Abstract
Detection of idiopathic interstitial pneumonias (IIPs) on chest X-ray is difficult for non-specialist physicians, especially in patients with mild IIPs. The current study aimed to evaluate the usefulness of a simple method for detecting IIPs by measuring vertical lung length (VLL) in chest X-rays to quantify decreased lung volume. A total of 280 consecutive patients with IIPs were randomly allocated to exploratory and validation cohorts, and 140 controls were selected for each cohort by propensity score-matching. Upper (uVLL; from apex to tracheal carina), lower (lVLL; from carina to costophrenic angle), and total VLL (tVLL; from apex to costophrenic angle), and the l/uVLL ratio were measured on chest X-rays. Patients in the exploratory cohort had significantly decreased uVLL, lVLL, tVLL, and l/uVLL ratio compared with controls (all p < 0.001). Receiver operating characteristic curve analyses demonstrated that lVLL (area under the curve [AUC] 0.86, sensitivity 0.65, specificity 0.92), tVLL (AUC 0.83, sensitivity 0.75, specificity 0.80), and l/uVLL ratio (AUC 0.80, sensitivity 0.72, specificity 0.79) had high diagnostic accuracies for IIPs. These results were reproduced in the validation cohort. IIP patients thus have decreased VLLs, and measurements of VLL may thus aid the accurate detection of IIPs.
Subject terms: Respiratory tract diseases, Diagnosis, Radiography
Introduction
Idiopathic interstitial pneumonias (IIPs) are progressive fibrotic diseases of the lungs with unknown etiology1. Although their precise prevalence is unclear, IIPs are not uncommon and idiopathic pulmonary fibrosis (IPF), as the main subtype of IIPs, was estimated to account for up to 65,000 s death in Europe and up to 17,000 in the United States in 20142, while an epidemiologic survey in Japan reported a prevalence of IPF of 10.0 per 100,000 population and a median survival time of 35 months3. Although IIPs have been poorly treated in the past, early intervention has become increasingly important over the last decade in line with the emergence of anti-fibrotic agents4–7, and routine screening in primary care practice is expected to improve the early detection of IIPs.
IIPs have also become clinically important for non-pulmonologists in relation to the increasing use of biological, molecular targeted, and immune checkpoint-inhibitor agents as standard therapies in various fields of clinical medicine. Despite their efficacy, these novel treatments have raised concern about the occurrence of drug-induced interstitial lung diseases as a life-threatening toxicity8–11. Pre-existing interstitial pneumonias, such as IIPs, are recognized as a major risk factor for drug-induced interstitial lung disease, and patients should thus be screened for interstitial pneumonia before administering these therapies8,9,12,13.
Radiologic imaging plays an important role in the screening and diagnosis of IIPs. Honeycombing, reticular shadows, and ground-grass opacity are typical radiologic features of IIPs1,14–17, and chest computed tomography (CT), especially high-resolution CT, is the gold standard for evaluating these features. However, the risk of radiation exposure and/or overuse of medical resources mean that routine chest CT screening of IIPs is not always practicable, especially in developing countries, where access to CT examinations is sometimes poor because of problems with medical resources and insurance systems.
Decreased lung volume, resulting from pulmonary fibrosis, is another feature of IIPs16,18 and can be confirmed by reduced lung fields and an elevated diaphragm on chest X-ray. However, precise evaluation of IIP-related pulmonary abnormalities on chest X-ray is difficult for non-pulmonologists, such as primary physicians or oncologists, and even well-trained pulmonologists and radiologists may not find it easy to detect early-stage IIPs on chest X-ray18,19. In contrast, reduced lung fields and an elevated diaphragm are easily evaluable and quantifiable on chest X-rays, even by doctors without expertise in diagnostic radiology, by measuring the vertical length of the lung. However, whether or how decreased lung volume is quantified on chest X-rays in patients with IIPs remain unclear. In the present study, we aimed to develop a method to quantify decreased lung volume by measuring the vertical lung length (VLL) on chest X-ray, and to evaluate its usefulness for the detection of IIPs.
Results
Patient characteristics
The current study included an exploratory and validation cohort, each comprising 140 patients with IIPs and 140 propensity-score matched control subjects (Fig. 1). The patient characteristics are presented in Table 1. A total of 137 patients (48.9%) had > 80% of %predicted forced vital capacity (FVC), indicating mild IIP. The patients with IIPs and matched control subjects in each cohort had comparable characteristics, except in terms of spirometry results. The exploratory and validation cohorts had comparable characteristics. The most dominant IIP subtype was IPF (74.2%). All of the patients with IIPs had a reticular pattern on chest CT images, and 70.4% and 94.3% had honeycombing and ground-glass opacity (GGO), respectively (Table 2).
Figure 1.
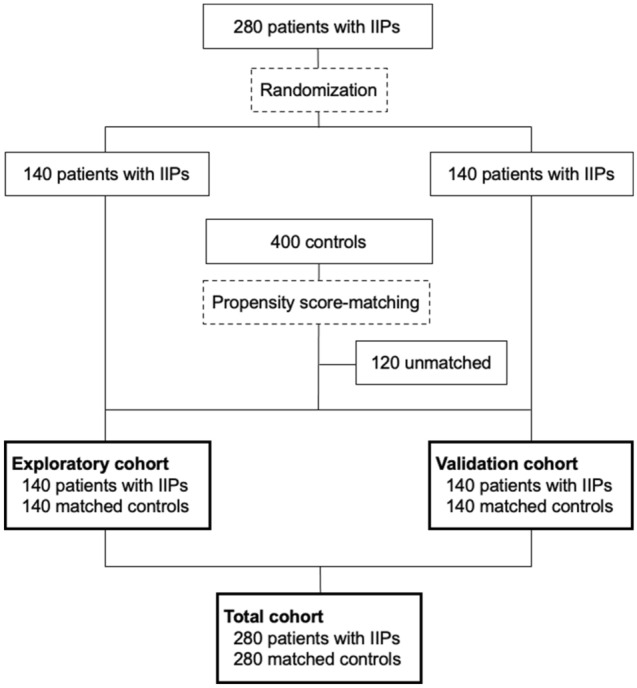
Diagram of the study. Patients with idiopathic interstitial pneumonias (IIPs) were randomized, stratified according to sex and %predicted forced vital capacity. Controls were selected by one-to-one propensity score-matching using age, sex, and body mass index.
Table 1.
