Key Points
Question
Were state-specific mobility restrictions during the first wave of the COVID-19 pandemic in the United States associated with the well-being of individuals in groups that have historically been marginalized on the basis of race/ethnicity, sex, or income?
Findings
In this cross-sectional study of 1 088 314 US adults, African American individuals with low income, Hispanic individuals, and women of all racial/ethnic groups had higher risks of experiencing unemployment, class cancellations, food insufficiency, and mental health problems during the first wave of the COVID-19 pandemic.
Meaning
These findings suggest that public health policies that ignore existing distributions of risks to well-being may be intrinsically regressive if they fail to target necessary relief measures to individuals who have historically experienced the most marginalization.
This cross-sectional study identifies and quantifies the association of race/ethnicity, sex, and income as well as state-specific lockdown measures with 6 well-being dimensions in the United States.
Abstract
Importance
An accurate understanding of the distributional implications of public health policies is critical for ensuring equitable responses to the COVID-19 pandemic and future public health threats.
Objective
To identify and quantify the association of race/ethnicity–based, sex-based, and income-based inequities of state-specific lockdowns with 6 well-being dimensions in the United States.
Design, Setting, and Participants
This pooled, repeated cross-sectional study used data from 14 187 762 households who participated in phase 1 of the population-representative US 2020 Household Pulse Survey (HPS). Households were invited to participate by email, text message, and/or telephone as many as 3 times. Data were collected via an online questionnaire from April 23 to July 21, 2020, and participants lived in all 50 US states and the District of Columbia.
Exposures
Indicators of race/ethnicity, sex, and income and their intersections.
Main Outcomes and Measures
Unemployment; food insufficiency; mental health problems; no medical care received for health problems; default on last month’s rent or mortgage; and class cancellations with no distance learning. Race/ethnicity, sex, income, and their intersections were used to measure distributional implications across historically marginalized populations; state-specific, time-varying population mobility was used to measure lockdown intensity. Logistic regression models with pooled repeated cross-sections were used to estimate risk of dichotomous outcomes by social group, adjusted for confounding variables.
Results
The 1 088 314 respondents (561 570 [51.6%; 95% CI, 51.4%-51.9%] women) were aged 18 to 88 years (mean [SD], 51.55 [15.74] years), and 826 039 (62.8%; 95% CI, 62.5%-63.1%) were non-Hispanic White individuals; 86 958 (12.5%; 95% CI, 12.4%-12.7%), African American individuals; 86 062 (15.2%; 95% CI, 15.0%-15.4%), Hispanic individuals; and 50 227 (5.6%; 95% CI, 5.5%-5.7%), Asian individuals. On average, every 10% reduction in mobility was associated with higher odds of unemployment (odds ratio [OR], 1.3; 95% CI, 1.2-1.4), food insufficiency (OR, 1.1; 95% CI, 1.1-1.2), mental health problems (OR, 1.04; 95% CI, 1.0-1.1), and class cancellations (OR, 1.1; 95% CI, 1.1-1.2). Across most dimensions compared with White men with high income, African American individuals with low income experienced the highest risks (eg, food insufficiency, men: OR, 3.3; 95% CI, 2.8-3.7; mental health problems, women: OR, 1.9; 95% CI, 1.8-2.1; medical care inaccessibility, women: OR, 1.7; 95% CI, 1.6-1.9; unemployment, men: OR, 2.8; 95% CI, 2.5-3.2; rent/mortgage defaults, men: OR, 5.7; 95% CI, 4.7-7.1). Other high-risk groups were Hispanic individuals (eg, unemployment, Hispanic men with low income: OR, 2.9; 95% CI, 2.5-3.4) and women with low income across all races/ethnicities (eg, medical care inaccessibility, non-Hispanic White women: OR, 1.8; 95% CI, 1.7-2.0).
Conclusions and Relevance
In this cross-sectional study, African American and Hispanic individuals, women, and households with low income had higher odds of experiencing adverse outcomes associated with the COVID-19 pandemic and stay-at-home orders. Blanket public health policies ignoring existing distributions of risk to well-being may be associated with increased race/ethnicity–based, sex-based, and income-based inequities.
Introduction
Since the COVID-19 outbreak was declared a global pandemic, the threat of the virus has been evolving and unpredictable. However, its disproportionate effect on populations that have been historically marginalized has been persistent and unsurprising.1 COVID-19 has highlighted systemic inequity as a planetary issue, a preexisting condition of disadvantage underlying the social structure of society, such that COVID-19 cannot be thought of as merely a health crisis. Structural and institutional disparities, particularly racial/ethnic disparities, are central to understanding the implications and mitigation of the disease.2,3 Increasingly, research, aided by ample historical precedents, indicates that the most socially marginalized populations are bearing the heaviest burden.4
During the early months of COVID-19 in the United States, stay-at-home orders were implemented in most states. The goal of these orders was to reduce the potential for personal contact, which can contribute to the spread of COVID-19.5 Statewide mandates, while varying in strictness, were blanket strategies that restricted movement by requiring citizens to stay home except to conduct essential tasks or business. These policies have been associated with important reductions in cases and deaths,6 although the benefits have been unequally distributed across the population. Groups that have historically been marginalized have disproportionately borne the burden of COVID-19–related infection and mortality3 as well as the unintended consequences of policies designed to prevent this disease burden.7,8,9 Given the biomedical nature of the pandemic, health research on pandemic-related inequities has largely been illness oriented, focusing on the disease burden1,2,10; however, a more broadly based epistemology of health11,12 recognizes that health and well-being depend on multiple factors (eg, social, environmental, economic) and require consideration of the latter incidental burdens.11 While evidence of the consequences of COVID-19 policies continues to grow,8,9,13,14 the distribution of risks to well-being associated with human mobility restrictions has yet to be modeled for the United States.9 Emergency response options have complex trade-offs between short-term and long-term consequences, between potential harms and benefits,15 all of which interact with existing disparities in well-being. Quantifying the heterogeneity of risks across the population can aid decision-makers in predicting and balancing consequences prior to policy implementation for more equitable COVID-19 pandemic outcomes.
The objective of this study was to estimate the associations between state-specific mobility restrictions and well-being across historically excluded groups, including those groups at the intersections of race/ethnicity, sex, and income categorizations.16 We hypothesized that the distribution of risks to well-being would reproduce patterns of social marginalization. We hypothesized that when mobility restrictions were high, the risk of COVID-19 spreading may have been lower and the risk of socioeconomic adversity higher.
