primary end‐point was the rate of ST individually (as per the Academic Research Consortium definition).
2.2. Data extraction and quality assessment
The following data were collected from eligible studies: first author name, year of publication, region, type of study, duration of follow‐up, number of participants, gender of the subjects, and treatment regimens. The data were independently collected by two authors. The discrepancies were resolved by discussion with a third author.
Quality of included studies was assessed in accordance with the Cochrane Risk of Bias Tool, which contains seven domains: (a) random sequence generation, (b) allocation concealment, (c) blinding of participants and personnel, (d) blinding of outcome assessment, (e) incomplete outcome data, (f) selective reporting, and (g) other bias. Two authors completed quality assessment separately, and any discrepancies would be resolved by a third author.
2.3. Statistical analysis
We performed statistical analyses with Stata Version 14.0 (Stata Corp, College Station, TX, USA) and R Version 3.4.2 (R Development Core Team, Vienna, Austria). We carried out a Bayesian network meta‐analysis using the “gemtc” package for R. We calculated odds ratios (ORs) and 95% confidence intervals (CIs) for comparisons between groups. We analyzed the convergence of Markov chain Monte Carlo chains for all model parameters using trace plots and Gelman‐Rubin diagnostic statistics. With regard to heterogeneity test, a P < 0.10 indicated statistically significant. The potential publication bias was estimated by funnel plot asymmetry.
3. RESULTS
3.1. Characteristics of included studies
Our literature search returned 1730 studies. After elimination of duplicate results, 910 studies were reviewed. After exclusion of 874 studies by title and/or abstract, 36 articles were reviewed in full‐text. Finally, 14 studies 8 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 that met all criteria were included in our meta‐analysis (Figure 1), with 46 983 participants. The duration of follow‐up was 11.1 ± 2.9 months, ranging from 6 to 15 months. As shown in Table 1, the majority of included studies were based in Asia, and the minority was from the America, Australia, Europe and other regions. Most studies included more males than females. Eight of 14 studies were multicenter studies. Six studies compared the difference of ST incidences between clopidogrel and ticagrelor, while four studies compared the difference between clopidogrel and prasugrel, and three studies compared ticagrelor with prasugrel. Only one study compared the difference between three agents.
FIGURE 1.
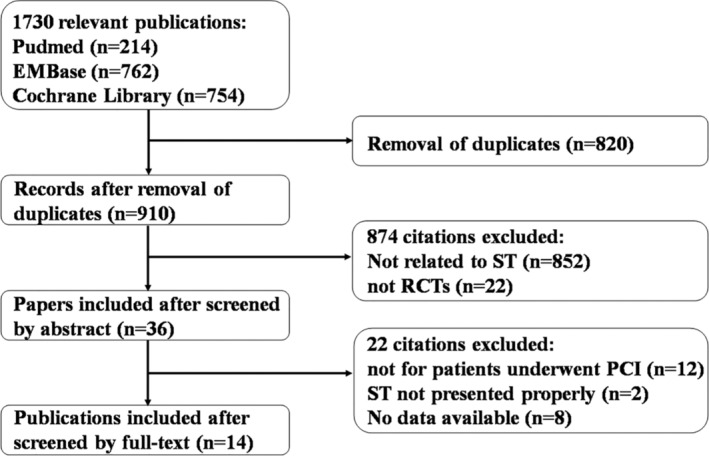
Flowchart of search strategy and article selection
TABLE 1.