Patient characteristics.
| Exploratory cohort | Validation cohort | Total cohort | ||||
|---|---|---|---|---|---|---|
| Controls, n = 140 | IIPs, n = 140 | Control, n = 140 | IIPs, n = 140 | Controls, n = 280 | IIPs, n = 280 | |
| Age | 70.5 (31–93) | 70 (41–92) | 71.0 (24–88) | 69 (36–85) | 71.0 (24–93) | 70 (36–92) |
| Sex, male | 107 (76.4) | 107 (76.4) | 107 (76.4) | 107 (76.4) | 214 (76.4) | 214 (76.4) |
| Body-mass index | 22.4 (16.5–48.0) | 23.1 (16.2–29.0) | 23.4 (14.7–33.1) | 22.7 (15.6–35.6) | 22.9 (14.7–48.1) | 23.0 (15.6–35.6) |
| Spirometry | ||||||
| %predicted FVC | 99.6 (80.9–132.2) | 78.8 (28.0–122.0)* | 100.2 (79.9–137.1) | 79.9 (30.0–132.8)* | 100.0 (79.9–137.1) | 79.3 (28.0–132.8)* |
| %predicted FEV1 | 95.8 (77.9–141.4) | 81.0 (34.8–130.6)* | 98.1 (78.7–135.6) | 84.5 (36.0–141.1)* | 97.1 (77.9–141.4) | 81.4 (34.8–141.1)* |
| FEV1/FVC ratio | 78.0 (70.1–105.1) | 81.5 (47.9–100.0)* | 79.4 (70.1–116.3) | 84.4 (57.0–99.0)* | 79.0 (70.1–116.3) | 83.2 (47.9–100.0)* |
| Subtypes of IIPs | ||||||
| IPF | 104 (74.3) | 104 (74.3) | 208 (74.2) | |||
| Fibrotic NSIP | 6 (4.3) | 8 (5.7) | 14 (5.0) | |||
| Unclassifiable | 19 (13.6) | 16 (11.4) | 35 (12.5) | |||
Data presented as median (range) or number (%).
FEV1 forced expiratory volume in 1s, FVC forced vital capacity, IIPs idiopathic interstitial pneumonias, IPAF interstitial pneumonia with autoimmune features, IPF idiopathic pulmonary fibrosis, NSIP non-specific interstitial pneumonia.
*p < 0.001 compared with control subjects in each cohort.
Table 2.
Findings of chest computed tomography in patients with idiopathic interstitial pneumonias.
| Exploratory cohort, n = 140 | Validation cohort, n = 140 | Total cohort, n = 280 | |
|---|---|---|---|
| Reticular pattern, grade 0/1/2/ ≥ 3 | 0 (0)/94 (67.1)/32 (22.9)/14 (10.0) | 0 (0)/92 (65.7)/42 (30.0)/6 (4.3) | 0 (0)/186 (66.4)/74 (26.4)/20 (7.2) |
| Honeycombing, grade 0/1/2/ ≥ 3 | 34 (24.3)/84 (60.0)/18 (12.9)/4 (2.8) | 49 (35.0)/71 (50.7)/15 (10.7)/5 (3.6) | 83 (29.6)/155 (55.4)/33 (11.8)/9 (3.3) |
| GGO, grade 0/1/2/ ≥ 3 | 10 (7.1)/122 (87.1)/8 (5.7)/0 (0) | 6 (4.3)/112 (80.0)/ 20 (14.3)/2 (1.4) | 16 (5.7)/234 (83.6)/28 (10.0)/2 (0.7) |
| %LAA | 10.7 (1.0–48.5) | 15.1 (1.0–52.0) | 12.8 (1.0–52.0) |
Data presented as median (range) or number (%). The extent of chest CT findings were semi-quantitatively evaluated as follows: grade 0 (0%), grade 1 (< 25%), grade 2 (25–50%), grade 3 (50–75%), and grade 4 (> 75%).
GGO ground-glass opacity, %LAA percentage low-attenuation area.
VLLs in patients with IIPs and controls in the exploratory cohort
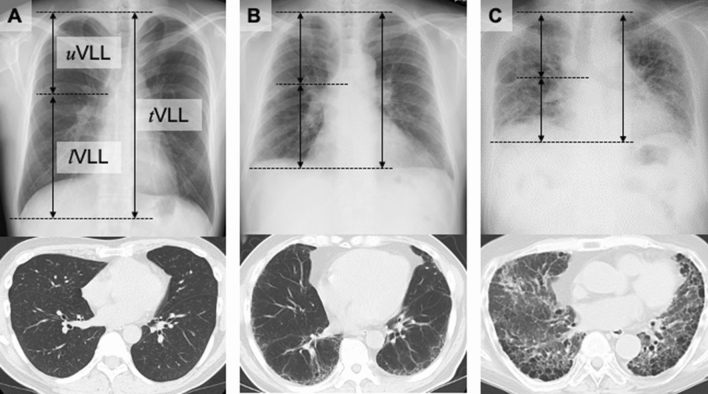
VLL was measured on chest X-rays as follows: (1) from the apex to the costophrenic angle (total VLL, tVLL); (2) from the apex to the carina of the trachea (upper VLL, uVLL); and (3) from the carina to the costophrenic angle (lower VLL, lVLL) (Fig. 2A–C). The VLLs were adjusted by body height [VLLs (mm/m) = unadjusted VLLs (mm)/body height (m)]. The intraclass correlation coefficients for tVLL, uVLL, lVLL, and the l/uVLL ratio in the total cohort were 0.924, 0.890, 0.893, and 0.827, respectively.
Figure 2.
Measurements of vertical lung length (VLL) on chest X-rays. Three VLL measurements were taken: upper VLL (uVLL), from the apex to the costophrenic angle; lower VLL (lVLL), from the tracheal carina to the costophrenic angle; and total VLL (tVLL), from the apex to the costophrenic angle. Measurements were performed in the right lung. Compared with control subjects (A), patients with mild interstitial pneumonia (IIP) (B) and severe IIP (C) demonstrated decreased uVLL, lVLL, and tVLL. The decrease in lVLL was especially notable.