Methods
Data
Data are from phase 1 of the Interagency Federal Statistical Rapid Response Survey to Measure Effects of the Coronavirus (COVID-19) Pandemic on the United States Household Population: 2020 Household Pulse Survey (HPS). The HPS used the US Census Bureau’s Master Address File to contact households via email, text message, and/or telephone and produce representative estimates at the national, state, and metropolitan area levels. A total of 1 088 314 successful interviews were completed via internet questionnaires between April 23 (week 1) and July 21 (week 12), 2020. Sample size was determined such that a 2 percentage point difference in weekly HPS survey estimates would be detectable for an estimated 40% of the population with a 90% confidence interval at each level.17 A Census Bureau Notice and Consent Warning was displayed prior to participation, and accessing the survey indicated participants’ consent.18 The data are publicly available and approved under the Office of Management and Budget.19 Further technical details are available on the Census Bureau website.18 A second data source was the publicly available COVID-19 projections of the Institute of Health Metrics and Evaluation (IHME). IHME provides modeled state-level estimates of (1) weekly case and death rates (sourced from the Johns Hopkins Coronavirus Resource Center20) and (2) movement of US state populations based on anonymous cell phone data from several technology companies (ie, Facebook, Google, SafeGraph, and Descartes Labs).21 Finally, we obtained population estimates stratified by race from the American Community Survey Demographic and Housing 2015 to 2019 Estimates of the Census Bureau.22 The study used secondary deidentified data, making it exempt from institutional review board review. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Outcomes
We examined the association of the COVID-19 pandemic with important indicators of well-being (eTable 1 in the Supplement). For several survey items, the questionnaire was explicit in asking participants to self-report causality by attributing outcomes to the pandemic (eg, “due to the coronavirus pandemic” or “since March 13, 2020”). Because of this unambiguity, we regarded these outcomes as pandemic-related. In total, we studied 6 composite well-being indicators, including pandemic-related unemployment, attributed to contracting COVID-19, being afraid of spreading COVID-19, being laid off because of COVID-19, or a business closing because of COVID-19; pandemic-related food insufficiency, defined as there sometimes or often not being enough food to eat in the last 7 days or food availability becoming worse after March 13, 2020; mental health problems, defined as respondents having scores of 12 or greater on indices of anxiety, worry, lack of pleasure, and hopelessness14; pandemic-related inaccessibility of medical care for health problems, defined as the respondent needing medical care for something other than COVID-19 in the past 4 weeks but not receiving it because of the pandemic; default on last month’s rent or mortgage; and pandemic-related class cancellations among households with school-aged children, defined as classes normally taught in person at school cancelled without any distance learning option (eTable 1 in the Supplement). If the outcome could not be explicitly attributed to the COVID-19 pandemic, which included mental health problems and default on rent or mortgage, it was restricted to the extremes of its distributions to capture the most severe conditions (eTable 2 in the Supplement).
Exposures
This study focused on 4 key exposures: race/ethnicity, sex, income, and mobility restrictions. Race/ethnicity was measured as the 3 dummy variables of African American, Hispanic, and Asian, with the non-Hispanic White population serving as the referent. In the HPS, race/ethnicity classifications were options defined by the Census Bureau and originally included for weighting survey estimates.18 Sex was measured as a dummy variable for female respondents. Income was measured by 2 dummy variables. Low-income households were those earning less than $35 000 per year, and lower-middle income households were those earning between $35 000 and $75 000 per year. The referent consisted of the comparatively higher-income households earning more than $75 000 per year.23
Mobility restriction measured the reduced potential for personal contact; these restrictions were designed to help to control viral spread.5 During the study period, mobility was dependent on the imposition of state-specific government mandates, including educational facility and business closures, stay-at-home orders, public gathering restrictions, and travel restrictions; therefore, it operated as an ecological-level exposure.24 We exploited within-state weekly variation to estimate the associations of mobility restrictions with the outcomes. Mobility restriction was expressed as a percentage, with 0% representing no restriction and 100% representing complete restriction on mobility (eFigure 1 and eFigure 2 in the Supplement).
Other covariates included age, education, marital status, and household size. State-specific and survey week–specific COVID-19 cases and deaths per 1000 were used as ecological-level controls24 in all models.
Statistical Analysis
We conducted our analyses using 2 sets of regression models to study (1) differences in outcomes with respect to race, sex, and income independently and (2) interactions of race, sex, and income. In the first set of logistic regression models, we determined the associations of race/ethnicity, sex, income (individual level), and mobility (state level) with each of the 6 binary outcomes (individual level). We modeled mobility as a continuous variable, assuming the outcomes responded linearly to changes in mobility (eTable 3 in the Supplement). In addition to the individual-level and household-level covariates, we included a discrete variable indicating survey week, which controlled for trends common to all states during the study period. We included 50 state dummy variables to control for all unobserved time-invariant confounders operating at the state level, such as the potential confounder of state-specific political ideology. Conditional on controlling for state dummy variables, mobility changes are likely quasi-exogenous (eMethods in the Supplement). To account for time-varying pandemic severity, we included weekly state-level COVID-19 case and death rates. It is important to control for pandemic severity, given that evidence suggests that states with higher COVID-19 case and mortality rates experienced larger economic damage early in the pandemic (eMethods in the Supplement).25 We applied HPS sampling weights to our coefficient estimates, rendering them representative of the population.26 SE estimates are robust and corrected for clustering (sandwich estimator) at the state level to account for intrastate correlations.27
Beyond singular group-level differences, our second set of models examined the interactions between race/ethnicity, sex, and income to probe the social patterning of the outcomes and identify high-risk groups.16 We created 3-way interaction dummy variables between the categories, assigning the referent to non-Hispanic White men with high income. Sample sizes for each intersectional category are in eTable 4 in the Supplement. In all other aspects, the models are identical to those in the first analysis set.
Regressions were run separately for each composite outcome in Stata version 15 (StataCorp). Statistical significance was set at P < .05, and tests were 2-tailed. Our models are theoretically motivated, and we report odds ratios (ORs) or probabilities with confidence intervals for all factors,28 thereby minimizing the problems associated with multiple comparisons. We circumscribed results in terms of association; however, due to plausible within-state quasi-exogeneity of mobility changes that approximates random assignment,29 there is likely a strong correspondence between mobility restrictions and the outcomes.30 In sensitivity analyses, we (1) relaxed our assumption of a linear mobility dose response; (2) explored sensitivity to potential autocorrelation at the individual and state levels; (3) and compared point estimates sensitivity to weekly vs monthly mobility restriction measurements (eMethods in the Supplement).
Results
Mobility restrictions varied across states and declined between April and July 2020. Mobility restrictions tended to be highest in April and ranged between 15% to 60% across states in the first week of the survey (eFigure 1 and eFigure 2 in the Supplement). A mean (SD) of 90 692.8 (22 305.2) individuals responded weekly, at an average response rate of 7.7% for a total of 1 088 314 respondents during the 12 weeks.19 Respondents were aged between 18 and 88 years of age (mean [SD] age, 51.55 [15.74] years), and 826 039 (62.8%; 95% CI, 62.5%-63.1%) were non-Hispanic White individuals; 86 958 (12.5%; 95% CI, 12.4%-12.7%), African American individuals; 86 062 (15.2%; 95% CI, 15.0%-15.4%), Hispanic individuals; and 50 227 (5.6%; 95% CI, 5.5%-5.7%), Asian individuals (Table 1). More than half of the respondents were married (626 307 [54.1%; 95% CI, 53.8%-54.4%]); 561 570 (51.6%; 95% CI, 51.4%-51.9%) were women; and nearly one-third held a bachelor’s degree (314 574 [16.8%; 95% CI, 16.7%-17.0%]) or graduate degree (273 966 [13.5%; 95% CI, 13.4%-13.7%]). A quarter of the households had low income (188 469 [24.4%; 95% CI, 24.1%-24.6%]), and 272 473 (26.4%; 95% CI, 26.2%-26.7%) had lower-middle income.