Study characteristics of included trials
| First author | Year | Region | Type of study | Follow‐up | Participants | Female sex (%) | Treatment regimens |
|---|---|---|---|---|---|---|---|
| Wallentin 17 | 2009 | Asia and Australia, Europe, Middle East, America | multicenter | 12 months | 11 289 | 23.8 | ticagrelor vs. clopidogrel |
| Tang 18 | 2016 | Asia | two‐center | 6 months | 400 | 28.0 | ticagrelor vs. clopidogrel |
| Li 19 | 2018 | Asia | single‐center | 12 months | 442 | 21.7 | ticagrelor vs. clopidogrel |
| Cai 20 | 2015 | Asia | single‐center | 12 months | 120 | NA | ticagrelor vs. clopidogrel |
| Zeng 21 | 2017 | Asia | single‐center | 12 months | 204 | ticagrelor vs. clopidogrel | |
| Zhang 22 | 2017 | Asia | single‐center | 6 months | 181 | 49.0 | ticagrelor vs. clopidogrel |
| Motovska 16 | 2017 | Czech Republic | multicenter | 12 months | 1230 | NA | prasugre vs. ticagrelor |
| Patel 23 | 2018 | Asia | single‐center | 12 months | 1150 | NA | prasugre vs. ticagrelor |
| Schüpke 14 | 2019 | Europe | multicenter | 12 months | 4018 | 23.8 | prasugre vs. ticagrelor |
| Trenk 24 | 2012 | Europe and America | multicenter | 6 months | 423 | 27.4 | prasugre vs. clopidogrel |
| Wiviott 8 | 2007 | Asia and Africa, Europe, Middle East, America | multicenter | 15 months | 13 608 | 26.0 | prasugre vs. clopidogrel |
| Brener 25 | 2014 | Europe and America | multicenter | 12 months | 452 | 26.1 | prasugre vs. clopidogrel |
| Montalescot 26 | 2009 | NA | multicenter | 15 months | 3534 | 22.6 | prasugre vs. clopidogrel |
| Welsh 15 | 2019 | NA | multicenter | 12 months | 9932 | 23.8 |
prasugre vs. ticagrelor & ticagrelor vs. clopidogrel |
3.2. Study quality