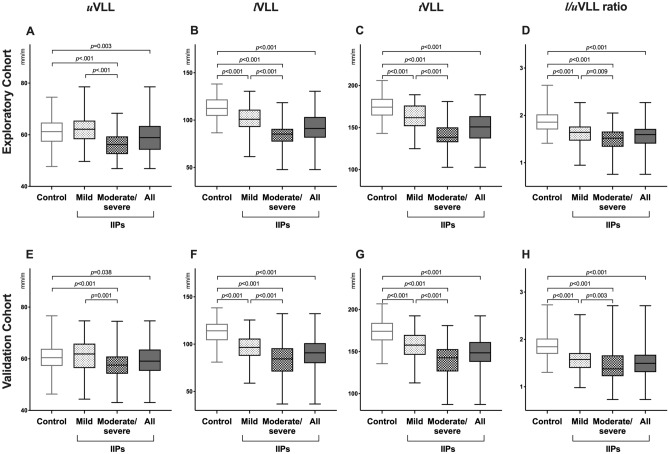
In the exploratory cohort, patients with IIPs had significantly lower uVLL, lVLL, tVLL, and l/uVLL ratio compared with the control subjects (p = 0.003, < 0.001, < 0.001, and < 0.001, respectively) (Fig. 3A–D, Supplementary Table 1). Patients with IIPs were grouped into mild IIPs (%predicted FVC ≥ 80%) and moderate/severe IIPs (< 80%). Patients with moderate/severe IIPs had significantly lower uVLL, lVLL, tVLL, and l/uVLL ratio compared with those with mild IIPs and control subjects (all p < 0.001, except p = 0.009 for l/uVLL ratio for mild IIPs). In addition, patients with mild IIPs also had significantly lower lVLL, tVLL, and l/uVLL ratio, but not uVLL, compared with the control subjects (all p < 0.001, except uVLL).
Figure 3.
Comparison of vertical lung lengths (VLLs) between patients with IIPs and controls. VLLs in the exploratory (A–D) and validation cohorts (E–H). Mild and moderate/severe idiopathic interstitial pneumonias (IIPs) were defined as patients with %predicted forced vital capacity ≥ 80% and < 80%, respectively. White, black, light grey, and grey boxes represent controls, all patients with IIPs, mild IIPs, and moderate/severe IIPs, respectively.
Receiver operating characteristic (ROC) analyses of VLL for detection of IIPs in the exploratory cohort
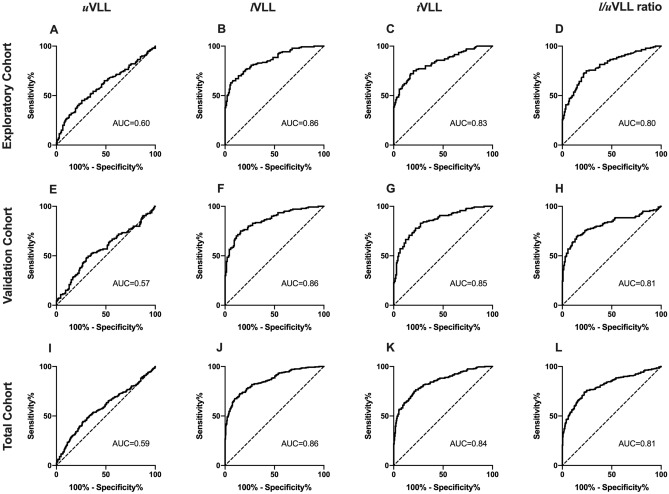
ROC analyses demonstrated high diagnostic accuracies of lVLL (area under the curve [AUC] 0.86), tVLL (AUC 0.83), and l/uVLL ratio (AUC 0.80), but not uVLL (AUC 0.60) for the detection of IIPs (Fig. 4A–D).
Figure 4.
Receiver operating characteristic curves of vertical lung lengths (VLLs) for the detection of IIPs. Receiver operating characteristic curve analyses of VLLs in the exploratory (A–D), validation (E–H), and total cohorts (I–L). AUC area under the curve.
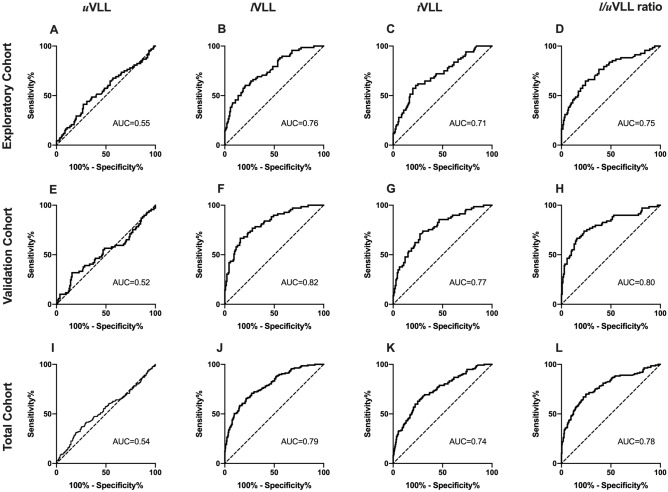
Cut-off values were 98 mm/m for lVLL (sensitivity 0.65, specificity 0.92), 163 mm/m for tVLL (sensitivity 0.75, specificity 0.80), and 1.68 for l/uVLL ratio (sensitivity 0.72, specificity 0.79). When limited to patients with mild IIPs, lVLL, tVLL, and l/uVLL ratio, but not uVLL, also demonstrated high diagnostic accuracies (AUCs 0.76, 0.71, 0.75, and 0.55, respectively) (Fig. 5A–D). Cut-off values were 103 mm/m for lVLL (sensitivity 0.60, specificity 0.79), 164 mm/m for tVLL (sensitivity 0.60, specificity 0.77), and 1.70 for l/uVLL ratio (sensitivity 0.65, specificity 0.76).
Figure 5.
Receiver operating characteristic curves of vertical lung lengths (VLLs) for the detection of mild IIPs. Receiver operating characteristic curve analyses of VLLs for the detection mild IIPs (%predicted forced vital capacity ≥ 80%) in the exploratory (A–D), validation (E–H), and total cohorts (I–L). AUC area under the curve.
Validation of differences in VLLs and cut-off values in validation cohort
The differences in VLLs between patients with IIPs and the control subjects were reproduced in the validation cohort. Patients with IIPs had significantly lower uVLL, lVLL, tVLL, and l/uVLL ratio compared with the control subjects (p = 0.038, < 0.001, < 0.001, and < 0.001, respectively) (Fig. 3E–H, Supplementary Table 1). Patients with moderate/severe IIPs also had significantly lower uVLL, lVLL, tVLL, and l/uVLL ratio compared with patients with mild IIPs and control subjects (all p < 0.001, except p = 0.001 and 0.003 for uVLL and l/uVLL ratio for mild IIP, respectively). Patients with mild IIPs had significantly lower lVLL, tVLL, and l/uVLL ratio, but not uVLL, compared with the control subjects (all p < 0.001, except uVLL).