Table 1. Socioeconomic Characteristics of 1 088 314 Participants in Sample.
| Characteristic | Participants, % (95% CI) |
|---|---|
| Age, y | |
| 18-34.9 | 27.6 (27.4-27.9) |
| 35-44.9 | 17.7 (17.5-17.9) |
| 45-54.9 | 16.2 (16.0-16.4) |
| 55-64.9 | 17.4 (17.2-17.6) |
| ≥65 | 21.0 (20.8-21.3) |
| Women | 51.6 (51.4-51.9) |
| Men | 48.4 (48.1-48.6) |
| Race | |
| Non-Hispanic White | 62.8 (62.5-63.1) |
| African American | 12.5 (12.4-12.7) |
| Asian | 5.6 (5.5-5.7) |
| Hispanic | 15.2 (15.0-15.4) |
| Other | 3.9 (3.8-4.0) |
| Education | |
| <High school | 2.6 (2.5-2.8) |
| Some high school | 5.9 (5.7-6.1) |
| High school graduate | 30.6 (30.3-30.9) |
| Some college | 21.3 (21.1-21.5) |
| Associate degree | 9.2 (9.0-9.3) |
| Bachelor’s degree | 16.8 (16.7-17.0) |
| Graduate degree | 13.5 (13.4-13.7) |
| Marital status | |
| Now married | 54.1 (53.8-54.4) |
| Widowed | 4.2 (4.1-4.3) |
| Divorced | 11.9 (11.8-12.1) |
| Separated | 2.3 (2.2-2.4) |
| Never married | 26.9 (26.6-27.1) |
| Household income in 2019, $ | |
| <$25 000 | 14.0 (13.7-14.2) |
| $25 000-$34 999 | 10.4 (10.2-10.6) |
| $35 000-$49 999 | 11.0 (10.8-11.2) |
| $50 000-$74 999 | 15.4 (15.3-15.6) |
| $75 000-$99 999 | 11.3 (11.1-11.4) |
| $100 000-$149 999 | 12.5 (12.4-12.7) |
| $150 000-$199 999 | 5.5 (5.5-5.6) |
| ≥$200 000 | 5.9 (5.8-6.0) |
| Household members, mean (95% CI), No. | |
| Adults | 2.8 (2.8-2.8) |
| Children | 0.7 (0.7-0.7) |
Table 2 shows the proportion of the population experiencing each well-being outcome; eTable 5 in the Supplement shows the estimated population affected. Among individuals who were not retired and willing to work, 18.8% (95% CI, 18.5%-19.0%; representing approximately 31.1 million individuals) experienced unemployment. Across all individuals, 22.4% (95% CI, 22.2%-22.7%; representing approximately 71.4 million individuals) experienced food insufficiency, 18.6% (95% CI, 18.3%-18.8%; representing approximately 60.8 million individuals) reported experiencing mental health problems, and 32.5% (95% CI, 32.2%-32.8%; representing approximately 107.2 million individuals) experienced inaccessibility of needed medical care for non–COVID-19 health problems in the previous month. Among those households with rent or mortgage payments, 15.1% (95% CI, 14.8%-15.3%; representing approximately 37.0 million individuals) did not pay last month’s rent or mortgage. Among households with children enrolled in school, 41.9% (95% CI, 41.4%-42.5%; representing approximately 29.5 million households) had class cancellations with no replacement of online or distance learning. There was a clear income gradient across all outcomes, with respondents with low income experiencing all domains at higher rates than respondents with lower-middle or high income. African American individuals experienced the highest burden of food insufficiency, inaccessibility of medical care, and rent or mortgage defaults. African American and Hispanic individuals experienced unemployment and cancellation of classes at similarly high rates. The prevalence of mental health problems was similar across all racial/ethnic groups.
Table 2. Prevalence of Outcomes Across Race/Ethnicity, Sex, and Income.
| Group | % (95% CI)a | |||||
|---|---|---|---|---|---|---|
| Pandemic-related class cancellations | Pandemic-related inaccessibility of medical care | Pandemic-related food insufficiency | Pandemic-related job losses | Mental health problems | Default on rent or mortgage | |
| Respondents, No. | 263 848 | 980 088 | 1 088 314 | 876 756 | 987 139 | 729 530 |
| All | 41.9 (41.4-42.5) | 32.5 (32.2-32.8) | 22.4 (22.2-22.7) | 18.8 (18.5-19.0) | 18.6 (18.3-18.8) | 15.1 (14.8-15.3) |
| Race/ethnicity | ||||||
| Non-Hispanic White | 38.8 (38.1-39.4) | 32.4 (32.1-32.7) | 19.3 (19.0-19.5) | 16.4 (16.1-16.6) | 17.6 (17.4-17.9) | 10.9 (10.6-11.1) |
| African American | 48.4 (47.0-49.9) | 34.3 (33.5-35.2) | 30.4 (29.7-31.2) | 22.6 (21.8-23.3) | 20.2 (19.4-20.9) | 27.2 (26.3-28.1) |
| Hispanic | 46.5 (44.9-48.1) | 31.3 (30.4-32.2) | 27.9 (27.1-28.7) | 23.1 (22.3-24.0) | 20.6 (19.8-21.4) | 20.2 (19.3-21.1) |
| Asian | 36.7 (34.7-38.8) | 27.1 (26.0-28.2) | 20.9 (19.9-22.0) | 21.0 (19.9-22.2) | 16.2 (15.2-17.3) | 14.2 (13.0-15.5) |
| Otherb | 43.4 (41.1-45.7) | 41.2 (39.9-42.6) | 28.6 (27.3-29.8) | 19.4 (18.2-20.6) | 24.9 (23.7-26.1) | 19.3 (18.0-20.6) |
| Income in 2019, $ | ||||||
| <35 000 | 50.9 (49.7-52.2) | 35.4 (34.8-36.0) | 34.3 (33.7-34.9) | 26.9 (26.3-27.5) | 27.3 (26.7-27.9) | 25.1 (24.5-25.8) |
| 35 000-75 000 | 44.9 (43.7-46.0) | 33.1 (32.6-33.6) | 23.6 (23.1-24.0) | 20.8 (20.3-21.3) | 18.9 (18.4-19.3) | 16 (15.5-16.4) |
| >75 000 | 34.9 (34.2-35.5) | 30.3 (30.0-30.6) | 16.0 (15.7-16.2) | 13.6 (13.4-13.9) | 13.0 (12.8-13.3) | 8.0 (7.8-8.3) |
| Sex | ||||||
| Men | 43.4 (42.5-44.3) | 29.3 (28.9-29.7) | 21.4 (21.0-21.7) | 19.1 (18.7-19.5) | 16.4 (16.0-16.7) | 14.2 (13.8-14.6) |
| Women | 40.7 (40.1-41.4) | 35.5 (35.2-35.9) | 23.4 (23.1-23.7) | 18.4 (18.1-18.7) | 20.6 (20.3-20.9) | 15.8 (15.5-16.2) |
Percentages reported in cells are probability-weighted and representative of the United States population aged 18 to 80 years.22
The Household Pulse survey defines the other category as “2 or more races plus other races, non-Hispanic.”