The Cochrane Risk of Bias tool was applied for assessment of methodological quality. 27 The quality evaluation of included studies was shown in Figures 2 and 3. Of the 14 studies included in this meta‐analysis, only four studies applied blinding method, while six studies had potential risk of bias due to lack of blinding for participants. In addition, the lack of clear statement of allocation concealment (in nine studies) and blinding of outcome assessment (in 10 studies) might result in potential risk of selection bias and detection bias, respectively.
FIGURE 2.
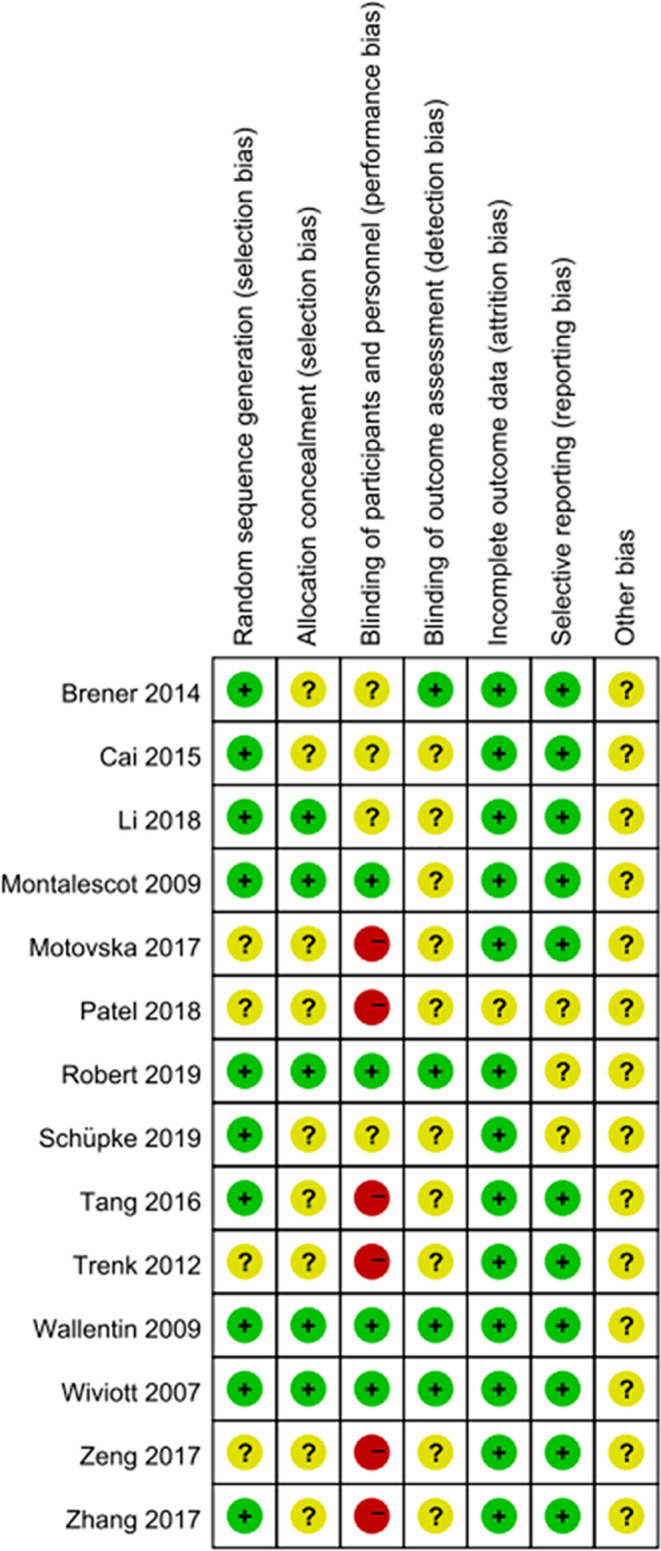
Risk of bias summary: the risk of bias of each domain in each study
FIGURE 3.
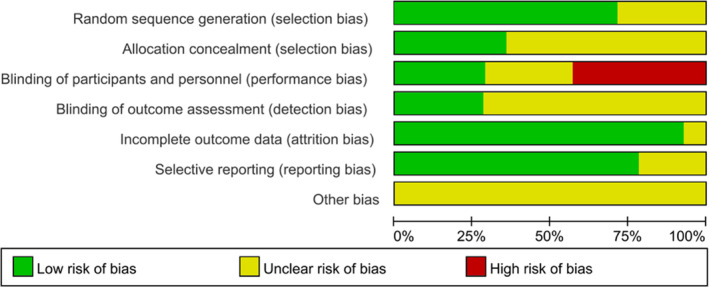
Risk of bias graph: an overall risk of bias of each domain. For example, the length of green rectangle means the number of studies being assessed as low risk of bias
3.3. Results of network meta‐analysis
As shown in Figure 4, a significant decrease in the frequency of ST was observed for prasugrel treatment compared with clopidogrel treatment (OR = 0.30, 95% CI = 0.052–0.73). Meanwhile, the frequency of ST was also significantly decreased for ticagrelor treatment compared with clopidogrel treatment (OR = 0.25, 95% CI = 0.035–0.65). No significant difference was observed between ticagrelor and prasugrel (OR = 0.86, 95% CI = 0.22–2.3).
FIGURE 4.
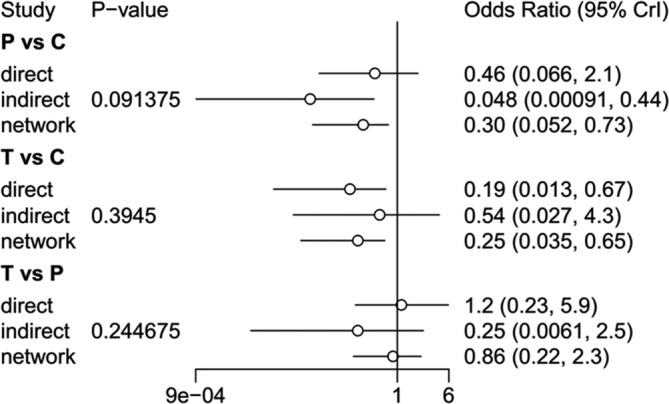
Network meta‐analysis results of ST among three DAPT regimen. C, clopidogrel; P, prasugrel; T, ticagrelor
3.4. Model convergence of our network meta‐analysis
The model convergence was checked using Brooks‐Gelman‐Rubin diagnostic statistics (Figure S1) and trace plots (Figure S2) for all model parameters. The Brooks‐Gelman‐Rubin statistics got close to one fast, which revealed that the three Markov chain Monte Carlo chains mixed well regardless of their different initial starting points. Meanwhile, the trace plots illustrated that every Markov chain Monte Carlo chains converged well.