The AUCs of uVLL, lVLL, tVLL, and l/uVLL ratio for the detection of IIPs were comparable to those in the exploratory cohort (0.57, 0.86, 0.85, and 0.81, respectively) (Fig. 4E–H). The cut-off values for the detection of IIPs determined in the exploratory cohort demonstrated reproducible diagnostic accuracies in the validation cohort (lVLL: sensitivity 0.71, specificity 0.87; tVLL: sensitivity 0.78, specificity 0.78; l/uVLL ratio: sensitivity 0.76, specificity 0.77).
Regarding patients with mild IIPs, the AUCs of uVLL, lVLL, tVLL, and l/uVLL ratio were also comparable to those in the exploratory cohort (0.52, 0.82, 0.77, and 0.80, respectively) (Fig. 5E–H), and the cut-off values determined in the exploratory cohort demonstrated reproducible diagnostic accuracies in the validation cohort (lVLL: sensitivity 0.79, specificity 0.76; tVLL: sensitivity 0.79, specificity 0.74; and l/uVLL ratio: sensitivity 0.75, specificity 0.74).
Final cut-off values in total cohort
The final cut-off values for the detection of IIPs in the total cohort were 98 mm/m for lVLL (sensitivity 0.68, specificity 0.90, AUC 0.86), 163 mm/m for tVLL (sensitivity 0.76, specificity 0.79, AUC 0.84), and 1.68 for l/uVLL ratio (sensitivity 0.74, specificity 0.78, AUC 0.81) (Fig. 4I–L). The AUC for lVLL was significantly higher than those for uVLL (p < 0.001), tVLL (p = 0.030), and l/uVLL ratio (p < 0.001). There was no significant difference in AUCs between tVLL and l/uVLL ratio.
When limited to patients with mild IIPs, the final cut-off values in the total cohort were 103 mm/m for lVLL (sensitivity 0.66, specificity 0.78, AUC 0.79), 164 mm/m for tVLL (sensitivity 0.63, specificity 0.76, AUC 0.74), and 1.70 for l/uVLL ratio (sensitivity 0.70, specificity 0.75, AUC 0.78) (Fig. 5I–L). The AUC for lVLL was significantly higher than those for uVLL (p < 0.001) and tVLL (p < 0.001). There was no significant difference in AUCs between lVLL and l/uVLL ratio, or between tVLL and l/uVLL ratio.
When using the VLL cutoff values in round numbers in clinical practice, an lVLL of 100 mm/m had a sensitivity of 0.71 and specificity of 0.86 for all IIPs, and a sensitivity of 0.54 and specificity of 0.86 for mild IIPs. A tVLL of 160 mm/m had a sensitivity of 0.70 and specificity of 0.83 for all IIPs, and a sensitivity of 0.49 and specificity of 0.83 for mild IIPs. An l/uVLL ratio of 1.70 had a sensitivity of 0.76 and a specificity of 0.75 for all IIPs, and a sensitivity of 0.70 and specificity of 0.75 for mild IIPs.
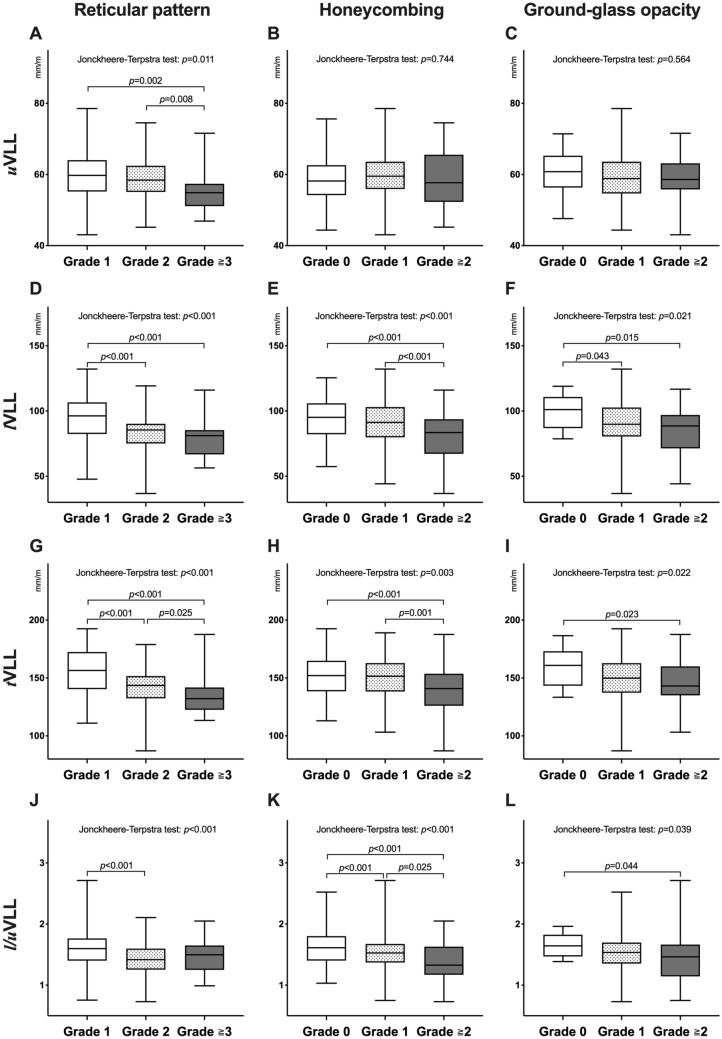
Correlations of VLLs with clinical factors and findings of chest computed tomography
The tVLL and lVLL showed moderate positive correlations with %predicted FVC (r = 0.63 and 0.60, respectively) and %predicted forced expiratory volume in 1 s (FEV1) (r = 0.54 and 0.53, respectively), and weak inverse correlations with body mass index (BMI) (r = − 0.31 and − 0.29, respectively) and FEV1/FVC ratio (r = − 0.27 and − 0.23, respectively) (Table 3). The uVLL and l/uVLL had weak positive correlations with %predicted FVC (r = 0.30 and 0.41, respectively) and %predicted FEV1 (r = 0.22 and 0.38, respectively), and weak inverse correlations with FEV1/FVC ratio (r = − 0.21 and − 0.10, respectively). The uVLL was negatively associated with the extent of the reticular pattern, but not with honeycombing or GGO (p = 0.011, 0.744, and 0.564, respectively) (Fig. 6A–C). lVLL, tVLL, and l/uVLL were negatively associated with the extent of the reticular pattern (all p < 0.001), honeycombing (p < 0.001, 0.003, and < 0.001, respectively), and ground-glass opacity (GGO) on chest computed CT images (p = 0.021, 0.022, and 0.039, respectively) (Fig. 6D–L). The patients with honeycombing (n = 190) had significantly lower lVLL, tVLL, and l/uVLL values than those without (n = 90) (p = 0.005, 0.020, and 0.001, respectively). When compared with the controls, both patients with and without honeycombing had significantly lower uVLL (p = 0.003 and 0.006, respectively), lVLL (both p < 0.001), tVLL (both p < 0.001), and l/uVLL (both p < 0.001) values. Percentage low-attenuation area (%LAA), defined by the percentage area below − 950 HU in the total lung area on chest CT images had weak positive correlations with uVLL, lVLL, and tVLL (r = 0.24, 0.38, and 0.34, respectively) and a very weak correlation with the l/uVLL (r = 0.19) (Table 3). After adjusting for age, sex, BMI, %predicted FVC, %predicted FEV1, and %LAA in multivariate analyses, lVLL, tVLL, and l/uVLL ratio were identified as independent predictive factors for the detection of IIPs and mild IIPs (Tables 4 and 5).