Mean (SD) mobility restriction was 24.8% (12.7) during the study period. In the fully adjusted logistic regression models with a linear mobility restriction exposure ranging from 1% to 60% (Figure 1), every 10% reduction in mobility was associated with higher odds of unemployment (OR, 1.3; 95% CI, 1.2-1.4), food insufficiency (OR, 1.1; 95% CI, 1.1-1.2), mental health problems (OR, 1.04; 95% CI, 1.0-1.1), and class cancellations (OR, 1.1; 95% CI, 1.1-1.2). Therefore, general population changes in these 4 outcomes were likely associated with the COVID-19 lockdown. Weekly mobility restrictions were not associated with inaccessibility of medical care or rent or mortgage defaults during the survey period. Our 3 sensitivity analyses yielded qualitatively similar findings. First, we found that the mobility dose responses for unemployment, class cancellations, and food insufficiency were linear (eFigure 3 in the Supplement). However, the association of mobility with mental health was attenuated. Second, the generalized estimating equation model, accounting for intra-individual correlations, provided similar estimates as our main model (eFigure 4 in the Supplement). Third, panel-data models, accounting for state-level autocorrelation, indicated that higher mobility restrictions were significantly associated with unemployment, food insufficiency, and class cancellations (eTable 6 in the Supplement). We found stronger correlations with mobility measured at the week level than at the month level.
Figure 1. Associations Between Changes in Mobility Restriction and in Outcomes.
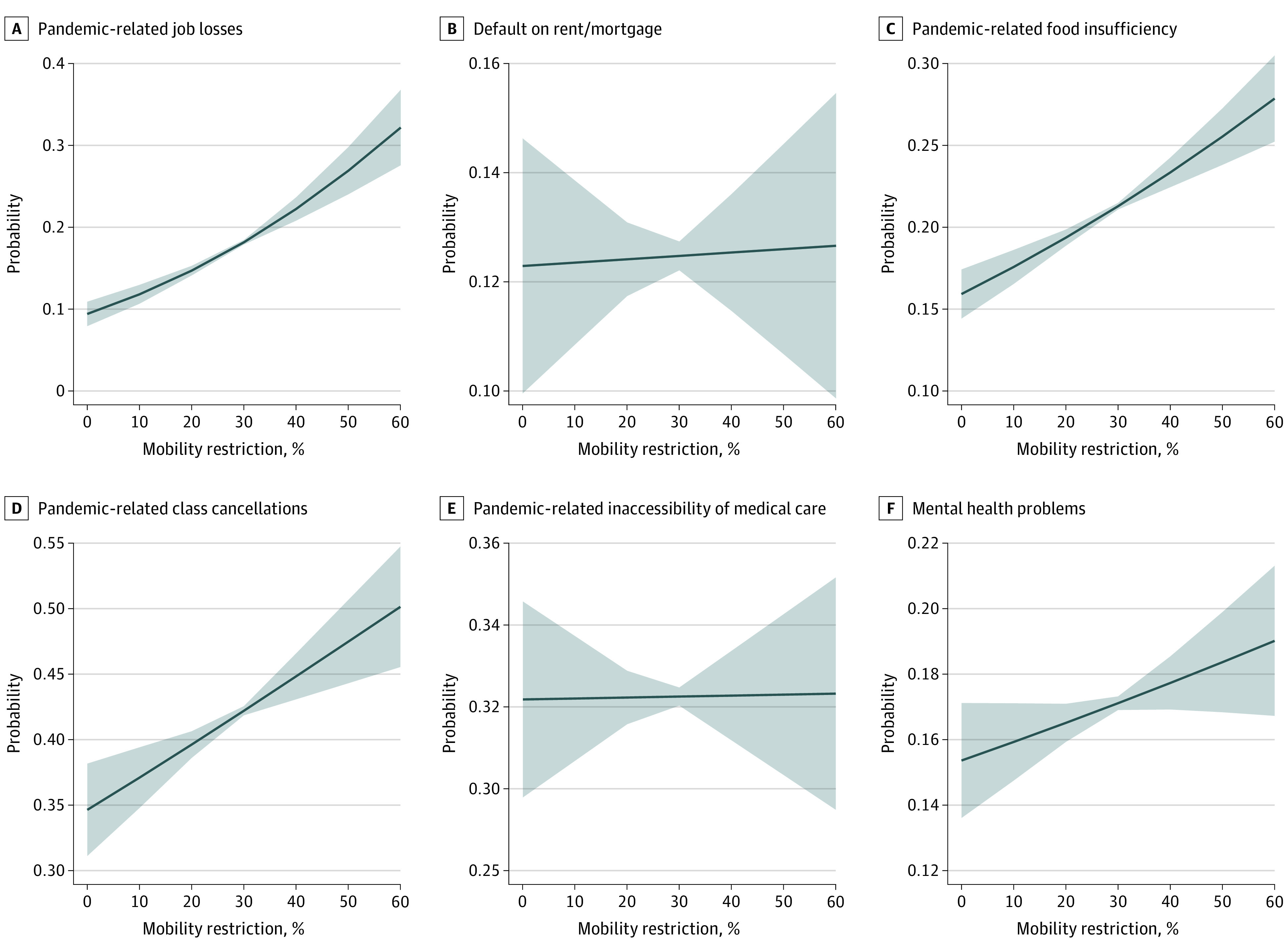
Solid lines represent probabilities from logistic regressions, holding all covariates at their sample means. Shaded areas represent 95% CIs. Mobility restriction represents within-state reductions in mobility based on week-to-week changes in mobility from normal levels. All models control for income, race/ethnicity, age, sex, education, marital status, numbers of individuals in the household, week of survey, state-level heterogeneity, and COVID-19 death and case rates. SE estimates are robust and clustered at the state level.
Individuals with low income were at the highest risk of experiencing all outcomes: unemployment (OR, 1.9; 95% CI, 1.8-2.0), food insufficiency (OR, 2.2; 95% CI, 2.1-2.3), mental health problems (OR, 2.0; 95% CI, 1.9-2.1), inaccessibility of medical care (OR, 1.3; 95% CI, 1.3-1.4), rent or mortgage defaults (OR, 2.6; 95% CI, 2.4-2.8), and class cancellations (OR, 1.6; 95% CI, 1.5-1.7) (Figure 2). Controlling for income and other covariates, compared with non-Hispanic White individuals, African American individuals experienced considerably higher risks of food insufficiency (OR, 1.3; 95% CI, 1.2-1.4), rent or mortgage defaults (OR, 2.0; 95% CI, 1.9-2.2), and class cancellations (OR, 1.3; 95% CI, 1.2-1.4). Hispanic individuals and women also experienced higher risks than non-Hispanic White individuals and men, respectively.
Figure 2. Risk of Outcome by Income, Race/Ethnicity, and Sex.