3.5. Heterogeneity test and publication bias analysis
No significant heterogeneity was observed across included studies (P = 0.980) (Figure S3). The identification of potential publication bias was estimated by funnel plot asymmetry (Figure 5). Moreover, Begg's test (P = 0.4) and Egger's test (t = −1.26, P = 0.229) showed that no publication bias was involved in this study.
FIGURE 5.
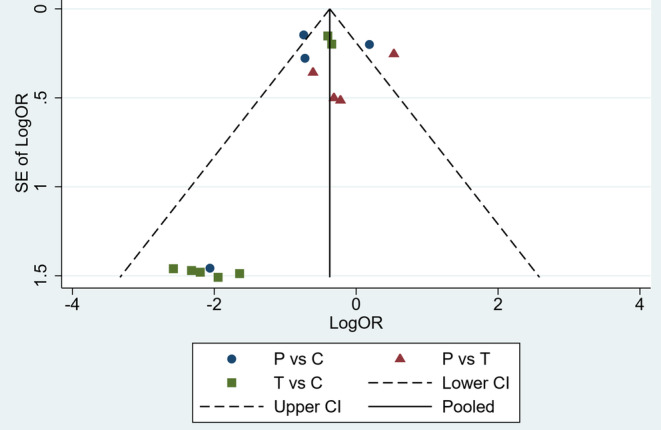
Funnel plot analysis on publication bias. P, prasugrel; T, ticagrelor; C, clopidogrel; OR, odds ratio; S.E. standard error; 95% CI, 95% confidence interval
4. DISCUSSION
Our network meta‐analysis indicated that prasugrel and ticagrelor had similar efficacy for preventing ST and both of them were more potent than clopidogrel. However, none of the three drugs could completely prevent ST.
As the most common complication, ST is a major clinical concern of post‐PCI treatment. Studies showed that the occurrence of ST was significantly related to inadequate antiplatelet therapy. 28 , 29 According to clinical guidelines, DAPT, with a combination of aspirin and one P2Y12 inhibitor (i.e., clopidogrel, prasugrel or ticagrelor), has been recommended to be used for antiplatelet therapy. 6 , 30 TRITON–TIMI 38 study revealed that prasugrel caused less ST than clopidogrel (68/6745 vs. 142/6653). 8 Similarly, PLATO investigators reported that ticagrelor was more efficient on the prevention of ST events than clopidogrel (71/5569 vs. 106/5543). 17 Our network meta‐analysis also obtained similar result. This might due to the different pharmacokinetics of these drugs. Prasugrel and ticagrelor generate active metabolite more rapidly than clopidogrel. 31 , 32 , 33 The conversion of clopidogrel is linked to ABCB1 which act as a transporting molecule mediating the uptake of drug by intestinal cells, CYP2C19 and paraoxonase 1 (PON1) which affect the biotransformation of clopidogrel. 34 , 35 , 36 This leads to a delayed anti‐platelet action of clopidogrel. 29 By contrast, prasugrel requires only a single CYP‐dependent oxidative step during its metabolic transformation, 37 while the action of ticagrelor needs no transformation. 32 , 33
Although ticagrelor has pharmacokinetic advantages over prasugrel, two indirect comparison meta‐analyses showed prasugrel might be more effective than ticagrelor for preventing ST. 12 , 13 However, subsequent head to head comparison studies, including the PRAGUE‐18 study (9/587 vs. 7/627), ISAR‐REACT 5 trial (22/1990 vs. 12/1994) and TOTAL trial (31/2188 vs. 30/1244), showed that patients treated with ticagrelor had a similar rate of ST compared to those treated with prasugrel. 14 , 15 , 16 Consistently, our network meta‐analysis confirmed the similar efficacy for the prevention of ST between prasugrel and ticagrelor (OR = 0.86, 95% CI = 0.22–2.3).