Table 3.
Correlations between vertical lung length and clinical factors.
| Age | Body mass index | %Predicted FVC | %Predicted FEV1 | FEV1/FVC | %LAA | |
|---|---|---|---|---|---|---|
| uVLL | 0.06 (0.13) | − 0.17 (< 0.01) | 0.30 (< 0.01) | 0.22 (< 0.01) | − 0.21 (< 0.01) | 0.24 (< 0.01) |
| lVLL | 0.01 (0.86) | − 0.29 (< 0.01) | 0.60 (< 0.01) | 0.53 (< 0.01) | − 0.23 (< 0.01) | 0.34 (< 0.01) |
| tVLL | 0.03 (0.52) | − 0.31 (< 0.01) | 0.63 (< 0.01) | 0.54 (< 0.01) | − 0.27 (< 0.01) | 0.38 (< 0.01) |
| l/uVLL ratio | − 0.06 (0.20) | − 0.17 (< 0.01) | 0.41 (< 0.01) | 0.38 (< 0.01) | − 0.10 (0.02) | 0.19 (< 0.01) |
Data expressed as Pearson’s correlation coefficient (p value).
FEV1 forced expiratory volume in 1s, FVC forced vital capacity, %LAA percentage low-attenuation area.
Figure 6.
Associations of vertical lung lengths (VLLs) with the extent of lung abnormalities on chest CT images. The association of reticular pattern, honeycombing, and ground-glass opacity with upper VLL (uVLL) (A–C), lower VLL (lVLL) (D–F), total VLL (tVLL) (G–I), and l/uVLL ratio (J–L) are shown. The extents of the lung abnormalities were semi-quantitatively evaluated as follows: grade 0 (0%), grade 1 (< 25%), grade 2 (25–50%), grade 3 (50–75%), and grade 4 (> 75%). The white, grey, and black boxes in the images represent grade 1, 2, and ≥ 3 for reticular pattern, respectively, or grade 0, 1, and ≥ 2 for honeycombing and ground-glass opacity, respectively.
Table 4.
Logistic regression analyses for idiopathic interstitial pneumonias.
| Variables | Odds ratio | p value | Odds ratio | p value | Odds ratio | p value | Odds ratio | p value |
|---|---|---|---|---|---|---|---|---|
| Age | 0.99 (0.96–1.01) | 0.361 | 0.99 (0.97–1.01) | 0.391 | 0.99 (0.96–1.01) | 0.337 | 0.98 (0.96–1.01) | 0.264 |
| Sex, male | 1.31 (0.69–2.51) | 0.408 | 0.78 (0.42–1.43) | 0.417 | 1.09 (0.56–2.10) | 0.807 | 0.70 (0.36–1.33) | 0.274 |
| BMI | 0.83 (0.76–0.91) | < 0.001 | 0.98 (0.92–1.05) | 0.569 | 0.82 (0.75–0.89) | < 0.001 | 0.91 (0.85–0.98) | 0.013 |
| FVC%pred | 0.95 (0.91–0.98) | < 0.001 | 0.91 (0.88–0.93) | < 0.001 | 0.94 (0.91–0.97) | < 0.001 | 0.91 (0.88–0.94) | < 0.001 |
| FEV1%pred | 0.99 (0.96–1.02) | 0.536 | 1.00 (0.97–1.03) | 0.778 | 1.00 (0.97–1.03) | 0.910 | 1.00 (0.97–1.04) | 0.819 |
| %LAA | 0.98 (0.96–1.00) | 0.109 | 0.97 (0.96–0.99) | 0.011 | 0.98 (0.96–1.00) | 0.078 | 0.98 (0.96–1.00) | 0.024 |
| tVLL | 0.93 (0.91–0.95) | < 0.001 | ||||||
| uVLL | 1.03 (0.99–1.06) | 0.144 | ||||||
| lVLL | 0.90 (0.88–0.93) | < 0.001 | ||||||
| l/uVLL ratio | 2.12 × 10–2 (0.76 × 10–2–0.60 × 10–1) | < 0.001 |
Data expressed as odds ratio (95% confidence interval). Odds ratios for continuous variables expressed as per 1 value increase.
BMI body mass index, FEV1%pred percentage predicted forced expiratory volume in 1s, FVC%pred percentage predicted forced vital capacity, tVLL total vertical lung length, uVLL upper vertical lung length, lVLL lower vertical lung length, %LAA percentage low-attenuation area.
Table 5.
Logistic regression analyses for mild idiopathic interstitial pneumonias.
| Variables | Odds ratio | p value | Odds ratio | p value | Odds ratio | p value | Odds ratio | p value |
|---|---|---|---|---|---|---|---|---|
| Age | 0.99 (0.96–1.02) | 0.397 | 0.99 (0.97–1.02) | 0.507 | 0.98 (0.96–1.01) | 0.280 | 0.99 (0.96–1.01) | 0.304 |
| Sex, male | 1.40 (0.72–2.71) | 0.324 | 0.70 (0.38–1.30) | 0.266 | 1.21 (0.61–2.40) | 0.589 | 0.69 (0.35–1.35) | 0.277 |
| BMI | 0.84 (0.77–0.92) | < 0.001 | 1.01 (0.94–1.08) | 0.815 | 0.82 (0.74–0.90) | < 0.001 | 0.93 (0.86–1.00) | 0.038 |
| FVC%pred | 0.97 (0.94–1.01) | 0.132 | 0.94 (0.91–0.97) | < 0.001 | 0.97 (0.94–1.01) | 0.123 | 0.95 (0.92–0.99) | 0.007 |
| FEV1%pred | 0.99 (0.96–1.02) | 0.523 | 0.99 (0.96–1.03) | 0.725 | 1.00 (0.96–1.03) | 0.849 | 1.00 (0.97–1.04) | 0.986 |
| %LAA | 0.98 (0.96–1.01) | 0.155 | 0.98 (0.96–1.00) | 0.039 | 0.98 (0.96–1.00) | 0.120 | 0.98 (0.96–1.00) | 0.061 |
| tVLL | 0.93 (0.91–0.95) | < 0.001 | ||||||
| uVLL | 1.05 (1.01–1.10) | 0.016 | ||||||
| lVLL | 0.90 (0.88–0.92) | < 0.001 | ||||||
| l/uVLL ratio | 1.14 × 10–2 (0.34 × 10–2–0.38 × 10–1) | < 0.001 |
Data expressed as odds ratio (95% confidence interval). Odds ratios for continuous variables expressed as per 1 value increase.
