CLINICAL HISTORY
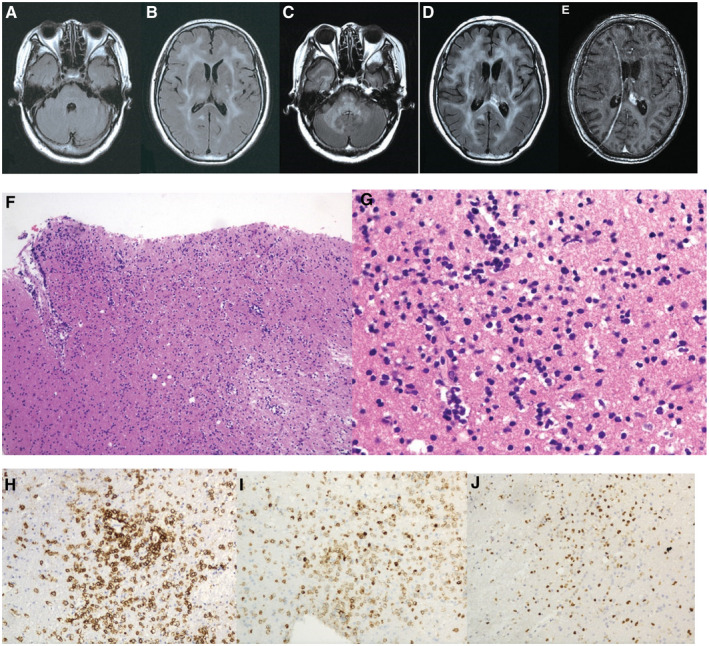
A 66‐year‐old Chinese woman presented with progressive cognitive decline, difficulty for calculating and dizziness for 2 years. She complained of bilateral limb weakness and gait disturbance which was characterized by small steps without falling for 1 month. No headache, nausea, vomiting, dysphagia, dysarthria, urinary incontinence, seizure attack, fever. Neurological examination showed an apathetic patient with severe cognitive decline (MMSE score was 14/30) and decreased muscle strength with limb spasm bilaterally. No hepatosplenomegaly and lymphadenopathy. Lumbar puncture showed normal pressure with mild lymphocytosis, glucose of 36 mg/dl, and protein of 60 mg/dl. PCR of CSF HSV and CMV returned negative. CSF was also negative for IgG oligoclonal bands. Serum EBV IgG was positive. EEG showed slowing of the normal background diffusely. Cranial MRI exhibited diffuse white matter changes, involving periventricular area, frontoparietal white matter, without mass effect (Figure 1A,B). Repeated MRI revealed progressive leukoencephalopathy involving brainstem and cerebellar peduncle (Figure 1C,D) with mild periventricular enhancement 5 months later (Figure 1E). Brain biopsy targeting periventricular deep white matter was therefore performed.
Figure 1.
PATHOLOGICAL FINDINGS
Microscopic histopathological examination of the surgical specimen from deep white matter revealed diffuse atypical lymphoid cells with enlarged round nuclei (Figure 1F,G). Necrosis was absent. These tumor cells were not cohesive. They infiltrated sub‐cortical white matter without solid mass formation. Mitotic figures were significant. Immunostains were positive for CD20 (Figure 1H), and CD79_ (Figure 1I), but negative for CD3, CD5, CD10, and CD56. EBER in situ hybridization was positive (not shown) and the ki‐67 was 50% (Figure 1J). What is your diagnosis?
DIAGNOSIS
Lymphomatosis cerebri (LC).