More interestingly, several recent real‐world studies actually found that ticagrelor was not superior to clopidogrel for preventing ST, 38 , 39 , 40 which was different from PLATO trial as well as our study. This might be explained by the following reasons. A potent mediator for efficacy attenuation of ticagrelor outside RCT might be decreased compliance because of the higher rate of adverse events (dyspnea, bleeding), administration of the drug twice daily and higher costs. 38 , 39 , 40 Additionally, the overall improvement in the clinical outcomes of patients with ACS 41 might be another possible explanation for the diminished benefit of ticagrelor in the modern era; particularly, this might be driven by progress in the use of drug‐eluting stents 42 and poststenting care.
Finally, it should be noted that some patients still experience ST events in spite of DAPT. This might partly result from the inadequate anti‐platelet activity of DAPT. Besides, procedural “trauma” to the vessel and inadequate stent deployment play a role in the development of ST. 5 Therefore, further research is needed to identify the mechanism of ST among individuals underwent PCI.
5. LIMITATIONS
Several limitations should be noticed in the present study. First, this study was a meta‐analysis of different trials, which were isolated designs. Although we included 46 983 patients in 14 studies, 34 829 (74.13%) were from three studies. These three studies weighted more in our pooled results than other 11 studies with small sample size. Therefore, it was apparent that the results in the three studies were more important due to not only large sample size but also high statistical power. Second, all the studies included in our network meta‐analysis are RCTs, and the conclusions may be discordant with real‐world studies because the RCT world does not correspond with the clinical practice. Therefore, this situation obviously limits the representability of our findings in current meta‐analysis. Third, different kinds of stents were used in the trials included in our study. Compared to bare‐metal stent, drug‐eluting stent was associated with a faster reendothelization and lower thrombotic risk. This might introduce bias in our results. Finally, due to lack of data, the effects of other high‐risk factors (i.e., type of myocardial infarction, complex coronary anatomy, and surgical factors) on ST were not evaluated in this study.
6. CONCLUSION
In conclusion, our findings suggest that prasugrel and ticagrelor are more effective than clopidogrel on prevention of ST among patients underwent PCI. Additionally, there is no significant difference in the prevention of ST between prasugrel and ticagrelor.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
Conceived and designed the meta‐analysis: Yuanmin Li and Haifeng Hou. Performed the study: Chen Zhang and Jian Zhao. Analyzed the data: Xiuxiu Xu and Qiang Xiao. Wrote the paper: Wenwen Chen.
Supporting information
FIGURE S1 Brooks‐Gelman‐Rubin diagnostic statistics. T, ticagrelor; C, clopidogrel; P, prasugrel; SE, standard error
Figure S2 Trace plots of our models. T, ticagrelor; C, clopidogrel; P, prasugrel; SE, standard error
Figure S3 Heterogeneity test. T, ticagrelor; C, clopidogrel; P, prasugrel; OR, odds ratio; 95% CI, 95% confidence interval
Chen W, Zhang C, Zhao J, et al. Effects of clopidogrel, prasugrel and ticagrelor on prevention of stent thrombosis in patients underwent percutaneous coronary intervention: A network meta‐analysis. Clin Cardiol. 2021;44:488–494. 10.1002/clc.23536
Funding information Academic Promotion Programme of Shandong First Medical University, Grant/Award Number: 2019QL017; Shandong Provincial Natural Science Foundation, China, Grant/Award Number: ZR2017MH097 ZR2017MH100
Contributor Information
Qiang Xiao, Email: tyfy8011@126.com.
Yuanmin Li, Email: liym575@126.com.
Haifeng Hou, Email: hfhou@163.com.
DATA AVAILABILITY STATEMENT
The data supporting this network meta‐analysis are from previously reported studies and datasets, which have been cited.