BMI body mass index, FEV1%pred percentage predicted forced expiratory volume in 1s, FVC%pred percentage predicted forced vital capacity, tVLL total vertical lung length, uVLL upper vertical lung length, lVLL lower vertical lung length, %LAA percentage low-attenuation area.
Subgroup analysis of patients with IPF and non-IPF
When patients with IIPs were divided into IPF and non-IPF groups, both groups demonstrated significantly lower uVLL (p = 0.003 and 0.005, respectively), tVLL (both p < 0.001), lVLL (both p < 0.001), and l/uVLL ratio (both p < 0.001) compared with the control subjects. Compared with the IPF group, non-IPF patients had significantly higher lVLL and l/uVLL ratio (p = 0.043 and 0.007, respectively), but similar uVLL and tVLL (p = 0.490 and 0.132, respectively). After adjusting for age, sex, BMI, %predicted FVC, %predicted FEV1, and %LAA in multivariate logistic regression analysis, there was no significant difference in uVLL, lVLL, tVLL, or l/uVLL ratio between the IPF and non-IPF groups (Supplementary Table 2).
Secondary interstitial pneumonia cohort
Next, we evaluated 240 patients with secondary interstitial pneumonias (IPs). The secondary IPs comprised collagen vascular disease (CVD)-associated IPs (n = 116), sarcoidosis (n = 76), chronic hypersensitivity pneumonia (CHP) (n = 40), and pneumoconiosis (n = 8). The types of CVD were rheumatoid arthritis (n = 49), dermatomyositis (n = 26), Sjögren syndrome (n = 17), scleroderma (n = 8), systemic lupus erythematosus (n = 2), a combination of two or more CVDs (n = 5), and others (n = 14). Compared with the patients with IIPs, those with secondary IPs were significantly younger (p < 0.001), female-dominant (p < 0.001), and had lower BMI (p = 0.006), higher %predicted FVC, higher %predicted FEV1 (p < 0.001), and lower FEV1/FVC (p = 0.009) (Supplementary Table 3). The patients with secondary IPs demonstrated significantly lower uVLL (p = 0.014) and higher lVLL, tVLL, and l/uVLL ratio (all p < 0.001), compared with those with IIPs (Supplementary Table 4).
When limited to the patients with %predicted FVC ≥ 80%, patients with secondary IPs demonstrated significantly lower uVLL (p = 0.002) and higher lVLL, tVLL, and l/uVLL ratio (p < 0.001, 0.002, and < 0.001, respectively), compared with those with IIPs (Supplementary Table 4).
Compared with patients with IPF, those with CVD-IP had significantly higher lVLL (p < 0.001), tVLL (p = 0.001), and l/uVLL ratio (p < 0.001); those with sarcoidosis had significantly lower uVLL (p = 0.009) and higher lVLL (p < 0.001), tVLL (p < 0.001), and l/uVLL ratio (p < 0.001); those with CHP had significantly lower uVLL (p < 0.001) and higher lVLL (p < 0.001) and l/uVLL ratio (p < 0.001); and those with pneumoconiosis had significantly higher lVLL (p < 0.001), tVLL (p = 0.003), and l/uVLL ratio (p = 0.002).
Discussion
In the present study, we evaluated reduced lung volume by measuring VLLs on chest X-rays, and found that VLLs were significantly decreased in patients with IIPs. Among the measured VLLs, lVLL, tVLL, and l/uVLL ratio demonstrated high diagnostic accuracies for the detection of IIPs, with lVLL having the highest accuracy. Importantly, decreases in lVLL, tVLL, and l/uVLL ratio were also observed in patients with mild IIPs, with a %predicted FVC > 80%. Chest X-rays are a non-invasive, low-radiation exposure, and low-cost diagnostic method, and the measurement of VLLs is simple and easy, even for doctors with no expertise in diagnostic radiology, thus aiding the early detection of IIPs in clinical practice.
Among the decreases in VLLs observed in patients with IIPs, the decrease in lVLL was more prominent compared with uVLL, possibly because pulmonary fibrosis occurs predominantly in the lower lobe of the lungs. Although the uneven distribution of pulmonary fibrosis in the lower lungs is well known in IPF14–16,20, the underlying mechanisms are unknown. One hypothesis suggests that mechanical stress caused by repeated ventilation is stronger in the lower lobe because of the large motion of the chest wall and diaphragm20–22. In addition to IPF, most IIPs demonstrate predominantly lower lobe lesions16,19,20,23. Patients in the current study with non-IPF IIPs showed decreased lVLL and l/uVLL ratio, similar to patients with IPF.
Interestingly, VLLs were decreased in patients with IIP but with no decline in %predicted FVC. In addition to lung elasticity, pulmonary function also depends on thoracic elasticity and the respiratory muscles, and patients with IPF were reported to show only a weak or moderate correlation between pulmonary function and radiologic severity at baseline and changes during follow-up17,24. In the present study, VLLs were only moderately correlated with %predicted FVC, and the decreases in VLLs were independent of clinical factors, including %predicted FVC. In addition, differences in the cut-off values between all IIPs and mild IIPs were small. These characteristics of VLLs thus enable the detection of early-stage IIPs, but conversely, VLLs may be of little clinical use for estimating the deterioration of pulmonary function.
Among the measured VLLs, although lVLL demonstrated the highest AUC for the detection of IIPs, the diagnostic accuracies of lVLL, tVLL, and l/uVLL ratio were similar from a clinical perspective. In contrast to lVLL and tVLL, which need to be adjusted for body height, l/uVLL ratio does not depend on height and can be calculated from chest X-ray images, and can thus be used as an alternative to lVLL.