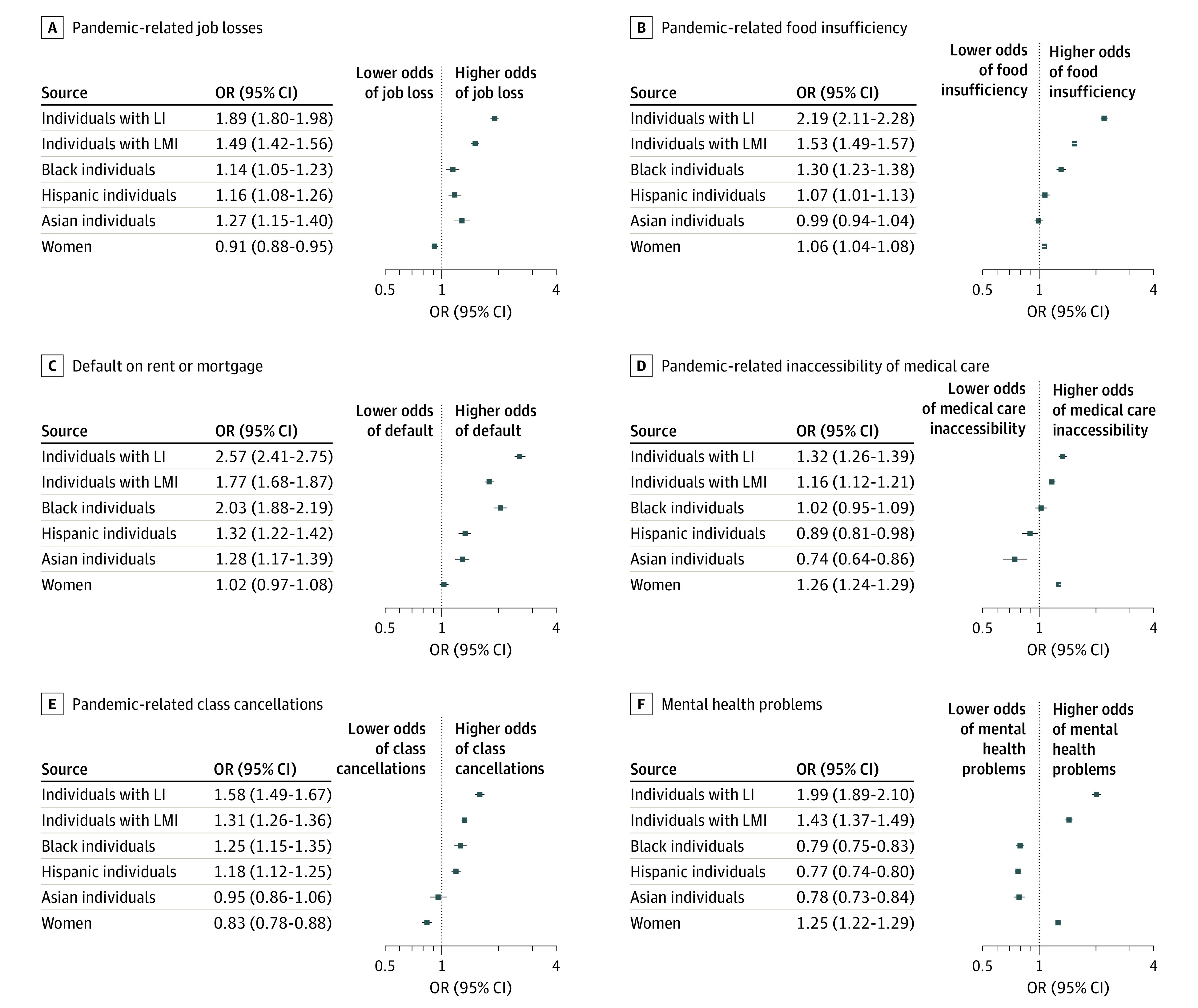
Dots are mutually adjusted point odds ratios, and whiskers represent 95% CIs. All models control for mobility, age, education, marital status, numbers of individuals in the household, week of survey, state-level heterogeneity, and COVID-19 death and case rates. SE estimates are robust and clustered at the state level. We provide more detail on the outcome descriptions in the legend for Figure 1. For African American, Hispanic, and Asian groups, the reference group was non-Hispanic White individuals. Low income (LI) was defined as households with income less than $35 000 per year; lower-middle income (LMI) are those with income between $35 000 and $75 000 per year. The reference group for low and lower-middle income groups is households with income greater than $75 000 per year.
Across most dimensions, African American individuals with low income experienced the highest risks (food insufficiency, men: OR, 3.3; 95% CI, 2.8-3.7; women: OR, 2.7; 95% CI, 2.5-3.0; mental health problems, men: OR, 1.9; 95% CI, 1.7-2.3; women: OR, 1.9; 95% CI, 1.8-2.1; medical care inaccessibility, men: OR, 1.3; 95% CI, 1.1-1.5; women: OR, 1.7; 95% CI, 1.6-1.9; class cancellations, men: OR, 2.0; 95% CI, 1.5-2.8; women: OR, 1.8; 95% CI, 1.6-2.0; unemployment, men: OR, 2.8; 95% CI, 2.5-3.2; women: OR, 2.0; 95% CI, 1.8-2.3; and rent/mortgage defaults, men: OR, 5.7; 95% CI, 4.7-7.1; women: OR, 5.3; 95% CI, 4.8-5.7) (Figure 3). Non-Hispanic White women with low income experienced the highest comparative risk of inaccessibility of medical care (OR, 1.8; 95% CI, 1.7-2.0); notably, African American women with high income were also at a higher risk of this outcome (OR, 1.7; 95% CI, 1.6-1.9) than the reference group. Non-Hispanic White women with low income (OR, 3.0; 95% CI, 2.7-3.2) were the most likely to experience mental health problems compared with the reference group. Hispanic men with low income (OR, 2.9; 95% CI, 2.5-3.4) experienced a higher risk of unemployment than the reference group.
Figure 3. Intersectionality of Sex, Race/Ethnicity, and Income: Groups With Highest Risks of Outcomes.