REFERENCES
- 1. Mukherjee D, Moliterno DJ. Effectiveness of PCI for non‐acute coronary artery disease. Lancet (London, England). 2009;373(9667):870‐872. [DOI] [PubMed] [Google Scholar]
- 2. Mehta SR, Cannon CP, Fox KA, et al. Routine vs selective invasive strategies in patients with acute coronary syndromes: a collaborative meta‐analysis of randomized trials. JAMA. 2005;293(23):2908‐2917. [DOI] [PubMed] [Google Scholar]
- 3. Mauri L, Hsieh WH, Massaro JM, Ho KK, D'Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug‐eluting stents. N Engl J Med. 2007;356(10):1020‐1029. [DOI] [PubMed] [Google Scholar]
- 4. Brener SJ, Kirtane AJ, Stuckey TD, et al. The impact of timing of ischemic and hemorrhagic events on mortality after percutaneous coronary intervention: the ADAPT‐DES study. JACC Cardiovascular Interventions. 2016;9(14):1450‐1457. [DOI] [PubMed] [Google Scholar]
- 5. Byrne RA, Joner M, Kastrati A. Stent thrombosis and restenosis: what have we learned and where are we going? The Andreas Gruntzig lecture ESC 2014. Eur Heart J. 2015;36(47):3320‐3331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: the task force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio‐Thoracic Surgery (EACTS). European Heart J. 2018;39(3):213‐260. [DOI] [PubMed] [Google Scholar]
- 7. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation. Kardiologia Polska. 2018;76(2):229‐313. [DOI] [PubMed] [Google Scholar]
- 8. Wiviott SD, Eugene B, Mccabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. New England J Med. 2007;357(20):2001‐2015. [DOI] [PubMed] [Google Scholar]
- 9. Lars W, Becker RC, Andrzej B, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. New England J Med. 2009;361(11):1045‐1057. [DOI] [PubMed] [Google Scholar]
- 10. Gosling R, Yazdani M, Parviz Y, et al. Comparison of P2Y(12) inhibitors for mortality and stent thrombosis in patients with acute coronary syndromes: single center study of 10 793 consecutive 'real‐world' patients. Platelets. 2017;28(8):767‐773. [DOI] [PubMed] [Google Scholar]
- 11. Krishnamurthy A, Keeble C, Anderson M, et al. Real‐world comparison of clopidogrel, prasugrel and ticagrelor in patients undergoing primary percutaneous coronary intervention. Open Heart. 2019;6(1):e000951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Biondi‐Zoccai G, Lotrionte M, Agostoni P, et al. Adjusted indirect comparison meta‐analysis of prasugrel versus ticagrelor for patients with acute coronary syndromes. Int J Cardiol. 2011;150(3):325‐331. [DOI] [PubMed] [Google Scholar]
- 13. Chatterjee S, Ghose A, Sharma A, Guha G, Mukherjee D, Frankel R. Comparing newer oral anti‐platelets prasugrel and ticagrelor in reduction of ischemic events‐evidence from a network meta‐analysis. J Thromb Thrombolysis. 2013;36(3):223‐232. [DOI] [PubMed] [Google Scholar]
- 14. Schupke S, Neumann FJ, Menichelli M, et al. Ticagrelor or Prasugrel in patients with acute coronary syndromes. N Engl J Med. 2019;381(16):1524‐1534. [DOI] [PubMed] [Google Scholar]
- 15. Welsh RC, Sidhu RS, Cairns JA, et al. Outcomes among Clopidogrel, Prasugrel, and Ticagrelor in ST‐elevation myocardial infarction patients who underwent primary percutaneous coronary intervention from the TOTAL trial. Can J Cardiol. 2019;35(10):1377‐1385. [DOI] [PubMed] [Google Scholar]
- 16. Motovska Z, Hlinomaz O, Kala P, et al. One‐year outcomes of Prasugrel versus Ticagrelor in acute myocardial infarction treated with primary angioplasty: the PRAGUE‐18 study. J American College Cardiol. 2017;71(4):S0735109717415245. [Google Scholar]
- 17. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045‐1057. [DOI] [PubMed] [Google Scholar]