The current study had three main limitations. First, VLLs are only evaluable on chest X-rays performed in an upright position, in patients with no abnormal changes other than interstitial pneumonias. Chest CT should be used to screen for IIPs in patients in the decubitus position, or those with a history of chest surgery or other obvious chest abnormalities. Similarly, severely obese patients may have an elevated diaphragm due to visceral fat and may therefore be unsuitable for the evaluation of VLLs. Second, the differential distribution of pulmonary fibrosis affects VLLs. Patients with secondary IPs demonstrated lower uVLL and higher lVLL than those with IIPs. This may be because secondary IPs, including sarcoidosis, CHP, and pneumoconiosis, demonstrate upper-lobe-predominant fibrosis, whereas IPF, the most dominant phenotype among IIPs, demonstrates lower-lobe-predominant fibrosis25–27. Furthermore, CVD-IPs are a heterogeneous group of different disease phenotypes, each with distinct lung abnormalities varying according to the phenotype. The utility of VLLs in secondary IPs needs to be investigated further. Third, the present study was retrospective in nature, with limited clinical information. The existence of respiratory symptoms, dyspnea, or abnormal respiratory sounds on auscultation may increase the diagnostic ability in combination with VLLs. The clinical utility of VLLs thus needs to be validated in a prospective, observational study in a real-world setting.
Conclusions
Patients with IIPs, including those with mild IIPs, had decreased VLLs, especially lVLL, on chest X-ray. The measurements of lVLL, tVLL, and l/uVLL ratio demonstrated high diagnostic accuracies for the detection of IIPs. This simple method may aid the early detection of IIPs by non-respiratory practitioners and physicians in areas with poor access to CT examinations.
Methods
Study design
This retrospective observational study was conducted in accordance with the ethical standards described in the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board of Hamamatsu University School of Medicine (No. 20-015). Each patient provided written informed consent to be included in the study. The study was registered with the University Hospital Medical Information Network Clinical Trial Registry (identification code: 000040724).
Patient eligibility
We retrospectively evaluated the medical records of patients with IIPs in our institute from January 2000 to December 2019. The diagnosis of IIP was made according to American Thoracic Society/European Respiratory Society Clinical Practice Guidelines1. The inclusion criteria were as follows: chest X-ray and spirometry performed within 1 week of each other, and clinically stable disease with no worsening for at least 4 weeks before spirometry and chest X-ray. If multiple data were available for the same patient, the earliest data from the initial diagnosis of IIP were evaluated. The exclusion criteria were as follows: patients with pleuroparenchymal fibroelastosis, characterized by upper-lobe-dominant fibrosis28; patients with anatomical chest abnormalities, abnormal chest shadows without IIP (e.g. lung cancer, pleural effusion, or pneumothorax), or a history of chest surgery; patients with missing data for either chest X-ray or spirometry within 1 week; and patients with clinically unstable disease within 4 weeks (e.g. pneumonia or acute exacerbation). Clinically stable patients without IIPs were evaluated as control subjects. Control subjects were required to have normal spirometry, no pulmonary disease, no anatomical chest abnormality, and no history of chest surgery.
Exploratory and validation cohorts
A total of 280 consecutive patients with IIPs and 400 control subjects were evaluated. The patients with IIPs were randomly allocated to the exploratory or validation cohort (Fig. 1). Control subjects were selected for each cohort by propensity score-matching using age, sex, and BMI. Each cohort finally included 140 patients with IIPs and 140 control subjects. The two cohorts were merged into a total cohort for final analysis.
Secondary interstitial pneumonia cohorts
A total of 240 consecutive patients with secondary IPs, including connective tissue diseases, sarcoidosis, hypersensitivity pneumonia, and pneumoconiosis, were evaluated as the secondary IP cohort.
Evaluation of chest X-rays and computed tomography
Lung volume loss was evaluated by measuring uVLL, lVLL, and tVLL in the right lung on chest X-rays taken in the upright position and at maximum inspiration (Fig. 2A–C). The data were adjusted for body height [VLLs (mm/m) = unadjusted VLLs (mm)/body height (m)]. The l/u VLL ratio was also calculated. The right (instead of the left) lung was evaluated to eliminate the possible effect of cardiac shadow. VLLs were evaluated by two independent investigators and the results are expressed as a mean of the two estimates. The extent of the reticular pattern, honeycombing, and GGO on chest CT images were semi-quantitatively evaluated as follows: grade 0 (0%), grade 1 (< 25%), grade 2 (25–50%), grade 3 (50–75%), and grade 4 (> 75%)29. The definitions of reticular pattern, honeycombing, and GGO were according to the Fleishner Society criteria30. The %LAA on chest CT images was calculated using image-analyzing software (SYNAPSE VINCENT; Fuji Film, Tokyo, Japan).
Statistical analyses
The randomization of patients with IIPs was stratified by sex and %predicted FVC. One-to-one propensity score-matching was performed using age, sex, and BMI as co-variables. Continuous variables were compared by Wilcoxon’s rank sum test and categorical variables by Fisher’s exact test. The predictive values of VLLs for the diagnosis of IIPs were evaluated by multivariate logistic regression analysis. The cut-off values of VLLs for the diagnosis of IIPs were estimated by ROC analysis and determined using Youden’s index (maximum value of [sensitivity + specificity − 1]). The correlations between VLLs and clinical factors were evaluated by Pearson’s correlation analysis. The correlations of VLLs with the increased extent of lung abnormalities in the patients with IIPs were evaluated by the Jonckheere–Terpstra test. The inter-observer reproducibility was evaluated by intraclass correlation analyses. A p value < 0.05 (two-sided) was considered significant. All statistical analyses were carried out using JMP v13.0.0 (SAS Institute Japan, Tokyo, Japan), except The Jonckheere–Terpstra test was performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).
Supplementary Information
Acknowledgements
We thank Susan Furness, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
M.K.: conceptualization, methodology, interpretation of data, writing-original draft. Y.A., H.Y.: acquisition and analysis. H.H., Y.S., K.F.: conceptualization and supervision. T.F., N.E., Y.N., N.I.: conceptualization, supervision, and writing-review and editing. T.S.: conceptualization, methodology, writing-review and editing, and supervision.
Data availability
All data generated or analyzed during this study are included in this published article and Supplementary Information file.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-87452-z.