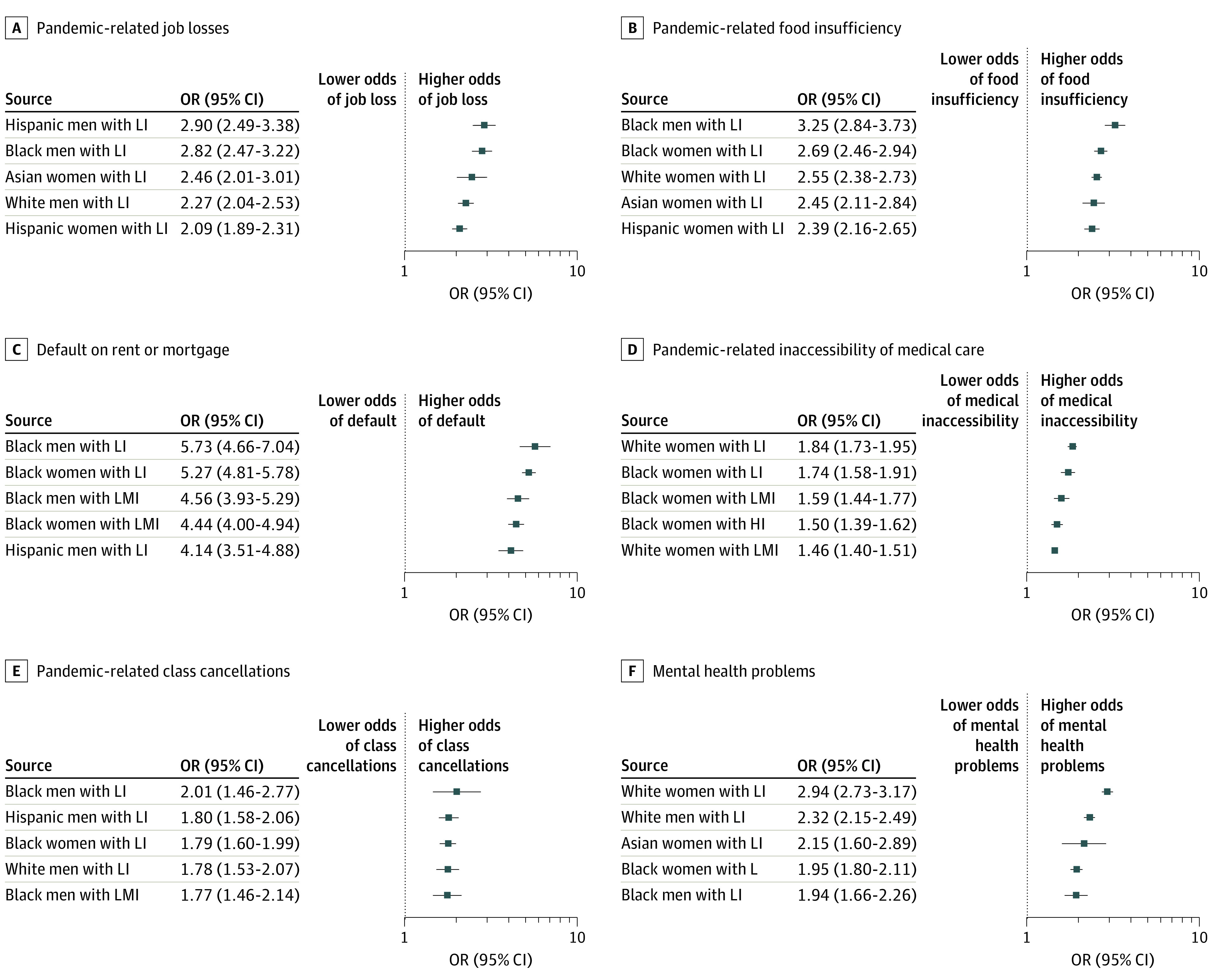
Dots are mutually adjusted odds ratios and whiskers represent 95% CIs. Models included 3-way interaction dummy variables for sex, race, and income groups. The reference group was non-Hispanic White men with high income (HI; ie, >$75 000/year). All models control for mobility, age, education, marital status, numbers of individuals in the household, week of survey, state-level heterogeneity, and COVID-19 death and case rates. SE estimates are robust and clustered at the state level. We provide more detail on the outcome descriptions in the legend for Figure 1. Low income (LI) was defined as households with income less than $35 000 per year; lower-middle income (LMI) are those with income between $35 000 and $75 000 per year.
Discussion
To our knowledge, this article provides the first population-representative distributional estimates of the associations of state-specific mobility restrictions with well-being. Our initial descriptions of population well-being suggested that low-income and African American populations were the most affected during the lockdowns across all outcomes. For several outcomes, while mobility restrictions significantly increased the risks for the average individual, wide confidence intervals indicated that these increases were highly heterogeneous across the population. Exploring this heterogeneity further, our first level of exposure stratification reaffirmed the findings from the initial well-being descriptions. Our second exposure stratification uncovered the intersecting identities most at risk of experiencing the outcomes, showing multiplicative differences in the ORs between those experiencing the most and least disadvantage across all outcomes. Women constituted 60% of these highest-risk groups; among these, African American women experienced the most risks to well-being.
In this study, we approached health from a well-being perspective and explored outcomes beyond the usual bounds of health and health care. We recognized conditions of unemployment, rent or mortgage defaults, and class cancellations as important,31 given that they can be upstream drivers of health.32 This paradigmatic move upstream enabled our analysis to better highlight racism at the headwaters of many health inequities.33 For example, unemployment is a distal factor associated with rates of overall mortality.32,34,35 Prior to the COVID-19 pandemic, and during the lockdowns (as evidenced in our results), unemployment rates among African American and Hispanic individuals exceeded overall national rates.36 Previous research has also shown that housing disparities are related to health, notably to the mental and physical health of African American individuals with mortgage strain,37,38,39 an unfortunately prevalent situation in our results, albeit with qualifications. Contributing to the literature showing a positive association between education and health,40 new studies have found an association between COVID-19–related education disruptions (including school nutrition41 and counselling service42 suspensions) to weight gain41 and mental health problems42 among adolescents, particularly among African American and Hispanic youth, groups that were also at higher risk in our results.
Our results also support existing evidence of sex as an intersecting component of health inequities.43 We found that women of all races/ethnicities with low income had some of the highest risks, with African American women at the highest risk of food insufficiency and inaccessibility of medical care. African American women with high income were also at a high risk of inaccessibility of medical care. Prior to the lockdowns, food insecurity44,45 and poor access to medical care,46 such as to prenatal care47 and cancer treatment,48 were prevalent among African American women. In addition, we found that non-Hispanic White individuals experienced the highest risk of mental health problems, which is consistent with prelockdown evidence of their likelihood of having49 and reporting50 mental health symptoms.
These findings support the notion that racism is a public health issue51 and suggest that blanket policies can be regressive if they ignore existing distributions of risks to well-being.52 Our results support the assertion of Ogedegbe and colleagues that “existing structural determinants—including inequality in housing, access to care, differential employment opportunities, and poverty—that remain pervasive”10 in African American and Hispanic communities align with the distribution of risks associated with COVID-19 policies. While mobility restrictions may be necessary to counter public health threats, underlying distributions of risk to well-being should inform corrective actions prior to implementation to minimize possible adverse distributional implications.
Even after the need for mobility restrictions has passed for the COVID-19 pandemic, recovery from the first stay-at-home orders may continue to be compounded by tenacious health disparities, which may require long-term corrective actions.53,54 Given persistent inequality in the United States,55 relief measures for those experiencing the greatest risks to well-being should not have arbitrary end dates. Instead, they should remain in place until economic indicators signal a robust recovery.56 Both during and after lockdowns, we encourage race/ethnicity–conscious, sex-conscious, and income-conscious policies for targeting assistance to promote health equity.57
Strengths and Limitations
This study has many strengths. First, we combined data sets with unique advantages, including representativeness, temporality, and COVID-19–pandemic relevance. Second, we established a plausible case for attribution given explicit survey language that led to self-reported causality by survey respondents. Additionally, the use of rigorous panel data techniques with large-sample repeated cross-sections lent confidence to our estimates. Third, by using intersectionality to identify those groups with the most risk, this analysis can improve public health policy targeting. Fourth, this study is relevant to current policy discussions on COVID-19 responses and racism as a public health issue.
This study is not without limitations. First, despite explicit survey language, there are inherent concerns associated with participants’ subjective reports of attribution. In the face of negative outcomes, participants may feel motivated to search for causal explanations58 and may choose to attribute their current state to the COVID-19 pandemic. Second, 2 outcomes, ie, default on rent or mortgage and inaccessibility of medical care, were not associated with mobility restrictions. Therefore, their significant adverse implications cannot be attributed directly to first-wave lockdowns. For these outcomes, we are less confident in the magnitudes of the associations, given the absence of baseline data. Third, we were unable to explore the interaction of mobility restrictions with subgroups because mobility responses to lockdowns are differential across socioeconomic groups, and mobility data with such granularity were unavailable.59
Conclusions
In this study, we found that groups that have historically been marginalized on the basis of race/ethnicity, sex, and income had higher risks of experiencing 6 negative well-being outcomes. Blanket public health policies that ignore existing distributions of risk to well-being may be associated with increased race/ethnicity–based, sex-based, and income-based inequities.
eMethods. Supplementary Methods
eFigure 1. Trend in Mobility Restriction Averaged Across US States in 2020
eFigure 2. Trend in Mobility Restriction Disaggregated by US States by Week of 2020 Household Pulse Survey
eFigure 3. Nonlinear Association Between Changes in Mobility Restriction and Changes in Outcomes
eFigure 4. Association Between Changes in Mobility Restriction and Changes in Outcomes Using Generalized Estimating Equations to Account for Within-Person Correlation
eTable 1. Definitions of Final Outcomes
eTable 2. Distributions of Intermediate Outcomes
eTable 3. Levels of Measurement in Outcomes and Covariates in the Merged Data Set
eTable 4. Intersectional Category Sample Sizes
eTable 5. Estimated Populations Affected, Calculated Using ACS Data
eTable 6. Panel-Data Regressions Using State-by-Week Averages of HPS Outcomes and Mobility Restriction
eReferences.