- 18. Tang X, Li R, Jing Q, et al. Assessment of Ticagrelor versus Clopidogrel treatment in patients with ST‐elevation myocardial infarction undergoing primary percutaneous coronary intervention. J Cardiovasc Pharmacol. 2016;68(2):115‐120. [DOI] [PubMed] [Google Scholar]
- 19. Li XY, Su GH, Wang GX, Hu HY, Fan CJ. Switching from ticagrelor to clopidogrel in patients with ST‐segment elevation myocardial infarction undergoing successful percutaneous coronary intervention in real‐world China: occurrences, reasons, and long‐term clinical outcomes. Clin Cardiol. 2018;41(11):1446‐1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cai L, Zhang F, Rong YD, et al. Effect and safety of ticagrelor on platelet in elderly patients undergoing PCI. J Am Geriatr Soc. 2018;66:S473. [Google Scholar]
- 21. Zeng DL, Duan XY, Fan WW, et al. Clinical therapeutic effect of ticagrelor for complicated coronary artery disease patients undergoing PCI. J Am Geriatr Soc. 2018;66:S474. [Google Scholar]
- 22. Zhang Y, Zhao Y, Pang M, et al. High‐dose clopidogrel versus ticagrelor for treatment of acute coronary syndromes after percutaneous coronary intervention in CYP2C19 intermediate or poor metabolizers: a prospective, randomized, open‐label, single‐Centre trial. Acta Cardiol. 2016;71(3):309‐316. [DOI] [PubMed] [Google Scholar]
- 23. Patel RA, Banker DN. Clinical outcomes of patients undergoing primary angioplasty for acute myocardial infarction treated with prasugrel versus ticagrelor at the end of 1 month & 1 year. Indian Heart J. 2018;70:S29. [Google Scholar]
- 24. Trenk D, Stone GW, Gawaz M, et al. A randomized trial of prasugrel versus clopidogrel in patients with high platelet reactivity on clopidogrel after elective percutaneous coronary intervention with implantation of drug‐eluting stents: results of the TRIGGER‐PCI (testing platelet reactivity in patients undergoing elective stent placement on Clopidogrel to guide alternative therapy with Prasugrel) study. J Am Coll Cardiol. 2012;59(24):2159‐2164. [DOI] [PubMed] [Google Scholar]
- 25. Brener SJ, Oldroyd KG, Maehara A, et al. Outcomes in patients with ST‐segment elevation acute myocardial infarction treated with clopidogrel versus prasugrel (from the INFUSE‐AMI trial). Am J Cardiol. 2014;113(9):1457‐1460. [DOI] [PubMed] [Google Scholar]
- 26. Montalescot G, Wiviott SD, Braunwald E, et al. Prasugrel compared with clopidogrel in patients undergoing percutaneous coronary intervention for ST‐elevation myocardial infarction (TRITON‐TIMI 38): double‐blind, randomised controlled trial. Lancet (London, England). 2009;373(9665):723‐731. [DOI] [PubMed] [Google Scholar]
- 27. Shi X, Yu W, Wang T, et al. A comparison of the effects of electroacupuncture vs transcutaneous electrical nerve stimulation for pain control in knee osteoarthritis: a protocol for network meta‐analysis of randomized controlled trials. Medicine. 2019;98(28):e16265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gurbel PA, Bliden KP, Samara W, et al. Clopidogrel effect on platelet reactivity in patients with stent thrombosis: results of the CREST study. J Am Coll Cardiol. 2005;46(10):1827‐1832. [DOI] [PubMed] [Google Scholar]
- 29. Steg PG, Harrington RA, Emanuelsson H, et al. Stent thrombosis with ticagrelor versus clopidogrel in patients with acute coronary syndromes: an analysis from the prospective, randomized PLATO trial. Circulation. 2013;128(10):1055‐1065. [DOI] [PubMed] [Google Scholar]
- 30. Correction to: 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST‐Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non‐ST‐Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guidelineon Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation. 2016;134(10):e192‐e194. [DOI] [PubMed] [Google Scholar]