References
- 1.Travis WD, et al. An official American thoracic society/european respiratory society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 2013;188:733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hutchinson JP, McKeever TM, Fogarty AW, Navaratnam V, Hubbard RB. Increasing global mortality from idiopathic pulmonary fibrosis in the twenty-first century. Ann. Am. Thorac. Soc. 2014;11:1176–1185. doi: 10.1513/AnnalsATS.201404-145OC. [DOI] [PubMed] [Google Scholar]
- 3.Natsuizaka M, et al. Epidemiologic survey of Japanese patients with idiopathic pulmonary fibrosis and investigation of ethnic differences. Am. J. Respir. Crit. Care Med. 2014;190:773–779. doi: 10.1164/rccm.201403-0566OC. [DOI] [PubMed] [Google Scholar]
- 4.Richeldi L, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014;370:2071–2082. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 5.King TE, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 2014;370:2083–2092. doi: 10.1056/NEJMoa1402582. [DOI] [PubMed] [Google Scholar]
- 6.Costabel U, et al. Pirfenidone is efficacious in patients with idiopathic pulmonary fibrosis (IPF) and mild restrictive disease. Pneumologie. 2016;70:2014–2015. [Google Scholar]
- 7.Flaherty KR, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N. Engl. J. Med. 2019;381:1718–1727. doi: 10.1056/NEJMoa1908681. [DOI] [PubMed] [Google Scholar]
- 8.Chikura B, Lane S, Dawson JK. Clinical expression of leflunomide-induced pneumonitis. Rheumatology. 2009;48:1065–1068. doi: 10.1093/rheumatology/kep050. [DOI] [PubMed] [Google Scholar]
- 9.Shi L, Tang J, Tong L, Liu Z. Risk of interstitial lung disease with gefitinib and erlotinib in advanced non-small cell lung cancer: a systematic review and meta-analysis of clinical trials. Lung Cancer. 2014;83:231–239. doi: 10.1016/j.lungcan.2013.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Nishino M, Giobbie-Hurder A, Hatabu H, Ramaiya NH, Hodi FS. Incidence of programmed cell death 1 inhibitor-related pneumonitis in patients with advanced cancer a systematic review and meta-analysis. JAMA Oncol. 2016;2:1607–1616. doi: 10.1001/jamaoncol.2016.2453. [DOI] [PubMed] [Google Scholar]
- 11.Hallowell RW, Horton MR. Interstitial lung disease in patients with rheumatoid arthritis: spontaneous and drug induced. Drugs. 2014;74:443–450. doi: 10.1007/s40265-014-0190-z. [DOI] [PubMed] [Google Scholar]
- 12.Yamaguchi T, et al. Pre-existing pulmonary fibrosis is a risk factor for anti-PD-1-related pneumonitis in patients with non-small cell lung cancer: a retrospective analysis. Lung Cancer. 2018;125:212–217. doi: 10.1016/j.lungcan.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Nakanishi Y, et al. Pre-existing interstitial lung abnormalities are risk factors for immune checkpoint inhibitor-induced interstitial lung disease in non-small cell lung cancer. Respir. Investig. 2019;57:451–459. doi: 10.1016/j.resinv.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Raghu G, et al. An Official ATS/ERS/JRS/ALAT Statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011;183:788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raghu G, et al. Diagnosis of idiopathic pulmonary fibrosis an official ATS/ERS/JRS/ALAT clinical practice guideline. Am. J. Respir. Crit. Care Med. 2018;198:e44–e68. doi: 10.1164/rccm.201807-1255ST. [DOI] [PubMed] [Google Scholar]
- 16.Jacob J, Hansell DM. HRCT of fibrosing lung disease. Respirology. 2015;20:859–872. doi: 10.1111/resp.12531. [DOI] [PubMed] [Google Scholar]
- 17.Lee HY, et al. High-resolution CT findings in fibrotic idiopathic interstitial pneumonias with little honeycombing: serial changes and prognostic implications. Am. J. Roentgenol. 2012;199:982–989. doi: 10.2214/AJR.11.8192. [DOI] [PubMed] [Google Scholar]
- 18.Walsh SLF, et al. Role of imaging in progressive-fibrosing interstitial lung diseases. Eur. Respir. Rev. 2018;27:1–8. doi: 10.1183/16000617.0073-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller WT. Chest radiographic evaluation of diffuse infiltrative lung disease: review of a dying art. Eur. J. Radiol. 2002;44:182–197. doi: 10.1016/S0720-048X(02)00264-4. [DOI] [PubMed] [Google Scholar]
- 20.Galvin JR, Frazier AA, Franks TJ. Collaborative radiologic and histopathologic assessment of fibrotic lung disease. Radiology. 2010;255:692–706. doi: 10.1148/radiol.10090717. [DOI] [PubMed] [Google Scholar]
- 21.Suki B, Bates JHT. Lung tissue mechanics as an emergent phenomenon. J. Appl. Physiol. 2011;110:1111–1118. doi: 10.1152/japplphysiol.01244.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leslie KO. Idiopathic pulmonary fibrosis may be a disease of recurrent, tractional injury to the periphery of the aging lung: a unifying hypothesis regarding etiology and pathogenesis. Arch. Pathol. Lab. Med. 2012;136:591–600. doi: 10.5858/arpa.2011-0511-OA. [DOI] [PubMed] [Google Scholar]
- 23.Ebner L, et al. Meta-analysis of the radiological and clinical features of usual interstitial pneumonia (UIP) and nonspecific interstitial pneumonia (NSIP) PLoS ONE. 2020;15:1–21. doi: 10.1371/journal.pone.0226084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balestro E, et al. High-resolution CT change over time in patients with idiopathic pulmonary fibrosis on antifibrotic treatment. J. Clin. Med. 2019;8:1469. doi: 10.3390/jcm8091469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nunes H, et al. Imaging of sarcoidosis of the airways and lung parenchyma and correlation with lung function. Eur. Respir. J. 2012;40:750–765. doi: 10.1183/09031936.00025212. [DOI] [PubMed] [Google Scholar]
- 26.Jeong YJ, et al. Chronic hypersensitivity pneumonitis and pulmonary sarcoidosis: differentiation from usual interstitial pneumonia using high-resolution computed tomography. Semin. Ultrasound CT MRI. 2014;35:47–58. doi: 10.1053/j.sult.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 27.Jun JS, et al. Complications of pneumoconiosis: radiologic overview. Eur. J. Radiol. 2013;82:1819–1830. doi: 10.1016/j.ejrad.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 28.Watanabe K, et al. Criteria for the diagnosis of idiopathic pleuroparenchymal fibroelastosis: a proposal. Respir. Investig. 2019;57:312–320. doi: 10.1016/j.resinv.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 29.Nishimoto K, et al. Pneumothorax in connective tissue diseaseassociated interstitial lung disease. PLoS ONE. 2020;15:1–12. doi: 10.1371/journal.pone.0235624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hansell DM, et al. Fleischner society: glossary of terms for thoracic imaging. Radiology. 2008;246:697–722. doi: 10.1148/radiol.2462070712. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article and Supplementary Information file.