References
- 1.Gray DM II, Anyane-Yeboa A, Balzora S, Issaka RB, May FP. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nat Rev Gastroenterol Hepatol. 2020;17(9):520-522. doi: 10.1038/s41575-020-0330-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adhikari S, Pantaleo NP, Feldman JM, Ogedegbe O, Thorpe L, Troxel AB. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw Open. 2020;3(7):e2016938-e2016938. doi: 10.1001/jamanetworkopen.2020.16938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466-2467. doi: 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chowkwanyun M, Reed AL Jr. Racial health disparities and COVID-19—caution and context. N Engl J Med. 2020;383(3):201-203. doi: 10.1056/NEJMp2012910 [DOI] [PubMed] [Google Scholar]
- 5.IHME COVID-19 Forecasting Team . Modeling COVID-19 scenarios for the United States. Nat Med. 2021;27(1):94-105. doi: 10.1038/s41591-020-1132-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Allcott H, Boxell L, Conway JC, Ferguson BA, Gentzkow M, Goldman B. What explains temporal and geographic variation in the early US coronavirus pandemic? NBER Working Paper. 2020:27965. doi: 10.3386/w27965 [DOI] [Google Scholar]
- 7.Gezici A, Ozay O.. How Race and Gender Shape COVID-19 Unemployment Probability. University of Massachusetts Amherst; 2020. doi: 10.2139/ssrn.3675022 [DOI] [Google Scholar]
- 8.Kofman YB, Garfin DR. Home is not always a haven: the domestic violence crisis amid the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S199-S201. doi: 10.1037/tra0000866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bavli I, Sutton B, Galea S. Harms of public health interventions against COVID-19 must not be ignored. BMJ. 2020;371:m4074. doi: 10.1136/bmj.m4074 [DOI] [PubMed] [Google Scholar]
- 10.Ogedegbe G, Ravenell J, Adhikari S, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Netw Open. 2020;3(12):e2026881. doi: 10.1001/jamanetworkopen.2020.26881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Chavez AC, Backett-Milburn K, Parry O, Platt S. Understanding and researching wellbeing: its usage in different disciplines and potential for health research and health promotion. Health Education Journal. 2005;64(1):70-87. doi: 10.1177/001789690506400108 [DOI] [Google Scholar]
- 12.World Health Organization . Constitution of the World Health Organization. Accessed March 8, 2021. https://www.who.int/governance/eb/who_constitution_en.pdf
- 13.Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(7):e901-e908. doi: 10.1016/S2214-109X(20)30229-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams-Prassl A, Boneva T, Golin M, Rauh C. The impact of the coronavirus lockdown on mental health: evidence from the US. Human Capital and Economic Opportunity Working Group. Published 2020. Accessed October 10, 2020. https://ideas.repec.org/p/hka/wpaper/2020-030.html
- 15.Donaldson C, Mitton C. Health economics and emergence from COVID-19 lockdown: the great big marginal analysis. Health Econ Policy Law. 2020;1-5. doi: 10.1017/S1744133120000304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evans CR, Williams DR, Onnela J-P, Subramanian SV. A multilevel approach to modeling health inequalities at the intersection of multiple social identities. Soc Sci Med. 2018;203:64-73. doi: 10.1016/j.socscimed.2017.11.011 [DOI] [PubMed] [Google Scholar]
- 17.US Census Bureau . Source of the data and accuracy of the estimates for the 2020 Household Pulse Survey. Published 2020. Accessed March 8, 2021. https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/Source-and-Accuracy-Statement-July-16-July-21.pdf
- 18.US Census Bureau . Design and operation of the 2020 Household Pulse Survey, 2020. Published 2020. Accessed March 8, 2021. https://www.census.gov/programs-surveys/household-pulse-survey/technical-documentation.html#phase1
- 19.US Census Bureau . Household Pulse Survey. Published 2020. Accessed October 13, 2020. https://www.census.gov/householdpulse
- 20.Johns Hopkins University and Medicine . Johns Hopkins coronavirus resource center. Accessed February 22, 2021. https://coronavirus.jhu.edu/
- 21.Institute of Health Metrics and Evaluation . COVID-19 resources. Accessed March 8, 2021. http://www.healthdata.org/covid
- 22.US Census Bureau . American Community Survey. Accessed February 25, 2021. https://www.census.gov/acs/www/data/data-tables-and-tools/american-factfinder/
- 23.Statista Research Department . US income distribution 2019. Published 2020. Accessed February 22, 2021. https://www.statista.com/statistics/203183/percentage-distribution-of-household-income-in-the-us/
- 24.Blakely TA, Woodward AJ. Ecological effects in multi-level studies. J Epidemiol Community Health. 2000;54(5):367-374. doi: 10.1136/jech.54.5.367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polyakova M, Kocks G, Udalova V, Finkelstein A. Initial economic damage from the COVID-19 pandemic in the United States is more widespread across ages and geographies than initial mortality impacts. Proc Natl Acad Sci U S A. 2020;117(45):27934-27939. doi: 10.1073/pnas.2014279117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Solon G, Haider SJ, Wooldridge JM. What are we weighting for? J Hum Resources. 2015;50(2):301-316. doi: 10.3368/jhr.50.2.301 [DOI] [Google Scholar]
- 27.Guillaume B, Hua X, Thompson PM, Waldorp L, Nichols TE; Alzheimer’s Disease Neuroimaging Initiative . Fast and accurate modelling of longitudinal and repeated measures neuroimaging data. Neuroimage. 2014;94:287-302. doi: 10.1016/j.neuroimage.2014.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakagawa S. A farewell to Bonferroni: the problems of low statistical power and publication bias. Behavioral Ecology. 2004;15(6):1044-1045. doi: 10.1093/beheco/arh107 [DOI] [Google Scholar]
- 29.Borusyak K, Hull P. Non-random exposure to exogenous shocks: theory and applications. NBER Working Paper. 2020:27845. doi: 10.3386/w27845 [DOI] [Google Scholar]
- 30.Hernán MA, Robins JM. Causal Inference: What If. Chapman and Hall/CRC; 2020. [Google Scholar]
- 31.Ku L, Brantley E. Widening social and health inequalities during the COVID-19 pandemic. JAMA Health Forum. 2020;1(6):e200721. doi: 10.1001/jamahealthforum.2020.0721 [DOI] [PubMed] [Google Scholar]
- 32.Jin RL, Shah CP, Svoboda TJ. The impact of unemployment on health: a review of the evidence. CMAJ. 1995;153(5):529-540. [PMC free article] [PubMed] [Google Scholar]