- 31. Niitsu Y, Jakubowski JA, Sugidachi A, Asai F. Pharmacology of CS‐747 (prasugrel, LY640315), a novel, potent antiplatelet agent with in vivo P2Y12 receptor antagonist activity. Semin Thromb Hemost. 2005;31(2):184‐194. [DOI] [PubMed] [Google Scholar]
- 32. Storey RF, Husted S, Harrington RA, et al. Inhibition of platelet aggregation by AZD6140, a reversible oral P2Y12 receptor antagonist, compared with clopidogrel in patients with acute coronary syndromes. J Am Coll Cardiol. 2007;50(19):1852‐1856. [DOI] [PubMed] [Google Scholar]
- 33. Husted S, Emanuelsson H, Heptinstall S, Sandset PM, Wickens M, Peters G. Pharmacodynamics, pharmacokinetics, and safety of the oral reversible P2Y12 antagonist AZD6140 with aspirin in patients with atherosclerosis: a double‐blind comparison to clopidogrel with aspirin. Eur Heart J. 2006;27(9):1038‐1047. [DOI] [PubMed] [Google Scholar]
- 34. Bouman HJ, Schomig E, van Werkum JW, et al. Paraoxonase‐1 is a major determinant of clopidogrel efficacy. Nat Med. 2011;17(1):110‐116. [DOI] [PubMed] [Google Scholar]
- 35. Mega JL, Close SL, Wiviott SD, et al. Cytochrome p‐450 polymorphisms and response to clopidogrel. N Engl J Med. 2009;360(4):354‐362. [DOI] [PubMed] [Google Scholar]
- 36. Viviani Anselmi C, Briguori C, Roncarati R, et al. Routine assessment of on‐clopidogrel platelet reactivity and gene polymorphisms in predicting clinical outcome following drug‐eluting stent implantation in patients with stable coronary artery disease. JACC Cardiovasc Interv. 2013;6(11):1166‐1175. [DOI] [PubMed] [Google Scholar]
- 37. Ohno Y, Okada S, Kitahara H, et al. Repetitive stent thrombosis in a patient who had resistance to both clopidogrel and prasugrel. J Cardiol Cases. 2016;13(5):139‐142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Völz S, Petursson P, Odenstedt J, et al. Ticagrelor is not superior to Clopidogrel in patients with acute coronary syndromes undergoing PCI: a report from Swedish coronary angiography and angioplasty registry. J Am Heart Assoc. 2020;9(14):e015990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Turgeon RD, Koshman SL, Youngson E, et al. Association of Ticagrelor vs Clopidogrel with major adverse coronary events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. JAMA Intern Med. 2020;180(3):420‐428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. You SC, Rho Y, Bikdeli B, et al. Association of Ticagrelor vs Clopidogrel with net adverse clinical events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. JAMA. 2020;324(16):1640‐1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Simonsson M, Wallentin L, Alfredsson J, et al. Temporal trends in bleeding events in acute myocardial infarction: insights from the SWEDEHEART registry. Eur Heart J. 2020;41(7):833‐843. [DOI] [PubMed] [Google Scholar]
- 42. Piccolo R, Bonaa KH, Efthimiou O, et al. Drug‐eluting or bare‐metal stents for percutaneous coronary intervention: a systematic review and individual patient data meta‐analysis of randomised clinical trials. Lancet. 2019;393(10190):2503‐2510. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE S1 Brooks‐Gelman‐Rubin diagnostic statistics. T, ticagrelor; C, clopidogrel; P, prasugrel; SE, standard error
Figure S2 Trace plots of our models. T, ticagrelor; C, clopidogrel; P, prasugrel; SE, standard error
Figure S3 Heterogeneity test. T, ticagrelor; C, clopidogrel; P, prasugrel; OR, odds ratio; 95% CI, 95% confidence interval
Data Availability Statement
The data supporting this network meta‐analysis are from previously reported studies and datasets, which have been cited.