DISCUSSION
Primary central nervous system lymphoma (PCNSL) is an extranodal non‐Hodgkin lymphoma constituting about 3% of all brain tumors, which has higher prevalence in immunocompromised patients. PCNSL is confined to the brain, leptomeninges, eyes, and spinal cord. Pathologically, most common type of PCNSL is DLBCL, which is strongly positive for CD20 staining. LC, firstly reported in 1999, is considered a very rare variant of DLBCL. Clinical manifestations include cognitive decline, gait disturbances and behavioral changes, which can be routinely considered as rapid progressive dementia (RPD). Almost all PCNSL presents lesions with distinct mass‐effect, homogeneous or ring enhancement on MRI. However, LC is the rare exception which is characterized by diffuse leukoencephalopathy without enhancement or mild enhancement on MRI 1. Differential diagnosis of subacute or chronic progressive dementia with diffuse leukoencephalopathy is always a diagnostic challenge. Toxic encephalopathy, infections or inflammation, hereditary vascular disorders, adult‐onset leukodystrophy, and gliomatosis cerebri can cause similar neuroimaging features. Toxic leukoencephalopathy can present with diffuse and symmetrical leukoencephalopathy. Contact history of certain objects, such as carbon monoxide, heroin, and chemotherapeutic drugs may provide clues for diagnosis. Progressive multifocal leukoencephalopathy (PML), caused by JC virus infection, should be considered. Cranial MRI always exhibits asymmetrical multifocal nonconsecutive non‐enhancement lesions, which is a different feature compared with LC. CSF PCR for JC virus can provide evidence for diagnosis. Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is a hereditary vascular disorder presenting with progressive dementia and diffuse leukoencephalopathy. Genetic test always reveals NOTCH 3 gene mutation on chromosome 19, which can make definite diagnosis. Adult‐onset adrenoleukodystrophy (ALD) has its specific location of lesions on MRI, characterized by the symmetrical parieto‐occipital leukoencephalopathy. Serum very long chain fatty acid (VLCFA) is always elevated. Gliomatosis cerebri always shows diffuse non‐enhancing leukoencephalopathy, which is very difficult for differentiation without brain biopsy.
Several immunohistochemical markers are recommended for the differential diagnosis of aggressive lymphomas. Phenotypically, B‐cell non‐Hodgkin lymphomas express pan‐B‐cell markers such as CD20, CD19, CD22 and CD79α, which constitute 92%–98% of PCNSL. Proliferative activity of DLBCL is generally high with Ki‐67 labeling indices of 50%–70%. Rare cases of Burkitt Lymphomas show an extremely high Ki‐67 up to 99% with the CD10 positive tumor cells. The EBV genome is present in tumors in the majority of cases. Considering the primary T‐cell lymphomas, the typical immunophenotype is CD3 and CD5. NK/T cell lymphoma confined to the CNS is extremely rare. The tumor cells are positive for CD56and CD2. On pathological examination, LC shows the feature of proliferation of B‐lymphocytes. These cells are not cohesive nor form solid tumor. The lesions are always characterized by non‐enhanced or mild‐enhanced symmetrical progressive leukoencephalopathy. These are the features for differentiation of typical DLBCL. This patient also has positive serum EBV antibody as well as positive EBER staining, which indicated that EBV infection may play an important role in pathogenesis of LC.
Once diagnosed of LC, chemotherapy combined with radiotherapy may improve the outcome. Corticosteroids can decrease tumor‐associated edema and may lead to partial radiographic regression of tumors. An initial response to corticosteroids is associated with a favorable outcome. However, almost all patients quickly experience relapse without other treatment. High‐dose chemotherapy (HDT) including administration of methotrexate (MTX), cytarabine, rituximab, and thiotepa, followed by autologous stem cell transplantation (ASCT), has been reported associated with favorable response rate for diffuse large B cell lymphoma. These therapies combined with whole‐brain radiotherapy (WBRT) may prolong survival time for the patients. Resection is not recommended because of diffuse distribution of lesions. However, due to delayed diagnosis, 50% LC patients survived not longer than 3 months after the diagnosis 2. Although LC has poor prognosis, early diagnosis and proper treatment at the early stage of disease can improve prognosis 3.
In conclusion, patients presenting with progressive cognitive decline with diffuse non‐enhancing leukoencephalopathy on MRI scan, should increase suspicion of LC. Early brain biopsy is always encouraged.
ACKNOWLEDGMENTS
Sheng Chen and Meng‐Sha Yao contributed equally to this case.
This work was supported by grants from the National Natural Sciences Foundation of China (81671241) and Shanghai New Youth Science and technology Project (15QA1403000) and Shanghai youth doctor training program.
REFERENCES
- 1. Kitai R, Hashimoto N, Yamate K, Ikawa M, Yoneda M, Nakajima T et al (2012) Lymphomatosis cerebri: clinical characteristics, neuroimaging, and pathological findings. Brain Tumor Pathol 29:47–53. [DOI] [PubMed] [Google Scholar]
- 2. Izquierdo C, Velasco R, Vidal N, Sanchez JJ, Argyriou AA, Besora S et al (2016) Lymphomatosis cerebri: a rare form of primary central nervous system lymphoma. Analysis of 7 cases and systematic review of the literature. Neuro Oncol 18:707–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Samani A, Davagnanam I, Cockerell OC, Ramsay A, Patani R, Chataway J (2015) Lymphomatosis cerebri: a treatable cause of rapidly progressive dementia. J Neurol Neurosurg Psychiatry 86:238–240. [DOI] [PMC free article] [PubMed] [Google Scholar]