- 33.Schulz AJ, Mehdipanah R, Chatters LM, Reyes AG, Neblett EW Jr, Israel BA. Moving health education and behavior upstream: lessons from COVID-19 for addressing structural drivers of health inequities. Health Educ Behav. 2020;47(4):519-524. doi: 10.1177/1090198120929985 [DOI] [PubMed] [Google Scholar]
- 34.Brenner MH, Mooney A. Unemployment and health in the context of economic change. Soc Sci Med. 1983;17(16):1125-1138. doi: 10.1016/0277-9536(83)90005-9 [DOI] [PubMed] [Google Scholar]
- 35.Dorling D. Unemployment and health. BMJ. 2009;338:b829. doi: 10.1136/bmj.b829 [DOI] [PubMed] [Google Scholar]
- 36.Lo CC, Cheng TC. Race, unemployment rate, and chronic mental illness: a 15-year trend analysis. Soc Psychiatry Psychiatr Epidemiol. 2014;49(7):1119-1128. doi: 10.1007/s00127-014-0844-x [DOI] [PubMed] [Google Scholar]
- 37.Libman K, Fields D, Saegert S.. Housing and health: a social ecological perspective on the US foreclosure crisis. Housing Theor Soc. 2012;29(1):1-24. doi: 10.1080/14036096.2012.624881 [DOI] [Google Scholar]
- 38.Keene DE, Lynch JF, Baker AC. Fragile health and fragile wealth: mortgage strain among African American homeowners. Soc Sci Med. 2014;118:119-126. doi: 10.1016/j.socscimed.2014.07.063 [DOI] [PubMed] [Google Scholar]
- 39.Cannuscio CC, Alley DE, Pagán JA, et al. Housing strain, mortgage foreclosure, and health. Nurs Outlook. 2012;60(3):134-142, 142.e1. doi: 10.1016/j.outlook.2011.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ross CE, Wu C. The links between education and health. Am Sociol Rev. 1995;60(5):719-745. doi: 10.2307/2096319 [DOI] [Google Scholar]
- 41.Rundle AG, Park Y, Herbstman JB, Kinsey EW, Wang YC. COVID-19-related school closings and risk of weight gain among children. Obesity (Silver Spring). 2020;28(6):1008-1009. doi: 10.1002/oby.22813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatr. 2020;174(9):819-820. doi: 10.1001/jamapediatrics.2020.1456 [DOI] [PubMed] [Google Scholar]
- 43.Ryan NE, El Ayadi AM. A call for a gender-responsive, intersectional approach to address COVID-19. Glob Public Health. 2020;15(9):1404-1412. doi: 10.1080/17441692.2020.1791214 [DOI] [PubMed] [Google Scholar]
- 44.Odoms-Young A, Bruce MA. Examining the impact of structural racism on food insecurity: implications for addressing racial/ethnic disparities. Fam Community Health. 2018;41(Suppl 2 Suppl, Food Insecurity and Obesity):S3-S6. doi: 10.1097/FCH.0000000000000183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coleman-Jensen A, Gregory C, Singh A. Household food security in the United States in 2013. Published September 2014. Accessed March 8, 2021. https://www.ers.usda.gov/webdocs/publications/45265/48787_err173.pdf
- 46.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57(suppl 1):108-145. doi: 10.1177/1077558700057001S06 [DOI] [PubMed] [Google Scholar]
- 47.Kogan MD, Kotelchuck M, Alexander GR, Johnson WE. Racial disparities in reported prenatal care advice from health care providers. Am J Public Health. 1994;84(1):82-88. doi: 10.2105/AJPH.84.1.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Parham G, Phillips JL, Hicks ML, et al. The National Cancer Data Base report on malignant epithelial ovarian carcinoma in African-American women. Cancer. 1997;80(4):816-826. doi: [DOI] [PubMed] [Google Scholar]
- 49.Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A. 2015;112(49):15078-15083. doi: 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lo CC, Cheng TC. The role of social structural factors in treatment of mental health disorder. J Ment Health. 2012;21(5):430-438. doi: 10.3109/09638237.2012.664303 [DOI] [PubMed] [Google Scholar]
- 51.Devakumar D, Selvarajah S, Shannon G, et al. Racism, the public health crisis we can no longer ignore. Lancet. 2020;395(10242):e112-e113. doi: 10.1016/S0140-6736(20)31371-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dingel JI, Neiman B. How many jobs can be done at home? J Public Econ. 2020;189:104235. doi: 10.1016/j.jpubeco.2020.104235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yancy CW. COVID-19 and African Americans. JAMA. 2020;323(19):1891-1892. doi: 10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]
- 54.Wolfson JA, Leung CW. Food insecurity during COVID-19: an acute crisis with long-term health implications. Am J Public Health. 2020;110(12):1763-1765. doi: 10.2105/AJPH.2020.305953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chetty R, Grusky D, Hell M, Hendren N, Manduca R, Narang J. The fading American dream: trends in absolute income mobility since 1940. Science. 2017;356(6336):398-406. doi: 10.1126/science.aal4617 [DOI] [PubMed] [Google Scholar]
- 56.Parrott S, Stone C, Huang C-C, et al. CARES Act includes essential measures to respond to public health, economic crises, but more will be needed. Center on Budget and Policy Priorities. Published March 27, 2020. Accessed March 8, 2021. https://www.cbpp.org/research/economy/cares-act-includes-essential-measures-to-respond-to-public-health-economic-crises
- 57.Schmidt H, Gostin LO, Williams MA. Is it lawful and ethical to prioritize racial minorities for COVID-19 vaccines? JAMA. 2020;324(20):2023-2024. doi: 10.1001/jama.2020.20571 [DOI] [PubMed] [Google Scholar]
- 58.Bohner G, Bless H, Schwarz N, Strack F. What triggers causal attributions? the impact of valence and subjective probability. Eur J Soc Psychol. 1988;18(4):335-345. doi: 10.1002/ejsp.2420180404 [DOI] [Google Scholar]
- 59.Weill JA, Stigler M, Deschenes O, Springborn MR. Social distancing responses to COVID-19 emergency declarations strongly differentiated by income. Proc Natl Acad Sci U S A. 2020;117(33):19658-19660. doi: 10.1073/pnas.2009412117 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Supplementary Methods
eFigure 1. Trend in Mobility Restriction Averaged Across US States in 2020
eFigure 2. Trend in Mobility Restriction Disaggregated by US States by Week of 2020 Household Pulse Survey
eFigure 3. Nonlinear Association Between Changes in Mobility Restriction and Changes in Outcomes
eFigure 4. Association Between Changes in Mobility Restriction and Changes in Outcomes Using Generalized Estimating Equations to Account for Within-Person Correlation
eTable 1. Definitions of Final Outcomes
eTable 2. Distributions of Intermediate Outcomes
eTable 3. Levels of Measurement in Outcomes and Covariates in the Merged Data Set
eTable 4. Intersectional Category Sample Sizes
eTable 5. Estimated Populations Affected, Calculated Using ACS Data
eTable 6. Panel-Data Regressions Using State-by-Week Averages of HPS Outcomes and Mobility Restriction
eReferences.


